Abstract
Background:
Physical therapy (PT) is often prescribed for patients with rotator cuff tears. The extent to which PT influences strength, range of motion (ROM), and patient-reported outcomes has been studied extensively, but the effect of PT on in vivo joint kinematics is not well understood.
Purpose:
To assess the influence of symptomatic rotator cuff pathology and the effects of PT on shoulder motion, strength, and patient-reported outcomes.
Study Design:
Controlled laboratory study.
Methods:
Twenty-five patients with a symptomatic rotator cuff tear and 25 age-matched asymptomatic control subjects were recruited. Shoulder motion was measured using a biplane radiography imaging system, strength was assessed with a Biodex dynamometer, and patient-reported outcomes were assessed using the Western Ontario Rotator Cuff Index and visual analog scale (VAS) pain scores. Data were acquired from the patients before and after 8 weeks of physical therapy. Data were acquired at 1 time point for the control subjects.
Results:
Compared with the control subjects, patients with a symptomatic rotator cuff tear had significantly worse pain/function scores (P < .01); less ROM (P < .01); lower abduction (ABD), external rotation (ER), and internal rotation (IR) strength (P < .01); less scapulothoracic posterior tilt (P = .05); and lower glenohumeral joint elevation (P < .01). Physical therapy resulted in improved pain/function scores (P < .01), increased ROM (P < .02), increased scapulothoracic posterior tilt (P = .05), increased glenohumeral joint elevation (P = .01), and decreased acromiohumeral distance (AHD) (P = .02).
Conclusion:
Compared with age-matched controls, patients had worse pain/function scores, less ROM, and lower ABD, ER, and IR strength. Patients also had less scapulothoracic anteroposterior tilt, less glenohumeral joint elevation, and an altered glenohumeral joint contact path. PT resulted in improved pain/function scores, increased ROM, greater posterior scapulothoracic tilt, increased glenohumeral joint elevation, an increased range of superoinferior joint contact, and a lower mean AHD. Of these differences, PT only returned scapulothoracic tilt to control levels.
Clinical Relevance:
This study documents the effects of PT on shoulder motion and conventional clinical outcomes. It is expected that understanding how changes in joint motion are associated with conventional clinical outcomes will lead to improved nonoperative interventions for patients with rotator cuff tears.
Keywords: shoulder, rotator cuff, biomechanics of tendon, motion analysis/kinesiology, physical therapy/rehabilitation
Rotator cuff tears are common, affecting about 40% (or more) of individuals older than 60 years26,41,55 and accounting for an economic burden of $3 to $5 billion per year in the United States alone.50,54 Many interventions have been described for managing rotator cuff tears, but current clinical practice guidelines support physical therapy (PT) as the first option and surgical repair later if shoulder pain and dysfunction persist, even though evidence does not yet exist to unequivocally support the use of a specific PT protocol or surgical technique.1,6,17,44,48 Previous research has investigated how PT affects conventional clinical outcomes, specifically, patient-reported outcomes29,47 and strength.18,35,46 Other recent research has investigated the effects of arm positioning on acromiohumeral distance (AHD),20,21,49 but little is reported on the effects of PT on AHD. For patients suffering with a rotator cuff tear, PT is based on the premise that restoring joint motion is one of many important factors that likely contribute to a satisfactory clinical outcome. However, there is mixed evidence regarding the efficacy of PT programs to have an appreciable impact on shoulder motion.33 For example, Camargo et al14 used electromagnetic sensors to evaluate the effects of a 4-week exercise program in patients with impingement syndrome. The study reported significant differences in scapular kinematics, but these changes in scapular motion were small (1°-3°) and not considered clinically meaningful.14 In contrast, previous studies have evaluated the effects of exercise programs in swimmers19 and patients with impingement39 but have failed to detect significant differences in shoulder kinematics. There is some evidence that patients with impingement or shoulder pain have altered scapulothoracic and/or glenohumeral joint (GHJ) motion when compared with healthy subjects,30,31,34 but these differences also tend to be subtle (eg, differences in scapular upward rotation of up to 7°30). Taken together, these studies suggest that alterations in shoulder motion due to pathology or treatment are likely small and may be difficult to detect in a reasonable sample size when using a motion capture system that relies on skin-mounted markers or sensors. Consequently, the effects of rotator cuff pathology and PT on shoulder motion are still not fully understood.
The objectives of this study were to assess the influence of symptomatic rotator cuff pathology and the effects of PT on shoulder motion, strength, and patient-reported outcomes. We hypothesized that patients with a symptomatic rotator cuff tear would have a smaller AHD, altered scapulothoracic motion, lower range of motion (ROM), altered GHJ motion, and lower strength when compared with age-matched control subjects. We also hypothesized that PT would result in significant improvements in AHD, scapulothoracic motion, ROM, strength, and patient-reported outcomes.
