Abstract
Shoulder arthroscopy is an orthopaedic procedure that has grown significantly in popularity over the last 40 years. The 2 principle patient positions during shoulder arthroscopy include the beach chair position and lateral decubitus position. This Technical Note details the operating room setup for shoulder arthroscopy in the beach chair position. Proper positioning for this procedure will minimize potential complications and facilitate ease of surgical intervention.
Shoulder arthroscopy is a common procedure performed for diagnostic and therapeutic purposes.1, 2, 3 Indications for shoulder arthroscopy are expanding, with increasing ability of the orthopaedic surgeon to identify lesions and perform more complex arthroscopic procedures.4, 5, 6 This article and Video 1 review the setup of the operating room, sterile preparation, and draping for shoulder arthroscopy in the beach chair position. Proper positioning for this procedure will minimize complications and facilitate surgical intervention during the procedure.
Surgical Technique
The patient is brought to the operating room after preoperative safety measures, which includes marking of the operative extremity by the surgeon (Table 1). Once in the operating room, the patient is identified and transferred to the operating table with timeout procedures performed to ensure patient safety. We prefer to use general anesthesia with a preprocedural interscalene nerve block for postprocedural pain control after shoulder arthroscopy. Shoulder arthroscopy can be performed in the lateral decubitus or beach chair position; however, this technical note and Video 1 will focus on the positioning technique for the beach chair position.
Table 1.
Potential Pearls and Pitfalls for Beach Chair Positioning for Shoulder Arthroscopy
| Pearls | Pitfalls |
|---|---|
|
|
Induction of Anesthesia
The choice of shoulder arthroscopy position is surgeon dependent. The senior author (M.T.F.) prefers labral work in the lateral decubitus position and all other procedures in the beach chair position. Anesthesia concerns are increased with the patient in the upright position because the sympathetic nervous system is responsible for increasing vascular resistance and mean arterial pressure (MAP), while decreasing cardiac output to maintain cerebral perfusion, which under general anesthesia has more difficulty responding or compensating.7 Thus, monitoring of the MAP, with a target between 80 and 100 mm Hg, is of the utmost importance. The anesthesia team will also maintain normothermia throughout the case with the infusion of warmed intravenous saline solution and the use of an inflatable warming blanket (3M Bair Hugger Intraoperative Blankets, St. Paul, MN) just below the nipple line to cover the lower extremities without impediment to the procedure.8
Operating Room Setup
The operating room setup is shown in Figure 1. The arthroscopic monitor, fluid management system, and operative devices, including the radiofrequency and arthroscopic shaver stations, are positioned on the contralateral side of the operative shoulder. The surgeon, surgical assistant, and surgical technologist are positioned ipsilateral to the operative shoulder. Once prepping and draping is complete, the primary instrument table and Mayo stand are moved to the operative side by the surgical technologist. Sterile field positioning should not compromise pathways for the circulating nurse to reach the arthroscopic pump, monitor, and additional equipment/supplies.
Fig 1.
Operative room setup for a left shoulder arthroscopy in the beach chair position. The locations of instruments and equipment in the operating theater are shown. The arthroscopic monitor, fluid management system, and operative devices are positioned contralateral (right) to the operative shoulder (left). The surgeon, surgical assistant, and surgical technologist are positioned on the operative side (left), with the surgeon positioned closest to the head of the bed, and the surgical technologist closest to the foot of the bed. A back table with surgical instruments is immediately adjacent to the surgical technician for ease of access. Finally, the anesthesiologist is at the head of the bed.
Patient Positioning
The patient is placed supine on the operating table and general endotracheal anesthesia is induced. The endotracheal tube should be taped to the contralateral side of the mouth to assure easy airway access during the procedure if needed. After induction, protective foam goggles (Bat Mask, Sharn, Tampa, FL) are placed over the patient's eyes for ocular protection during the procedure. Additional intravenous access (on the contralateral arm), monitors, as well as other protective anesthesia measures are placed at this time. A Foley catheter is inserted if the procedure length may exceed 3 hours. The catheter is secured to the patient's abdomen and handed off the head of the operative table to the anesthesia staff for urine output monitoring.
