Abstract
Valgus knee alignment in excess of physiological valgus leads to excessive loading of the lateral compartment, which can potentially increase the risk of osteoarthritis and can place the medial knee structures at risk of chronic attenuation. Varus-producing distal femoral osteotomies have been proposed for correction of valgus malalignment, to relieve tension on medial-sided structures, as well as to off-load the lateral compartment. Understanding that symptomatic valgus deformity of the knee represents a complex problem that is magnified in the setting of lateral compartment arthritis or medial ligamentous incompetence, we present our preferred technique for a varus-producing distal femoral osteotomy using plate osteosynthesis and cancellous bone allograft.
Alignment deformities in the lower extremity affect joint loading and can be a significant cause of morbidity. Whereas varus deformity at the knee is more common, valgus deformity at the knee can be idiopathic or can arise from previous fracture with malunion, metabolic disorders, osteoarthritis, rheumatoid arthritis, rickets, polio, or other metabolic diseases.1 In these cases, valgus knee alignment in excess of physiological valgus (5° to 8°) leads to excessive loading of the lateral compartment, which can potentially increase the risk of osteoarthritis progression and can place the medial knee structures at risk of chronic attenuation.2
With valgus deformities at the knee, the joint line often slopes from superolaterally to inferomedially in the coronal plane, and the resultant deformity resides largely on the femoral side. Because of this, proximal tibial osteotomy is less successful in the management of valgus knees because of the tendency to create an oblique joint line in this setting. This was reinforced by Coventry,3 who showed poor results after proximal tibial osteotomy in patients with valgus deformity in comparison with those with varus deformity. Because of this, varus-producing distal femoral osteotomies (DFOs) are widely accepted to treat lateral compartment overload or isolated osteoarthritis, especially if the deformity is greater than 12° of valgus.2, 3, 4
Recently, the indications for varus-producing DFOs have expanded to include the treatment of valgus malalignment in the setting of central or medial ligamentous instability or incompetence.5, 6, 7, 8, 9, 10, 11, 12, 13, 14 This is of particular importance and utility because several authors have also reported that healing of both the native and reconstructed medial collateral ligament (MCL) is impaired with persistent valgus deformity at the knee.6 For this reason, many surgeons now choose to perform a DFO to correct the valgus deformity at the knee not only in the setting of isolated lateral compartment pathology but also in the setting of medial ligamentous incompetence.5, 6, 15
Although several techniques have been described, our preferred technique for unloading the lateral compartment, as well as for managing valgus malalignment in the setting of medial ligamentous incompetence, is a varus-producing lateral opening-wedge DFO. The purpose of this technical note is to describe our DFO technique using plate internal fixation with adjunctive bone allograft.
Surgical Technique
Objective Diagnosis
All patients should be evaluated with radiographs, including anteroposterior, lateral, and 45° patellar axial views, as well as a long double-leg standing anteroposterior alignment radiograph. To determine the mechanical axis, a straight line is drawn from the center of the femoral head to the center of the talar dome (Fig 1). The preoperative mechanical axis should be calculated as a percentage across the tibial plateau with the medial edge considered 0% and the lateral 100%. Valgus malalignment is identified when the mechanical axis lies lateral to the tip of the lateral tibial eminence or more than 56% across the tibial plateau in the coronal plane.16
Fig 1.
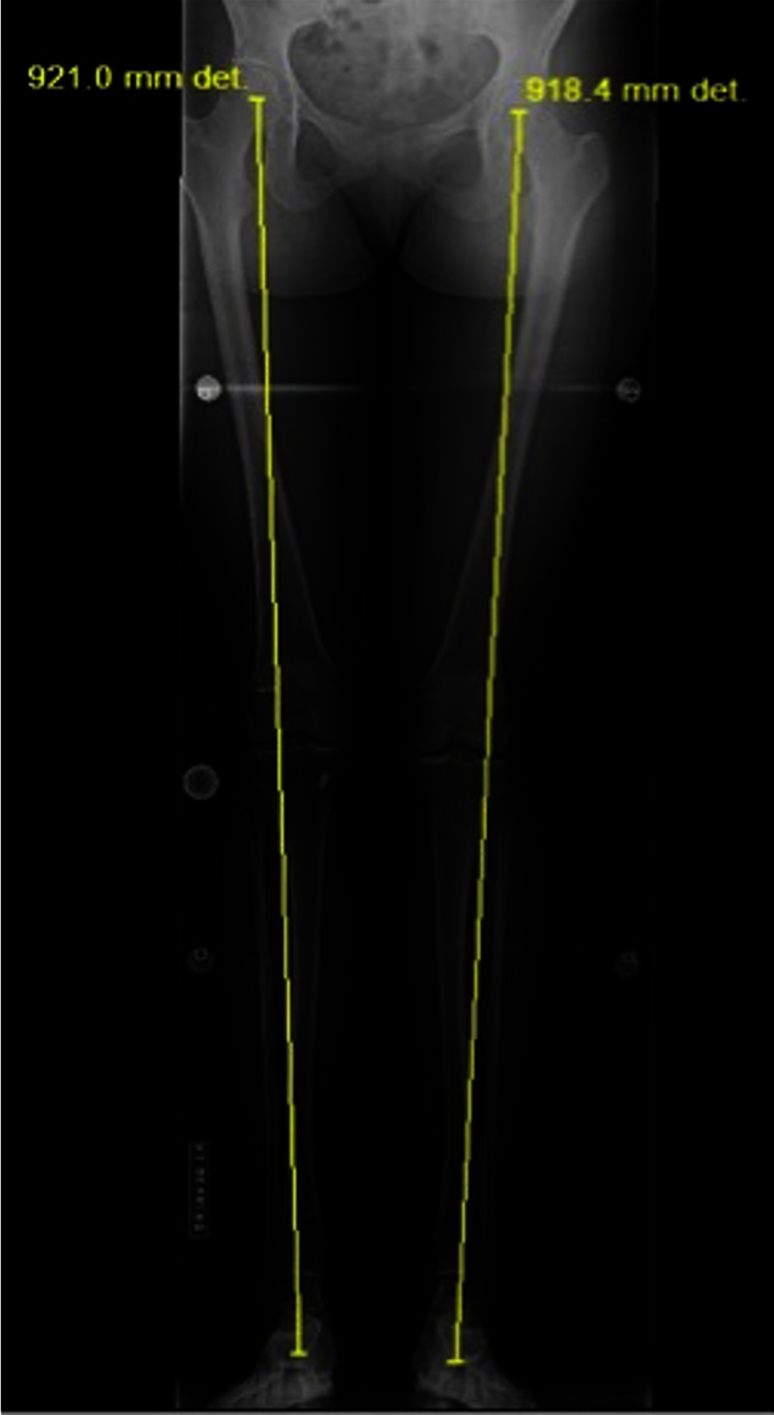
Standing anteroposterior alignment film of the bilateral lower extremities. A line drawn from the center of the femoral head to the center of the talar dome reveals medial translation of the mechanical axis, consistent with valgus malalignment of both knees. (“det” is a computer-generated mark and has no meaning.)
