Abstract
This review describes the rationale, biochemical, and clinical data related to the use of inositols in polycystic ovary syndrome (PCOS). It covers studies related to the mechanism of action of myo-inositol and D-chiro-inositol (MDI), with randomized controlled trials conducted in women with PCOS, and utilizes these data to suggest pragmatic indications and methods for using MDI combination in PCOS. Rationally crafted inositol combinations have a potential role to play in maintaining metabolic, endocrine, and reproductive health in women with PCOS.
Keywords: D-chiro-inositol, diabetes, infertility, metabolic syndrome, myo-inositol, ovarian paradox, ovulation, polycystic ovary syndrome
INTRODUCTION
The inositol stereoisomers, myo-inositol (MI) and D-chiro-inositol (DCI), are hexahydroxycyclohexanes, with the same molecular formula as glucose. They are the two most abundant members of a family of nine steroisomeric inositols, and are found widely in nature.[1]
Present in fruits and beans, the inositols are incorporated into cell membranes as phosphatidyl-MI, which is a precursor of inositol triphosphate (InsP3). InsP3 is a second messenger for many hormones including insulin and follicle-stimulating hormone (FSH). Defects in this pathway can lead to impaired insulin signaling and cause insulin resistance.[2] This is the rationale for the suggested use of inositols in the management of insulin resistance syndromes, including polycystic ovary syndrome (PCOS).
THE SECOND MESSENGER
Insulin has multiple effects on metabolism, which can be classified as metabolic and mitogenic. Metabolic effects can be further divided into those related to glucose transport and to glycogen synthesis. These dual metabolic effects sometimes occur in discordance with each other.[1]
This suggests the existence of more than one downstream insulin signaling pathway. While the dominant action occurs though the insulin receptor tyrosine kinase and its primary tyrosine phosphorylated substrates (insulin receptor substrate protein family) second messengers, inositol glycans also mediate many metabolic actions of insulin. The inositol glycans are insulinomimetic, and have an activating/sensitizing effect.
SYSTEMIC PHYSIOLOGY
Two inositols of physiologic interest are MI and DCI. The enzyme epimerase converts MI to DCI, maintaining a physiological ratio, which varies from tissue to tissue. A ratio of 40:1 is thought to be physiological for most tissues.[3] Epimerase is a NAD, NADH-dependent enzyme which is stimulated by insulin to work as per tissue requirement. This stimulus is lost during insulin resistance in the systemic milieu. However, different tissues have varying requirements of these molecules. In the systemic intracellular pool, for example, 99% of all inositols are MI. A high concentration of MI is required to ensure healthy oocyte maturation in the ovary.[4]
The three target organs of insulin, i.e., adipose tissue, liver, and skeletal muscle have a different ratio of the main inositol isomers. In these tissues, a relatively higher proportion of DCI is required to maintain homeostasis. In the setting of epimerase deficiency, less MI can be converted to DCI, a state of relative DCI deficiency occurs, and insulin resistance is promoted.[5] This, in turn, leads to the metabolic complications of hyperinsulinemia.
OVARIAN PHYSIOLOGY
At the same time, the ovary remains sensitive to the effects of insulin, as it is immune to insulin resistance. This is known as the DCI paradox.[4] Hyperinsulinemia alters the FSH to luteinizing hormone (LH) shift, preventing the selection of a dominant follicle. Insulin increases granulose cell sensitivity to LH, thus increasing ovarian androgen production as well. This is mediated by a stimulation of cytochrome P450c17α. Ovarian theca cells in women with PCOS are also more efficient at testosterone production. High-insulin levels impede ovulation, too, probably through the inositol pathway.
Insulin activates mitogenic pathways in ovarian cells, increasing the transcription of steroidogenic acute regulatory protein and causing an increased production of androgens.[1,2] Hyperandrogenemia worsens insulin resistance, accentuating a vicious cycle, by interfering with insulin signaling directly as well as indirectly. Androgens encourage lipolysis, leading to an increased free fatty acid concentration, which reduces insulin sensitivity. Androgens also reduce the proportion of highly oxidative, insulin-sensitive Type I muscle fibers, in comparison with glycolytic, insulin-resistant Type II muscle fibers. This vicious cycle is promoted by obesity, which enhances androgen synthesis in both ovaries and adrenals, and promotes leptin-mediated inflammation.