Methods
Subjects
After institutional approval and informed consent, 2 subject populations were recruited for this study. The patient population consisted of 25 patients (mean age, 60.2 ± 8.4 years; range, 48-79 years; 7 males, 18 females) who had been diagnosed by an orthopaedic surgeon with a chronic (symptoms >6 months), small (<3 cm in greatest diameter) rotator cuff tear that had been documented using either magnetic resonance imaging (MRI) or ultrasound; 21 tears were documented with ultrasound and 4 were documented with MRI. All imaging was interpreted by a musculoskeletal radiologist. Potential study participants were excluded if they had any other injury or disease that may have interfered with shoulder function, had an outstanding workers’ compensation claim, or had been treated previously for their rotator cuff tear. Patients were recruited over 17 months from the Department of Orthopaedic Surgery at Henry Ford Health System. Twenty of 25 patients presented with tears in their dominant shoulder. For comparison, a control population was recruited that consisted of 25 age-matched volunteers (mean age, 59.0 ± 5.5 years; range, 51-74 years; 7 males, 18 females) who denied any history of shoulder pain, injury, or surgery. A standard clinical ultrasound examination was performed to document the condition of the rotator cuff in the dominant shoulder of each control subject. Thirty patients were initially recruited to participate in the study but 5 dropped out. None of the control subjects dropped out of the study.
Physical Therapy
Patients with a symptomatic rotator cuff tear were prescribed a standardized PT protocol that was based on previously reported systemic reviews.15,16,24,28,45,53 The PT protocol included supervised and home-based exercises designed to improve ROM and strength. Supervised therapy by 1 of 19 different physical therapists occurred approximately 2 to 3 times per week for approximately 8 weeks. Patients were instructed to perform ROM exercises daily and rotator cuff strengthening and scapulothoracic retraining exercises 3 times per week. To enhance the uniformity of PT, the physical therapist study coordinator (D.C.) communicated weekly with the therapists responsible for treating patients enrolled in the study. Electronic medical records were reviewed to document each patient’s number of supervised visits with a physical therapist.
Patient Testing
In vivo shoulder kinematics were measured using a biplane radiography imaging system during frontal-plane abduction, starting with the subject’s arm at his or her side and ending at approximately 120° of abduction. Testing was performed on the symptomatic shoulder of the patients and the dominant shoulder of the control subjects. Subjects were instructed to perform this motion in 2 seconds, and the motion speed was guided by a metronome. Subjects performed this shoulder motion while holding a 0.45-kg hand weight. Three trials were acquired, with a minimum of 2 minutes between trials. Radiographic images of the shoulder were acquired at 60 Hz with the biplane radiography system. A computed tomography (CT) scan of the humerus, scapula, and upper thorax was also acquired from each participant. The CT images were manually segmented and reconstructed into 3-dimensional (3D) bone models for the humerus, scapula, and ribs 3 and 4 (Mimics 13.1; Materialise). The 3D locations of anatomical landmarks were identified and used to define anatomical coordinate systems for the humerus, scapula, and thorax.7–10
Shoulder Motion
The 3D position and orientation of the humerus, scapula, and ribs 3 and 4 were measured from the biplane radiography images using model-based tracking, which has been shown to be accurate to within ±0.4 mm and 0.5°.9,11 Using these data, we measured conventional humerothoracic, glenohumeral, and scapulothoracic kinematics.4,9 Scapulothoracic and glenohumeral ranges of motion were calculated from 20° to 105° of humerothoracic elevation. In addition, GHJ contact patterns were estimated by combining the joint motion data measured from biplane radiographic images with the subject-specific bone models.8 Briefly, the GHJ contact center was estimated by calculating the centroid of the minimum distance between humerus and glenoid bone model surfaces for each frame of data and expressing the contact center position relative to the glenoid. To account for differences in subject size, these estimates of the GHJ contact center were normalized relative to the glenoid height and width as determined from the patient-specific bone models. Using these data, we determined the mean anteroposterior (AP) contact center and the average superoinferior (SI) contact center over each trial. In addition, we calculated the AP contact center range, the SI contact center range, and the contact center path length over each trial.8,10 The technique for estimating GHJ contact patterns was also used to determine the AHD. Specifically, we calculated the shortest distance between the humeral and acromial surfaces for every frame of data and then computed the mean distance over the entire trial. The GHJ contact center data and acromiohumeral data were determined from 20° to 70° of glenohumeral elevation.
