Abstract
Background:
Long-term therapy with metformin was shown to decrease the Vitamin B12 level and manifested as peripheral neuropathy.
Aim:
The aim of this study is to define the prevalence of Vitamin B12 deficiency in early Type 2 diabetic patients (duration ≤5 years or drug treatment ≤3 years) and the relationship among metformin exposure and levels of cobalamin (Cbl), folic acid, and homocysteine (Hcy) with severity of peripheral neuropathy.
Methodology:
This is a cross-sectional study involving randomly selected ninety patients (male 56, female 34) between age groups of 35 and 70 years, comparing those who had received >6 months of metformin (Group A) (n = 35) with those without metformin (Group B) (n = 35) and patients taking metformin with other oral hypoglycemic agent (Group C) (n = 20). Comparisons were made clinically, biochemically (serum Cbl, fasting Hcy, and folic acid), and with electrophysiological measures (nerve conduction studies of all four limbs). Comorbidities contributing to neuropathy were excluded from the study.
Results:
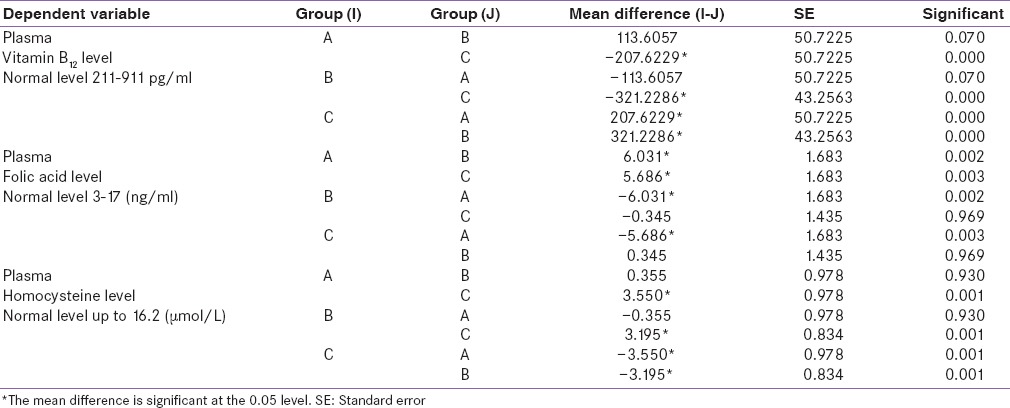
Group A patients (54.28%) were prone to develop peripheral neuropathy comparing Group B (28.57%) and Group C (35%). There was significantly low plasma level of Cbl in Group A (mean 306.314 pg/ml) than in Group B (mean 627.543 pg/ml) and Group C (mean 419.920 pg/ml). There was insignificant low-level plasma folic acid in Group A (16.47 ng/ml) than in Group B (16.81 ng/ml) and Group C (22.50 ng/ml). There was significantly high level of Hcy in Group A (mean 17.35 µmol/L) and Group C (mean 16.99 µmol/L) than in Group B (mean 13.22 µmol/L). Metformin users even for 2 years showed evidence of neuropathy on nerve conduction velocity though their body mass index and postprandial blood sugar were maintained. There was significant difference in between groups regarding plasma Cbl, folic acid, and Hcy level as significance level <0.05 in all three groups (F [2, 87] = 28.1, P = 0.000), (F [2, 87] = 7.43, P = 0.001), (F [2, 87] = 9.76, P = 0.000). Post hoc study shows significant (P < 0.05) lowering of Cbl and Hcy level in Group A (mean = 306.314, standard deviation [SD] = 176.7) than in Group C (mean = 419.92, SD = 208.23) and Group B (mean = 627.543, SD = 168.33).
Discussion:
Even short-term treatment with metformin causes a decrease in serum Cbl folic acid and increase in Hcy, which leads to peripheral neuropathy in Type 2 diabetes patients. A multicenter study with heterogeneous population would have increased the power of the study. We suggest prophylactic Vitamin B12 and folic acid supplementation or periodical assay in metformin user.