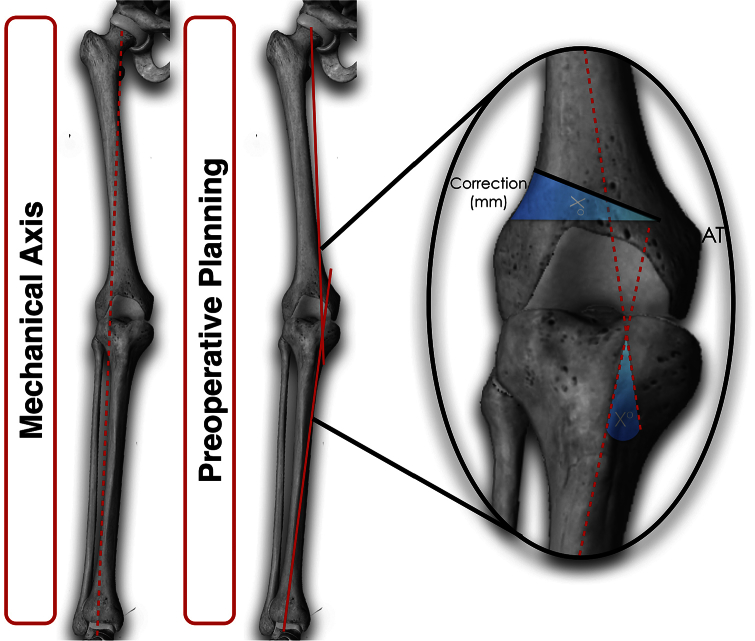
Preoperative planning aims to restore the mechanical axis through the apex of the medial tibial eminence (41%).16 To calculate the desired angle of correction, a line is drawn from the center of the femoral head through the apex of the medial tibial eminence. Next, a line is drawn from the center of the talar dome through the same point on the tibia. The angle formed by the intersection of these 2 lines provides the necessary osteotomy correction angle. The obtained angle is transposed and starts at the location of the most medial cut of the planned osteotomy (aimed toward the adductor tubercle) on the distal aspect of the medial femur and expanded to the lateral distal femur. This calculated angulation creates a triangle with the height (in millimeters) at the lateral cortex representing the amount of correction required for the osteotomy (Fig 2). The osteotomy should leave 1 cm of the medial cortex intact to avoid medial cortex fracture.
Fig 2.
Methodology by which varus correction can be made using preoperative radiographs. The angle of correction is determined by an angle created by the crossing of lines drawn through the anatomic axes of the femur and of the tibia. This angle is then transposed to the lateral aspect of the femur. Of note, 1 cm of the medial cortex should be left intact while the surgeon is performing the osteotomy to avoid medial cortex fracture. (AT, adductor tubercle.)
Varus-Producing DFO Indications
Indications for a varus opening-wedge DFO are valgus deformity with isolated lateral compartment osteoarthritis in young active patients. In addition, this procedure is indicated in patients with valgus deformity of the knee and concurrent symptomatic MCL incompetence. A tibial osteotomy is sometimes necessary instead of a DFO when there is anterior cruciate ligament (ACL) insufficiency with an abnormally steep sagittal-plane tibial slope or, conversely, when there is posterior cruciate ligament insufficiency with an abnormally flat sagittal-plane tibial slope. Contraindications to the procedure include inflammatory arthritis, flexion contracture of greater than 15°, knee flexion of less than 90°, fixed valgus deformity of greater than 20°, and arthritis in the medial or patellofemoral compartments.1, 7, 9
Patient Positioning and Anesthesia
The patient is placed in the supine position on the operating table, and general anesthesia is used for induction. A well-padded high-thigh tourniquet (Zimmer, Warsaw, IN) is placed on the operative leg, and a bump is then placed under the knee so that it rests at approximately 30° of flexion. The contralateral leg is secured to the table in full extension with a pneumatic compression device to help prevent deep venous thrombosis. Examination under anesthesia is performed to evaluate the cruciate and collateral ligaments, as well as to assess range of motion.