In the ovary, MI and DCI have specific duties to perform. MI supports FSH signaling, whereas DCI is responsible for insulin-mediated testosterone synthesis. In the normal ovary, these activities proceed in balance, allowing the maintenance of normal hormonal levels and facilitating ovarian function. In the polycystic ovary, systemic insulin resistance (hyperinsulinemia) accentuates epimerase activity, thus creating a higher DCI-to-MI ratio. This promotes hyperandrogenism and reduces the efficiency of MI-mediated FSH signaling.
INOSITOL BALANCE
The relative concentrations of MI and DCI are dynamic, and vary in health and disease. These concentrations are organ-specific. Diabetes is a state of inositol imbalance, with a MI/DCI ratio of 20.4 (Type 2 diabetes) or 13.6 (Type 1 diabetes), as compared to 13.2 (nondiabetic relatives of Type 2 diabetic patients) and 2.5 (controls) in urine. In muscle biopsy specimens, MI concentration is increased in persons with Type 2 diabetes, and increases further after the administration of insulin.[6]
In contrast, DCI is virtually undetectable in Type 2 diabetes muscle biopsy specimens and remains refractory to insulin infusion. In obese persons, there is an increased renal clearance of DCI, and this may account for a relatively higher urinary DCI concentration in obese patients.
In general, as patients progress from normal to impaired glucose tolerance, and then to Type 2 diabetes, urine DCI decreases progressively. This inositol imbalance is related to insulin resistance. Similar deficiency of DCI is found in women with PCOS and pre-eclampsia, both of which are syndromes of the underlying insulin resistance. DCI deficiency may be due to a defect in epimerase-mediated conversion of MI. Such conversion varies from 0.7% in the heart and 2.2% in the liver to 36% in urine, and 60.4% in blood (of nondiabetic rats). Conversion is much lower in diabetic rats as compared to nondiabetic animals.[6,7]
This hypothesis is strengthened by evidence from various studies on ovarian tissue. An in vitro study has demonstrated enhanced epimerase activity in theca cells of PCOS women. Another study reported an MI/DCI ratio of 100:1 in follicular fluid of healthy women, compared to a ratio of 0.2:1 in women with PCOS.[8] This creates uncertainty about the exact ratio of MI/DCI that should be aimed for while managing PCOS.
INOSITOLS: THERAPEUTIC POTENTIAL
It is suggested that the inositols MI and DCI can reduce insulin resistance, improve ovarian function, and reduce androgen levels in women with PCOS. The effect of MI on ovarian function and oocyte quality is independent of its concentration in circulation.[9]
DCI has been shown to be involved in insulin metabolism. Urinary DCI levels are lower in patients with diabetes or impaired glucose tolerance. Serum levels of DCI are reported to be lower in women with PCOS, both at baseline and after administration of glucose loads. DCI treatment has been found to reduce insulin levels, lipids, and blood pressure, in women with PCOS.[10]
CLINICAL EVIDENCE: MYO-INOSITOL
MI has been found to improve the number of good quality oocytes, clinical pregnancies, and delivery rates in overweight women with PCOS. Thus, it modulates the reproductive axis in a beneficial manner. In all these trials, a daily dose of 2 g MI was used over an observation period of 3–6 months. The biochemical, endocrine, and clinical benefits of MI were thought to be due to its insulin-sensitizing action.
