Abstract
Introduction
The primary objective of this project was to examine the effectiveness of an internet-based smoking cessation intervention combined with a tele-health medication clinic for nicotine replacement therapy (NRT) compared to referral to clinic-based smoking cessation care.
Methods
A total of 413 patients were proactively recruited from the Durham VA Medical Center and followed for 12 months. Patients were randomized to receive either a referral to VA specialty smoking cessation care (control) or to the internet intervention and tele-health medication clinic. Primary outcomes included (1) intervention reach, (2) self-reported 7-day point prevalence abstinence rates at 3 months and 12 months, and 3) relative cost-effectiveness.
Results
Reach of the internet intervention and use of smoking cessation aids were significantly greater compared to the control. At 3 months-post randomization, however, there were no significant differences in quit rates: 17% (95% CI: 12%–23%) in the internet-based intervention compared to 12% (95% CI: 8%–17%) in the control arm. Similarly, there were no differences in quit rates at 12 months (13% vs. 16%). While costs associated with the internet arm were higher due to increased penetration and intensity of NRT use, there were no statistically significant differences in the relative cost effectiveness (e.g., life years gained, quality adjusted life years) between the two arms.
Conclusions
Current results suggest that using an electronic medical record to identify smokers and proactively offering smoking cessation services that are consistent with US Public Health Guidelines can significantly reduce smoking in veterans. Novel interventions that increase the reach of intensive treatment are needed to maximize quit rates in this population.
1.0 INTRODUCTION
An estimated 44.5 million adults smoke cigarettes, resulting in death or disability for half (Mokdad, Marks, Stroup, & Gerberding, 2004). More deaths are caused each year by tobacco use than by all deaths from AIDS, illegal drugs, alcohol use, motor vehicle accidents, suicides, and murders combined (Centers for Disease Control and Prevention, 2002). Coupled with this enormous health toll is the significant economic burden of tobacco use, with more than $96 billion per year in medical expenditures alone (Centers for Disease Control and Prevention, 2008). While great strides have been made to reduce smoking in military populations, smoking rates in active duty military populations remain as high as 32% (Barlas, Higgins, Pflieger, & Diecker, 2013; Bray et al., 2005). Unfortunately, smoking in the military is associated with a lifelong pattern of increased cigarette consumption (Feigelman, 1994; McKinney, McIntire, Carmody, & Joseph, 1997). As many as 50% of veterans returning from service in Iraq and Afghanistan (i.e., Operation Enduring Freedom, Operation Iraqi Freedom, Operation New Dawn; OEF/OIF) using Veterans Health Administration (VA) healthcare have a lifetime history of smoking and 24% currently smoke (Acheson, Straits-Troster, Calhoun, Beckham, & Hamlett-Berry, 2011). Rates are higher among veterans and the general public with mental health problems such as posttraumatic stress disorder (PTSD) (Kirby et al., 2008).
Specialty clinic-based tobacco cessation programs have been shown to be efficacious in reducing smoking (Fiore, 2000; Shipley, Steffen, & Riley, 1999) but such programs are infrequently attended (Sherman, Yano, Lanto, Simon, & Rubenstein, 2005; Thompson et al., 1988; Yano et al., 2008). This limits the impact on prevalence, disease impact, and economic costs of smoking (Sherman et al., 2006). Attendance to specialty-based smoking cessation clinics is as low as 6%–14% (Sherman et al., 2005; Thompson et al., 1988; Yano et al., 2008). While the VA removed co-pays for smoking cessation care visits in 2005, other barriers (e.g., travel, scheduling conflicts) continue to limit access.
There is significant disagreement in the tobacco control field with regard to how smoking cessation care should be structured (Sherman et al., 2006). Many experts emphasize treatment in specialty clinics, as intensive programs have been shown to be most efficacious (Fiore et al., 2000). Others have highlighted the need of adopting a public health approach to smoking cessation (Sherman & Farmer, 2004). From a public health perspective, impact has been defined as Reach (i.e., number of people who access/receive an intervention) X Efficacy (effect size of an intervention) (Abrams et al., 1996). Current approaches reflect a tradeoff between low reach/high efficacy (e.g., clinic-based care) and high reach/low efficacy (e.g., physician advice).
Internet interventions could be used to improve reach of smoking cessation interventions by avoiding barriers that limit participation in specialty care. Smoking cessation treatment may be particularly well suited to delivery via the internet through on-line chat groups, contacts with experts, and individually-tailored information and feedback regarding behavioral skills. Treatment can be provided in “real time” and at the convenience of the user for as long as he/she needs it, which may help prevent relapse (Bock et al., 2004). The anonymity of online interactions can facilitate social support (Kramish et al., 2001). On the other hand, internet interventions are generally less intensive than in person interventions, which could result in lower efficacy.
Although there are relatively few studies that have evaluated internet-based cessation interventions, initial evidence examining web-based interventions have documented cessation rates ranging from 13%–15% (Graham, Cobb, Raymond, Sill, & Young, 2007). Internet interventions might be particularly effective for younger veterans who are more likely to have home-based internet access (Schneiderman, Lincoln, Curbow, & Kang, 2004). No studies have examined the effectiveness of internet based smoking cessation interventions in a veteran population. The purpose of the current study was to compare the impact (i.e., intervention reach and efficacy) and cost-effectiveness of an internet-based smoking cessation intervention paired with a tele-medicine clinic for nicotine replacement therapy (NRT) to an assisted referral to specialty smoking cessation clinic-based care for veteran smokers.