Clinical Outcomes
Isometric shoulder strength while seated was measured using an isokinetic dynamometer (Biodex System 2) during frontal-plane abduction (ABD) at 30° abduction, sagittal-plane elevation (ELEV) at 30° of elevation, internal rotation (IR) at 15° of frontal-plane abduction and 0° of humeral rotation, and external rotation (ER) at 15° of frontal-plane abduction and 0° of humeral rotation.10 Three trials were acquired at each position, and both shoulders were tested. To account for differences in strength among subjects, strength of the involved shoulder was calculated as a percentage of the uninvolved shoulder. For control subjects, the strength data were normalized by calculating dominant shoulder strength as a percentage of nondominant shoulder strength. Patient-reported outcomes were assessed using a 10-cm visual analog scale (VAS) for pain and the Western Ontario Rotator Cuff Index (WORC). The VAS asked study participants to rate their shoulder pain on the day of laboratory testing. The WORC is a disease-specific quality-of-life measurement tool that provides a cumulative score based on the domains of physical symptoms, sport/recreation, work function, lifestyle function, and emotional function. The WORC has been shown to be a valid and reliable measurement tool for patients with rotator cuff disease.27 Last, active range of motion (AROM) and passive range of motion (PROM) while seated were manually measured using a goniometer for frontal-plane ABD, sagittal-plane ELEV, IR, and ER. The IR and ER measurements were performed from a starting position of 90° of frontal plane abduction and the forearm parallel to the ground. For the AROM measurements, study participants were asked to move their shoulders as far as possible unless limited by pain. For the PROM measurements, study participants were instructed to allow the examiner to move their shoulders as far as possible unless limited by pain. ROM data were acquired from the dominant shoulder of the control subjects. Three ROM measurements were taken for each subject at each testing time point. These clinical outcomes were assessed by physician-trained laboratory personnel with extensive experience in acquiring these outcome measures.
For the patients with a symptomatic rotator cuff tear, all data were acquired prior to beginning PT and again within 1 week on completion of approximately 8 weeks of PT. Data from the control subjects were acquired at a single time point.
Statistical Analysis
For all analyses, the data from all 3 trials were averaged. Outliers were identified as any data that were ±2.5 standard deviations away from the mean and excluded from analysis. Differences between the patients’ pre- and post-PT measures of shoulder motion, strength, ROM, pain, and WORC scores were assessed using paired t tests. Differences in shoulder motion, strength, and ROM between control subjects and patients both prior to PT and after PT were assessed using unpaired t tests. Significance was set at P ≤ .05.
Results
The patients’ mean age (60.2 ± 8.4 years; range, 48-79 years) was not significantly different than that for the control subjects (59.0 ± 5.5 years; range, 51-74 years; P = .55). The rotator cuff tear was in the dominant shoulder in 80% (20 of 25) of patients. The patients completed a mean 9.8 ± 2.7 (range, 6-15) supervised PT sessions. The mean treatment duration for physical therapy patients was 47.4 ± 19.4 days (range, 19-71 days).
Ultrasound Imaging
Only 9 of 25 asymptomatic control subjects were identified as having a normal, healthy rotator cuff. Tendinosis of the rotator cuff in general or supraspinatus in particular was noted in 15 control subjects, 4 control subjects were identified as having a partial-thickness rotator cuff tear, and 3 control subjects were identified as having a full-thickness rotator cuff tear. These 3 rotator cuff tears were described by the radiologist as a small- to moderate-sized mildly retracted tear measuring 1.5 cm (AP), a small nondisplaced tear measuring 0.6 cm (AP), and a 0.7-cm (AP) tear with differential retraction of approximately 2.4 cm. The symptomatic patients had a mean tear size of 1.4 cm (range, 0.8-2.6 cm).
Patient-Reported Pain and Function
PT had a significant effect on pain, with the VAS decreasing from 3.8 ± 2.7 (range, 0-9) before PT to 1.7 ± 2.1 (range, 0-7) after PT (P < .01). The patients’ composite WORC scores also improved significantly, from 40.6 ± 22.7 (range, 6.1-85.3) before PT to 70.3 ± 26.7 (range, 15.7-99.7) after PT (P < .01). In addition, the individual domains of the WORC score (physical function, sports, work, lifestyle, and emotions) improved significantly after PT (P < .01). Not surprisingly, the control subjects’ WORC score (98.2 ± 2.8; range, 89.6-100) was significantly higher than that for patients both before (P < .01) and after (P < .01) PT.
Range of Motion
PT had a significant effect on active ROM (Table 1 and Figure 1). Specifically, there were statistically significant increases in active ROM during ABD (P = .01), ELEV (P < .01), ER (P = .02), and IR (P = .03). Prior to PT, all patients’ active ROM measures were significantly lower than those for control subjects (P < .01) (Table 1 and Figure 1). After PT, the patients’ active ROM remained significantly lower than those for control subjects for ABD (P = .03), ELEV (P = .05), and ER (P < .01).
TABLE 1.