Surgical Approach
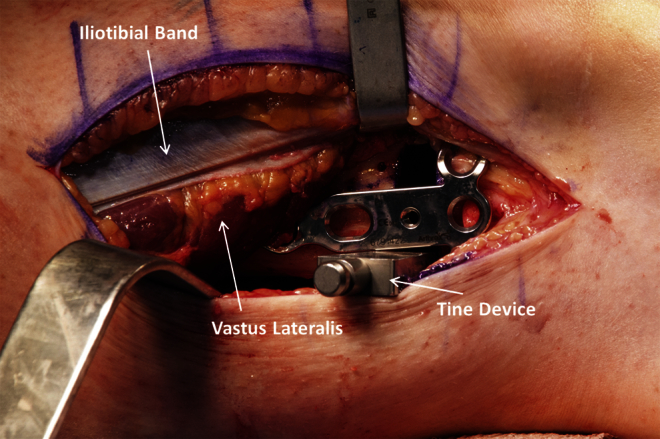
A 4- to 6-cm midaxial skin incision is made along the axis of the iliotibial band (ITB) on the distal lateral aspect of the leg overlying the distal femur. Subcutaneous dissection is performed to reveal the underlying ITB, which is incised along the length of its fibers (Fig 3). This exposes the vastus lateralis muscle, and care is taken to gently separate this muscle from the overlying ITB with a Cobb elevator (V. Mueller, San Diego, CA). Subperiosteal dissection and elevation of the vastus lateralis are then performed, with care taken to avoid damage to the muscular fibers. The Cobb elevator is further used to continue blunt subperiosteal dissection such that the anterior and posterior aspects of the distal femoral diaphysis and metadiaphyseal flare are exposed. Blunt retractors are then placed anteriorly underneath the quadriceps tendon and posteriorly above the hamstring musculature to protect the neurovascular structures. A radiolucent retractor is used to protect the neurovascular structures posteriorly and for later ease of visualization under fluoroscopy.
Fig 3.
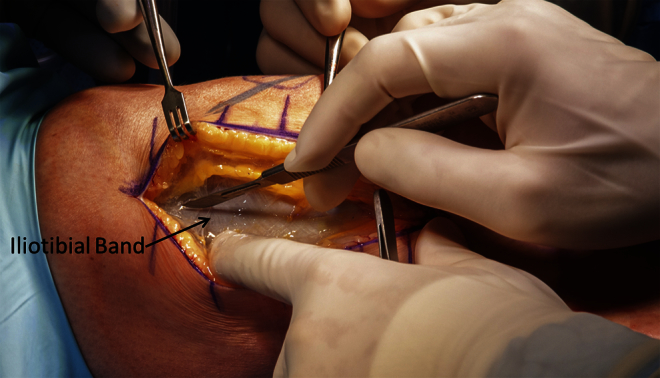
Intraoperative photograph of a right lower extremity with the patient in the supine position showing dissection of the subcutaneous tissues to the level of the iliotibial band. This structure is then incised along the length of its fibers to reveal the underlying vastus lateralis muscle.
After dissection and exposure of the distal femur, radiographs are obtained to assist in planning the trajectory of the osteotomy. A guide pin (Arthrex, Naples, FL) is inserted into the lateral femoral cortex and advanced until it contacts the medial cortex and is left in place. An osteotomy guide (Arthrex) is then assembled over the top of the guide pin (Fig 4). The osteotomy guide is adjusted until the desired angle is achieved, at which point a second guide pin is inserted to secure the osteotomy guide. The guide pins may be left intact or broken away to allow later ease of passage for the saw and osteotomy tools.
Fig 4.
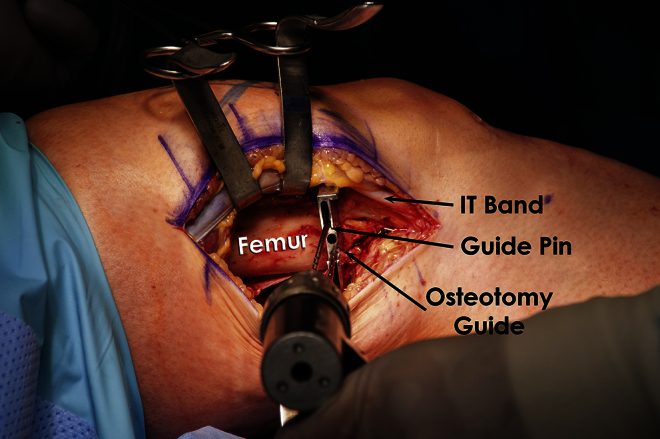
Intraoperative photograph of a right lower extremity showing placement of guide pins in the lateral femoral cortex and the assembled osteotomy guide over these pins to guide the distal femoral osteotomy. (IT, iliotibial.)
Care is taken to ensure appropriate positioning of both the anterior and posterior retractors. A reciprocating saw (ConMed, Utica, NY) is placed along the border of the osteotomy cutting guide and used to breach the lateral femoral cortex (Fig 5). The saw and guidewires are removed, and under fluoroscopic guidance, an osteotome is advanced from laterally to medially to complete the osteotomy (Fig 6). It is important to leave intact a medial cortical hinge of 1 to 2 cm. Care must be taken at this step to ensure release of both the anterior and posterior cortices while protecting the surrounding soft tissues with blunt retractors (Arthrex).
Fig 5.