Sequential compression devices are placed on the patient's lower extremities for deep venous thrombosis prophylaxis. Protective padding is then placed under the heels to prevent compression of bony prominences. The patient is then moved on the operating table to align the greater trochanter with the break in the operating table to allow hip flexion preventing sciatic nerve compression. The head, neck, and torso are supported in neutral position by straps to prevent any cervical stress during the procedure. The patient's head is carefully placed in the head positioner (Universal Head Positioner, Arthrex, Naples, FL) with the airway properly secured. Care must be taken to assure that the head positioner is locked and that anesthesia is comfortable with the positioning. The padded head straps (Universal Head Positioner, disposable, Arthrex) are applied across the patient's forehead and under the chin to assure stability. A locking mechanism avoids compression of the head holder within the occiput region.
The operating table is then adjusted using the motorized controls to achieve 30° to 40° of hip flexion to prevent the patient from sliding down the operative table and the knees should be flexed 30° to relieve sciatic nerve tension and decrease popliteal fossa pressure during the procedure. The patient is moved into the upright beach chair position in conjunction with the anesthesia staff to ensure that the patient does not become hypotensive during this positioning maneuver. We recommend cycling the blood pressure before raising the head to have accurate and current blood pressure data.
A seatbelt is placed over the patient's legs with foam padding between the belt and legs and an additional strap is placed across the abdomen with foam padding between the patient and the strap. The ipsilateral back third of the table is removed exposing the posterior aspect of the shoulder and a padded seatbelt is passed from a vertical bar on the contralateral side of the table along the patient's operative side and is secured with Velcro. Attention is then turned to the contralateral arm, which is placed in a padded arm holder (LPS Arm Support, Arthrex) to ensure that the wrist is in a neutral position and avoids compression of the ulnar nerve. The operative table is then tilted (“airplaned”) toward the nonoperative side to allow easier access to the shoulder. These steps convert a standard operating table into a “beach chair” table. The SPIDER2 Limb Positioner (Smith & Nephew, Memphis, TN), which allows for 3-dimensional intraoperative positioning of the shoulder, is then fixed to the ipsilateral side of the operating table. The positioner should allow for adequate external rotation of the operative shoulder.
Sterile Preparation and Draping
Once the patient is properly positioned (Fig 2), a final preparation timeout is performed to confirm the operative side for patient safety. Next, sterile preparation and draping can proceed. The operative extremity is prescrubbed with chlorhexidine solution. The forearm of the operative extremity is held while the surgeon cleans the skin with sterile 3M ChloraPrep (CareFusion, San Diego, CA) from the axilla to the hand and nipple to the medial border of the scapula. The surgeon uses a sterile stockinette (3M Health Care, St. Paul, MN) to cover the hand. A sterile plastic blue U-Drape (1015 U-drape, 3M Health Care) is placed across the neck and down the chest and back to isolate the sterile field, followed by a second plastic blue U-Drape (1015 U-drape, 3M Health Care) across the axilla and up the chest and back. A sterile drape with an arthroscopic fluid collection pocket and associated drain is then used (3M Health Care). This drape will isolate anesthesia from the sterile field. A sterile connection is then placed on the base of the SPIDER2 Limb Positioner arm. The operative extremity is placed in a padded arm holder that connects directly to the SPIDER2 Limb Positioner allowing for the extremity to be fixed by a series of padded straps (Smith & Nephew), while maintaining the ability to have full range of motion. The forearm and hand of the operative side is wrapped in a 3M Coban Wrap (3M Health Care). The surgeon will then use a pen on the skin for landmarks of the acromion, clavicle, and coracoid to determine the positions of the portals. Once these landmarks have been identified, one sheet of Ioband (3M Health Care) is cut into quarters, and fixed to the edges of the operative area to prevent the drapes from pulling away from their position. At the conclusion of patient positioning (Fig 3), the surgical team should change gloves and conduct a final preincision timeout.
