Summary
Background:
Using lingual enamel surfaces for bracket placement not only has esthetic advantages, but may also be suitable in terms of reducing frequencies of enamel decalcifications.
Objective:
To test the null-hypothesis that there is no significant difference in enamel decalcification or cavitation incidence adjacent to and beneath bracket bases between two lingual multi-bracket (MB) appliances that are different in terms of design, material composition, and manufacturing technology (group A: WIN, DW-LingualSystems; group B: Incognito, 3M-Unitek), taking into account patient- and treatment-related variables on white spot lesion (WSL) formation.
Methods:
Standardized, digital, top-view photographs of 630 consecutive subjects (16214 teeth; n Incognito = 237/6076 teeth; n WIN = 393/10138 teeth; mean age: 17.47±7.8; m/f 43.2/56.8%) with completed lingual MB treatment of the upper and lower permanent teeth 1–7 were screened for decalcification or cavitation adjacent to and beneath the bracket bases before and after treatment, scored from 0 to 7. Non-parametric ANOVA was used for main effects ‘appliance type’, ‘gender’, ‘treatment complexity’, ‘grouped age’ (≤16/>16 years), and ‘treatment duration’ as covariable, at an α-level of 5%.
Results:
About 2.57% [5.94%] of all teeth in group A [B] developed decalcifications. Subject-related incidence was 9.59% [16.17%] for upper incisors in group A [B], and 12.98% [25.74%] for all teeth 16–46. There were significant effects by gender, age, and treatment duration.
Conclusion:
The null-hypothesis was rejected: sub-bracket lesions were significantly less frequent in group A, while frequencies of WSL adjacent to brackets were not significantly affected by appliance type. In view of the overall low incidences of lingual post-orthodontic white-spot lesions, the use of lingual appliances is advocated as a valid strategy for a reduction of enamel decalcifications during orthodontic treatment.
Introduction
Successful orthodontic treatment of large parts of populations is based on non-compliance multi-bracket (MB) treatment. These appliances have undergone many developments before taking on the form they have today. The process of development has mostly focussed on rationalization and standardization of the treatment procedure: Examples are modifications of the bracket design, or attempts to decrease treatment time and forces applied by using self-ligating brackets and nickel-titanium archwires, thereby reducing side-effects that are related to long durations of treatment, such as root resorptions. Other developments aim at enhancing esthetics, by using smaller or clear brackets, or lingual appliances (1–3).
However, even today, prevention of white spot lesions (WSL) remains a challenge in orthodontics, as they present not only esthetic problems in the majority of finished orthodontic cases (4, 5), but are also, in the first line, an incipient caries (International Statistical Classification of Diseases and Related Health Problems, ICD-10/K02.0). WSLs are generated when the balance between natural enamel re-mineralization and demineralization is shifted to the latter (6). Risk factors for deterioration during orthodontic treatment which are more or less controllable by the orthodontist include inadequate oral hygiene, pre-existing WSL, absence or lack of fluoride supply, and a patient being pre-adolescent at the start of treatment (7–9). However, even in the absence of these risk factors, WSL may form within a matter of weeks (5), and the reasons for the variation in WSL susceptibility relates to individual salivary composition and salivary flow rates (10).
Data are available that demonstrate the persistence of WSLs over 12 years or more after completion of orthodontic therapy, and it is unlikely that they will ever completely disappear without additional treatment. Modern dentistry offers a diversity of approaches to, first and foremost, prevent WSL or, as a secondary objective, improve their appearance (11). However, most of these preventive approaches require permanent care and the attention of both the orthodontist and the patient, and are frequently associated with additional costs. If the esthetic recovery of demineralized enamel is the focus, as with micro-abrasion or the infiltration technique, the cost factor also comes into consideration (8). Finally, minimally invasive and micro-invasive approaches are limited in effectiveness when applied to deeper-seated lesions (11).
Recently, an entirely different approach to WSL prevention has been presented which proposes the use of lingual orthodontics, instead of conventional buccal appliances still used in the majority of orthodontic treatments (12). Recent research has highlighted the fact that using lingual enamel surfaces for bracket placement not only has esthetic advantages, but may also be superior to conventional labial appliances, in terms of reducing decalcifications (12).
Little substantial information is available based on in vivo research on the subject of improving WSL protection during fixed orthodontic treatment by selecting lingual appliances instead of conventional fixed-labial approaches. However, lingual enamel surfaces show less pronounced conformity compared with labial enamel surfaces. A technical challenge to overcome when attempting to decrease numbers of WSLs by utilizing lingual orthodontic appliances is that the quality of the fitting of bracket bases and the adhesive layer to the enamel surfaces potentially have an influence on WSL formation: the problem of WSL and cavitation not only next to, but also beneath the bracket base, as a result of potential inaccuracies at the bracket base/enamel interface, has been described recently (13). The higher the congruence between bracket base and lingual enamel surface, the better will be the fit of the bracket, and the thinner will be the bonding or adhesive layer needed. Completely customized lingual bracket systems with individual base contours have been reported to be superior to readymade brackets or half-customized bracket systems, in terms of both fitting and quality of treatment results achieved (3). The types of completely customized lingual bracket systems currently available vary fundamentally in terms of design, material composition, and manufacturing technology.