A study used MI 2 g and folic acid as a soluble powder, twice daily, continuously, till the end of study (6 months) or a positive pregnancy test was obtained. Of 25 women with PCOS, 22 (88%) experienced a first menstrual cycle after 34.6–5.5 days. Of these 22, 18 continued to have regular menstruation and documented spontaneous ovulation. The length of successive cycles improved to 31.7 ± 3.2 days, and there was a significant fall in serum testosterone and free testosterone. Two more women showed follicular development on ultrasound, but did not exhibit an elevation of progesterone, thus suggesting anovulation. A total of ten biochemical pregnancies occurred during 6 months, of which one ended in a spontaneous abortion and one was a biochemical abortion. No multiple gestations were noted. MI can, thus, be used as a safe means of induction of ovulation in women with PCOS.[11]
In a study of fifty women with PCOS, 2 g MI was found to reduce the risk of ovarian hyper stimulation syndrome with ovulation-induction protocols. Concentrations of LH, prolactin, androstenedione, insulin, and LH/FSH ratio were reduced significantly. Insulin sensitivity improved as well. The duration of ovulation induction and dose requirement of recombinant FSH were significantly lower with MI therapy. MI administration achieved lower oocyte retrieval, but had a greater proportion of large dimension (top quality) oocytes, which translated to a higher pregnancy rate. Biochemical pregnancy occurred in 15, clinical pregnancy in 10, and successful delivery in 8 women treated with MI, as compared to 8, 4, and 3 non-MI-treated participants. All these differences were statistically significant.[9]
An Iraqi study on 95 participants reported that a combination of inositol 500 mg, with choline 500 mg and metformin 850 mg, all administered twice daily for 6 months led to a significant decrease in body mass index (BMI), serum leptin, and serum anti-Mullerian hormone (AMH), as compared to metformin monotherapy and lifestyle management alone. The isomer of inositol was not specified in the study.[12]
Systematic reviews and meta-analysis have collated data on the efficacy of MI in PCOS, and suggest the need for further studies.[13,14] Data also support the use of this molecule in gestational diabetes mellitus (GDM),[15,16] which is also a syndrome characterized by insulin resistance.
CLINICAL EVIDENCE: D-CHIRO-INOSITOL
Various authors have studied the effect of DCI on endocrine, metabolic, and reproductive parameters in PCOS. Administration of 600 mg DCI/day for 6-8 weeks to lean women with PCOS (BMI 20.0–24.4 kg/m2) reduces insulin and free testosterone levels, while decreasing systolic blood pressure, diastolic blood pressure, and serum triglycerides. A higher rate of ovulation is noted with DCI, though the difference is not statistically significant.[17]
In obese PCOS women (BMI >26 kg/m2) also, DCI is found to improve endocrine parameters including serum testosterone, serum androstenedione, and gonadotropin-releasing hormone-induced LH response. It also reduces BMI and improves insulin sensitivity markers in PCOS patients with diabetic relatives, who exhibit a greater response as compared to those with no family history of diabetes.[18]
The effect of DCI extends to menstrual regularity, which improves with its supplementation.[19] This regularity is associated with a decrease in serum AMH and in insulin resistance. Low AMH, high homeostatic model of assessment index, and presence of oligomenorrhea at the first visit are the independent predictors of achieving menstrual regularly with DCI.
This effect may be mediated through a decrease in follicular fluid oxidative stress status. In a study conducted on 68 participants, women with PCOS were pretreated before ovarian stimulation with either DCI 500 mg b.d or metformin 850 mg b.d. or left untreated for 3 months. DCI improved the maturity and quality of oocytes significantly, while reducing oxidative stress (as measured by amino acidic free - SH group labeling). The usage of DCI was not associated with any adverse effect in this study.[20]
These studies complement a relatively old Cochrane review, which assessed the role of insulin-sensitizing agents in the management of PCOS.[21] A similar Cochrane review, focusing on MI, is in progress for GDM.[16]
MYO-INOSITOL/D-CHIRO-INOSITOL COMBINATION
Administration of exogenous DCI may be a means of bypassing defective epimerase activity[6] and achieving the downstream metabolic effects of insulin in DCI-deficient tissues. Epimerase activity is unidirectional, and DCI administration alone will not be able to mimic the effects of MI. Therefore, it is rational to provide a combination of both to ensure optimal insulin sensitivity. At the same time, the positive impact of MI on ovarian physiology may be due to its minimal conversion to DCI.[9] This hypothesis suggests that lower doses of MI may suffice if co-administered with DCI.