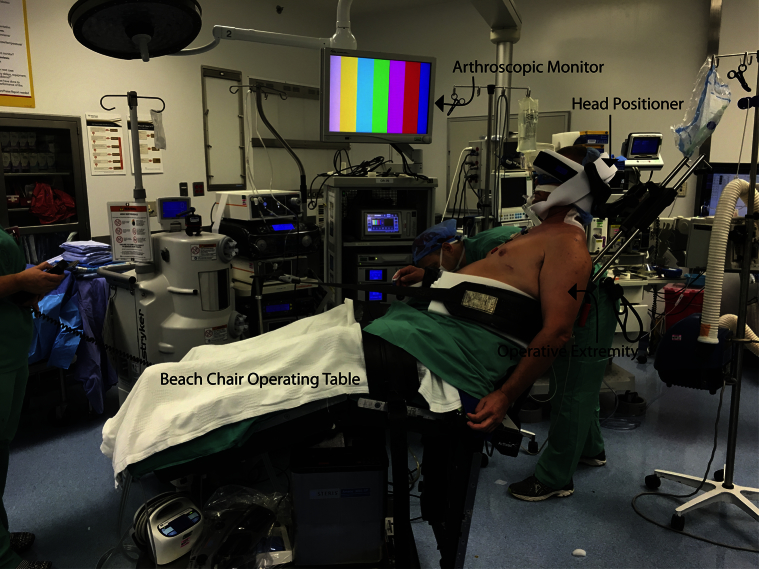
Fig 2.
Patient positioned in the beach chair position for a left shoulder arthroscopy before preparation and draping. Take note of the adjusted operating table to 30°-40° of hip flexion to prevent the patient from sliding down the operative table and the 30° of knee flexion to relieve sciatic nerve tension and decrease popliteal fossa pressure during the procedure.
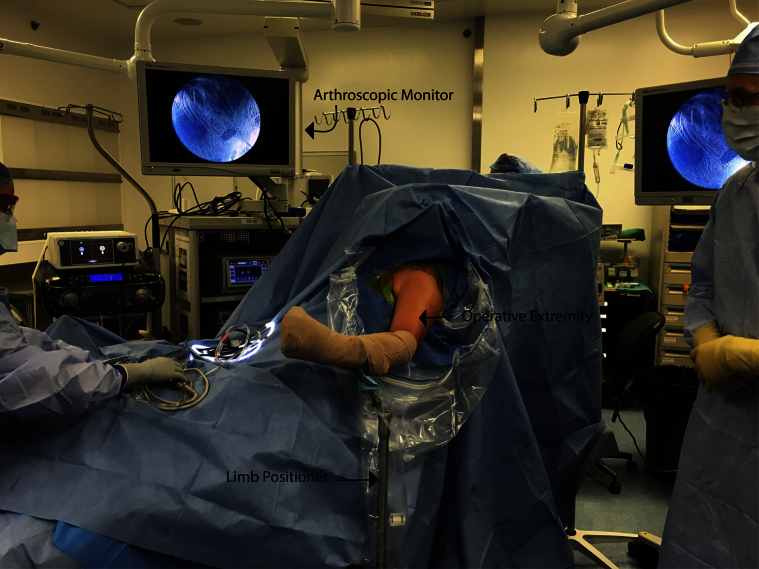
Fig 3.
Patient positioned in the beach chair position and prepared and draped for a left shoulder arthroscopy. The operative extremity (left) is held by the limb positioner, which will allow complete stability during the procedure with the option of full range of motion.
Discussion
Arthroscopic shoulder surgery is highly effective at treating shoulder pathology and continues to grow in popularity because of its success.7, 9, 10 Shoulder arthroscopy evolved from a solely diagnostic procedure to the current ability to perform complex repairs and reconstructions. Arthroscopy offers several advantages versus open procedures including decreased morbidity, length of hospital stay, and postoperative pain, in addition to improved cosmesis.11, 12, 13 Furthermore, continued progression of technology has allowed the treatment of more complex shoulder pathology.3
The 2 positions that may be used when performing shoulder arthroscopy are the beach chair and lateral decubitus positions. The position chosen is chiefly dependent on surgeon preference and neither has been shown to be superior to the other.14 The scope of this article focuses on beach chair positioning and the critical steps taken to minimize perioperative complications.
Cerebral hypoperfusion is a recognized and catastrophic complication of the beach chair position.15, 16, 17, 18, 19, 20 Koh et al.21 showed that using an interscalene nerve block with sedation instead of general anesthesia will maintain a higher MAP and decrease the number of cerebral desaturation events, thus minimizing this risk. However, Pohl and Cullen15 reported that hyperextension and rotation or tilt of the head can decrease vertebral artery flow, resulting in infarcts in the distribution of the posterior cerebral artery. Furthermore, Park and Kim22 reported a case series of neuropraxia thought to have been caused by malposition of the head and neck in the beach chair position resulting in excess pressure on superficial nerves. Thus, the surgeon must be vigilant in assuring proper head alignment during patient positioning as well as proper padding of bony prominences. Finally, during sterile preparation of the surgical field, care should be taken to isolate the surgical field while maintaining satisfactory area to place the relevant portals.