2. METHOD
2.1 Participants
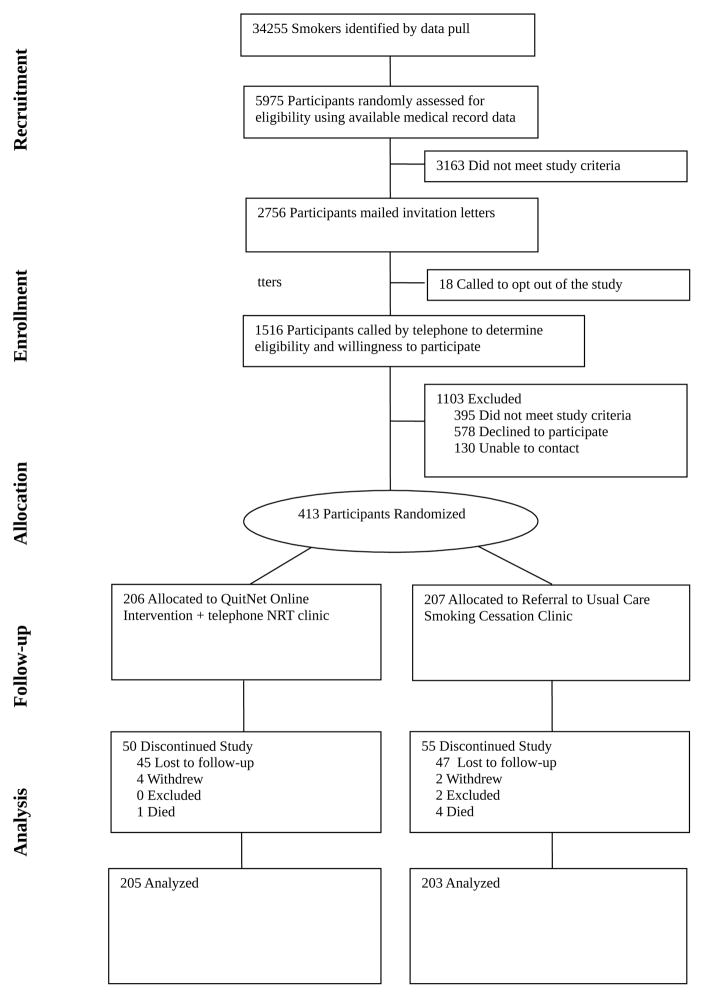
Patients (N=413) were recruited from the Durham VA Medical Center and followed for at least 12 months. Eligible patients included current smokers (any tobacco use in the past month including cigarettes and cigars) who a) were enrolled at the VA for primary care and b) were willing to make a quit attempt in the next 30 days. Exclusion criteria included an active diagnosis of psychosis in the medical record, no regular access to a telephone, refusal to provide informed consent, and severely impaired hearing or speech that would make him/her unable to respond to telephone interviews. A CONSORT diagram for the trial is shown in Figure 1.
Figure 1.
Consort Diagram
2.2 Procedures
Veterans with tobacco use were identified from electronic medical records (EMR) based on the presence of an ICD-9 code for nicotine dependence or identification of current smoking status based on results of required annual screening. Veterans were sent an introductory letter that described the study and encouraged smoking cessation and included a toll-free opt out number. Those that did not decline were called and asked if they were currently smoking cigarettes and willing to quit smoking in the next 30 days. Participating veterans completed a baseline survey that included demographic data, smoking characteristics, and screens for PTSD, depression, and alcohol misuse. Participants were compensated $25 each for completion of baseline and two follow-up surveys, and received up to $50 for return of saliva samples. Participants enrolled in the study were randomized to receive either an internet-based intervention combined with a tele-health medication clinic or a referral to standard specialty-clinic based treatment (control). Participants were randomized to treatment arm using blocked randomization (in blocks of 4), stratified by gender and presence of psychiatric symptoms (i.e., PTSD/Depression/Alcohol abuse vs. None) was used. Study staff members were blinded to the block size.
2.3 Intervention Description
2.3.1 Specialty Clinic Based Smoking Cessation (Control)
Patients randomized to receive referral to specialty care had a consult placed to the VA specialty-based clinic on their behalf. The clinic subsequently sent a pre-appointment letter and scheduled visits. The clinic provides group and telephone counseling provided by doctoral-level psychologists based on the QuitSmart™ Program (Cooper, Dundon, Hoffman, & Stoever, 2006; Shipley, 1998), with medication management provided by a psychiatrist. NRT and medications were provided as per usual, i.e., veterans attending specialty care met with a psychiatrist at the end of the first clinic session and were offered their choice of NRT and other smoking cessation medications (e.g., Bupropion SR). These smoking cessation aids (NRT, medications) were provided during the clinic visit with renewals sent via mail.
2.3.2 Internet Intervention
Patients randomized to the internet-based intervention were provided a free, lifetime membership to the full, enhanced version of QuitNet® (www.QuitNet.com). The website provides 24/7 access to tailored, online tobacco cessation support that is personalized based on each user’s readiness to quit. The enhanced site offers direct access to online smoking cessation counselors, access to interactive features that offer assistance in selecting a quit date and choosing medications, unlimited access to social support features (e.g., forums, buddies, chat rooms), and access to pro-active email support. Veterans randomized to the internet intervention were encouraged (but not required) to register on-line via a QuitNet® home page branded for the current study.
For patients randomized to the internet intervention, at the end of the baseline assessment call, a study staff member discussed types and side effects of each type of NRT available. Interested participants received a tailored dose of NRT and delivery type based on number of cigarettes smoked per day using an established protocol (e.g., Bastian et al., 2012). This could include an 8-week course of nicotine patches and up to two rescue methods (e.g., nicotine lozenge, gum). The study physician wrote NRT prescriptions, and NRT was provided by the Durham VAMC pharmacy. Patients who reported contraindications at baseline (i.e., high blood pressure not controlled by medication) had to obtain VA physician authorization prior to receiving NRT. Participants were instructed to call the study physician with questions or concerns related to NRT.
2.4 Measures
Demographic information was collected at the baseline survey. Nicotine dependence was assessed with the 6-item Fagerström Test for Nicotine Dependence (Heatherton, Kozlowski, Frecker, & Fagerström, 1991). Depressive symptoms were measured using the 10-item version of the Center for Epidemiological Studies Depression Scale [CES-D 10; (Anderson, Malmgren, Carter, & Patrick, 1994)], which has been used extensively in epidemiologic studies (Andresen, Malmgren, Carter, & Patrick, 1994). A score of 10 or higher indicated significant depressive symptoms (Anderson et al., 1994; Bjorgvinsson, Kertz, Bigda-Peyton, McCoy, & Aderka, 2013). The Primary Care PTSD screen [(Prins et al., 2004); PC-PTSD] was used to screen for clinically significant PTSD symptoms. The PC-PTSD has demonstrated good reliability and validity (Prins et al., 2004). A score of 3 or more was used to suggest possible PTSD (Calhoun et al., 2010). Alcohol misuse was assessed with the three-item AUDIT-C, which has demonstrated adequate reliability and validity in studies comparing outcomes to interview-based diagnostic criteria pertaining to alcohol abuse or dependence in the VA and general U.S. populations (Bradley et al., 2003; Crawford et al., 2013). Scores of ≥ 5 for men and ≥ 4 for women were used to suggest possible alcohol abuse (Crawford et al., 2013).