In a randomized controlled trial conducted in fifty obese PCOS women, a combination of 550 mg MI and 13.6 mg DCI, in capsule formulation, was found better than 2 g powdered MI, at improving metabolic, endocrine, and ovulation parameters, when administered twice daily over 6 months.[22] Another study showed a significant improvement in insulin sensitivity as well as lipid profile in such patients.[23]
In a large study of 100 women, MI and DCI combination (1.1 g and 27.6 mg, respectively) was found to improve oocyte quality, embryo quality, and pregnancy rates, during in vitro fertilization.[24]
A randomized controlled trial is currently underway in Spain to compare the effect of increasing the proportion of DCI in a MI/DCI combination and to assess the effect on oocyte quality and pregnancy rates in women with PCOS. Along with folic acid, parallel groups are being administered either MI 550 mg + DCI 150 mg (ratio 3.6:1) or MI 550 mg + DCI 13.8 mg (ratio 40:1), twice daily, for 12 weeks, in a double-blind fashion.
SAFETY/TOLERABILITY
Inositol is generally regarded as safe and can be used in pregnancy.[25] Its excretion in breast milk, and safety in lactation, is unknown. Gastrointestinal symptoms can occur, but are rare.
PRAGMATIC PRESCRIPTION
Keeping in view the above physiologic and pharmacological evidence, we suggest pragmatic use of inositol therapy in the prevention and management of PCOS. While the 2013 Endocrine Society guidelines for the management of PCOS do not suggest the use of inositols,[26] there is a definite role for this upcoming therapy.[27] Currently, PCOS treatment is based on lifestyle modification and metformin for metabolic modulation; clomiphene for the induction of ovulation; and oral contraception for menstrual regularity and management of hyperandrogenism. All these modes of treatment have their advantages and limitations. All of them focus on a single aspect of PCOS pathophysiology, and none is able to address all clinical aspects of the syndrome. While metformin does improve insulin sensitivity, thus alleviating the core defect of insulin resistance, it is not approved as a first line drug for the management of cutaneous or hyperandrogenic features.
Combination inositol therapy (MI and DCI) has the potential to improve all symptoms, signs, and laboratory anomalies of PCOS. Both inositols, prescribed together, should be able to improve the required inositol concentrations in both systemic circulation and the ovary, thus addressing the ovary inositol paradox. The correction of systemic insulin resistance by MI will treat the metabolic features of PCOS. Simultaneously, adequate DCI levels will create a healthy intra-ovarian milieu, which will correct hyperandrogenism, improve menstrual regularity, and promote ovulation and fertility.
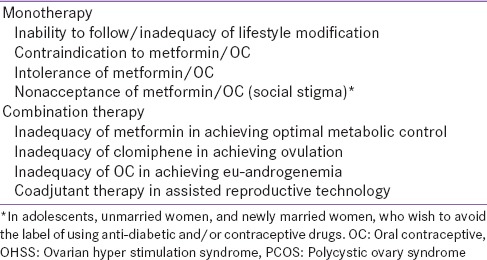
Myo- + D-chiro-inositol (MDI) therapy can be used in PCOS as monotherapy or as a combination with other treatment modalities. Such usage is based on biomedical as well as psychosocial factors [Table 1]. The choice of an MDI preparation and MI/DCI ratio should be based on physiological factors. Current evidence is inadequate to provide a definite answer regarding the optimal MI/DCI ratio. While MI is necessary for metabolic management, DCI is equally important for menstrual, ovulatory, and cutaneous hyperandrogenic resolution. Therefore, the ratio may be less important than the absolute concentrations of both inositols. It is clear, therefore, that a high concentration of DCI is necessary to circumvent epimerase deficiency and ensure adequate levels in the ovary. Most pharmaceutical preparations provide very low amounts of DCI, which are insufficient to achieve adequate levels in the ovary. Hence, formulations with relatively higher levels of DCI are preferred.
Table 1.