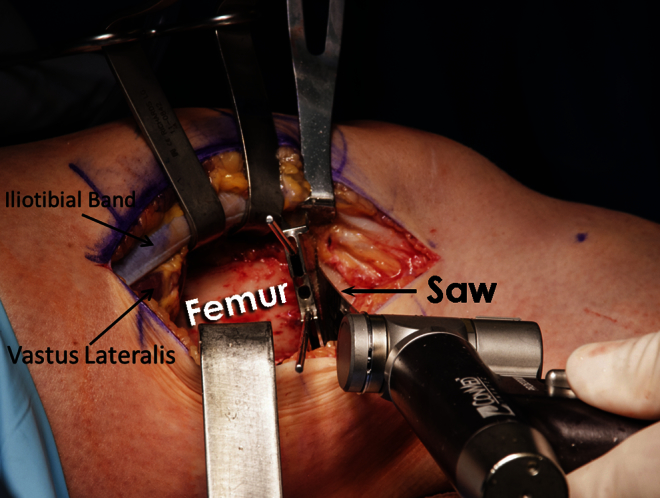
Intraoperative photograph of a right lower extremity with the patient in the supine position. A reciprocating saw is placed within the osteotomy guide to begin the distal femoral osteotomy on the right lower extremity. As shown in this image, care is taken to protect the surrounding soft tissues.
Fig 6.

Intraoperative fluoroscopic image of a right knee showing the beginning of a distal femoral osteotomy through the lateral cortex of the femur with advancement of a osteotome within the bone, leaving the medial cortex intact.
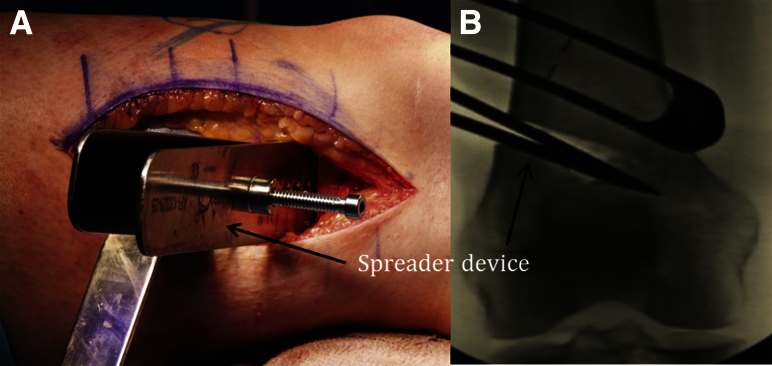
To begin the varus osteotomy correction, a spreading device (Arthrex) is inserted into the osteotomy tract and slowly and carefully expanded until the desired amount of correction is achieved (Fig 7). Two blunt angled tines (Arthrex) are then assembled onto a handled impactor (Arthrex) and placed into the expanded lateral cortical defect. With careful mallet impaction, the tines are advanced into the osteotomy defect until the desired angular correction is achieved. This correction should be performed in a slow and controlled fashion to avoid fracture propagation and to allow for plastic deformation of the medial cortex. Many systems have markings on the tines to help the surgeon observe the amount of angular correction achieved as the tines are advanced. Under fluoroscopic image intensification, correction to a neutral axis can be confirmed either with a leg alignment rod or with use of a radiopaque string or cable (Fig 7).
Fig 7.
Intraoperative (A) and fluoroscopic (B) images of proper placement and expansion of a blunt spreading device within the previously created defect in the lateral cortex of the right distal femur with the patient in the supine position on the radiolucent bed.
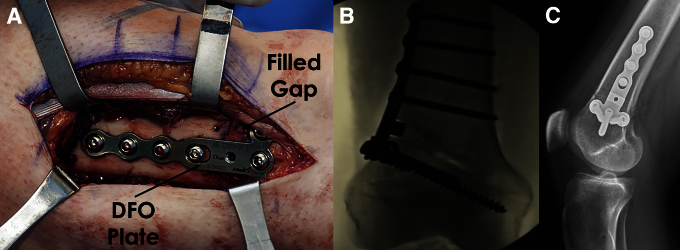
After correction is confirmed, a lateral femoral plate with a predetermined spacer matching the desired correction is chosen for fixation of the osteotomy. The plate may be precontoured using plate benders to match the anatomy of the femur (Fig 8).
Fig 8.
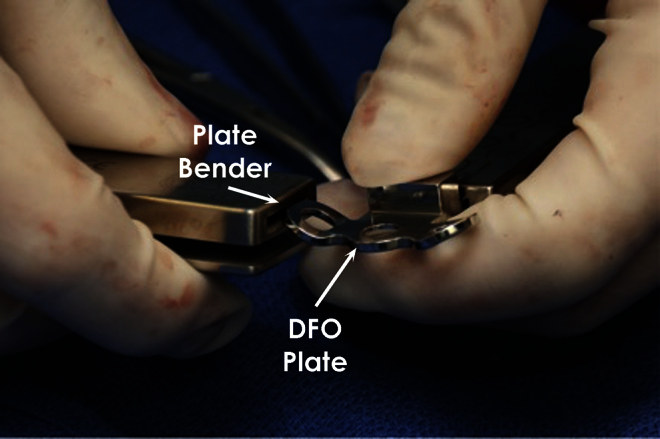
Intraoperative image showing the appropriate technique for contouring the distal femoral plate for placement on the lateral aspect of the distal femur. (DFO, distal femoral osteotomy.)
The handle is removed from the tines, and a small amount of bone graft may be inserted through the tines to assist with maintaining desired angulation. A single tine may then be removed to allow for ease of plate application (Fig 9). Alternatively, the lateral femoral plate may be placed centrally on the femur between the tines and provisionally secured in place proximally with a fully threaded bicortical nonlocking screw (Synthes, West Chester, PA). Regardless of the technique chosen, the plate is applied and secured in place proximally with three to four 4.5-mm fully threaded bicortical nonlocking screws (Synthes) and distally with three 6.5-mm fully threaded cancellous screws (Synthes). Fluoroscopic imaging should be used to ensure that the distal screws do not violate the posterior femoral fossa or the trochlea anteriorly. A finger can be used to palpate these regions to further confirm that the screws are maintained within bone.