Clinical Outcome Measuresa
| Measure | Control | Pre | Post | P Value | ||
|---|---|---|---|---|---|---|
| Pre vs Control | Post vs Control | Pre vs Post | ||||
| Age, y | 59.0 ± 5.5 (51-74) | 60.2 ± 8.4 (48-79) | — | .55 | — | — |
| Subjective pain and function | ||||||
| Pain VAS | 0.0 ± 0.2 (0-1) | 3.8 ± 2.7 (0-9) | 1.7 ± 2.1 (0-7) | <.01 | <.01 | <.01 |
| WORC | 98.2 ± 2.8 (89.6-100) | 40.6 ± 22.7 (6.1-85.3) | 70.3 ± 26.7 (15.7-99.7) | <.01 | <.01 | <.01 |
| Active ROM, deg | ||||||
| ABD | 180 ± 0 (180-180) | 131.5 ± 54.1 (25.7-180) | 164.7 ± 31.6 (87.7-180.0) | <.01 | .03 | .01 |
| ELEV | 180 ± 0 (180-180) | 140.7 ± 50.2 (34.7-180) | 169.4 ± 22.8 (101-180) | <.01 | .05 | <.01 |
| ER | 102.0 ± 8.8 (85.3-120) | 71.5 ± 25.4 (9.7-103) | 86.2 ± 15.4 (58.3-116.3) | <.01 | <.01 | .02 |
| IR | 64.7 ± 10.3 (47.3-95.7) | 40.2 ± 24.1 (0-83.7) | 55.4 ± 23.3 (13-85.7) | <.01 | .08 | .03 |
| Passive ROM, deg | ||||||
| ABD | 180 ± 0 (180-180) | 135.2 ± 52.2 (44.3-180) | 164.3 ± 32.4 (83-180) | <.01 | .03 | <.01 |
| ELEV | 180 ± 0 (180-180) | 145.7 ± 48.5 (58.7-180) | 176.8 ± 15.1 (109-180) | <.01 | .33 | .02 |
| ER | 103.6 ± 7.8 (88.3-120) | 74.3 ± 27.0 (9.3-128.3) | 88.4 ± 16.0 (40-110.3) | <.01 | <.01 | .01 |
| IR | 57.3 ± 10.3 (42.3-78) | 34.3 ± 16.2 (10-66.3) | 43.8 ± 15.6 (14.3-76.3) | <.01 | <.01 | <.01 |
| Normalized strength, % | ||||||
| ABD | 96.8 ± 33.9 (36.1-172.5) | 63.8 ± 41.0 (0-146.7) | 59.7 ± 27.3 (9.0-120.8) | <.01 | <.01 | .17 |
| ELEV | 82.9 ± 22.2 (32.9-122.1) | 78.3 ± 46.0 (0-179.6) | 58.9 ± 32.3 (5.4-127.3) | .67 | <.01 | .11 |
| ER | 111.9 ± 16.3 (80.8-136.9) | 69.3 ± 24.0 (20.2-114.7) | 83.7 ± 27.7 (29.2-135.2) | <.01 | <.01 | .09 |
| IR | 111.7 ± 20.7 (70.1-148.0) | 78.3 ± 29.5 (15.6-144.6) | 87.9 ± 26.1 (10-142.6) | <.01 | <.01 | .33 |
aData are reported as mean ± SD (range). Boldfaced numbers indicate statistically significant difference (P ≤ .05). ABD, coronal plane abduction; ELEV, sagittal plane elevation; ER, external rotation; IR, internal rotation; post, post–physical therapy; pre, pre–physical therapy; ROM, range of motion; VAS, visual analog scale; WORC, Western Ontario Rotator Cuff index.
Figure 1.
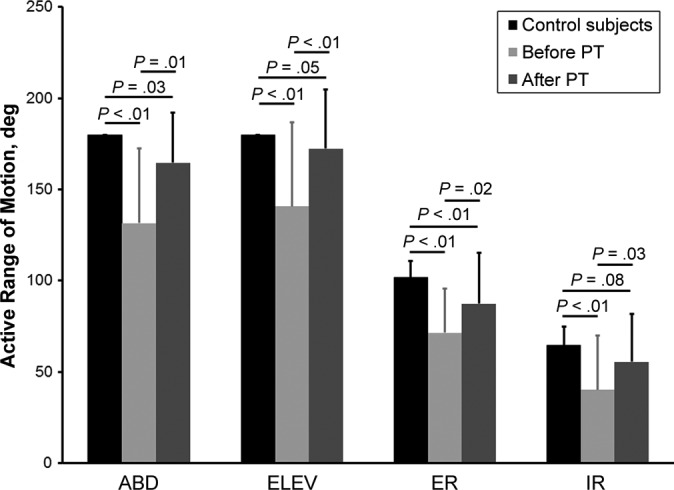
Physical therapy (PT) resulted in a statistically significant increase in active range of motion during coronal plane abduction (ABD), sagittal plane elevation (ELEV), external rotation (ER), and internal rotation (IR).
PT also resulted in significant increases in passive ROM (Table 1). Specifically, there were statistically significant increases in passive ROM during ABD (P < .01), ELEV (P = .02), ER (P = .01), and IR (P < .01). Prior to PT, all of the patients’ passive ROM measures were significantly lower than the control subjects’ (P < .01). After PT, the patients’ passive ROM remained significantly lower than the control subjects’ passive ROM for ABD (P = .03), ER (P < .01), and IR (P < .01), but no difference was detected between the control subjects and patients in passive ROM during ELEV (P = .33).