Utilization of smoking cessation aids (e.g., NRT) was based on review of the EMR and self-report at follow-up surveys. Medical chart reviews were also conducted to examine the number of sessions attended in the usual care condition. Utilization of the website, including registration, frequency of visits, number of page views, contact time (minutes per page), areas of the site visited, use of social support components, use of expert counseling, and use of email support, were provided by QuitNet®.
2.5 Outcome Measures
Reach of the internet intervention was defined as the proportion of veterans who registered and visited the internet site at least once. Reach of the specialty care referral intervention was defined as the proportion of veterans who attended at least one clinic-based session. At both the short (3-month post randomization) and long-term (12 months) follow-ups, participants completed a telephone survey and were asked if they had smoked a cigarette or taken even a puff in the preceding 7 days. Letters were mailed to veterans who did not complete the phone survey to query smoking status. The primary outcome of the trial was self-reported 7-day point-prevalent abstinence at the short-term follow-up. The long-term abstinence was defined as 7-day point-prevalence at the long-term follow-up. Although the primary outcome measure was self-reported abstinence, participants were told that self-reported abstinence would be bio-verified via the use of saliva-sampling kits to test for cotinine among those who reported quitting. Saliva kits were mailed to participants with instructions and postage-paid return envelopes. This method is reported to yield response rates that are comparable to in-person collection methods (McBride et al., 1998; McBride et al., 1999). The cutting score used to assess smoking status was 15 ng/mL unless the participant reported living with a smoker, in which case a cutting score of 18 ng/mL was used to avoid false identification of non-smokers as smokers (Jarvis et al., 2008).
2.6 Cost-Effectiveness Measurement
Cost-effectiveness analysis was conducted from the perspective of the VA as payer and provider. The intervention cost in the analysis was the cost of QuitNet® membership for participants randomized to the intervention group and smoking cessation clinic participation for participants randomized to the specialty clinic referral (control) arm. Provider surveys were used to collect time data for time required to review a consult, mail an appointment letter and make outreach calls. A medical clerk salary level with 30% fringe rate (2014 federal General Schedule (GS) 7-5 salary for Durham, NC was $45,756 -- available at https://www.opm.gov/policy-data-oversight/pay-leave/salaries-wages/2014/general-schedule/) was applied to this time data to derive a cost estimate of enrollment in clinic-based care. All patients randomized to the control arm incurred this enrollment cost. Medical records indicated the number of sessions each control participant attended. Time data was collected from providers for pre-session preparation, clinic session, post-session tasks (e.g., writing chart notes, NRT orders, etc.), and a post-session follow-up call to each patient who attended. A psychologist (GS 13-5, $96,515) salary level with 30% fringe benefit rate in wages was applied to the session time data. The second cost category was smoking cessation aid medications prescribed. Unit costs for smoking cessation aid medications were calculated from the VA’s Pharmacy Benefits Management database. For cases where a type of medication was available from more than one manufacturer, an average cost across brands was used to calculate medication cost incurred.
The measures used for cost effectiveness analyses included 12-month quit rates, life years gained, and quality-adjusted life years (QALYs). We calculated both undiscounted QALYs and QALYs discounted at 3%. If there was missing data or if participants reported being abstinent at the short-term follow-up but not at the long-term follow-up, they were counted as a smoker. Participants who self-reported abstinence at the long-term follow-up were treated as life-long quitters and appropriate gender and age stratified gains in life years and QALYs estimated by Fiscella and Franks (Fiscella & Franks, 1996) were applied to attribute effectiveness.
2.7 Statistical Analysis
Sample size estimation was based on the primary hypothesis that the internet intervention would have higher impact as measured by self-reported 7-day point prevalent abstinence at the short-term follow-up as compared to specialty referral. While the efficacy of receiving intensive specialty interventions is as high 23% (Fiore et al., 2000), the reach of these clinics is low (6–14%) (Sherman et al., 2005; Thompson et al., 1988; Yano et al., 2008). Thus, we expected that the overall quit-rate (impact) of referral to specialty care would approach 6%–8%. Based on a differential rate of at least 10% (e.g., 8% vs 18%), sample size calculations assumed a power of 80% and a two-sided type-I error rate of 5% and used standard methods for a difference in proportions. To detect a difference of 10% at the short-term follow-up, 175 participants in each group were needed; however, we enrolled 413 veterans to ensure adequate statistical power.
Differences in intervention reach were estimated using a logistic regression model that included intervention arm and the stratification variables. A generalized linear model (GLM) with a logit link was used to estimate differences in self-reported abstinence rates for the internet intervention as compared to specialty referral at both the short-term and long-term follow-up end points. Model parameters were estimated via generalized estimating equations (GEE) and included indicators for time, intervention arm, and their interaction, as well as the stratification variables of sex and psychiatric symptoms. An exchangeable covariance was used to account for the correlation between patients’ repeated measures over time. In the primary analyses, the non-respondents to the follow-up interviews and letters were treated as smokers.
Additional analyses used multiple imputation procedures to impute missing data based on the assumption that data were missing not at random (MNAR), i.e., that a missed interview was directly related to smoking status. The MNAR multiple imputation analysis follows the multiple imputation methods proposed in Hedeker et al. (Hedeker, Mermelstein, & Demirtas, 2007). In the imputation model, the odds ratio reflecting the association between missing and smoking was set to a range of values (2, 5, and 10), indicating a high likelihood that non-responders were smoking, while allowing for variation in the missing data, rather than treating the missing data as constant. One hundred imputed datasets were generated and fit with the same GLM as described above. PROC MIANALYZE was used to combine the model estimates and standard errors across the 100 imputations; therefore, the standard error estimates (i.e., width of the confidence intervals) reflect the additional variation attributable to imputing missing data. Post-hoc analyses compared abstinence rates between the study arms for OEF/OIF veterans versus other era veterans using a GLM with the multiply imputed data. Post-hoc analyses also compared quit rates (missing=smoking) between smokers who screened positive for a psychiatric condition versus those who did not.
To calculate cost-per-quit, we used the respective quit rate estimates based on missing=smoking. Statistical significance of differences in median costs were examined via Wilcoxon two-sample tests. Differences in incremental cost effectiveness including life years gained and QALYs between the internet and specialty care groups were assessed using t-tests based on unequal variances. All analyses were conducted using SAS 9.2 (SAS Institute, Cary, NC).