Fig 9.
Expansion of the distal femoral cortical defect in a right femur with a single tine to allow for ease of placement of the distal femoral plate (with patient in supine position).
Bone graft is then placed into the osteotomy bone void around the plate. Precontoured wedges may be used; however, our preferred method is placement of cancellous demineralized bone matrix allograft (RTI Biologics, Alachua, FL) into the void (Fig 10). Final fluoroscopic images are obtained to confirm appropriate plate positioning, amount of correction, and placement of bone graft (Fig 11). The surgical wound is then cleansed with saline solution and closed in a layered fashion. Video 1 details the surgical steps in detail, Table 1 discusses the pearls and pitfalls of this surgical procedure, and Table 2 shows the advantages and disadvantages.
Fig 10.
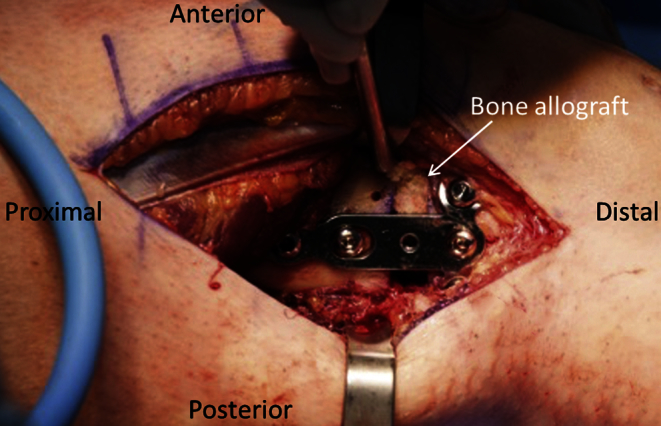
Right lateral distal femur in a supine patient with the final construct secured in place with adjunctive bone allograft within the void created by the osteotomy.
Fig 11.
Final fluoroscopic (A) and intraoperative (B) images of a right knee and distal femur showing appropriately placed fixation with the desired amount of correction. (C) Postoperative lateral radiograph showing plate placement and bone healing. (DFO, distal femoral osteotomy.)
Table 1.
Pearls and Pitfalls of Lateral Opening-Wedge DFO
| Pearls |
| In patients with valgus misalignment and central or medial ligamentous incompetence, a varus-producing DFO should be considered in conjunction with surgical ligamentous reconstruction or repair. |
| Preoperative templating is performed using full-leg standing alignment films. This allows for determination of the amount of correction required. |
| Radiolucent retractors are used to facilitate ease of visualization during intraoperative fluoroscopy. |
| The surgeon should ensure appropriate placement of retractors to protect the neurovascular structures during guide pin drilling and passage of the saw or osteotomes. |
| To provide a hinge, 1-2 cm of medial cortex should be preserved. |
| Expansion of the osteotomy site should be performed in a slow and controlled fashion to avoid fracture propagation. |
| The surgeon should ensure complete release of both anterior and posterior cortices to allow for expansion of the osteotomy site. |
| Precontouring of the distal femoral plate to fit the anatomic profile of the femur should be considered. |
| Malleable bone graft should be used to allow for complete filling of the osteotomy void. |
| A predetermined and early rehabilitation program should be started immediately after surgery to decrease the risk of arthrofibrosis and to improve range of motion. |
| Pitfalls |
| Studies have reported that performing ACL or PLC reconstruction in patients with varus malalignment leads to increased stress on the grafts and a higher chance of graft failure. Similar findings can be seen in MCL-deficient knees with valgus malalignment. |
| Poor preoperative planning can lead to under-correction or residual malalignment. |
| Failure to use a posterior retractor can result in injury to the neurovascular structures. |
| Rapid expansion of the lateral cortex or aggressive medial osteotomy can lead to fracture propagation requiring adjunctive stabilization. |
| Improper screw placement can occur within either the posterior femoral hiatus or the anterior trochlea. |
| Early weight bearing before bony healing and incorporation can destabilize the construct and lessen the amount of correction achieved. |
| Failure to achieve full range of motion within the first 4 to 6 wk after surgery can occur, leading to limitation in function. |
ACL, anterior cruciate ligament; DFO, distal femoral osteotomy; MCL, medial collateral ligament; PLC, posterolateral corner.
Table 2.
Advantages and Disadvantages of Lateral Opening-Wedge DFO
| Advantages |
| Varus-producing DFOs may be performed to treat lateral compartment overload or isolated osteoarthritis, especially if the deformity is > 12° of valgus. |
| DFO can be used to address valgus deformity at the knee in the setting of medial ligamentous incompetence. |
| Using allograft to fill the defect created by the DFO limits morbidity associated with autograft harvest. |
| Eighty percent survival rates have been reported at 10 years' follow-up, delaying the indication for a total knee replacement in some cases. |
| Disadvantages |
| The patient remains non–weight bearing for 8 wk, with an immobilizer. |
| The use of allograft introduces additional risk of disease transmission or host rejection. |
| If required in the future, arthroplasty can be more technically challenging. |
DFO, distal femoral osteotomy.
Rehabilitation
Postoperatively, the patient is to remain non–weight bearing for 8 weeks. During this time, a knee immobilizer brace (Össur, Foothill Ranch, CA) should be worn. Starting on postoperative day 1, a supervised physical therapy program is initiated, with emphasis on quadriceps activation. Quadriceps sets and straight-leg raises are to be performed 3 to 5 times daily. Passive range of motion can be initiated on day 1 postoperatively and can be increased as tolerated. After 8 weeks, weight bearing is gradually increased based on clinical and radiographic evidence of bone healing. Table 3 shows a detailed outline of our postsurgical rehabilitation protocol.