Study aim
The aim of the study presented here was to assess the incidence and severity of white-spot lesion formation following lingual MB treatment, taking into account the appliance type, gender of the patient, treatment complexity, grouped age (≤16/>16 years), and treatment duration.
We tested the null-hypothesis of no significant difference in WSL formation both adjacent and beneath the bracket base area (sub-bracket lesions, SBL) following incorporation of either of two customized lingual orthodontic appliances that are different in terms of design, material composition, and manufacturing technology.
Subjects and methods
Ethical approval was obtained prior to the start of the trial from the University of Hannover Medical School Ethics Committee [#1189/2011]. This trial included 630 consecutive patients (16214 teeth) who met the ‘inclusion criteria’ of having received comprehensive lingual bracket treatment of both the upper and the lower permanent teeth 1–7 during the time period 1 April 2010 to 30 September 2014 in one orthodontic center (Bad Essen, Germany) with either of two different lingual appliances (group A, WIN, DW LingualSystems and group B, Incognito, 3M-Unitek, TOP-Service für Lingualtechnik; both Bad Essen, Germany). All appliance bondings were carried out using the Incognito system (group B) until November 2011, and using the WIN system (group A) since then. A detailed description of the participant characteristics, such as appliance type distribution, age, gender distribution, and treatment duration is presented in Table 1.
Table 1.
Descriptive analysis of the trial sample.
| Group A (n = 393 subjects, 10138 teeth) | Group B (n = 237 subjects, 6067 teeth) | All groups (n = 630 subjects, 16214 teeth) | |
|---|---|---|---|
| Patients’ age at T0 (years; Mean ± SD) [Min; Max; Median] | 17.47±8.1 Y [11.33; 14.79] | 17.48±7.3 Y [11.34; 53.13; 15.0] | 17.47±7.8 [11.33; 62.93; 14.87] |
| Age group n, % (≤16 / >16 Y) | 273 / 120, 69.47% / 30.53% | 152 / 85, 64.14% / 35.86% | 425 / 205, 67.46% / 32.53% |
| Treatment duration (months; Mean ± SD) [Min; Max; Median] | 21.04±7.31 [3.68; 41.4; 20.3] | 24.71±7.99 [3.26; 44.39; 25.03] | 22.42±7.77 [3.26; 44.39; 21.38] |
| Gender (m / f) n, (%) | 165 / 228 (41.98% / 58.02%) | 107 / 130 (45.15% / 54.85%) | 272 / 358 (43.17% / 56.82%) |
A t-test revealed no significant differences in terms of age of subjects (unpaired t-test, P = 0.99), grouped age distribution, or gender distribution (Pearson chi-square, P = 0.17 and P = 0.44) between the two appliance groups A (WIN) and B (Incognito). The difference in mean treatment duration between the two types of appliances was significant (unpaired t-test, P < 0.0001).
No subject was excluded because of missing records or low quality photo documentation. ‘Exclusion criteria for single teeth’ were 1. restorations or pre-existing WSLs in the area of the palatal or lingual bracket bases; 2. deciduous teeth; and 3. teeth that were tilted such that lingual surfaces were not clearly visible on either of the photographs. Of a total of 17640 (630×28) potentially eligible teeth, 16214 were classified as valid trial teeth. Proportions of missing or non-eligible teeth are given in Table 2, separately for different tooth groups and exclusion criteria.
Table 2.
Proportions of missing teeth, or teeth that were non-eligible according to various exclusion criteria, separately for the tooth groups of maxillary incisors and complete upper and lower dental arches.
| Group | Subjects (n) | Potentially eligible teeth (n) | Valid trial teeth (n) | Missing, restored, or not judgeable upper incisors 12–22 (n) [%] | Missing, restored, or not judgeable teeth 17–47 (n) [%] | Teeth with pre- existing WSLs |
|---|---|---|---|---|---|---|
| A | 393 | 11004 | 10138 | 103 [0.94%] | 838 [7.62%] | 28 [0.25%] |
| B | 237 | 6636 | 6076 | 34 [0.51%] | 526 [7.93%] | 34 [0.51%] |
| Total | 630 | 17640 | 16214 | 137 [1.27%] | 1364 [2.98%] | 62 [0.35%] |
WSL, white spot lesion.
In order to enable assessment of the impact of individual treatment complexities, the severity of malocclusion was categorized as either mild to moderate (S1) or severe malocclusions and difficult (S2) treatments. Subjects were allocated to group S2 if they met at least one of the following criteria which have previously been demonstrated to significantly prolong treatment duration as substantiated by systematic reviews (14):
1. Extractions (covering subjects with severe dental crowding, without the need for error-prone tooth-space analyses);
2. Agenesis of at least one tooth (space opening or dental gap closing treatment)
3. Impacted or dislocated teeth
4. Subjects requiring TADs or Herbst treatment
5. Orthognathic surgery (requiring complex and time-consuming interdisciplinary logistics).
Bonding procedure
Standardization of indirect bracket bonding was implemented using transfer trays and utilizing a procedure that was identical for both types of appliances (MaximumCure, Reliance Orthodontic Products, Inc., Itasca, Illinois, USA; and bonding agent ExciTE F DSC, Ivoclar Vivadent, Ellwangen, Germany) as described earlier for bonding of lingual appliances (13). Subjects received identical oral hygiene instructions following bracketing, including the advice to brush the teeth at least three times daily using a 1400–1450 ppm fluoride dentifrice.