Keywords: Diabetes mellitus, metformin, screening, Vitamin B12 deficiency
INTRODUCTION
Diabetes mellitus (DM) is associated with risk of cardiovascular diseases, which cannot be fully justified by important risk factors such as hyperglycemia,[1] hypertension,[2] and dyslipidemia.[3] Among all risk factors, homocysteine (Hcy) is recognized as an independent,[4] and potentially modifiable,[5] risk factor that may be strongly linked to cardiovascular prognosis in Type 2 diabetes.[6] It can also be a determinant of microalbuminuria and diabetic retinopathy.
Hcy is produced during the demethylation of methionine. It is normally metabolized by two pathways, remethylation and transsulfuration. Remethylation acts as a catalyst for methionine synthase. In this reaction, 5-methyltetrahydrofolate is a methyl group donor and Vitamin B12 is a cofactor.
Several studies found decreased serum Vitamin B12 level among metformin-treated diabetes patients[7] probably due to malabsorption.[8] Hence, during metformin treatment, Hcy level might increase, but data on this issue are contradictory.[9,10]
With this idea in mind, we conducted a study at B.R. Singh Hospital, Kolkata, among the Type 2 diabetic patients who are on metformin for at least 2 years but not more than 3 years after they were first detected with diabetes and compared them with patients not on metformin for the same duration. The effects of metformin treatment on serum levels of Hcy, Vitamin B12 and folate level in patients with Type 2 diabetes were studied.
Aims and objectives
To study the blood level of Vitamin B12, folic acid, and Hcy in metformin-treated early Type 2 DM
To study the evidence of peripheral neuropathy in metformin-treated early Type 2 DM.
METHODOLOGY
A hospital-based, comparative, descriptive study was conducted in the Department of Medicine, B.R. Singh Hospital, Kolkata, during August 2010–June 2012. A total of ninety patients were recruited for the study after proper screening and sampling. Systematic sampling procedure was used as sampling. Here, three groups were created and they are as follows. Group A (20 patients): Patients on tablet metformin with other oral hypoglycemic agent (OHA) treatment, Group B (35 patients): Patient on tablet metformin, and Group C (35 patients): Patient on other OHA than metformin. Patients were diagnosed by the American Diabetes Association (ADA) guidelines. All the patients were properly examined and related tests were conducted according to the protocol.
Nerve conduction velocity (NCV) tests were performed using RMS EMG EP MARK II 2 CH Machine kit in all patients, and results were assessed according to the ADA diabetic neuropathy protocol. The NCV studies were carried out through device. Median, ulnar, peroneal nerve conduction studies, F-wave, and median, ulnar, and sural NCVs were recorded at room temperature maintained at 22–24°C. Standard NCVs were used.
Polyneuropathy types were described as either demyelinating or axonal.
Demyelinating neuropathy was diagnosed as:
A reduction of conduction velocities of at least 40% in at least 2 motor or 1 sensory nerves
Prolonged terminal motor latencies
Partial conduction block
An absent F-wave or prolonged F-wave latencies in 2 or more motor nerves.
Axonal neuropathy was diagnosed as:
Conduction velocities were normal
The size of compound muscle action potential and sensory nerve action potentials were decreased in at least two motor nerves and one sensory nerve.
Inclusion criteria for patients:
Patient detected with Type 2 DM with disease duration <5 years
Patients getting treatment for Type 2 DM not more than 3 years
Patients getting metformin up to 2 g per day.
Exclusion criteria for patients:
Patients suffering from diabetes more than 5 years
Patients who are strictly on vegetarian diet
Patients suffering from multiple complications of Type 2 DM and overt diabetic
Patients suffering from kidney, liver, thyroid diseases
Patients with alcohol abuse, smoker
Family history of peripheral nerve disease
History of malignancies
History of toxic exposure and drug exposure causing peripheral neuropathy
Patients with autoimmune disorder or pregnancy
Unconscious and severely ill patients
Patients who were mentally impaired and/or unable to give consent.
An informed consent based on an appreciation and understanding of the study and its procedures was taken from each patient, and the study was approved by the Institutional Ethical Committee.