The advantages of the beach chair position have been outlined in the literature as having a lower incidence of neuropathies, decreased risk of neurovascular complications during portal placement, decreased surgical time, easier conversion to an open procedure, and better visualization of the joint.7, 14, 23, 24 Accordingly, the beach chair position was reportedly used in 64% of shoulder arthroscopies performed by members of the American Shoulder and Elbow Surgeons Society.25 However, supporters of the lateral decubitus position point to the increased equipment costs associated with the beach chair position, potential mechanical blocks for posterior and superior portal placement, obstructed camera view due to fluid causing fog on the camera or cautery bubbles in the subacromial space, and an increased risk of air embolus and hypotension.7, 14
In conclusion, obtaining optimal postoperative outcomes requires optimal preoperative patient positioning. To achieve this we rely on a safe, reproducible technique ideal for surgical intervention. Proper patient positioning requires the assistance and expertise of the entire operating room team. If the surgical team is well versed in the positioning and sterile preparation for shoulder arthroscopy in the beach chair position, this will aid in the efficiency of the operative procedure and minimize risk to the patient.
Footnotes
The authors report the following potential conflict of interest or source of funding: S.M. and C.J.T. receive funding from Wake Forest Innovations Spark Award Research Grant. S.M. and C.J.T. were also awarded with US patent 08926626. M.T.F. receives support from Smith & Nephew, DJO, and DePuy Mitek.
Supplementary Data
Beach chair patient positioning for a left shoulder arthroscopy: operating room setup and positioning of the arms, head, and sterile preparation and draping. The video outlines the key steps when preparing a patient for a left shoulder arthroscopy in the beach chair position and how to minimize complications, while maximizing efficiency.
References
- 1.Correa M.C., Goncalves L.B., Andrade R.P., Carvalho L.H., Jr. Beach chair position with instrumental distraction for arthroscopic and open shoulder surgeries. J Shoulder Elbow Surg. 2008;17:226–230. doi: 10.1016/j.jse.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 2.Bhaskar S.B., Manjuladevi M. Shoulder arthroscopy and complications: Can we afford to relax? Indian J Anaesth. 2015;59:335–337. doi: 10.4103/0019-5049.158729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farmer K.W., Wright T.W. Shoulder arthroscopy: The basics. J Hand Surg Am. 2015;40:817–821. doi: 10.1016/j.jhsa.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 4.Iqbal S., Jacobs U., Akhtar A., Macfarlane R.J., Waseem M. A history of shoulder surgery. Open Orthop J. 2013;7:305–309. doi: 10.2174/1874325001307010305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Snyder S.J., Karzel R.P., Del Pizzo W., Ferkel R.D., Friedman M.J. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274–279. doi: 10.1016/0749-8063(90)90056-j. [DOI] [PubMed] [Google Scholar]
- 6.Carr A.J., Price A.J., Glyn-Jones S., Rees J.L. Advances in arthroscopy-indications and therapeutic applications. Nat Rev Rheumatol. 2015;11:77–85. doi: 10.1038/nrrheum.2014.174. [DOI] [PubMed] [Google Scholar]
- 7.Paxton E.S., Backus J., Keener J., Brophy R.H. Shoulder arthroscopy: Basic principles of positioning, anesthesia, and portal anatomy. J Am Acad Orthop Surg. 2013;21:332–342. doi: 10.5435/JAAOS-21-06-332. [DOI] [PubMed] [Google Scholar]
- 8.Oh J.H., Kim J.Y., Chung S.W. Warmed irrigation fluid does not decrease perioperative hypothermia during arthroscopic shoulder surgery. Arthroscopy. 2014;30:159–164. doi: 10.1016/j.arthro.2013.11.017. [DOI] [PubMed] [Google Scholar]
- 9.Ogilvie-Harris D.J., Wiley A.M. Arthroscopic surgery of the shoulder. A general appraisal. J Bone Joint Surg Br. 1986;68:201–207. doi: 10.1302/0301-620X.68B2.3958003. [DOI] [PubMed] [Google Scholar]
- 10.Owens B.D., Harrast J.J., Hurwitz S.R., Thompson T.L., Wolf J.M. Surgical trends in Bankart repair: An analysis of data from the American Board of Orthopaedic Surgery certification examination. Am J Sports Med. 2011;39:1865–1869. doi: 10.1177/0363546511406869. [DOI] [PubMed] [Google Scholar]