3.0 RESULTS
3.1 Study Response and Participant Characteristics
Because all of our primary and secondary analyses involved imputation of missing values at the follow-up visits, patients who died after randomization (n=5) were not included in analyses. Demographics of the analyzed sample (N=408) are shown in Table 1. The mean age of the sample was 42.9 years (SD=13.9), 51% were White, 16% were female, most (82%) had internet access at home, and 48% served during OEF/OIF. Many participants screened positive for PTSD (41%), depression (44%), and alcohol abuse (29%). In total, 66% (n=270) of the sample screened positive for PTSD or depression or alcohol abuse. Rates of dropout were similar between the two arms. Of the 205 patients randomized to the internet intervention, 36 (18%) were missing at the short-term follow-up and 49 (24%) were missing at the long-term follow-up. Among the 203 randomized to specialty referral, the missing rates were 19% and 25% at the short and long-term follow-ups, respectively. Participants lost to follow-up at the primary endpoint did not significantly differ from respondents as a function of nicotine dependence, age, gender, race, education, employment status or presence of probable PTSD, depression, or alcohol misuse. However, a larger proportion of OEF/OIF participants were missing (24%) than veterans of other eras (13%; OR = 2.20; 95% CI 1.31–3.69, p=.003).
Table 1.
Baseline characteristics of Participants
| Overall (n=408) | Internet Intervention (n=205) | Clinic Based Specialty Care (n=203) | |
|---|---|---|---|
| Mean age (SD) | 42.9 (13.9) | 43.3 (13.6) | 42.6 (14.3) |
| Percent Female | 16 | 15 | 16 |
| Percent Caucasian/White | 51 | 51 | 51 |
| Percent African American/Black | 39 | 37 | 41 |
| Percent Hispanic/Latino | 4 | 5 | 4 |
| Percent Married | 54 | 59 | 50 |
| Percent Education | |||
| High school or less | 24 | 27 | 20 |
| More than high school | 76 | 73 | 80 |
| Percent Employed Full or Part Time | 44 | 46 | 42 |
| Percent Era of Service | |||
| OEF/OIF/OND | 48 | 48 | 48 |
| Other | 52 | 52 | 52 |
| Percent Internet Access in Home | 82 | 84 | 80 |
| Mean Age started smoking (SD) | 17 (4.0) | 17.1 (4.1) | 17.0 (3.9) |
| Tobacco Type | |||
| Cigarettes | 96 | 95 | 97 |
| Other | 4 | 4.9 | 3.0 |
| Mean Number of Daily Cigarettes (SD) | 15.2 (8.7) | 15.7 (8.8) | 14.6 (8.5) |
| Mean Nicotine Dependence (FTND) Score* | 3.5 (2.4) | 3.6 (2.4) | 3.4 (2.3) |
| Percent Positive Depression (CESD Score ≥10) | 44 | 44 | 43 |
| Percent Positive PTSD (PC-PTSD Score ≥ 3) | 41 | 42 | 39 |
| Percent Positive AUDIT-C (Score ≥ 5 for men, ≥ 4 for women) | 29 | 30 | 29 |
| Mean Self-Efficacy (SD) | 5.3 (1.6) | 5.4 (1.5) | 5.2 (1.7) |
Note: OEF/OIF/OND = Operation Enduring Freedom/Operation Iraqi Feedom/Operation New Dawn; FTND = Fagerström Test for Nicotine Dependence;
FTND score based on cigarette score unless participant only used cigars;
CESD = Center for Epidemiologic Studies Depression Scale; PC_PTSD = Primary Care PTSD Screen; AUDIT-C = Alcohol Use Disorders Identification Test
Follow-up assessments were attempted beginning at 3 months post-randomization (short-term follow-up) and again at 12-months randomization (long-term follow-up). The median (mean) time until short-term follow-up was 115 days (122 days), while the median (mean) time until long-term follow-up was 385 days (419 days).
3.2 Intervention Reach
Reach of the internet intervention was significantly greater than the control. Fifty percent of those randomized to the internet arm went online and completed registration on the web-based smoking cessation site, whereas only 39 (19%) of those randomized to specialty care attended any clinic based sessions (OR = 4.17; 95% CI 2.67–6.49, p<.0001). Veterans randomized to the internet intervention were also significantly more likely to receive NRT than those randomized to specialty care; 76% versus 20% (OR = 12.83; 95% CI 8.00–20.58, p <.0001). Post-hoc analysis indicated that among those randomized to the internet intervention, reach was significantly higher among those who had home-based internet access (55.5%) compared to those without internet access at home (18.8%; OR = 5.40, 95% CI 2.11–13.79, p=.0004).
3.3 Primary Outcome: Self-reported 7-day Abstinence
No significant differences by intervention arm were observed at the short-term or long-term follow-ups. Based on the primary analysis where missing=smoking, model-adjusted quit rates in the internet-based intervention were 16.8% (95% CI 12.3–22.7) at the short-term endpoint compared to 11.7% (95% CI 8.0–16.8) in the standard specialty care arm (see Table 2). Additionally, no significant differences between groups at the long-term follow up were observed. The multiple imputation analyses resulted in slightly higher abstinence rate estimates and wider confidence intervals due to increased variability in the missing response variable (see Table 2). Imputation results revealed no significant differences between the groups at the short- and long-term follow-up.
Table 2.
Self-Reported 7-Day Point Prevalence Abstinence (95% Confidence Intervals) at Short and Long Term Follow-ups
| Short term Follow-up | Long Term Follow-up | |||||
|---|---|---|---|---|---|---|
| Internet Intervention | Specialty Care | Internet Intervention | Specialty Care | |||
| N=205 | N=203 | p-value | N=205 | N=203 | p-value | |
| Analysis with missing=smokinga,c | 16.8% (12.3%, 22.7%) | 11.7% (8.0%, 16.8%) | 0.14 | 13.5% (9.4%, 19.0%) | 15.6% (11.3%, 21.3%) | 0.53 |
| Multiple Imputation Analysis with OR=5b,c | 17.4% (12.7%, 23.3%) | 12.7% (8.7%, 18.0%) | 0.19 | 15.2% (10.7%, 21.3%) | 16.9% (12.2%, 22.8%) | 0.66 |
Note:
Analysis treats participants with missing outcome data as smokers.
The MNAR imputation analysis follows the multiple imputation methods proposed in Hedeker et al. (2007). In the imputation model, the odds ratio reflecting the association between missing and smoking was set to 5, indicating a high likelihood that non-responders were smoking.