Table 3.
Distal Femoral Osteotomy Postoperative Rehabilitation Protocol
| Week |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 12 | 16 | 20 | 24 | 28 | 30 | 36 | |
| Initial exercises | |||||||||||||||||
| Flexion-extension | |||||||||||||||||
| Wall slides | ● | ● | ● | ● | ● | ● | ● | ● | |||||||||
| Seated | ● | ● | ● | ● | ● | ● | ● | ● | |||||||||
| Patellar tendon mobilization | ● | ● | ● | ● | ● | ● | ● | ● | |||||||||
| Extension mobilization | ● | ● | ● | ● | ● | ● | ● | ● | |||||||||
| Quadriceps series | ● | ● | ● | ● | ● | ● | ● | ● | |||||||||
| Hamstring sets | ● | ● | ● | ● | ● | ● | ● | ● | |||||||||
| Sit and reach for hamstrings (towel) | ● | ● | ● | ● | ● | ● | ● | ● | |||||||||
| Ankle pumps | ● | ● | ● | ● | ● | ● | ● | ● | ● | ||||||||
| Crutch weaning | ● | ● | ● | ||||||||||||||
| Toe and heel raises | ● | ● | ● | ||||||||||||||
| Balance series | ● | ● | ● | ● | ● | ||||||||||||
| Cardiovascular exercises | |||||||||||||||||
| Bike with both legs | |||||||||||||||||
| No resistance | ● | ● | ● | ||||||||||||||
| Resistance | ● | ● | ● | ● | ● | ● | |||||||||||
| Aqua jogging | ● | ● | ● | ● | ● | ● | |||||||||||
| Treadmill walking with 7% incline | ● | ● | ● | ||||||||||||||
| Swimming with fins | ● | ● | ● | ● | |||||||||||||
| Elliptical trainer | ● | ● | ● | ||||||||||||||
| Rowing | ● | ● | ● | ||||||||||||||
| Stair stepper | ● | ● | ● | ||||||||||||||
| Weight-bearing strength | |||||||||||||||||
| Double knee bends | ● | ● | ● | ||||||||||||||
| Double leg bridges | ● | ● | ● | ||||||||||||||
| Reverse lunge with static hold | ● | ● | ● | ||||||||||||||
| Beginning cord exercises | ● | ● | |||||||||||||||
| Balance squats | ● | ● | |||||||||||||||
| Single-leg dead lift | ● | ● | ● | ||||||||||||||
| Leg press | ● | ● | ● | ||||||||||||||
| Sports test exercises | ● | ● | |||||||||||||||
| Agility exercises | |||||||||||||||||
| Running progression | ● | ● | |||||||||||||||
| Initial—single plane | ● | ● | |||||||||||||||
| Advanced—multidirectional | ● | ||||||||||||||||
| Functional sports test | ● | ||||||||||||||||
| High-level activities | |||||||||||||||||
| Golf | ● | ● | |||||||||||||||
| Outdoor biking, hiking, snowshoeing | ● | ● | |||||||||||||||
| Skiing, basketball, tennis, football, soccer | ● | ||||||||||||||||
NOTE. A bullet point indicates that the patient should perform the listed exercise for that week. The range-of-motion restrictions were 0° to 90° for 2 weeks, followed by full passive range of motion. Regarding brace settings, an immobilizer was used for 8 weeks. Regarding weight-bearing status, progression to weight bearing was held until follow-up radiographic approval. The patient was non–weight bearing for 8 weeks and then progressed to one-fourth body weight per week to wean off crutches. The time lines were as follows: week 1, postoperative days 1 through 7; week 2, postoperative days 8 through 14; week 3, postoperative days 15 through 21; and week 4, postoperative days 22 through 28.
Discussion
This lateral opening-wedge DFO technique is used to correct genu valgum deformity. Although this procedure has most commonly been described for young and active patients with isolated lateral compartment osteoarthritis, it has additionally been an effective treatment for valgus malalignment with concurrent central ligamentous deficiency or valgus laxity due to MCL insufficiency.
In the past 40 years, authors have increasingly suggested the use of varus-producing DFOs in young patients with isolated lateral compartment osteoarthritis. In their sentinel article, Healy et al.1 reported on 23 patients who underwent a varus-producing DFO for isolated lateral compartment arthrosis with good to excellent results in 83% at minimum 2-year follow-up. Several authors have since reproduced excellent results using the technique of Healy et al. in appropriately selected patients with unicompartmental disease.11, 13, 17, 18
With its proven track record, the indications for this procedure have been expanding in recent years. Several authors have advocated performing a DFO in the setting of valgus deformity with associated MCL incompetence5, 6; however, there remains a paucity of literature regarding this topic. Recently, one article reported the use of lateral opening-wedge DFO to treat a patient with valgus malalignment, MCL and ACL insufficiency, and functional instability.7 The authors reported decreased medial compartment gapping immediately postoperatively with a valgus stress test.
Studies have reported that performing ACL or posterolateral corner reconstruction in patients with varus malalignment leads to increased stress on the grafts and a higher chance of graft failure.15, 19, 20 Therefore, alignment should be corrected either before or concurrently with ligament reconstruction.19, 20 We believe the same principle can be extrapolated for patients with valgus malalignment and MCL deficiency.
Recently, Hetsroni et al.7 reported that sectioning the superficial MCL resulted in statistically significantly decreased medial compartment knee opening with valgus stress in 30° of flexion after a DFO compared with superficial MCL sectioning before a DFO. Despite the statistical significance, the authors remained cautious about the clinical significance because the change in medial compartment opening was small in magnitude.