Pragmatic use of D-chiro-inositol (myo- + D-chiro-inositol) therapy in polycystic ovary syndrome
SUMMARY
Inositols act as second messengers for insulin, and their deficiency contributes to the various features of PCOS. Correction of MI and DCI deficiency simultaneously, by using MDI therapy, may help in alleviating metabolic, menstrual/ovulatory, and cutaneous hyper androgenic features of PCOS. Thus, MDI is a rational treatment choice, both as monotherapy and in combination, in managing PCOS. Ongoing research will help enhance confidence in the scientific use of these molecules. Till then, pragmatic usage of MDI, in women with contraindications or intolerance to, and inadequacy of, other treatment modalities, should be advised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Larner J, Brautigan DL, Thorner MO. D-chiro-inositol glycans in insulin signaling and insulin resistance. Mol Med. 2010;16:543–52. doi: 10.2119/molmed.2010.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Croze ML, Soulage CO. Potential role and therapeutic interests of myo-inositol in metabolic diseases. Biochimie. 2013;95:1811–27. doi: 10.1016/j.biochi.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 3.Bizzarri M, Carlomagno G. Inositol: History of an effective therapy for polycystic ovary syndrome. Eur Rev Med Pharmacol Sci. 2014;18:1896–903. [PubMed] [Google Scholar]
- 4.Carlomagno G, Unfer V, Roseff S. The D-chiro-inositol paradox in the ovary. Fertil Steril. 2011;95:2515–6. doi: 10.1016/j.fertnstert.2011.05.027. [DOI] [PubMed] [Google Scholar]
- 5.Galazis N, Galazi M, Atiomo W. D-Chiro-inositol and its significance in polycystic ovary syndrome: A systematic review. Gynecol Endocrinol. 2011;27:256–62. doi: 10.3109/09513590.2010.538099. [DOI] [PubMed] [Google Scholar]
- 6.Larner J. D-chiro-inositol–its functional role in insulin action and its deficit in insulin resistance. J Diabetes Res. 2002;3:47–60. doi: 10.1080/15604280212528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sun TH, Heimark DB, Nguygen T, Nadler JL, Larner J. Both myo-inositol to chiro-inositol epimerase activities and chiro-inositol to myo-inositol ratios are decreased in tissues of GK Type 2 diabetic rats compared to Wistar controls. Biochem Biophys Res Commun. 2002;293:1092–8. doi: 10.1016/S0006-291X(02)00313-3. [DOI] [PubMed] [Google Scholar]
- 8.Heimark D, McAllister J, Larner J. Decreased myo-inositol to chiro-inositol (M/C) ratios and increased M/C epimerase activity in PCOS theca cells demonstrate increased insulin sensitivity compared to controls. Endocr J. 2014;61:111–7. doi: 10.1507/endocrj.ej13-0423. [DOI] [PubMed] [Google Scholar]
- 9.Artini PG, Di Berardino OM, Papini F, Genazzani AD, Simi G, Ruggiero M, et al. Endocrine and clinical effects of myo-inositol administration in polycystic ovary syndrome. A randomized study. Gynecol Endocrinol. 2013;29:375–9. doi: 10.3109/09513590.2012.743020. [DOI] [PubMed] [Google Scholar]
- 10.Nestler JE, Jakubowicz DJ, Reamer P, Gunn RD, Allan G. Ovulatory and metabolic effects of D-chiro-inositol in the polycystic ovary syndrome. N Engl J Med. 1999;340:1314–20. doi: 10.1056/NEJM199904293401703. [DOI] [PubMed] [Google Scholar]
- 11.Papaleo E, Unfer V, Baillargeon JP, De Santis L, Fusi F, Brigante C, et al. Myo-inositol in patients with polycystic ovary syndrome: A novel method for ovulation induction. Gynecol Endocrinol. 2007;23:700–3. doi: 10.1080/09513590701672405. [DOI] [PubMed] [Google Scholar]
- 12.Ali LQ, Luaibi NM, Majeed BJ. Used inositol decreased anti-Mullerian hormone (AMH) in polycystic ovary syndrome women. Int J Adv Res. 2015;3:857–69. [Google Scholar]
- 13.Unfer V, Carlomagno G, Dante G, Facchinetti F. Effects of myo-inositol in women with PCOS: A systematic review of randomized controlled trials. Gynecol Endocrinol. 2012;28:509–15. doi: 10.3109/09513590.2011.650660. [DOI] [PubMed] [Google Scholar]