Data were collected and diagram was prepared on the basis of baseline demographic parameters and the statistical analysis was done using SPSS version 11.5 (SPSS Inc, headquartered in Chicago, IL, USA) for ANOVA, post hoc test, and Chi-square test keeping α level to 0.05.
RESULTS
A total ninety diabetes patient were followed. Among them, twenty patients belonged to Group A (patients on tablet metformin with other OHA treatment), 35 patients belonged to Group B (patient on tablet metformin), and the rest 35 patients belonged to Group C (patient on other OHA than metformin).
The mean ± standard deviation (years) of age of Groups A, B, and C were 49.45 ± 5.41, 50.46 ± 7.48, and 50.46 ± 4.96, respectively. Totally, 34 females and 56 males participated in the study [Table 1].
Table 1.
Participants, treatment and Bio-chemistry related characteristic of three groups
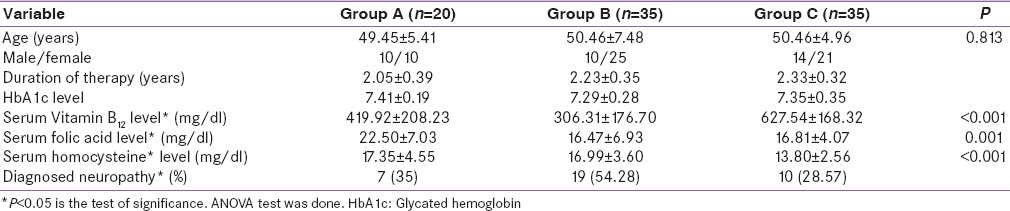
The serum Vitamin B12 level is much higher among patients who did not take tablet metformin. This difference is statistically significant by ANOVA test. The level of folic acid is significantly lower among Group B than other groups. It is also observed that 54.28% of Group B patients have neuropathy, which is much higher than Group A (35%) and Group C (28.57%) [Table 1]. Sensory neuropathy is only present among of them [Table 2].
Table 2.
Neuropathy present in study population
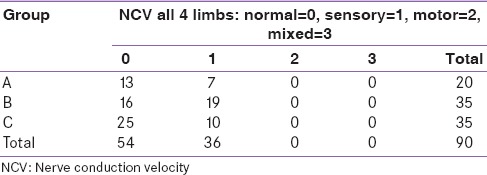
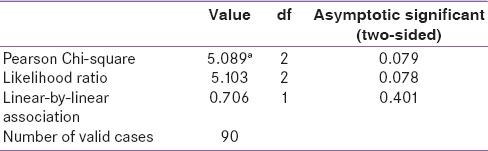
In Chi-square test, a trend of association observed that metformin users were more prone to develop sensory neuropathy [Table 3].
Table 3.
Chi-square tests
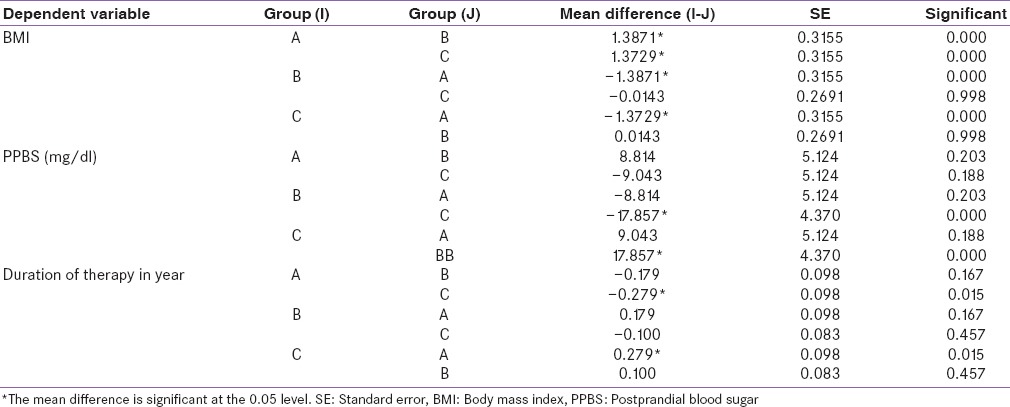
Post hoc study shows that there is significant lowering in the level of Vitamin B12 and Hcy level in patients who are using only metformin for controlling blood sugar than who are using metformin with other OHD and who are controlling it without metformin. Plasma folic acid level has insignificant variation in metformin user and not metformin user groups; this may be due to their food habit [Table 4].