Good outcomes have been reported for varus-producing DFOs in patients with valgus malalignment,12, 21 as well as in those with congenital or developmental deformity resulting in valgus alignment and subsequent MCL laxity.5 However, to determine the long-term effectiveness of restoring alignment and medial compartment stability, high-quality studies are needed.
We believe performing a varus-producing lateral opening-wedge DFO in genu valgum patients with isolated lateral compartment arthrosis, as well as in those with MCL insufficiency, is a viable option to restore both stability and alignment. If instability remains after completion of a supervised physical therapy program along with clinical and radiologic evidence of osteotomy healing, a superficial MCL augmentation or reconstruction can be performed.
Using the distal femur as the site of osteotomy is advantageous because correction through the proximal tibia can limit or prevent appropriate correction of the joint line and can result in lateral subluxation of the tibia.22 Further, poor results have been shown in patients with valgus deformity when using a tibial-based approach.3 For this reason, varus-producing DFOs are widely accepted to treat valgus deformities with lateral compartment osteoarthritis and/or medial ligamentous incompetence. In addition, using allograft to fill the defect created by the DFO limits morbidity associated with autograft harvest and improves surgical efficiency.
It should be noted that one of the limitations of an opening-wedge DFO is that it does not allow for correction of the sagittal-plane tibial slope. Furthermore, this procedure requires extensive preoperative planning and careful surgical technique followed by postoperative restrictions on weight bearing and activity. The use of cancellous allograft also introduces a small risk of disease transmission or host rejection, and such allograft may not heal as fast as autograft bone graft. Despite these limitations, we have found this technique to be safe and reproducible and encourage other groups to test the validity of this technique and to assess for long-term results.
Footnotes
The authors report the following potential conflict of interest or source of funding: R.F.L. receives support from Arthrex; Smith & Nephew; Ossur; Health East, Norway; and an NIH R13 grant for biologics. Steadman Philippon Research Institute provided support by Arthrex, Ossur, Siemens, and Smith & Nephew.
Supplementary Data
Long-leg standing radiographs of the patient are presented to show valgus malalignment of the right knee in the coronal plane. The patient is placed supine on the operating table, and a bilateral examination under anesthesia is performed. A midaxial skin incision is made along the axis of the iliotibial band (ITB) on the distal lateral aspect of the right femur. The ITB is incised along the length of its fibers. A subvastus dissection is performed to gently separate the vastus lateralis from the overlying ITB with a Cobb elevator. The surgeon continues with subperiosteal dissection and elevation of the vastus lateralis, taking care to avoid damage to the muscular fibers. Blunt subperiosteal dissection is continued such that the anterior and posterior aspects of the distal femoral diaphysis and metadiaphyseal flare are exposed. Retractors are placed anteriorly underneath the quadriceps tendon and posteriorly above the hamstring musculature to protect the neurovascular structures. Guide pins are inserted into the lateral cortex, and an osteotomy guide is assembled. An oscillating saw is used to breach the lateral cortex, and a series of osteotomes is used to complete the cut, leaving an approximately 1- to 2-cm medial bone hinge. A spreader device is used to slowly open the osteotomy until the desired correction is achieved. The spreader device is removed, and a tine device is gently impacted until the desired correction is once again attained. Fluoroscopic images are acquired to ensure correction of the malalignment. A distal femoral plate is secured proximally with three to four 4.5-mm fully threaded bicortical nonlocking screws and distally with three 6.5-mm fully threaded cancellous screws. Malleable bone matrix allograft is then placed into the osteotomy site, and final images are obtained.
References
- 1.Healy W.L., Anglen J.O., Wasilewski S.A., Krackow K.A. Distal femoral varus osteotomy. J Bone Joint Surg Am. 1988;70:102–109. [PubMed] [Google Scholar]
- 2.Gugenheim J.J., Jr., Brinker M.R. Bone realignment with use of temporary external fixation for distal femoral valgus and varus deformities. J Bone Joint Surg Am. 2003;85:1229–1237. doi: 10.2106/00004623-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Coventry M. Proximal tibial varus osteotomy for osteoarthritis of the lateral compartment of the knee. J Bone Joint Surg Am. 1987;69:32–38. [PubMed] [Google Scholar]
- 4.McDermott A., Finklestein J., Farine I., Boynton E., MacIntosh D., Gross A. Distal femoral varus osteotomy for valgus deformity of the knee. J Bone Joint Surg Am. 1988;70:110–116. [PubMed] [Google Scholar]
- 5.Paley D., Bhatnagar J., Herzenberg J.E., Bhave A. New procedures for tightening knee collateral ligaments in conjunction with knee realignment osteotomy. Orthop Clin North Am. 1994;25:533–555. [PubMed] [Google Scholar]
- 6.Wijdicks C.A., Griffith C.J., Johansen S., Engebretsen L., LaPrade R.F. Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am. 2010;92:1266–1280. doi: 10.2106/JBJS.I.01229. [DOI] [PubMed] [Google Scholar]
- 7.Hetsroni I., Lyman S., Pearle A.D., Marx R.G. The effect of lateral opening wedge distal femoral osteotomy on medial knee opening: Clinical and biomechanical factors. Knee Surg Sports Traumatol Arthrosc. 2014;22:1659–1665. doi: 10.1007/s00167-013-2405-3. [DOI] [PubMed] [Google Scholar]