WSL and enamel cavitation assessments
Frequencies of WSL, SBL, and cavitations were assessed prior to bracketing (Baseline, T0), as well as directly following completion of lingual MB treatment (de-bonding, T1), using standardized digital high-resolution, top-view photographs of both the upper and the lower dental arches (D-200, AF Mikro Nikkon 105mm, Macro Speedlight SB-29; Nikon, Tokyo, Japan). In addition, photo documentation was carried out during treatment with incorporated appliances and was used to judge the exact position of bracket bases, and to distinguish between WSL adjacent to bracket bases and SBL at T1.
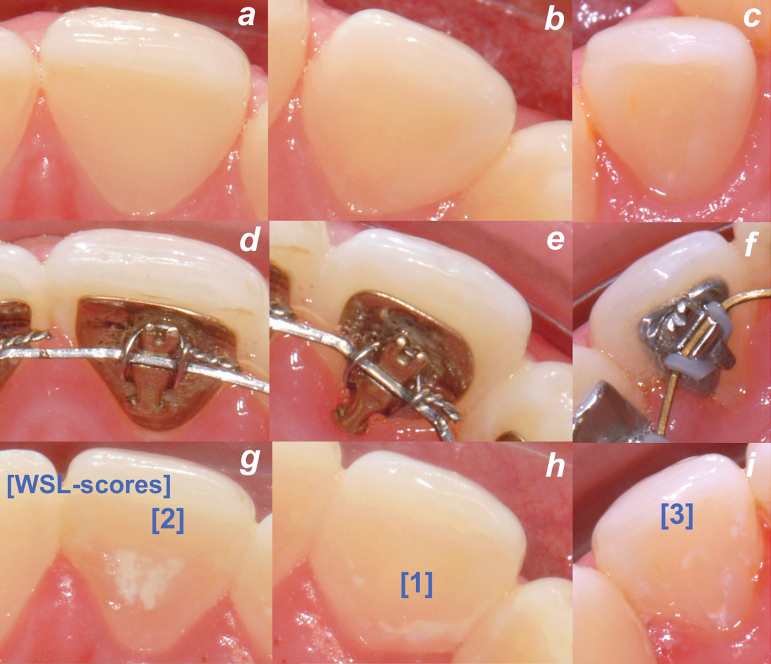
A score from 0 to 7 was used to classify WSL and cavitations adjacent to and/or beneath the bracket base (BB) area: [0], sound enamel; [1], WSL adjacent to or [2] beneath BB; [3], combination of [1, 2]; [4], cavitation adjacent to BB; [5], cavitation beneath BB; [6], combination of [1, 5]; [7], combination of [4, 5]. See Figure 1 for examples of WSL grading.
Figure 1.
Examples of lingual white spot lesions (WSLs) and sub-bracket lesions following treatment with the Incognito (a, d, g; b, e, h) or WIN appliance (c, f, i). See text for definition of WSL grading.
A high-resolution screen was used for WSL trial assessments (VP950b; screen diameter 19″; max. resolution 1280×1024; ViewSonic, Walnut, California, USA) by enlarging each single lingual surface to full-screen size. Trial screenings of the lingual enamel surfaces were performed by one assessor (EK) who was previously trained and calibrated for WSL assessments.
Statistical and method error analysis
Analysis of WSL formation or cavitation adjacent to (score 1;3;4) and beneath the bracket bases (score 2;3;5;6;7) was descriptive and employed non-parametric ANOVA, with the main effects ‘appliance type’ (group A, WIN; group B, Incognito), ‘gender’, severity of malocclusion, and ‘grouped age’ (≤16/>16 years), and the treatment duration as covariables. Numbers of new WSLs were assessed for all teeth, including second molars. To aid comparison of our findings with those from previous research on WSL incidence following labial bracket treatment, analyses were performed separately for upper front teeth (group 12–12), and the tooth groups of maxillary and mandibular dental arches including second premolars (group 15–45), first molars (group 16–46), or complete upper and lower dental arches, including second molars (group 17–47). Forty randomly (www.random.org) selected trial participants were used to calculate inter- and intra-operator method errors separately with reference to absolute numbers of unequal assessments, as well as in relation to deviations by trend (2071 single assessments, Table 3). The significance level was set at α = 5%. SAS version 9.3 (SAS Institute; Cary, North Carolina, USA) was used for all statistical analyses.
Table 3.
Proportions of inter-operator and intra-operator deviations were calculated separately with reference to absolute numbers of unequal assessments, as well as in relation to deviations by trend.
| Time point | Subjects (n) | Unequal lesion classifications / valid teeth n (%) | Unequal lesion classifications by trend / valid teeth n (%) | ||
|---|---|---|---|---|---|
| Inter-operator error | Intra-operator error | Inter-operator error | Intra-operator error | ||
| Baseline [T0] | 40 | 25 / 1035 (2.4%) | 9 / 1039 (0.9%) | 21 / 1035 (2.0%) | 8 / 1039 (0.8%) |
| De-bonding [T1] | 40 | 86 / 1036 (8.3%) | 49 / 1032 (4.8%) | 68 / 1036 (6.6%) | 37 / 1032 (3.6%) |
| All [T0 + T1] |
80 | 111 / 2071 (5.4%) | 58 / 2071 (2.8%) | 89 / 2071 (4.3%) | 45 / 2071 (2.2%) |
In case of deviations by trend, an agreement was seen if changes in enamel decalcifications were detected at all, regardless of the score 1–7, or not. All teeth from 40 randomly selected subjects (2071 single assessments) were re-assessed at both time points T0 and T1.