Model adjusted for sex and presence of psychiatric symptoms, the stratification variables
Although the primary outcome of the trial was self-reported abstinence, saliva was collected from participants reporting abstinence to verify smoking status. At the 3-month follow-up, 20 participants in the intervention group (57% of those reporting abstinence) provided a saliva sample. Of these, ten were deemed untestable due to insufficient saliva (n=2) or the participant reported using NRT (n=6) or other products containing nicotine such as snuff (n=2). In the control group, 13 samples (54%) were returned and 11 were tested (2 were untestable due to reported NRT use). At the 12-month follow-up, 13 participants in the intervention group provided a sample (46% of those reporting abstinence). Two samples were determined to be untestable due to report of exposure to products containing nicotine. Forty-one percent of participants who reported abstinence in the control group (n=13) returned a saliva sample; two were deemed untestable due to insufficient saliva or report of NRT. There was not a statistically significant difference between groups in the concordance of self-report with cotinine results at the short-term or long-term follow-ups. Overall, the observed concordance in the intervention group was excellent (91%), while the concordance in the control group was 77%. Bio-verified long term abstinence rates based on missing=smoking analysis and treating untestable samples as smoking were 5.4% in the internet arm and 3.5% in the control arm.
3.4 Utilization of Smoking Cessation Treatment and Outcomes
Across both arms of the study, participants who requested NRT had similar smoking cessation rates at both the short-term (16% vs. 13%, χ2=0.90, n.s.) and long-term (15% vs. 14%; χ2=0.06, n.s.) follow-ups compared with those not requesting NRT. Among those randomized to usual care, quit rates for those participants that attended at least one session were 21%. The number of clinic sessions completed was related to both short-term (Cochran-Armitage Z = −3.03, p < .003) and long term quit rates (Cochran-Armitage Z = −2.01 p<.05).
Among those who registered with the internet site (n=102), average time online the site was associated with long-term abstinence (r=.21, p<.05). Overall, however, there was relatively little use of the site. Veterans who registered on the internet intervention returned to the site an average of 1 time (range = 0–5; M = 0.77, SD=0.87; median=1). Forty-five veterans (44%) did not use the site after they initially registered; 38% returned to the site once, and 18% returned to the site 2–5 times. On average, registered participants spent 33 minutes on the site (SD = 38.0; median = 35 minutes; first-third quartiles = 0–47 minutes). There was almost no use of many of the interactive expert systems and social support programs built into the site. Twenty-seven (26%) of registered participants used the expert system to help them set a quit date. There was no use of expert forums (0%). Few (<1%) posted to a public forum or added a quit buddy and none of the registered participants used the club and chat functions. Few (< 1%) sent an internal email to communicate with other QuitNet® members, with 7% receiving an internal email from other users.
3.5 Subgroup Analyses
While OEF/OIF veterans (15%) appeared to have decreased attendance rates at specialty clinic-based care compared to other era veterans (23%), this difference was not statistically significant. OEF/OIF veterans, however, were more likely to use the internet intervention compared to other era veterans (61% vs. 40%; OR=2.34, 95% CI 1.34–4.11, p<.01). Model estimates (results not shown) examining results stratified by OEF/OIF status suggest that OEF/OIF status did not significantly moderate the effect of treatment within usual care or the internet arm. Collapsing across arms of the study, however, analyses assuming missing=smoking suggest that OEF/OIF veterans were less likely to have quit smoking at 12 months than other era veterans (11% vs. 18%; OR = 0.53, 95% CI 0.30–0.93, p<.05).
Compared to smokers who did not screen positive for a mental health condition, those who screened positive for either PTSD, depression, or alcohol abuse were less likely to report abstinence at the primary end-point (17.4% vs. 13.0%), although this difference did not reach statistical significance. There was a similar non-significant trend for smokers who screened positive for PTSD, depression or alcohol abuse to report lower quit rates at the 12-month follow-up (17.4% vs. 13.3%).
3.6 Costs and Cost-Effectiveness
Per-patient costs were significantly higher for patients randomized to the internet arm where mean costs were $178 (median=$113) versus $26 (median=$7) for those randomized to referral for specialty care [median two-sample test p<.0001]. Of the $178 in costs for the internet participants, $121 (median=$58) was due to NRT costs; NRT costs for specialty care participants on average represented $12 (median=$0) of their $26 per-patient costs (p<.0001). These costs reflect that both penetration and intensity of NRT use was substantially higher among those in the internet intervention arm. Among participants who used some form of NRT, the NRT cost was much greater in the internet arm (n=153) compared to the specialty care group (n=40) ($162 (median=$96) vs. $60 (median=$52) p < 0.001).
The internet intervention resulted in 28 quits at 12 months, a gain of 0.51 life years, 0.63 undiscounted QALYS, and 0.27 discounted QALYs gained per patient. Specialty care participants had 32 quits, gained 0.48 life years, 0.60 undiscounted QALYS, and 0.27 discounted QALYs gained per patient. None of the differences in incremental effectiveness measures were statistically significant.
4.0 DISCUSSION
This is the first comparative effectiveness trial comparing an internet intervention paired with a tele-medicine clinic for NRT with referral to standard clinic-based smoking cessation care for veteran smokers. As predicted, the reach of the internet intervention (defined as registering with and visiting the web intervention) was greater than referral to specialty care, where reach was defined as attending one or more clinic sessions. The proportion of participants using NRT was also higher among those referred to the internet plus telemedicine clinic arm compared to usual care. Self-reported short and long-term cessation rates, however, were not significantly different. Overall quit rates in both arms (> 13%) compare favorably to rates achieved in pro-active telephone counseling interventions that have used similar proactive recruitment methods (Tzelepis, Paul, Walsh, McElduff, & Knight, 2011).
The impact of clinic-based care is often limited by low attendance rates. Documented attendance to specialty-based smoking cessation clinics is as low as 6%–14% (Sherman et al., 2005; Thompson et al., 1988; Yano et al., 2008). Thus, we expected that despite high efficacy, the overall impact of specialty care would be low. Consistent with expectations, the observed efficacy of specialty clinic-based care for those that attended at least one session in the current trial was high (21%) and was consistent with quit rates observed in other intensive interventions, e.g., an average efficacy rate of 23%; 95% CI, 19.9%–26.6% (Fiore et al., 2000). In the current trial, however, attendance at clinic-based specialty care was higher than anticipated (19%), which contributed to higher than expected impact for specialty care. It is unclear why attendance rates observed during the trial appear higher than usual. It is possible that smokers who agree to make a quit attempt in the next 30 days after they are contacted proactively by phone represent a group with greater intention to quit than patients who are advised to quit by their primary care provider and agree to a referral during the context of a primary care visit.