Shoulder Strength
PT had no significant effect on normalized shoulder strength (Table 1 and Figure 2). Compared with control subjects, the patients’ normalized strength was significantly lower both before and after PT for ABD, ER, and IR (P < .01) (Table 1 and Figure 2). No significant differences in ELEV strength were detected between control subjects and patients before PT (P = .67), but after PT, the patients’ ELEV strength was significantly lower than that for control subjects (P < .01).
Figure 2.
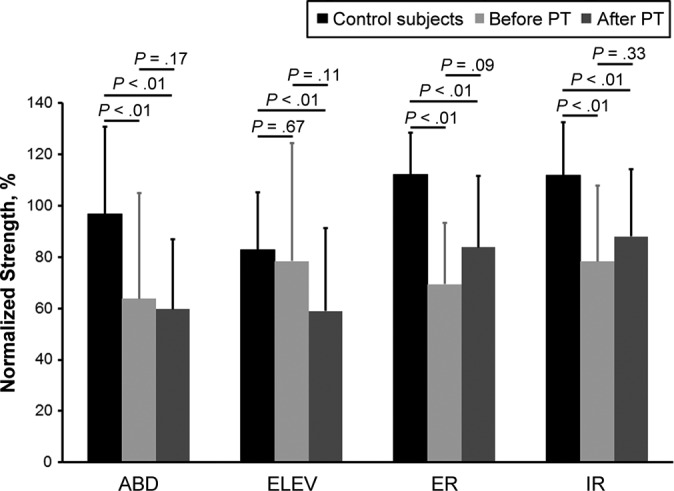
No statistically significant differences in normalized shoulder strength were detected as a result of physical therapy (PT). ABD, coronal plane abduction; ELEV, sagittal plane elevation; ER, external rotation; IR, internal rotation.
Scapulothoracic ROM
PT had a modest effect on joint ranges of motion during shoulder elevation (Table 2 and Figure 3). The range of scapulothoracic AP tilt increased from 20.0° ± 8.3° before PT to 24.6° ± 4.2° after PT (P = .05). The range of scapulothoracic upward rotation from pre-PT (23.8° ± 12.3°) to post-PT (27.4° ± 7.6°) time points was not found to be statistically significant (P = .17). The range of scapulothoracic internal/external rotation was also not found to be significantly different between pre-PT (10.3° ± 7.2°) and post-PT (9.8° ± 5.2°) time points (P = .68). Prior to PT, patients had significantly lower scapulothoracic AP tilt than control subjects (P = .05), but otherwise no statistically significant differences in scapulothoracic ranges of motion were detected between control subjects and patients (P > .33).
TABLE 2.
Joint Kinematic Measuresa
| Measure | Control | Pre | Post | P Value | ||
|---|---|---|---|---|---|---|
| Pre vs Control | Post vs Control | Pre vs Post | ||||
| Scapulothoracic ROM (Figure 3), deg | ||||||
| Internal/external rotation | 11.0 ± 4.8 (3.5 to 21.8) | 10.3 ± 7.2 (1.8 to 24.1) | 9.8 ± 5.2 (3.3 to 20.5) | .69 | .41 | .68 |
| AP tilt | 25.0 ± 5.2 (15.7 to 34.3) | 20.0 ± 8.3 (4.8 to 32.5) | 24.6 ± 4.2 (19.2 to 36.1) | .05 | .73 | .05 |
| Upward/downward rotation | 26.5 ± 5.6 (17.3 to 39.1) | 23.8 ± 12.3 (5.5 to 50.0) | 27.4 ± 7.6 (16.3 to 45.1) | .33 | .62 | .17 |
| Glenohumeral ROM, deg | ||||||
| Elevation | 54.0 ± 5.2 (43.2 to 61.0) | 37.0 ± 17.9 (2.9 to 61.6) | 47.3 ± 9.2 (18.9 to 60.7) | <.01 | .01 | .01 |
| Joint contact path (Figure 4) | ||||||
| Path length, % glenoid height | 31.6 ± 11.0 (17.2 to 58.8) | 26.7 ± 15.8 (0 to 65.6) | 33.0 ± 15.0 (5.2 to 59.4) | .23 | .72 | .10 |
| Joint contact center (Figure 5) | ||||||
| Mean SI position, % glenoid height | 6.1 ± 8.8 (–12.2 to 18.7) | 2.4 ± 8.9 (–15.5 to 20.0) | 1.8 ± 9.4 (–20.9 to 19.6) | .16 | .10 | .49 |
| Mean AP position, % glenoid width | –4.3 ± 6.0 (–17.5 to 8.6) | –4.8 ± 6.8 (–15.4 to 11.2) | –4.9 ± 10.9 (–31.5 to 15.2) | .78 | .80 | .20 |
| SI range, % glenoid height | 12.6 ± 5.9 (4.9 to 29.9) | 11.0 ± 6.1 (0.0 to 23.2) | 14.2 ± 7.1 (2.5 to 29.6) | .39 | .40 | .01 |
| AP range, % glenoid width | 8.8 ± 4.1 (3.8 to 21.3) | 7.1 ± 4.2 (0.0 to 19.0) | 8.8 ± 4.1 (3.8 to 21.3) | .17 | .33 | .48 |
| Acromiohumeral distance (Figure 6) | ||||||
| Mean, mm | 4.6 ± 1.2 (2.9 to 8.2) | 4.1 ± 1.6 (1.7 to 8.0) | 3.8 ± 1.6 (0.9 to 7.8) | .22 | .07 | .02 |
aData are presented as mean ± SD (range). Boldfaced numbers indicate statistically significant difference (P ≤ .05). AP, anteroposterior; post, post–physical therapy; pre, pre–physical therapy; ROM, range of motion; SI, superoinferior.