Results
Details of the sample characteristics and significance of differences for treatment duration, age, and gender distribution are given in Table 1. At baseline, no significant differences in pre-existing WSL (scores unequal to 0) were found between the two appliance types. Despite a significant difference in relation to treatment duration in the two groups of severity of malocclusion (S1, S2; unpaired t-test, P < 0.0001), there were separate significant effects by appliance type on treatment duration, independent of the factor treatment complexity or severity of malocclusion (Table 4). Treatment duration had a significant impact on WSL and SBL formation in all tooth groups (Table 5). SBL formation is significantly increased in pre-adolescents (≤16 years) compared with adolescents (>16 years), and it increased significantly in subjects treated with the Incognito appliance (Tables 5 and 6). Moreover, there were additional significant gender and age effects on enamel decalcification (Tables 5 and 6). Further details regarding subject- and tooth-related incidences of sub-bracket lesions and WSL adjacent to bracket bases are given in Table 7, separately for the two appliances and distinctive tooth groups (12–22; 15–45; 16–46; 17–47).
Table 4.
Treatment duration segregated by severity of malocclusion and appliance.
| Severity of malocclusion | Appliance (group) | N (%) | Treatment duration (month), Mean [SD] | Min | Max | Median | P-value |
|---|---|---|---|---|---|---|---|
| S1 | A | 364 (92.62%) | 20.64 [7.12] | 3.68 | 40.48 | 19.84 | 0.001 |
| B | 181 (76.37%) | 22.75 [7.33] | 3.25 | 41.89 | 22.14 | ||
| S2 | A | 29 (7.38%) | 26.09 [7.93] | 11.97 | 41.40 | 25.99 | 0.003 |
| B | 56 (23.63%) | 31.06 [6.65] | 16.01 | 44.39 | 31.93 | ||
| All groups | 630 | 22.42 [7.77] | 3.25 | 44.39 | 21.38 |
A chi-square-test indicates significantly (P < 0.0001) higher proportions of treatment complexities judged as ‘severe’ (S2) for Incognito. Therefore, the factor‚ ‘severity of malocclusion’ was included in the ANOVA as a main factor. Accordingly, there was a significant difference in treatment duration between the appliance types (A, WIN; B, Incognito), in both classifications S1 and S2, independent of the classification of treatment complexities.
Table 5.
Subject- and teeth-related white spot lesion (WSL) and sub-bracket lesion (SBL) formation in the specific tooth groups.
| Effect | Score changes from 0 to | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1;4) | (1;3;4) | (2;3;5;6;7) | (1;2;3;4;5;6;7) | ||||||||||||||
| Pr > F | Pr > F | Pr > F | Pr > F | ||||||||||||||
| Tooth group: | 12–22 | 15–45 | 16–46 | 17–47 | 12–22 | 15–45 | 16–46 | 17–47 | 12–22 | 15–45 | 16–46 | 17–47 | 12–22 | 15–45 | 16–46 | 17–47 | |
| Type of appliance (group A; B) | 0.86 | 0.35 | 0.42 | 0.18 | 0.46 | 0.23 | 0.29 | 0.07 | <0.0001 | 0.015 | 0.006 | <0.0001 | 0.01 | 0.014 | 0.012 | <0.0001 | |
| Severity of malocclusion (S1; S2) | 0.22 | 0.85 | 0.77 | 0.74 | 0.29 | 0.72 | 0.64 | 0.48 | 0.64 | 0.99 | 0.81 | 0.85 | 0.34 | 0.73 | 0.78 | 0.83 | |
| Appliance × Severity | 0.38 | 0.2 | 0.31 | 0.63 | 0.42 | 0.25 | 0.39 | 0.66 | 0.048 | 0.53 | 0.22 | 0.09 | 0.77 | 0.81 | 0.72 | 0.23 | |
| Gender (m; f) | 0.005 | 0.002 | 0.001 | 0.023 | 0.013 | 0.003 | 0.002 | 0.04 | 0.34 | 0.001 | 0.004 | 0.04 | 0.02 | 0.0005 | 0.001 | 0.03 | |
