Sir,
Read with interest the article, prevalence of colonic polyp and its predictors in patients with acromegaly.[1] Pachydermoperiostosis (PDP) or primary hypertrophic osteoarthropathy is a rare disorder that is characterized by digital clubbing and subperiosteal new bone formation associated with pain, polyarthiritis, cutis verticis gyrata, seborrhea, and hyperhidrosis. It is important to the endocrinologist as it needs to be distinguished from acromegaly. Considering its rarity, here, we describe a man who was referred to our center for acromegaly but had PDP.
A 27-year-old male presented with enlargement of fingers and toes for the past 15 years. He was referred to our institute with a provisional diagnosis of acromegaly. He complained of pain over ankles and knees and hyperhidrosis for the past 2 years. He had been evaluated outside for acromegaly. His post-glucose growth hormone suppression test was suppressible. His magnetic resonance imaging sella done outside was normal. He denied any history of the abnormal increase in height. He did not have any respiratory, cardiovascular, or gastrointestinal symptoms. There was no family history of similar illness.
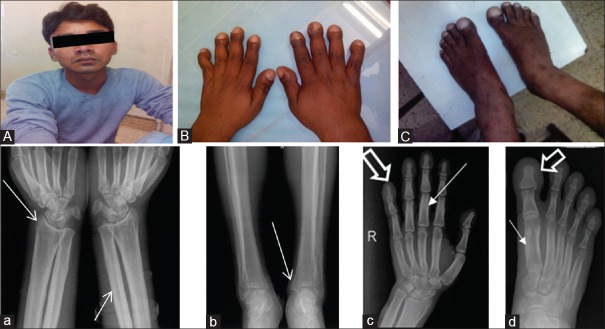
On examination, there was bulbous swelling of the tips of fingers and toes [Figure 1A-C]. There was no frontal bossing or prognathism. His hemogram and biochemistry including C-reactive protein and insulin-like growth factor-1 were within normal range. Radiological examination revealed extensive and symmetrical periosteal reaction in the bones of bilateral forearms and legs, small bones of hands, and feet feet [Figure a-d, thin arrow]. The periosteal reaction involved diaphysis, metaphysis as well as epiphysis of long bones. There was bulbous appearance [Figure c and d, outlined arrow] of tips of fingers and toes due to increased soft tissue in that region. Thus, he had clubbing and periostitis with the absence of pachyderma, features suggestive of an incomplete form of PDP. His pain subsided with indomethacin.
Figure 1.
(A-C) Clinical photographs of face, both hands and feet showing normal facial skin, bulbous enlargement of fingers and toes as well as enlargement of both ankles. Multiple skeletal radiographs (a-d) show extensive and symmetrical periosteal reaction (thin arrow) seen in the bones of bilateral forearms and legs, small bones of hands and feet. The periosteal reaction involved diaphysis, metaphysis as well as epiphysis of long bones. There was bulbous appearance (outlined arrow) of tips of fingers and toes due to increased soft tissue in that region
There are three clinical variants of PDP described: (i) Complete form, with pachydermia, clubbing and periostosis, (ii) incomplete form, with isolated periostosis and limited skin changes and (iii) fruste form, with predominant pachydermia and minimal periostosis.[2]
The disease starts at puberty, progresses variably to another 5–20 years and then remains stable. The disease course may be complicated by arthralgia, arthritis, and hemarthroses. A rare, but dreaded complication is myelofibrosis. Radiologically, there is periosteal new bone formation, the proliferation of soft tissues around tips of fingers and toes, acro-osteolysis and calcifications of ligaments and interosseous membranes.
The clinical diagnosis is considered after exclusion of different causes of secondary hypertrophic osteoarthropathy as well as acromegaly and confirmed with the help of a typical radiological appearance.
Although mostly sporadic, both autosomal dominant and recessive forms are described.[3] X-linked transmission or role of testosterone is also to be considered in view of skewed sex ratio (male:female = 9:1). Two prostaglandin pathway genes, namely, HPGD and SLCO2A1 are associated with this clinical condition.
Pathogenetic mechanisms[4] proposed are: (i) Proliferation of dermal and bone marrow fibroblast, (ii) diffuse dermal endothelial hyperplasia, (iii) partial occlusion of the vascular lumen, (iv) pericapillary lymphohistiocytic infiltration, (v) thickening of dermal collagens, (vi) elevated dermal sulfated glycosaminoglycans and proteoglycans, (vii) increased plasma levels of osteocalcin, endothelin-1, beta-thromboglobulin, platelet-derived growth factor, von Willebrand factor, vascular endothelial growth factor, (viii) high concentration of nuclear steroid receptors and low concentration of epidermal growth factor receptors.
These patients classically respond to nonsteroidal anti-inflammatory drugs. Intravenous zolendronic acid[5] is also used for symptomatic pain relief. On long term, they live a normal lifespan with not more than moderate disability.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Agarwal P, Rai P, Jain M, Mishra S, Singh U, Gupta SK. Prevalence of colonic polyp and its predictors in patients with acromegaly. Indian J Endocr Metab. 2016;20:437–42. doi: 10.4103/2230-8210.183455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Auger M, Stavrianeas N. Pachydermoperiostosis. Orphanet Encyclopedia. 2004. [Last accessed on 2016 May 20]. Avaialble from: http://www.orpha.net/data/patho/GB/uk-pachydermoperiostosis.pdf .
- 3.Castori M, Sinibaldi L, Mingarelli R, Lachman RS, Rimoin DL, Dallapiccola B. Pachydermoperiostosis: An update. Clin Genet. 2005;68:477–86. doi: 10.1111/j.1399-0004.2005.00533.x. [DOI] [PubMed] [Google Scholar]
- 4.Matucci-Cerinic M, Cinti S, Morroni M, Lotti T, Nuzzaci G, Lucente E, et al. Pachydermoperiostosis (primary hypertrophic osteoarthropathy): Report of a case with evidence of endothelial and connective tissue involvement. Clin Exp Rheumatol. 1989;48:240–6. doi: 10.1136/ard.48.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chakraborty PP, Bhattacharjee R, Mukhopadhyay S, Chowdhury S. Pseudoacromegaly in pachydermoperiostosis. BMJ Case Rep 2016. 2016 doi: 10.1136/bcr-2016-214624. pii: Bcr2016214624. [DOI] [PMC free article] [PubMed] [Google Scholar]