Figure 3.
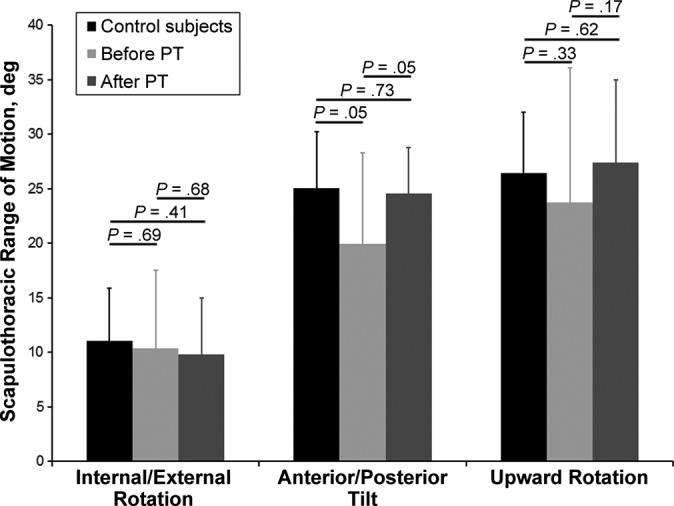
Physical therapy (PT) resulted in a significant increase in scapulothoracic anterior/posterior tilt range of motion (P = .05). After PT, the anterior/posterior tilt was not different from controls (P = .73).
Glenohumeral ROM
PT resulted in increased glenohumeral ELEV range of motion, increasing from 37.0° ± 17.9° before PT to 47.3° ± 9.2° after PT (P = .01) (Table 2). However, these ranges of motion were significantly lower than that for control subjects before (P < .01) and after (P = .01) PT.
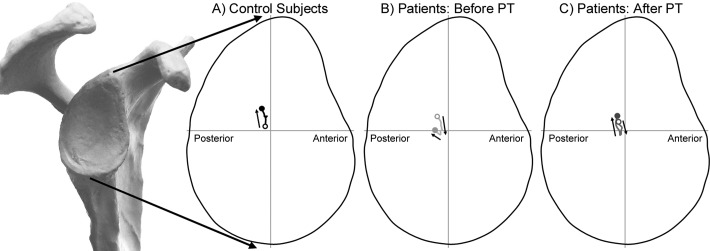
Glenohumeral Joint Contact Patterns
The humerus’ path of contact on the glenoid moved primarily in the SI direction during shoulder elevation for both control subjects and patients (Figure 4). More specifically, the joint contact center moved superiorly on the glenoid, with increasing shoulder elevation in the control subjects. However, for patients, the joint contact center moved inferiorly on the glenoid from approximately 20° to 50° of glenohumeral elevation and then reversed direction and moved superiorly on the glenoid. This pattern of joint contact occurred at both the pre- and post-PT time points, although the joint contact center moved more superiorly on the glenoid after PT. No difference in mean SI joint contact center was detected between control subjects and patients before PT (P = .16) or between controls and after PT (P = .10) (Figure 5).
Figure 4.
The lines superimposed on the glenoid indicate the path of joint contact during shoulder elevation for (A) control subjects, (B) patients before physical therapy (PT), and (C) patients after PT. In each figure, the open circle (^) indicates the center of contact at 20° of glenohumeral elevation and the closed circle (•) indicates the center of contact at 70° of glenohumeral elevation. The arrows indicate the direction of the contact path with increasing glenohumeral elevation.
Figure 5.