| Appliance × Gender | 0.73 | 0.87 | 0.8 | 0.61 | 0.94 | 0.89 | 0.96 | 0.48 | 0.61 | 0.87 | 0.81 | 0.94 | 0.97 | 0.9 | 0.78 | 0.65 | |
| Severity × Gender | 0.009 | 0.006 | 0.005 | 0.026 | 0.046 | 0.021 | 0.017 | 0.026 | 0.92 | 0.52 | 0.62 | 0.74 | 0.13 | 0.08 | 0.11 | 0.35 | |
| Appliance × Severity × Gender | 0.86 | 0.93 | 0.83 | 0.78 | 0.52 | 0.87 | 0.99 | 0.83 | 0.71 | 0.44 | 0.36 | 0.7 | 0.57 | 0.52 | 0.44 | 0.45 | |
| Grouped age (≤16 / >16 Y) | 0.71 | 0.33 | 0.26 | 0.14 | 0.49 | 0.16 | 0.12 | 0.035 | <0.0001 | 0.003 | 0.004 | 0.003 | 0.01 | 0.002 | 0.002 | 0.0003 | |
| Appliance × Age | 0.2 | 0.31 | 0.26 | 0.21 | 0.12 | 0.16 | 0.13 | 0.08 | 0.0003 | <0.0001 | 0.0003 | 0.002 | 0.001 | 0.007 | 0.01 | 0.006 | |
| Severity × Age | 0.24 | 0.32 | 0.37 | 0.59 | 0.44 | 0.37 | 0.42 | 0.63 | 0.08 | 0.18 | 0.35 | 0.62 | 0.95 | 0.75 | 0.99 | 0.73 | |
| Appliance × Severity × Age | 0.91 | 0.54 | 0.73 | 0.76 | 0.76 | 0.7 | 0.92 | 0.53 | 0.03 | 0.01 | 0.01 | 0.004 | 0.25 | 0.59 | 0.49 | 0.046 | |
| Gender × Age | 0.65 | 0.80 | 0.60 | 0.72 | 0.35 | 0.94 | 0.72 | 0.76 | 0.63 | 0.93 | 0.58 | 0.67 | 0.51 | 0.91 | 0.6 | 0.81 | |
| Appliance × Gender × Age | 0.16 | 0.32 | 0.3 | 0.46 | 0.46 | 0.54 | 0.51 | 0.55 | 0.9 | 0.26 | 0.11 | 0.51 | 0.5 | 0.58 | 0.38 | 0.82 | |
| Severity × Gender × Age | 0.42 | 0.96 | 0.99 | 0.5 | 0.36 | 0.76 | 0.79 | 0.52 | 0.2 | 0.3 | 0.13 | 0.61 | 0.78 | 0.54 | 0.36 | 0.83 | |
| Appliance × Severity × Gender × Age | 0.1 | 0.26 | 0.18 | 0.43 | 0.16 | 0.35 | 0.23 | 0.42 | 0.18 | 0.09 | 0.04 | 0.32 | 0.1 | 0.32 | 0.15 | 0.64 | |
| Treatment duration | 0.12 | 0.001 | 0.0002 | 0.0004 | 0.05 | <0.0001 | <0.0001 | <0.0001 | 0.049 | 0.011 | 0.01 | 0.0045 | 0.015 | 0.0002 | <0.0001 | <0.0001 | |
Overview of significance of effects using non-parametric three-factorial ANOVA with the main effects‚ ‘appliance type’, ‘gender’, and ‘age group’ yielded the result of significantly smaller score-deteriorations towards WSL or cavitation beneath the bracket bases (scores 2, 3, 5, 6, 7) for group A (WIN appliance), compared with group B, while there was no significant difference in terms of WSL formation next to bracket bases (scores 1, 3, 4). Thus, the null-hypothesis of no significant difference in WSL formation following incorporation of either of two different lingual orthodontic appliances was rejected for SBL.
Table 6.
The impact of gender and grouped age on white spot lesion (WSL) formation.
| Tooth group | ||||||||
|---|---|---|---|---|---|---|---|---|
| 12–22 | 15–45 | 16–46 | 17–47 | |||||
| Effect | Males | Females | Males | Females | Males | Females | Males | Females |
| No incidence | 219 | 306 | 184 | 285 | 176 | 273 | 142 | 222 |
| Incidence | 51 | 45 | 88 | 73 | 96 | 85 | 130 | 136 |
| Incidence (%) | 18.89 | 12.82 | 32.35 | 20.39 | 35.29 | 23.74 | 47.79 | 37.99 |
| Valid (N) | 270 | 351 | 272 | 358 | 272 | 358 | 272 | 358 |
| Effect | ≤16 Y | >16 Y | ≤16 Y | >16 Y | ≤16 Y | >16 Y | ≤16 Y | >16 Y |
| No incidence | 343 | 182 | 295 | 174 | 279 | 170 | 216 | 148 |
| Incidence | 80 | 16 | 130 | 31 | 146 | 35 | 209 | 57 |
| Incidence (%) | 18.91 | 8.08 | 30.59 | 15.12 | 34.35 | 17.07 | 49.18 | 27.80 |
| Valid (N) | 423 | 198 | 425 | 205 | 425 | 205 | 425 | 205 |
Frequencies of subjects with any WSL score unequal to 0 before bracketing (T0) and following de-bonding (T1). There was a significant deteriorating effect in males and in subjects ≤16 years of age (see also Table 4).
Table 7.