Table 4.
Post hoc test of plasma Vitamin B12, folic acid, homocysteine level
These significant differences were observed among three groups related with body mass index (BMI), postprandial blood sugar (PPBS), and duration of therapy by post hoc test [Table 5].
Table 5.
Post hoc test of body mass index, postprandial blood sugar, and duration of therapy
DISCUSSION
Metformin, an oral biguanide, has been used as antidiabetic agent for more than 40 years. The UK Prospective Diabetes Study recommends lifestyle modification and metformin to be the first-line therapy for Type 2 DM. However, long-term therapy with metformin was shown to decrease the Vitamin B12 level and manifested as peripheral neuropathy, cognitive impairment, subacute degeneration of cord with macrocytic anemia.[8,9,11,12,13] Even short-term therapy with metformin can cause a decrease in serum Vitamin B12 and folic acid level and an increase in Hcy level.[11] In our study, we found that study population using only metformin (54.28%) is prone to develop peripheral neuropathy than study population with no metformin (28.57%) and metformin with other drugs (35%). There is significant low level of plasma Vitamin B12 associated with only metformin therapy (mean 306.314 pg/ml), than without metformin (mean 627.543 pg/ml) and metformin with other drugs (mean 419.920 pg/ml); patients using metformin either as alone or along with other drug have a trend to develop Vitamin B12 deficiency. There is insignificant low level of plasma folic acid in only metformin user (mean 16.47 ng/ml) than in no metformin (16.81 ng/ml) and metformin with other drugs (22.50 ng/ml); this may be due to the fact that all of our patients are having good dietary advice and taking a good amount of green leafy vegetables. There are significant high levels of Hcy in population with only metformin therapy (mean 17.35 µmol/L) and population taking metformin with other drugs (mean 16.99 µmol/L) than in population not taking metformin (mean 13.22 µmol/L). From our study, it is seen that BMI is better controlled in patients who are taking metformin only for DM control than other two groups. This may be due to the fact that some of our patients are on thiazolidinediones which can cause an increase in body weight[14] although there is insignificant BMI variation in metformin and no metformin group. From our study, it is seen that PPBS is well controlled in only metformin user group than in other two groups of patients; from this result, we may say that metformin use can control PPBS well, along with other groups of drugs such as α-glucosidase inhibitors. In our study, patients with Vitamin B12 deficiency presented clinically either with symptoms of altered joint position sense, large fiber neuropathy, or asymptomatic.
Tomkin et al. showed that metformin is one of the pharmacological causes of Vitamin B12 deficiency, and it is evident that from their study, 10% to 30% patients developed evidence of Vitamin B12 deficiency.[12] Pflipsen et al. in another study showed a 22% prevalence of Vitamin B12 in metformin-treated DM.[15] In our study, population who were taking only metformin have a lower mean Vitamin B12 level than population taking other drugs with metformin and population who are not taking metformin at all. Wile and Toth showed in their study that more than 6 months treatment with metformin could cause a low level of Vitamin B12 and a high level of Hcy associated with peripheral neuropathy.[16] In our study also, there is significant lower level of Vitamin B12 and higher level of Hcy associated with peripheral neuropathy in metformin-treated patients.
Liu et al. reported two cases of very long-term treatment (20 and 8 years, respectively) with metformin therapy associated with advanced neurological and hematological side effects due to metformin-induced Vitamin B12 deficiency.[17] In our study, even patients with approximate 2 years of metformin therapy showed evidence of peripheral neuropathy.
Adams et al. showed in their study that 30% of 46 patients undergoing biguanide therapy developed Vitamin B12 malabsorption, which resolved in half on stopping the drug.[18] In our study, 54.28% of patients taking only metformin therapy and 35% of patients taking metformin along with other drugs for controlling their Type 2 DM developed Vitamin B12 deficiency, whether this could be reversible we do not know as our study design is a cross-sectional study.