Under Federal Law (38 CFR. 17.108 (e) (13)) the VA removed co-pays for individual and group smoking cessation counseling. Thus, in terms of direct costs to patients there were no differences between the interventions. More patients in the internet intervention arm, however, received NRT compared to those randomized to usual care (where provision of NRT was limited to those who attended clinic-based sessions). Proactively recruiting smokers using the EMR, screening them via telephone, and mailing tailored dosages of NRT could be used to significantly increase the reach of NRT utilization over currently employed clinic-based methods.
From the VA perspective, the QuitNet® group incurred substantially higher intervention costs than those in the usual care group and effectiveness (as measured by self-reported quits, life years and QALYs) was similar. The majority of the differences in costs were related to NRT medication utilization observed between the two groups. Counseling costs of specialty-based care were based on costs associated with a doctoral level psychologist counselor, which is standard in the majority of specialty based smoking cessation clinics in VA (Department of Veterans Affairs, 2010). Other staffing models (e.g., nurses) would obviously be associated with different costs.
It is surprising that the large difference in NRT utilization and costs between arms was not associated with a significant increase in cessation rates. While the evidence for the efficacy of NRT in clinical trials is convincing (Stead et al, 2012), there is growing controversy and concern over the effectiveness of NRT in real world settings. Several recent studies have shown little to no benefit for NRT in the context of effectiveness trials or real world settings (Alpert et al., 2012; Bastian et al.,2012; Kotz et al., 2013; Kotz et al., 2014). A recent large, population-based effectiveness study (Cunningham et al., 2016) that examined the effectiveness of simply mailing NRT to smokers found that NRT was associated with significantly higher cessation rates; 7.4% of smokers mailed NRT (without behavioral support) reported abstinence compared to 3% in a control group that received no NRT (bio-verified results suggest 2.8% of smokers in the NRT intervention were abstinent vs. 1% in the control group). These results provide support for the continued use of NRT at the population level. More work needs to be done, however, to examine the characteristics of smokers who choose to use NRT and to examine how adherence to NRT affects smoking cessation outcomes.
The 12-month quit rates observed in the internet arm (13%–15%) are consistent with a previous uncontrolled trial of QuitNet® that was paired with a $132 financial incentive among IBM employees. Graham and colleagues reported a 7-day point-prevalence abstinence rate of 15.2% using missing=smoking analyses among those who used QuitNet® (Graham et al., 2007). Participants in the current trial were not offered a financial incentive to use the website but had the choice of free NRT. The observed positive relationship between treatment contact time and smoking cessation outcomes in the current study is consistent with other treatment modalities as described in the Public Health Service Clinical Practice Guideline (Fiore, 2000).
Most previous studies of internet interventions have limited the sample to those with internet access. Given the current study was designed as an effectiveness trial, we did not limit the sample to those with internet access at home. While most veterans in the study (82%) reported having access to the internet at home, use of the website was lower among those who did not have internet access at home (18.8% vs. 55.5%). Lack of internet access is an obvious barrier to e-health interventions, however, internet access is increasingly common and is almost universal among OEF/OIF era veterans using VA (Sayer et al., 2010).
Overall, however, there was relatively low utilization of the website and almost no use of the social support features on QuitNet®. Although anonymity of online interactions has been thought to facilitate social support (Kramish et al., 2001), few veterans in the current study took advantage of available on-line chat groups, forums, buddies, or contacts with experts. Previous evaluations of QuitNet® conducted among IBM employees and general users have documented higher utilization rates of the social support features of the site (Cobb et al., 2005; Graham et al., 2007). A non-randomized evaluation of QuitNet found that individuals who use the social support features on the site are more than three times more likely to quit smoking compared to less engaged users (Cobb et al., 2005). It remains unclear why so few veterans engaged with the social support features of the site. A recent investigation of the key structural characteristics of the QuitNet® social network, however, found that most users of the social network are women (Cobb et al., 2010). Only 16% of the current sample were women, which could partially explain differences between the current study and previous evaluations of QuitNet®. More work needs to be done to examine ways of increasing the intensity of utilization of web or other e-health interventions.
Results from the current effectiveness study documenting low rates of utilization of the internet based intervention are consistent with low utilization rates observed among veterans after the VA partnered with TRICARE so that veterans could utilize the “QUIT TOBACCO Make Everyone Proud” smoking cessation website (http://www.ucanquit2.org/). Based in part upon limited utilization of the Department of Defense site, the VA no longer funds an internet-based smoking cessation site. Some of the new resources promoted by VA include the creation of a VA-centric quitline 1-855-QUIT VET, the Stay Quit Coach mobile application (a relapse prevention app) and a smoking cessation texting program (SmokefreeVET). The efficacy of Stay Quit Coach and SmokefreeVet remain important avenues for future research.
Psychiatric comorbidity was highly prevalent in the current sample of veteran smokers. Smokers who screened positive for PTSD, depression or alcohol abuse were less likely to report abstinence in the current trial, although this difference did not reach statistical significance. There is a large literature documenting that smokers with psychiatric disorders have increased difficulty quitting smoking (Ziedonis et al., 2008). Novel interventions that increase reach of intensive treatment may be needed to maximize quit rates among veterans and smokers with psychiatric disorders. A recent approach that uses a mobile health platform (smartphones) to implement contingency management (an intensive behavioral therapy) paired with smoking cessation medications and cognitive behavioral telephone counseling for relapse prevention appears promising but needs further evaluation (Carpenter et al., 2015; Hertzberg et al., 2013).
There are a number of limitations associated with the study. First, while proactive recruitment methods were used to maximize generalizability of results, participants were limited to veteran smokers who reported they were willing to make a quit attempt in the next 30 days. All participants were VA users. Results may not generalize to the population of veteran smokers who are not ready to quit or who are not VHA users. Costs observed in the VHA may not be similar to those at non-VHA health systems. Other systems may use less expensive providers to conduct the smoking cessation sessions and their patients may incur different NRT costs, especially if buying NRT over-the-counter. We compared VHA NRT costs with those available at drugstore.com (www.drugstore.com, access on 9/13/15) and found their prices to be comparable. However, the copay for NRT for veterans is likely lower than that incurred by non-veterans. Similarly, results may not generalize to all web-based interventions. QuitNet® is a commercial web site that includes interactive social support features, tailored content, direct access to smoking cessation counselors, and smoking cessation content that is in accordance with national guidelines (Fiore et al., 2000). While we encouraged veterans to register on the specially branded internet site, we were unable to send them an email link to the site due to VA privacy rules. More veterans may have chosen to register and use the site if the registration process had been streamlined. Finally, although we attempted biochemical confirmation of smoking abstinence for all self-reported quitters, rates of return for saliva kits were less than 50% in both arms. False reporting of smoking status, however, is considered to be minimal among adult populations, especially when participants know that bio-verification will occur such as in the current trial (Patrick et al., 1994).