Subject-related and tooth-related incidences.
| Group of teeth | Valid numbers of subjects [teeth], n | Type of appliance | WSL score changes from 0 to | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (1;4) | (1;3;4) | (2;3;5;6;7) | (1–7) | (1;4) | (1;3;4) | (2;3;5;6;7) | (1–7) | |||
| Subjects, n (%) | Subjects, n (%) | Subjects, n (%) | Subjects, n (%) | Teeth, n (%) | Teeth, n (%) | Teeth, n (%) | Teeth, n (%) | |||
| 12–22 | 386 [1464] | A | 22 (5.7%) | 23 (5.96%) | 16 (4.15%) | 37 (9.59%) | 39 (2.66%) | 42 (2.87%) | 21 (1.43%) | 60 (4.1%) |
| 15–45 | 393 [7381] | A | 40 (10.18%) | 43 (10.94%) | 42 (10.69%) | 71 (18.07%) | 75 (1.02%) | 82 (1.11%) | 56 (0.76%) | 131 (1.77%) |
| 16–46 | 393 [8872] | A | 46 (11.7%) | 50 (12.72%) | 51 (12.98%) | 86 (21.88%) | 86 (0.97%) | 94 (1.06%) | 69 (0.78%) | 155 (1.75%) |
| 17–47 | 393 [10138] | A | 59 (15.01%) | 67 (17.05%) | 96 (24.43%) | 133 (33.84%) | 116 (1.14%) | 129 (1.27%) | 145 (1.43%) | 261 (2.57%) |
| 12–22 | 235 [909] | B | 28 (11.91%) | 33 (14.04%) | 38 (16.17%) | 59 (25.11%) | 50 (5.5%) | 63 (6.93%) | 77 (8.47%) | 127 (13.97%) |
| 15–45 | 237 [4453] | B | 57 (24.05%) | 62 (26.16%) | 55 (23.21%) | 90 (37.97%) | 98 (2.2%) | 118 (2.65%) | 122 (2.74%) | 220 (4.94%) |
| 16–46 | 237 [5364] | B | 58 (24.47%) | 63 (26.58%) | 61 (25.74%) | 95 (40.08%) | 101 (1.88%) | 122 (2.27%) | 137 (2.55%) | 238 (4.44%) |
| 17–47 | 237 [6076] | B | 68 (28.69%) | 80 (33.76%) | 102 (43.04%) | 133 (56.12%) | 120 (1.97%) | 156 (2.57%) | 241 (3.97%) | 361 (5.94%) |
| 12–22 | 621 [2373] | ALL | 50 (8.05%) | 56 (9.02%) | 54 (8.7%) | 96 (15.46%) | 89 (3.75%) | 105 (4.42%) | 98 (4.13%) | 187 (7.78%) |
| 15–45 | 630 [11834] | ALL | 97 (15.4%) | 105 (16.67%) | 97 (15.4%) | 161 (25.56%) | 173 (1.46%) | 200 (1.69%) | 178 (1.5%) | 351 (2.97%) |
| 16–46 | 630 [14236] | ALL | 104 (16.51%) | 113 (17.94%) | 112 (17.78%) | 181 (28.73%) | 187 (1.31%) | 216 (1.52%) | 206 (1.45%) | 393 (2.76%) |
| 17–47 | 630 [16214] | ALL | 127 (20.16%) | 147 (23.33%) | 198 (31.43%) | 266 (42.22%) | 236 (1.46%) | 285 (1.76%) | 386 (2.38%) | 622 (3.84%) |
WSL, white spot lesion. Frequencies and percentage of subjects affected by at least one new WSL, and teeth affected by new WSL or cavitations adjacent to bracket base area (scores 1, 3, 4) and (1; 4), and sub-bracket lesions or cavitations (score changes from 0 to 2; 3; 5; 6; or 7), separate for the distinctive tooth groups (upper anterior 12–22; 15–45; 16–46; 17–47).
Discussion
The null-hypothesis of no significant difference in WSL or SBL formation following incorporation of either of two different lingual orthodontic appliances was rejected for SBL formation. Therefore, the choice of lingual appliance has a significant and clinically relevant impact on formation of sub-bracket lesions (the score changes from 0 to 2;3;5;6;7), whereas frequencies of WSL next to brackets (scores 1, 3, and 4) were not significantly affected (Table 7).
The relevance of patient- and treatment-related variables such as gender, the subject’s age, or the initial degree of severity of malocclusions on the incidence and severity of WSL or SBL formation was also investigated. There were no significant differences in the distribution of age groups or gender between the two types of appliances (Table 1). WSL incidence in trial subjects ≤16 and >16 years of age were analyzed separately, as there is evidence of increased caries susceptibility in pre-adolescents (9). In agreement with previous findings reported in the literature, in our study a subject’s adolescence (≤16 years) increased significantly the risk of developing SBL, as did the treatment of males’ compared with females’ WSL (15, 16).
In accordance with the evidence stemming from systematic reviews (14) and previous incidence studies (15, 17), we found that treatment duration in our trial had a significant detrimental effect on lesions adjacent to bracket bases and also on sub-bracket lesions. In order to segregate the effect of treatment complexity or severity of malocclusion from other patient-related characteristics, a decision was made to allocate the subjects to groups with either easy to moderate, or severe treatment complexity on the basis of criteria that are known to prolong treatment duration significantly, at the evidence level of systematic reviews (14). As a result, we detected a significant difference in treatment duration between the appliance types, with shorter treatment durations in group A, in both the S1 and S2 categories, independent of the classification of treatment complexities (Table 4).
The phenomenon of SBL has rarely been described in the literature (13). Lingual or palatal enamel curvatures display much more pronounced inter-individual inconsistencies of shape, when compared with the relatively consistent buccal enamel curvatures which calls for a customization of lingual bracket bases (1, 18). Lingual bracket bonding is normally accomplished using very thin layers of bonding materials at the bracket base/enamel interface (13). The better and more congruent the shape of the bracket base to the lingual enamel surface, the thinner is the bonding layer between bracket base and enamel surface, and the higher the accuracy of lingual bracket fit. In relation to prevention of lingual WSL or cavitations beneath the bracket bases, appliance used in subjects of group A performed significantly better than did that used in group B, which may have been the result of a better fit of the bracket bases, in combination with the effect of significantly shorter mean treatment duration mainly because of a more straight forward finishing phase, with smaller numbers of finishing bends compared to the Incognito appliance.