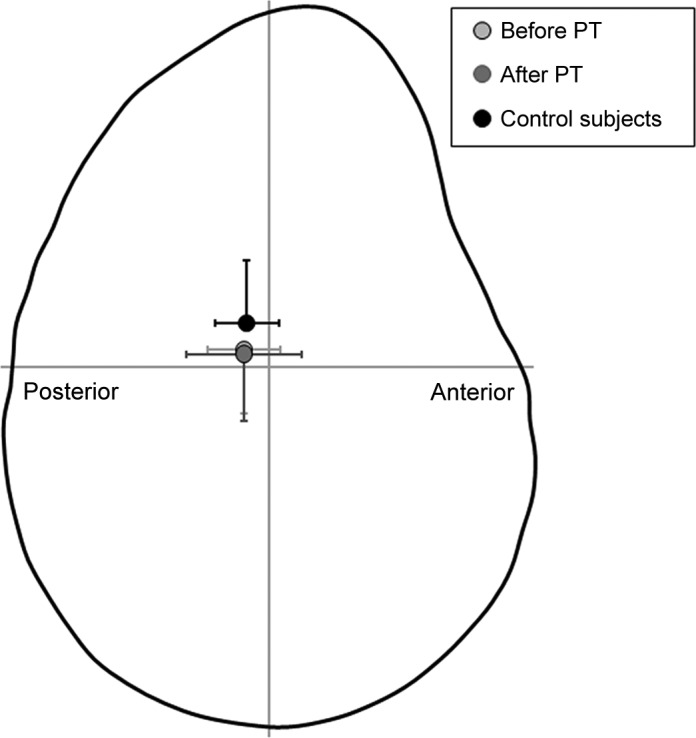
The control subjects’ mean joint contact center was positioned higher on the glenoid than the patients’ mean joint contact center, although no significant differences were found (P ≥ .10). PT, physical therapy.
PT did not significantly change the patients’ joint contact path length (Table 2; P = .10), and neither the pre- nor the post-PT values of the path length were significantly different than those of control subjects (P > .23). PT resulted in an increase in the range of SI joint contact (P = .01), but no changes due to PT were detected in the range of AP joint contact (P = .48). No difference was detected between control subjects and patients (before and after PT) in terms of the AP range of joint contact (P > .17) and the SI range of joint contact (P > .39).
Acromiohumeral Distance
In control subjects and patients, the AHD was at its maximum at 20° of glenohumeral elevation and decreased to a minimum at approximately 50° to 55° of glenohumeral elevation (Figure 6). The mean AHD from 20° to 70° of glenohumeral elevation decreased from 4.1 ± 1.6 mm before PT to 3.8 ± 1.6 mm after PT (P = .02). The decrease in AHD from before to after PT was statistically significant at 25° of glenohumeral elevation and again from 35° to 45° of glenohumeral elevation. The mean AHD from 20° to 70° of glenohumeral elevation for the control subjects was 4.6 ± 1.2 mm. The control subjects’ AHD was significantly greater than the patients’ pre- and post-PT AHD from 55° to 70° of glenohumeral elevation (Figure 6).
Figure 6.
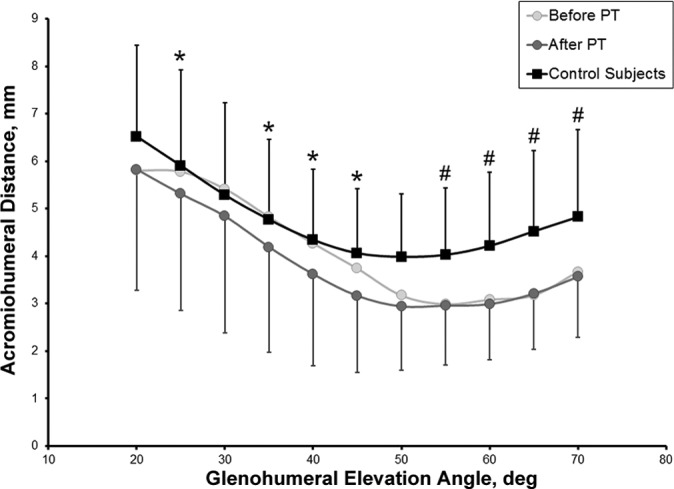
Physical therapy (PT) resulted in a small decrease in the acromiohumeral distance at certain glenohumeral joint angles (25°, 35°-45°). The control subjects’ acromiohumeral distance was significantly greater than the patients’ acromiohumeral distance from 55° to 70° of glenohumeral elevation before and after physical therapy (P < .02). Statistically significant difference *between pre- and post-PT values and #between control subjects and physical therapy patients (P ≤ .05).
Discussion
Compared with age-matched asymptomatic subjects, the study indicated that patients with a symptomatic rotator cuff tear had worse pain/function scores, less ROM, and lower ABD, ER, and IR strength. These patients also had less scapulothoracic AP tilt, less GHJ elevation, and an altered GHJ contact path than control subjects. The study also indicated that PT resulted in improved pain/function scores and increased ROM. In addition, after PT, patients had greater posterior scapulothoracic tilt, increased GHJ elevation, an increased range of SI joint contact, and a lower mean AHD.