5.0 CONCLUSION
Electronic and mobile health interventions can improve reach of available smoking cessation services. The current trial demonstrates that it is feasible to use the VA’s electronic medical record to identify smokers and proactively contact them to gauge willingness to make a quit attempt. Twenty-nine percent of veterans reached by phone were currently smoking tobacco, willing to make a quit attempt in the next 30 days, and willing to be enrolled in the trial. There were no statistical differences in overall quit rates or cost effectiveness between veterans referred to clinic-based specialty care or to an internet intervention paired with a tele-medicine clinic for NRT. Leveraging electronic medical records to identify smokers and implementing proactive methods to offer smoking cessation interventions that are consistent with clinical practice guidelines may be an ideal strategy to reduce smoking in VA and other large health care organizations. Novel interventions that increase reach of intensive smoking cessation treatment are needed to maximize quit rates.
Highlights.
The Internet intervention arm was associated with increased reach over usual care.
There were no significant differences between arms in quit rates at 3 or 12 months.
Both interventions were cost effective.
Costs were higher for the internet arm due to increased penetration of NRT.
Acknowledgments
We would like to express our gratitude for the study staff who conducted the research including Lesley Rohrer, Michael Hill, Lillian Haley, Sherman Lee, Susan Elinoff, and Ania Oddone. The authors would like thank all the participants who kindly volunteered to participate in this study. The views expressed in this paper are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the United States government.
FUNDING
This work was supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, and Health Services Research and Development IIR-08-032. The VHA had no role in the design of the study, in the collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Footnotes
DECLARATION OF INTERESTS
The authors have no conflicts of interest to declare.
References
- Abrams DB, Orleans CT, Niaura RS, Goldstein MG, Prochaska JO, Velicer W. Integrating individual and public health perspectives for treatment of tobacco dependence under managed health care: A combined stepped care and matching model. Annals of Behavioral Medicine. 1996;18:290–304. doi: 10.1007/BF02895291. [DOI] [PubMed] [Google Scholar]
- Acheson SK, Straits-Troster K, Calhoun PS, Beckham JC, Hamlett-Berry K. Characteristics and correlates of tobacco use among U.S. veterans returning from Iraq and Afghanistan. Military Psychology. 2011;23(2):297–314. doi: 10.1080/08995605.2011.570589. [DOI] [Google Scholar]
- Anderson EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventative Medicine. 1994;10:77–84. [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Barlas FM, Higgins WB, Pflieger JC, Diecker K. 2011 Department of Defense health related behaviors survey of active duty military personnel. Fairfax, VA: 2013. [Google Scholar]
- Bastian LA, Fish LJ, Gierisch JM, Rohrer LD, Stechuchak KM, Grambow SC. Comparative effectiveness trial of family-supported smoking cessation intervention versus standard telephone counseling for chronically ill veterans using proactive recruitment. Compartive Effectivness Research. 2012;2:45–56. [Google Scholar]
- Bjorgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20(4):429–436. doi: 10.1177/1073191113481998. [DOI] [PubMed] [Google Scholar]
- Bock B, Graham A, Sciamanna C, Krishnamoorthy J, Whiteley J, Carmona-Barros R, … Abrams D. Smoking cessation treatment on the Internet: Content, quality, and usability. Nicotine & Tobacco Research. 2004;6(2):207–219. doi: 10.1080/14622200410001676332. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, … Kivlahan DR. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): Validation in a female veterans affairs patient population. Archives of Internal Medicine. 2003;163(7):821–829. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Bray RM, Hourani LL, Olmsted KL, Witt W, Brown JM, Pemberton MR, … Hayden D. RT Institute, editor. Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel. U.S. Department of Defense; 2005. pp. 1–359. [Google Scholar]
- Calhoun PS, McDonald SD, Guerra VS, Eggleston AM, Beckham JC, Straits-Troster K. Clinical utility of the Primary Care-PTSD Screen among U.S. veterans who served since September 11, 2001. Psychiatry Res. 2010;178(2):330–335. doi: 10.1016/j.psychres.2009.11.009. [DOI] [PubMed] [Google Scholar]
- Carpenter VL, Hertzberg JS, Kirby AC, Calhoun PS, Moore SD, Dennis MF, … Beckham JC. Multicomponent smoking cessation treatment including mobile contingency management in homeless veterans. Journal of Clinical Psychiatry. 2015;76:959–964. doi: 10.4088/JCP.14m09053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Annual smoking-attributable mortality years of potential life lost and economic costs--United States, 1995–1999. Morbidity and Mortality Weekly Report. 2002;51:300–303. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses - United States, 2000–2004. Morbidity and Mortality Weekly Report. 2008;57(45):1226–1228. [PubMed] [Google Scholar]
- Cooper TV, Dundon M, Hoffman BM, Stoever CJ. General and smoking cessation related weight concerns in veterans. Addictive Behaviors. 2006;31(4):722–725. doi: 10.1016/j.addbeh.2005.05.045. [DOI] [PubMed] [Google Scholar]
- Crawford EF, Fulton JJ, Swinkels CM, Beckham JC, VA, Calhoun PS Mid-Atlantic MIRECC OEF/OIF Registry Workgroup. Diagnostic efficiency of the AUDIT-C in U.S. veterans with military service since September 11, 2001. Drug and Alcohol Dependence. 2013;132(1):101–106. doi: 10.1016/j.drugalcdep.2013.01.012. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Kushnir V, Selby P, Tyndale RF, Zawertailo L, Leatherdale ST. Effect of mailing nicotine patches on tobacco cessation among adult smokers: A randomized clinical trial. JAMA Internal Medicine. 2016;176(2):184–190. doi: 10.1001/jamainternmed.2015.7792. [DOI] [PubMed] [Google Scholar]
- Department of Veterans Affairs. Smoking and Tobacco Use Cessation Report. 2010. [Google Scholar]
- Feigelman W. Cigarette smoking among former military service personnel: A neglected social issue. Preventative Medicine. 1994;23:235–241. doi: 10.1006/pmed.1994.1032. [DOI] [PubMed] [Google Scholar]