Incidence of decalcification: lingual versus labial enamel sites
With a sample size of 630 subjects, this is—to the best of our knowledge—the largest report on WSL formation and incidence of enamel cavitation following lingual orthodontic treatment. Not only does it exceed previous reports on lingual MB-induced WSL by far (12, 13), but it is also at least on a par with the larger studies of the more common labial WSL in terms of sample size (4, 15, 19). Compared with data from previous reports on the incidence of decalcification or cavitation following conventional labial appliances, frequencies of lingual incipient caries lesions were distinctively reduced: Enaia et al. (4) reported a subject-related incidence of 60.9% for the group of upper incisors, and a teeth-related incidence of 57.4%, of which most patients (63.3%) had mild lesions, but the others were severely affected with (26.9%) and without (9.9%) cavitations. For the same tooth group, we found a subject-related incidence of 9.59% [25.11%] for group A [group B], and teeth-related incidences of 4.1% [13.97%], respectively. This indicates that subject-related incidences were reduced by the factor 6.35 [2.43], while teeth-related WSL incidences were even 14 times less for group A, or more than four times for group B.
Considering complete dental arches including first molars, as are usually considered in WSL incidence studies, a subject-related incidence of 72.9% (teeth-related: 17.3%) has been reported in the literature, and this incidence is 2.3% for cavitated lesions (19). In contrast, we found subject-related incidences which were reduced by a factor of 3.3, or [1.8] times for group A [group B] (21.88% [40.08%]), and the same comparison yielded a tooth-related incidence that was almost ten [group B: almost four] times less following lingual treatment (1.75% group A [4.44% group B], Table 7).
Quite frequently, studies on WSL incidences have not included an assessment of second molars, and this may be attributed to both the fact that second molars are inconsistently considered in fixed orthodontic treatment and also to those WSL screenings being mostly performed on the basis of standard photo documentation in which second molars are often not clearly visible. To complete the picture of lingual orthodontic WSL incidences, we found a global 17–47 WSL incidence in 2.57% [5.94%] of WIN [Incognito] treated teeth, or 33.84% [43.04%] of subjects (Table 7).
While labial-side WSL are often not noticed by patients during MB treatment, they become a matter of concern following de-bonding. The use of lingual appliances instead of conventional labial appliances not only reduces frequencies of enamel decalcifications but, as an obvious additional advantage, lingual WSL does not compromise the esthetics of smiling.
Study limitations
In comparison to the chair-side assessments during orthodontic office hours, the advantages of the method of screening top-view photographies for assessing the incidence of lingual enamel decalcifications includes the possibility of generating higher sample sizes. Also, more diligent evaluations using high-resolution screens and magnification are feasible, and the option of assessing both inter- and intra-operator method error adds to the validity of the approach. On the other hand, the method of screening dental photographs has a limitation in that in some cases of highly inclined single teeth some single areas may not be fully visible, and therefore could not be judged. Any surface that was not visible at either of the assessment time points was excluded for both time points, no matter whether it was visible on the other time point (Table 2).
A higher number of subjects was available for group A, compared with group B. This was due to a consistent change of the appliance system in November, 2011: Patients have been consecutively allocated to Incognito treatment (group B) until November 2011, and to WIN treatment (group A) since then. However, the sample sizes of completed cases have been abundant for both groups, and an effect on the results in terms of frequencies of decalcifications can be excluded. In addition, the applied statistical methods are able to handle unequal sample sizes.
This trial did not consider the number of bracket failures, with subsequent need for a rebonding, and its potential impact on a local increase or decrease of enamel decalcification.
Conclusions
Based on the findings of this study, we draw the following conclusions:
1. The incidence of sub-bracket lesions in subjects treated with the WIN appliance is significantly decreased in a clinically relevant manner compared to Incognito-treated cases, whereas frequencies of WSL adjacent to brackets were not significantly affected by the type of appliance.
2. Compared with previous reports on the subject-related incidence of decalcification or cavitation following conventional labial appliances, frequencies of lingual decalcification in subjects of group A [group B] were distinctively reduced, by about 6.35 [2.43] times, in upper incisors (incidence: 9.59% [25.11]), or 3.3 [1.8] times (incidence 21.88% [40.08%]) for a consideration of complete dental arches including first molars (teeth 16–46).
3. In terms of percentages of WSL-affected teeth (teeth-related incidence), there is a reduction by the factor of 14 [4] for the tooth group of upper incisors in group A [B], and this reduction was almost ten [group B: almost four] times for tooth group 16–46 following lingual compared to labial MB treatment.
4. The use of lingual appliances instead of conventional labial appliances is advocated, in order to achieve a reduction in frequency of enamel decalcifications in MB patients.