Reinstatler et al. in their study showed that there was a significant low value of Vitamin B12 in persons using metformin for their Type 2 DM treatment. Shortcoming of this study is that they were not using any functional biomarker for Vitamin B12 such as methylmalonic acid or Hcy.[19] In our study, we also found similar results, but we have used Hcy level as functional biomarker. Our sample size was not based on a predetermined power analysis though our study populations were selected randomly.
Chen et al. in their study measured holotranscobalamin and methylmalonic acid which are more specific and sensitive markers of Vitamin B12 deficiency and showed that there was Vitamin B12 deficiency in metformin-treated Type 2 DM.[20] This is a shortcoming of our study that we could not measure both holotranscobalamin and methylmalonic acid, but we do conclude that even 2 years continuous therapy with metformin can cause Vitamin B12 deficiency.
Wulffelé et al. in their 16-week comprehensive short-term metformin treatment study showed that there was decrease in the Vitamin B12 and folic acid level and increase in the Hcy level even with short-term therapy with metformin.[11] In our study, decreased Vitamin B12 level and increased Hcy level noted in metformin – treated population. But folate level difference was not so much high than the other OHA treated population with metformin treated population. This may be due to that our patients counseled about dietary folate supplementation through green leafy vegetable intake. From our study, no one should interpret that metformin is not a good choice of drug to start with rather it is desirable to estimate an annual Vitamin B12 for monitoring deficiency state of the same.
Pierce et al. and Bell recommended this in their individual studies.[21,22] None of our patients show any hematological evidence of Vitamin B12 and folic acid deficiency, i.e. macrocytic anemia; this may be due to the fact that we enroll only those patients taking metformin for <3 years, and therefore, we recommend a long-term regular follow-up of these patients with complete hemogram.
From our study, another interesting fact we also come across along with the Vitamin B12, folic acid, Hcy level that patients using metformin only for controlling their plasma glucose have their PPBS lower than other two groups of patients. Lund et al. in their study showed that postprandial glucose can also be well controlled with use of metformin.[23]
Although India is the diabetic capital, our study population is very small as we exclude the patients who were suffering for a long (>5 years) duration. Diabetes itself on long duration can cause sensory neuropathy mainly involving small fibers causing tingling–burning sensations.[24,25]
Our study had certain practical limitations. We could not perform nerve biopsy which also suggests annual screening of the pathological gold standard for determination of the presence and types of neuropathy. Therefore, confirmation of the electrophysiological findings could not be done. This was because very few patients gave consent for an invasive procedure like nerve biopsy and lack of expertise needed for biopsy and preparation and interpretation of results. A multicentric study would have made the patient population more heterogeneous and would have increased the power of the study. As the study was undertaken in a tertiary care referral hospital, it was very difficult to find patients without a prescription of metformin, and most of our patients are in advanced stages of Type 2 DM so that we were restricted our study population in small groups. As we did not follow up our patients with an increased Hcy level, we cannot comment about the cardiovascular effect of increased level of Hcy in the long run.
Due to lack of follow-up in this study, we are not able to show that Vitamin B12 supplementation or change over to other antidiabetic can improve the condition as evident in case report by Kumthekar et al.[26] At the end of this discussion, we can conclude by saying that metformin due to its cost-effectiveness and worldwide availability, surely, the first choice of antidiabetic in treatment of Type 2 DM. It induces peripheral neuropathy by initiating Vitamin B12 deficiency through probably blocking its absorption through calcium-mediated channel in the intestine. For proper monitoring of deficiency status, it is desirable that an annual Vitamin B12, folic acid, and Hcy level estimation can predict the after coming event of peripheral neuropathy, which is a preventable and reversible cause.
CONCLUSION
Metformin, oral biguanide, is the first choice of medication to control plasma glucose levels along with lifestyle modification. It is also cost-effective in a country like us. However, initiation of metformin therapy even early and for short duration can induce Vitamin B12, folic acid deficiency and an increase in plasma Hcy level, which can precipitate peripheral neuropathy. From our study, we observed that with metformin, BMI and PPBS were well maintained comparing combination therapy with and without metformin. Thus, it should not be interpreted from our study that it is not so good agent to start with initial management of Type 2 DM rather start with a supplementation of Vitamin B12 along with it. This is also desirable that one should observe Vitamin B12 level annually for monitoring of patients on long-term therapy.