- Fiore MC. A clinical practice guideline for treating tobacco use and dependence: A US public health service report. Journal of the American Medical Association. 2000;283(24):3244–3254. doi: 10.1016/j.amepre.2008.04.009. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services; 2000. Treating Tobacco Use and Dependence. [Google Scholar]
- Fiscella K, Franks P. Cost-effectiveness of the transdermal nicotine patch as an adjunct to physicians’ smoking cessation counseling. Journal of the American Medical Association. 1996;275:1247–1251. doi: 10.1001/jama.1996.03530400035035. [DOI] [PubMed] [Google Scholar]
- Graham AL, Cobb NK, Raymond L, Sill S, Young J. Effectiveness of an internet-based worksite smoking cessation intervention at 12 months. Journal of Occupational and Environmental Medicine. 2007;49:821–828. doi: 10.1097/JOM.0b013e3180d09e6f. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Mermelstein RJ, Demirtas H. Analysis of binary outcomes with missing data: Missing = smoking, last observation carried forward, and a little multiple imputation. Addiction. 2007;102(10):1564–1573. doi: 10.1111/j.1360-0443.2007.01946.x. [DOI] [PubMed] [Google Scholar]
- Hertzberg JS, Carpenter VL, Kirby AC, Calhoun PS, Moore SD, Dennis MF, … Beckham JC. Mobile contingency management as an adjunctive smoking cessation treatment for smokers with posttraumatic stress disorder. Nicotine & Tobacco Research. 2013;15(11):1934–1938. doi: 10.1093/ntr/ntt060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby AC, Hertzberg BP, Collie CF, Yeatts B, Dennis MF, McDonald SD, … Beckham JC. Smoking in help-seeking veterans with PTSD returning from Afghanistan and Iraq. Addictive Behaviors. 2008;33:1448–1453. doi: 10.1016/j.addbeh.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramish M, Meier A, Enga Z, James AS, Reedy J, Zheng B. Health behavior changes after colon cancer: a comparison of findings form face-to-face and online focus groups. Family Community Health. 2001;24:88–103. doi: 10.1097/00003727-200110000-00010. [DOI] [PubMed] [Google Scholar]
- McBride CM, Curry SJ, Grothaus LC, Nelson JC, Lando H, Pirie PL. Partner smoking status and pregnant smoker’s perceptions of support for and likelihood of smoking cessation. Health Psychology. 1998;17:63–69. doi: 10.1037//0278-6133.17.1.63. [DOI] [PubMed] [Google Scholar]
- McBride CM, Curry SJ, Lando HA, Pirie PL, Grothaus LC, Nelson JC. Prevention of relapse in women who quit smoking during pregnancy. American Journal of Public Health. 1999;89:706–711. doi: 10.2105/ajph.89.5.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinney WP, McIntire DD, Carmody TJ, Joseph A. Comparing the smoking behavior of veterans and nonveterans. Public Health Reports. 1997;112:212–217. [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States. Journal of the American Medical Association. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: A review and meta-analysis. American Journal of Public Health. 1994;84(7):1086–1093. doi: 10.2105/ajph.84.7.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Ouimette PC, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, … Sheikh JI. The Primary Care PTSD Screen (PC-PTSD): Development and operating characteristics. International Journal of Psychiatry in Clinical Practice. 2004;9:9–14. doi: 10.1185/135525703125002360. [DOI] [Google Scholar]
- Sayer NA, Noorbaloochi S, Frazier P, Carlson K, Gravely A, Murdoch M. Reintegration problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical care. Psychiatric Services. 2010;61:589–597. doi: 10.1176/ps.2010.61.6.589. [DOI] [PubMed] [Google Scholar]
- Schneiderman AL, Lincoln AE, Curbow B, Kang HK. Variations in health communication needs among combat veterans. American Journal of Public Health. 2004;(94):2074–2076. doi: 10.2105/ajph.94.12.2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman SE, Farmer MM. Best practices in tobacco control: Identifying effective strategies for improving quality within the Veterans Health Administration. Paper presented at the VA in the Vanguard: Building on Success in Smoking Cessation.Sep 21, 2004. [Google Scholar]
- Sherman SE, Joseph AM, Yano EM, Simon BR, Arikian NJ, Rubenstein LV, … Mittman BS. Assessing the institutional approach to implementing smoking cessation practice guidelines in Veterans Health Administration facilities. Military Medicine. 2006;171:80–87. doi: 10.7205/milmed.171.1.80. [DOI] [PubMed] [Google Scholar]
- Sherman SE, Yano EM, Lanto AB, Simon BF, Rubenstein LV. Smokers’ interest in quitting and services received: Using practice information to plan quality improvement and policy for smoking cessation. American Journal of Medical Quality. 2005;20(1):33–39. doi: 10.1177/1062860604273776. [DOI] [PubMed] [Google Scholar]
- Shipley RH. QuitSmart leader manual: Scientific foundations and implementation guidelines for the QuitSmart stop smoking system. Durham, NC: QuitSmart Stop Smoking Resources, Inc; 1998. [Google Scholar]
- Shipley RH, Steffen P, Riley K. Effectiveness of a stop smoking program for veterans with and without psychiatric diagnoses. Veterans Health System Journal. 1999;4(5):65–67. [Google Scholar]
- Thompson RS, Michnich ME, Friedlander L, Gilson B, Grothaus LC, Storer B. Effectiveness of smoking cessation interventions integrated into primary care practice. Medical Care. 1988;26:62–76. doi: 10.1097/00005650-198801000-00007. [DOI] [PubMed] [Google Scholar]
- Tzelepis F, Paul CL, Walsh RA, McElduff P, Knight J. Proactive telephone counseling for smoking cessation: Meta-analyses by recruitment channel and methodological quality. J Natl Cancer Inst. 2011;103(12):922–941. doi: 10.1093/jnci/djr169. [DOI] [PubMed] [Google Scholar]
- Yano EM, Rubenstein LV, Farmer MM, Chernof BA, Mittman BS, Lanto AB, … Sherman SE. Targeting primary care referrals to smoking cessation clinics does not improve quit rates: Implementing evidence-based interventions into practice. Health Services Research. 2008;43(5):1637–1660. doi: 10.1111/j.1475-6773.2008.00865.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziedonis D, Hitsman B, Beckham JC, Zvolensky M, Adler LE, Audrain-McGovern J, … Riley WT. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine & Tobacco Research. 2008;10(12):1691–1715. doi: 10.1080/14622200802443569. [DOI] [PubMed] [Google Scholar]