References
- 1. Andrews L.F. (1976) The straight-wire appliance, origin, controversy, commentary. Journal of Clinical Orthodontics, 10, 99–114. [PubMed] [Google Scholar]
- 2. Segal G.R. Schiffman P.H. and Tuncay O.C (2004) Meta analysis of the treatment-related factors of external apical root resorption. Orthodontics & Craniofacial Research, 7, 71–78. [DOI] [PubMed] [Google Scholar]
- 3. Wiechmann D. Rummel V. Thalheim A. Simon J.S. and Wiechmann L (2003) Customized brackets and archwires for lingual orthodontic treatment. American Journal of Orthodontics and Dentofacial Orthopedics, 124, 593–599. [DOI] [PubMed] [Google Scholar]
- 4. Enaia M. Bock N. and Ruf S (2011) White-spot lesions during multibracket appliance treatment: a challenge for clinical excellence. American Journal of Orthodontics and Dentofacial Orthopedics, 140, e17–e24. [DOI] [PubMed] [Google Scholar]
- 5. Tufekci E. Dixon J.S. Gunsolley J.C. and Lindauer S.J (2011) Prevalence of white spot lesions during orthodontic treatment with fixed appliances. The Angle Orthodontist, 81, 206–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fejerskov O. Nyvad B. and Kidd E.A.M (2003) Clinical and histological manifestations of dental caries. In Fejerskov O. and Kidd E.A.M (eds.), Dental Caries—The Disease and Its Clinical Management. Blackwell Munksgaard, Ames, Iowa, Chapter 5, pp. 72–97. [Google Scholar]
- 7. Benson P.E. Parkin N. Dyer F. Millett D.T. Furness S. and Germain P (2013) Fluorides for the prevention of early tooth decay (demineralised white lesions) during fixed brace treatment. The Cochrane Database of Systematic Reviews, 12, CD003809. [DOI] [PubMed] [Google Scholar]
- 8. Heymann G.C. and Grauer D (2013) A contemporary review of white spot lesions in orthodontics. Journal of Esthetic and Restorative Dentistry, 25, 85–95. [DOI] [PubMed] [Google Scholar]
- 9. Chapman J.A. Roberts W.E. Eckert G.J. Kula K.S. and González-Cabezas C (2010) Risk factors for incidence and severity of white spot lesions during treatment with fixed orthodontic appliances. American Journal of Orthodontics and Dentofacial Orthopedics, 138, 188–194. [DOI] [PubMed] [Google Scholar]
- 10. Bardow A. Nyvad B. and Nauntofte B (2001) Relationships between medication intake, complaints of dry mouth, salivary flow rate and composition, and the rate of tooth demineralization in situ. Archives of Oral Biology, 46, 413–423. [DOI] [PubMed] [Google Scholar]
- 11. Knösel M. Eckstein A. and Helms H.J (2013) Durability of esthetic improvement following Icon resin infiltration of multibracket-induced white spot lesions compared with no therapy over 6 months: a single-center, split-mouth, randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics, 144, 86–96. [DOI] [PubMed] [Google Scholar]
- 12. van der Veen M.H. Attin R. Schwestka-Polly R. and Wiechmann D (2010) Caries outcomes after orthodontic treatment with fixed appliances: do lingual brackets make a difference? European Journal of Oral Sciences, 118, 298–303. [DOI] [PubMed] [Google Scholar]
- 13. Beyling F. Schwestka-Polly R. and Wiechmann D (2013) Lingual orthodontics for children and adolescents: improvement of the indirect bonding protocol. Head & Face Medicine, 9, 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mavreas D. and Athanasiou A.E (2008) Factors affecting the duration of orthodontic treatment: a systematic review. European Journal of Orthodontics, 30, 386–395. [DOI] [PubMed] [Google Scholar]
- 15. Julien K.C. Buschang P.H. and Campbell P.M (2013) Prevalence of white spot lesion formation during orthodontic treatment. The Angle Orthodontist, 83, 641–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Al Maaitah E.F. Adeyemi A.A. Higham S.M. Pender N. and Harrison J.E (2011) Factors affecting demineralization during orthodontic treatment: a post-hoc analysis of RCT recruits. American Journal of Orthodontics and Dentofacial Orthopedics, 139, 181–191. [DOI] [PubMed] [Google Scholar]
- 17. Lovrov S. Hertrich K. and Hirschfelder U (2007) Enamel demineralization during fixed orthodontic treatment—incidence and correlation to various oral-hygiene parameters. Journal of Orofacial Orthopedics, 68, 353–363. [DOI] [PubMed] [Google Scholar]
- 18. Knösel M. Jung K. Gripp-Rudolph L. Attin T. Attin R. Sadat-Khonsari R. Kubein-Meesenburg D. and Bauss O (2009) Changes in incisor third-order inclination resulting from vertical variation in lingual bracket placement. The Angle Orthodontist, 79, 747–754. [DOI] [PubMed] [Google Scholar]
- 19. Richter A.E. Arruda A.O. Peters M.C. and Sohn W (2011) Incidence of caries lesions among patients treated with comprehensive orthodontics. American Journal of Orthodontics and Dentofacial Orthopedics, 139, 657–664. [DOI] [PubMed] [Google Scholar]
- 20. Lossdörfer S. Bieber C. Schwestka-Polly R. and Wiechmann D (2014) Analysis of the torque capacity of a completely customized lingual appliance of the next generation. Head & Face Medicine, 10, 4. [DOI] [PMC free article] [PubMed] [Google Scholar]