- 14.Galletta M, Grasso S, Vaiarelli A, Roseff SJ. Bye-bye chiro-inositol-myo-inositol: True progress in the treatment of polycystic ovary syndrome and ovulation induction. Eur Rev Med Pharmacol Sci. 2011;15:1212–4. [PubMed] [Google Scholar]
- 15.Zheng X, Liu Z, Zhang Y, Lin Y, Song J, Zheng L, et al. Relationship between myo-inositol supplementary and gestational diabetes mellitus: A meta-analysis. Medicine (Baltimore) 2015;94:e1604. doi: 10.1097/MD.0000000000001604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crawford TJ, Crowther CA, Alsweiler J, Brown J. Antenatal dietary supplementation with myo-inositol in women during pregnancy for preventing gestational diabetes. Cochrane Database of Systematic Reviews. 2015 doi: 10.1002/14651858.CD011507.pub2. DOI: 10.1002/14651858.CD011507.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iuorno MJ, Jakubowicz DJ, Baillargeon JP, Dillon P, Gunn RD, Allan G, et al. Effects of d-chiro-inositol in lean women with the polycystic ovary syndrome. Endocr Pract. 2002;8:417–23. doi: 10.4158/EP.8.6.417. [DOI] [PubMed] [Google Scholar]
- 18.Genazzani AD, Santagni S, Rattighieri E, Chierchia E, Despini G, Marini G, et al. Modulatory role of D-chiro-inositol (DCI) on LH and insulin secretion in obese PCOS patients. Gynecol Endocrinol. 2014;30:438–43. doi: 10.3109/09513590.2014.897321. [DOI] [PubMed] [Google Scholar]
- 19.La Marca A, Grisendi V, Dondi G, Sighinolfi G, Cianci A. The menstrual cycle regularization following D-chiro-inositol treatment in PCOS women: A retrospective study. Gynecol Endocrinol. 2015;31:52–6. doi: 10.3109/09513590.2014.964201. [DOI] [PubMed] [Google Scholar]
- 20.Piomboni P, Focarelli R, Capaldo A, Stendardi A, Cappelli V, Cianci A, et al. Protein modification as oxidative stress marker in follicular fluid from women with polycystic ovary syndrome: The effect of inositol and metformin. J Assist Reprod Genet. 2014;31:1269–76. doi: 10.1007/s10815-014-0307-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang T, Lord JM, Norman RJ, Yasmin E, Balen AH. Insulin-sensitising drugs (metformin, rosiglitazone, pioglitazone, D-chiro-inositol) for women with polycystic ovary syndrome, oligo amenorrhoea and subfertility. Cochrane Database of Systematic Reviews. 2012 doi: 10.1002/14651858.CD003053.pub5. DOI: 10.1002/14651858.CD003053.pub5. [DOI] [PubMed] [Google Scholar]
- 22.Nordio M, Proietti E. The combined therapy with myo-inositol and D-chiro-inositol reduces the risk of metabolic disease in PCOS overweight patients compared to myo-inositol supplementation alone. Eur Rev Med Pharmacol Sci. 2012;16:575–81. [PubMed] [Google Scholar]
- 23.Minozzi M, Nordio M, Pajalich R. The combined therapy myo-inositol plus D-Chiro-inositol, in a physiological ratio, reduces the cardiovascular risk by improving the lipid profile in PCOS patients. Age (Years) 2013;26:5–1. [PubMed] [Google Scholar]
- 24.Colazingari S, Treglia M, Najjar R, Bevilacqua A. The combined therapy myo-inositol plus D-chiro-inositol, rather than D-chiro-inositol, is able to improve IVF outcomes: Results from a randomized controlled trial. Arch Gynecol Obstet. 2013;288:1405–11. doi: 10.1007/s00404-013-2855-3. [DOI] [PubMed] [Google Scholar]
- 25.Carlomagno G, Unfer V. Inositol safety: Clinical evidences. Eur Rev Med Pharmacol Sci. 2011;15:931–6. [PubMed] [Google Scholar]
- 26.Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, Pasquali R, et al. Diagnosis and treatment of polycystic ovary syndrome: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013;98:4565–92. doi: 10.1210/jc.2013-2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Facchinetti F, Bizzarri M, Benvenga S, D’Anna R, Lanzone A, Soulage C, et al. Results from the International Consensus Conference on myo-inositol and d-chiro-inositol in obstetrics and gynecology: The link between metabolic syndrome and PCOS. Eur J Obstet Gynecol Reprod Biol. 2015;195:72–6. doi: 10.1016/j.ejogrb.2015.09.024. [DOI] [PubMed] [Google Scholar]