- 11.Harris J.D., Gupta A.K., Mall N.A. Long-term outcomes after Bankart shoulder stabilization. Arthroscopy. 2013;29:920–933. doi: 10.1016/j.arthro.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 12.Godin J., Sekiya J.K. Systematic review of arthroscopic versus open repair for recurrent anterior shoulder dislocations. Sports Health. 2011;3:396–404. doi: 10.1177/1941738111409175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang A.L., Montgomery S.R., Ngo S.S., Hame S.L., Wang J.C., Gamradt S.C. Arthroscopic versus open shoulder stabilization: Current practice patterns in the United States. Arthroscopy. 2014;30:436–443. doi: 10.1016/j.arthro.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 14.Peruto C.M., Ciccotti M.G., Cohen S.B. Shoulder arthroscopy positioning: Lateral decubitus versus beach chair. Arthroscopy. 2009;25:891–896. doi: 10.1016/j.arthro.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Pohl A., Cullen D.J. Cerebral ischemia during shoulder surgery in the upright position: A case series. J Clin Anesth. 2005;17:463–469. doi: 10.1016/j.jclinane.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 16.Papadonikolakis A., Wiesler E.R., Olympio M.A., Poehling G.G. Avoiding catastrophic complications of stroke and death related to shoulder surgery in the sitting position. Arthroscopy. 2008;24:481–482. doi: 10.1016/j.arthro.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Li X., Eichinger J.K., Hartshorn T., Zhou H., Matzkin E.G., Warner J.P. A comparison of the lateral decubitus and beach-chair positions for shoulder surgery: Advantages and complications. J Am Acad Orthop Surg. 2015;23:18–28. doi: 10.5435/JAAOS-23-01-18. [DOI] [PubMed] [Google Scholar]
- 18.Pant S., Bokor D.J., Low A.K. Cerebral oxygenation using near-infrared spectroscopy in the beach-chair position during shoulder arthroscopy under general anesthesia. Arthroscopy. 2014;30:1520–1527. doi: 10.1016/j.arthro.2014.05.042. [DOI] [PubMed] [Google Scholar]
- 19.Tange K., Kinoshita H., Minonishi T. Cerebral oxygenation in the beach chair position before and during general anesthesia. Minerva Anestesiol. 2010;76:485–490. [PubMed] [Google Scholar]
- 20.Dippmann C., Winge S., Nielsen H.B. Severe cerebral desaturation during shoulder arthroscopy in the beach-chair position. Arthroscopy. 2010;26:S148–150. doi: 10.1016/j.arthro.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 21.Koh J.L., Levin S.D., Chehab E.L., Murphy G.S. Neer Award 2012: Cerebral oxygenation in the beach chair position: A prospective study on the effect of general anesthesia compared with regional anesthesia and sedation. J Shoulder Elbow Surg. 2013;22:1325–1331. doi: 10.1016/j.jse.2013.01.035. [DOI] [PubMed] [Google Scholar]
- 22.Park T.S., Kim Y.S. Neuropraxia of the cutaneous nerve of the cervical plexus after shoulder arthroscopy. Arthroscopy. 2005;21:631. doi: 10.1016/j.arthro.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 23.Gelber P.E., Reina F., Caceres E., Monllau J.C. A comparison of risk between the lateral decubitus and the beach-chair position when establishing an anteroinferior shoulder portal: A cadaveric study. Arthroscopy. 2007;23:522–528. doi: 10.1016/j.arthro.2006.12.034. [DOI] [PubMed] [Google Scholar]
- 24.Kim K.C., Rhee K.J., Shin H.D. Beach-chair lateral traction position using a lateral decubitus distracter in shoulder arthroscopy. Orthopedics. 2007;30:1001–1003. doi: 10.3928/01477447-20071201-01. [DOI] [PubMed] [Google Scholar]
- 25.Friedman D.J., Parnes N.Z., Zimmer Z., Higgins L.D., Warner J.J. Prevalence of cerebrovascular events during shoulder surgery and association with patient position. Orthopedics. 2009;32:256. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Beach chair patient positioning for a left shoulder arthroscopy: operating room setup and positioning of the arms, head, and sterile preparation and draping. The video outlines the key steps when preparing a patient for a left shoulder arthroscopy in the beach chair position and how to minimize complications, while maximizing efficiency.