At the end our study, we recommend further studies in:
Follow-up study of the patient with peripheral neuropathy if they can improve with Vitamin B12 supplementation
Further cross-over study to look for any improvement in neuropathy status with change of antidiabetic therapy, to observe dose-dependent changes in NCV study in metformin-treated patients, and to observe dose-dependent changes in Vitamin B12, Hcy level in metformin-treated patients.
Financial support and sponsorship
Nil.
Conflicts of interest
Abstract has been submitted through on-line portal for presentation in the World Diabetes Congress 2016 organized by the International Diabetes Federation.
REFERENCES
- 1.Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ. 2000;321:405–12. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ. 1998;317:703–13. [PMC free article] [PubMed] [Google Scholar]
- 3.Haffner SM. The Scandinavian Simvastatin Survival Study (4S) subgroup analysis of diabetic subjects: Implications for the prevention of coronary heart disease. Diabetes Care. 1997;20:469–71. doi: 10.2337/diacare.20.4.469. [DOI] [PubMed] [Google Scholar]
- 4.Bostom AG, Rosenberg IH, Silbershatz H, Jacques PF, Selhub J, D’Agostino RB, et al. Nonfasting plasma total homocysteine levels and stroke incidence in elderly persons: The Framingham study. Ann Intern Med. 1999;131:352–5. doi: 10.7326/0003-4819-131-5-199909070-00006. [DOI] [PubMed] [Google Scholar]
- 5.Brattström LE, Israelsson B, Jeppsson JO, Hultberg BL. Folic acid – An innocuous means to reduce plasma homocysteine. Scand J Clin Lab Invest. 1988;48:215–21. doi: 10.3109/00365518809167487. [DOI] [PubMed] [Google Scholar]
- 6.Hoogeveen EK, Kostense PJ, Beks PJ, Mackaay AJ, Jakobs C, Bouter LM, et al. Hyperhomocysteinemia is associated with an increased risk of cardiovascular disease, especially in non-insulin-dependent diabetes mellitus: A population-based study. Arterioscler Thromb Vasc Biol. 1998;18:133–8. doi: 10.1161/01.atv.18.1.133. [DOI] [PubMed] [Google Scholar]
- 7.DeFronzo RA, Goodman AM. Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. The Multicenter Metformin Study Group. N Engl J Med. 1995;333:541–9. doi: 10.1056/NEJM199508313330902. [DOI] [PubMed] [Google Scholar]
- 8.Caspary WF, Zavada I, Reimold W, Deuticke U, Emrich D, Willms B. Alteration of bile acid metabolism and Vitamin-B12-absorption in diabetics on biguanides. Diabetologia. 1977;13:187–93. doi: 10.1007/BF01219698. [DOI] [PubMed] [Google Scholar]
- 9.Carlsen SM, Følling I, Grill V, Bjerve KS, Schneede J, Refsum H. Metformin increases total serum homocysteine levels in non-diabetic male patients with coronary heart disease. Scand J Clin Lab Invest. 1997;57:521–7. doi: 10.3109/00365519709084603. [DOI] [PubMed] [Google Scholar]
- 10.10 Aarsand AK, Carlsen SM. Folate administration reduces circulating homocysteine levels in NIDDM patients on long-term metformin treatment. J Intern Med. 1998;244:169–74. doi: 10.1046/j.1365-2796.1998.00361.x. [DOI] [PubMed] [Google Scholar]
- 11.Wulffelé MG, Kooy A, Lehert P, Bets D, Ogterop JC, Borger van der Burg B, et al. Effects of short-term treatment with metformin on serum concentrations of homocysteine, folate and Vitamin B12 in type 2 diabetes mellitus: A randomized, placebo-controlled trial. J Intern Med. 2003;254:455–63. doi: 10.1046/j.1365-2796.2003.01213.x. [DOI] [PubMed] [Google Scholar]