- 8.Dewilde T.R., Dauw J., Vandenneucker H., Bellemans J. Opening wedge distal femoral varus osteotomy using the Puddu plate and calcium phosphate bone cement. Knee Surg Sports Traumatol Arthrosc. 2013;21:249–254. doi: 10.1007/s00167-012-2156-6. [DOI] [PubMed] [Google Scholar]
- 9.Forkel P., Achtnich A., Metzlaff S., Zantop T., Petersen W. Midterm results following medial closed wedge distal femoral osteotomy stabilized with a locking internal fixation device. Knee Surg Sports Traumatol Arthrosc. 2015;23:2061–2067. doi: 10.1007/s00167-014-2953-1. [DOI] [PubMed] [Google Scholar]
- 10.Jacobi M., Wahl P., Bouaicha S., Jakob R.P., Gautier E. Distal femoral varus osteotomy: Problems associated with the lateral open-wedge technique. Arch Orthop Trauma Surg. 2011;131:725–728. doi: 10.1007/s00402-010-1193-1. [DOI] [PubMed] [Google Scholar]
- 11.Kosashvili Y., Safir O., Gross A., Morag G., Lakstein D., Backstein D. Distal femoral varus osteotomy for lateral osteoarthritis of the knee: A minimum ten-year follow-up. Int Orthop. 2010;34:249–254. doi: 10.1007/s00264-009-0807-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saithna A., Kundra R., Modi C.S., Getgood A., Spalding T. Distal femoral varus osteotomy for lateral compartment osteoarthritis in the valgus knee. A systematic review of the literature. Open Orthop J. 2012;6:313–319. doi: 10.2174/1874325001206010313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sternheim A., Garbedian S., Backstein D. Distal femoral varus osteotomy: Unloading the lateral compartment: Long-term follow-up of 45 medial closing wedge osteotomies. Orthopedics. 2011;34:e488–e490. doi: 10.3928/01477447-20110714-37. [DOI] [PubMed] [Google Scholar]
- 14.Thein R., Bronak S., Thein R., Haviv B. Distal femoral osteotomy for valgus arthritic knees. J Orthop Sci. 2012;17:745–749. doi: 10.1007/s00776-012-0273-1. [DOI] [PubMed] [Google Scholar]
- 15.van de Pol G.J., Arnold M.P., Verdonschot N., van Kampen A. Varus alignment leads to increased forces in the anterior cruciate ligament. Am J Sports Med. 2009;37:481–487. doi: 10.1177/0363546508326715. [DOI] [PubMed] [Google Scholar]
- 16.LaPrade R.F., Spiridonov S.I., Nystrom L.M., Jansson K.S. Prospective outcomes of young and middle-aged adults with medial compartment osteoarthritis treated with a proximal tibial opening wedge osteotomy. Arthroscopy. 2012;28:354–364. doi: 10.1016/j.arthro.2011.08.310. [DOI] [PubMed] [Google Scholar]
- 17.Drexler M., Gross A., Dwyer T. Distal femoral varus osteotomy combined with tibial plateau fresh osteochondral allograft for post-traumatic osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2015;23:1317–1323. doi: 10.1007/s00167-013-2828-x. [DOI] [PubMed] [Google Scholar]
- 18.Backstein D., Morag G., Hanna S., Safir O., Gross A. Long-term follow-up of distal femoral varus osteotomy of the knee. J Arthroplasty. 2007;22:2–6. doi: 10.1016/j.arth.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 19.Badhe N.P., Forster I.W. High tibial osteotomy in knee instability: The rationale of treatment and early results. Knee Surg Sports Traumatol Arthrosc. 2002;10:38–43. doi: 10.1007/s001670100244. [DOI] [PubMed] [Google Scholar]
- 20.Arthur A., LaPrade R.F., Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: A prospective clinical study. Am J Sports Med. 2007;35:1844–1850. doi: 10.1177/0363546507304717. [DOI] [PubMed] [Google Scholar]
- 21.Terry G.C., Cimino P.M. Distal femoral osteotomy for valgus deformity of the knee. Orthopedics. 1992;15:1283–1289. doi: 10.3928/0147-7447-19921101-07. [DOI] [PubMed] [Google Scholar]
- 22.Hanssen A.D., Stuart M.J., Scott R.D., Scuderi G.R. Surgical options for the middle-aged patient with osteoarthritis of the knee joint. Instr Course Lect. 2001;50:499–511. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Long-leg standing radiographs of the patient are presented to show valgus malalignment of the right knee in the coronal plane. The patient is placed supine on the operating table, and a bilateral examination under anesthesia is performed. A midaxial skin incision is made along the axis of the iliotibial band (ITB) on the distal lateral aspect of the right femur. The ITB is incised along the length of its fibers. A subvastus dissection is performed to gently separate the vastus lateralis from the overlying ITB with a Cobb elevator. The surgeon continues with subperiosteal dissection and elevation of the vastus lateralis, taking care to avoid damage to the muscular fibers. Blunt subperiosteal dissection is continued such that the anterior and posterior aspects of the distal femoral diaphysis and metadiaphyseal flare are exposed. Retractors are placed anteriorly underneath the quadriceps tendon and posteriorly above the hamstring musculature to protect the neurovascular structures. Guide pins are inserted into the lateral cortex, and an osteotomy guide is assembled. An oscillating saw is used to breach the lateral cortex, and a series of osteotomes is used to complete the cut, leaving an approximately 1- to 2-cm medial bone hinge. A spreader device is used to slowly open the osteotomy until the desired correction is achieved. The spreader device is removed, and a tine device is gently impacted until the desired correction is once again attained. Fluoroscopic images are acquired to ensure correction of the malalignment. A distal femoral plate is secured proximally with three to four 4.5-mm fully threaded bicortical nonlocking screws and distally with three 6.5-mm fully threaded cancellous screws. Malleable bone matrix allograft is then placed into the osteotomy site, and final images are obtained.