- 12.Tomkin GH, Hadden DR, Weaver JA, Montgomery DA. Vitamin-B12 status of patients on long-term metformin therapy. Br Med J. 1971;2:685–7. doi: 10.1136/bmj.2.5763.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kibirige D, Mwebaze R. Vitamin B12 deficiency among patients with diabetes mellitus: Is routine screening and supplementation justified? J Diabetes Metab Disord. 2013;12:17. doi: 10.1186/2251-6581-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis SN. 11th ed. New York: McGraw-Hill; 2006. Insulin, oral hypoglycaemic agents, and the pharmacology of the endocrine pancreas. The Pharmacological Basis of Therapeutics; pp. 1613–45. [Google Scholar]
- 15.Pflipsen MC, Oh RC, Saguil A, Seehusen DA, Seaquist D, Topolski R. The prevalence of Vitamin B (12) deficiency in patients with type 2 diabetes: A cross-sectional study. J Am Board Fam Med. 2009;22:528–34. doi: 10.3122/jabfm.2009.05.090044. [DOI] [PubMed] [Google Scholar]
- 16.Wile DJ, Toth C. Association of metformin, elevated homocysteine, and methylmalonic acid levels and clinically worsened diabetic peripheral neuropathy. Diabetes Care. 2010;33:156–61. doi: 10.2337/dc09-0606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu KW, Dai LK, Woo J. Metformin related Vitamin B12 deficiency. Oxf J Med Age Ageing. 2006;35:200–2. doi: 10.1093/ageing/afj042. [DOI] [PubMed] [Google Scholar]
- 18.Adams JF, Clark JS, Ireland JT, Kesson CM, Watson WS. Malabsorption of Vitamin B12 and intrinsic factor secretion during biguanide therapy. Diabetologia. 1983;24:16–8. doi: 10.1007/BF00275941. [DOI] [PubMed] [Google Scholar]
- 19.Reinstatler L, Qi YP, Williamson RS, Garn JV, Oakley GP., Jr Association of biochemical B12 deficiency with metformin therapy and Vitamin B12 supplements: The National Health and Nutrition Examination Survey, 1999-2006. Diabetes Care. 2012;35:327–33. doi: 10.2337/dc11-1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen S, Lansdown JA, Moat SJ, Ellis R, Goringe A, Dunstan DF, et al. An observational study of the effect of metformin on B12 status and peripheral neuropathy. Br J Diabetes Vascular Dis. 2012;12:189–93. [Google Scholar]
- 21.Bell DS. Metformin-induced Vitamin B12 deficiency presenting as a peripheral neuropathy. South Med J. 2010;103:265–7. doi: 10.1097/SMJ.0b013e3181ce0e4d. [DOI] [PubMed] [Google Scholar]
- 22.Pierce SA, Chung AH, Black KK. Evaluation of Vitamin B12 monitoring in a veteran population on long-term, high-dose metformin therapy. Ann Pharmacother. 2012;46:1470–6. doi: 10.1345/aph.1R223. [DOI] [PubMed] [Google Scholar]
- 23.Lund SS, Tarnow L, Frandsen M, Smidt UM, Pedersen O, Parving HH, et al. Impact of metformin versus the prandial insulin secretagogue, repaglinide, on fasting and postprandial glucose and lipid responses in non-obese patients with type 2 diabetes. Eur J Endocrinol. 2008;158:35–46. doi: 10.1530/EJE-07-0500. [DOI] [PubMed] [Google Scholar]
- 24.Gale EA, Anderson JV. Kumar and Clark's Clinical Medicine. 7th ed. Ch. 19. Oxford: Elsevier; 2010. Diabetes mellitus and other disorders of metabolism; pp. 1029–63. [Google Scholar]
- 25.Powers AC. Harrison's Principles of Internal Medicine. Part 16. 18th ed. Ch 344. London: The McGraw-Hill Companies; 2012. Diabetes mellitus; pp. 2968–3003. [Google Scholar]
- 26.Kumthekar AA, Gidwani HV, Kumthekar AB. Metformin associated B12 deficiency. J Assoc Physicians India. 2012;60:58–60. [PubMed] [Google Scholar]