There is ample evidence that PT has a positive effect on clinical outcomes in patients suffering from rotator cuff pathology, and the findings from the current study are consistent with previous research. For example, Kuhn et al29 reported that approximately 6 weeks of PT resulted in significant improvements in pain/function scores and shoulder ROM. Significant improvements in patient-reported pain/function scores and ROM after PT, either alone or in conjunction with other modalities, have been reported in other studies.2,5,32,39,40 The improvements in patient-reported pain and function in this study are encouraging, since current clinical practice guidelines support PT interventions as the first option in managing rotator cuff tears. Specifically, the improvements in ROM due to PT generally exceeded the minimal clinically important difference (MCID) of 10° to 15° as reported by Muir et al,43 the increase in WORC score of approximately 30 points exceeded the MCID of 11.7,27 and the decrease of 2.1 points for VAS pain exceeded the MCID of 1.4 as previously reported.52 It was perhaps not surprising that no significant differences in shoulder strength were detected in the current study, as this finding is consistent with previous research,3,51 and increasing shoulder strength was not the sole objective of the exercises prescribed in the PT protocol. Furthermore, previous research suggests that a longer exercise duration (eg, 12 vs 8 weeks) and/or a more rigorous strength-building protocol may be necessary to demonstrate significant improvements in strength in this patient population.36
Despite the significant improvements after 8 weeks of PT in conventional clinical outcome measures, the study is consistent with previous reports indicating that PT has only a subtle effect on GHJ or scapulothoracic motion patterns.14,19,30,31,33,39 For example, previous studies have reported that 4- to 6-week exercise programs result in only small and potentially clinically insignificant changes in scapulothoracic motion.14,39 Similarly, Lawrence et al30 also reported subtle differences in scapulothoracic upward rotation and AP tilt of approximately 3° to 7° between subjects with and without shoulder pain. The findings on scapulothoracic motion from the current study, which indicate increases in the ranges of AP tilt and upward rotation of approximately 3° to 5°, are consistent with previous studies. Although this study was not designed to evaluate the association between changes in joint motion and improvements in clinical outcomes, it is possible that changes in joint motion may indeed play a role in the etiology and treatment of rotator cuff pathology. It is important, however, to recognize that the MCID for changes in scapulothoracic motion, as well as the minimum change in scapulothoracic motion that can be accurately and reliably detected in a clinical setting, have not yet been established.
The study indicated that, prior to PT, symptomatic rotator cuff tear patients had approximately 5° less scapular posterior tilt (P = .05) than control subjects and that PT increased posterior tilt and essentially restored it to control subject levels. These findings are consistent with the concept of scapular dyskinesis and emphasize the importance of improving scapular mobility and stability in patients with rotator cuff pathology.13,22,23,25 It is tempting to suggest that an increase in posterior tilting of the scapula may decrease impingement pain by increasing the acromiohumeral distance, but the mean acromiohumeral distance in this study actually decreased slightly after PT (P = .02) (Figure 6). Furthermore, Karduna et al21 demonstrated in a cadaver study that posterior tilting had no effect on subacromial contact forces. Consequently, if decreases in pain after PT are related to changes in scapulothoracic motion, it seems unlikely that this is due solely to changes in AP tilt of the scapula.
The average GHJ contact paths (Figure 4) and joint contact centers (Figure 5) are consistent with previous studies10,12,37 and provide insight into the relationship between GHJ mechanics and rotator cuff pathology. For example, there was little difference in the mean SI joint contact center between the asymptomatic control subjects in the current study (mean age, 59.0 ± 5.5 years) and younger asymptomatic control subjects in previous work (mean age, 30.2 ± 7.9 years).10 The SI joint contact center of the older subjects in the current study was located 6.1% above the midpoint of the glenoid, whereas the SI joint contact center of the younger subjects was located 7.5% above the midpoint of the glenoid. However, the path lengths were substantially different, with the younger control subjects having a path length of only 21.5% ± 10.4% of glenoid height versus the older control subjects’ path length of 31.6% ± 11.0% of glenoid height. This finding may suggest that GHJ excursion increases with age, perhaps due to decreases in rotator cuff strength or changes in neuromuscular function, and that this change in joint mechanics may contribute to the development of rotator cuff pathology. However, it is important to reiterate that 16 of the 25 older control subjects in the current study had some form of ultrasound-diagnosed rotator cuff pathology, and therefore we cannot eliminate the possibility that rotator cuff pathology precipitated this change in joint mechanics.
The joint contact paths reported in the current study also suggest that supraspinatus function is significantly compromised in patients with a symptomatic rotator cuff tear. Specifically, inferior translation of the mean joint contact center from approximately 20° to 50° of GHJ elevation is a strong indication that the supraspinatus, which electromyographic studies indicate should be active over this range of motion,16 is not helping to stabilize the humerus against the glenoid. Consequently, it is not surprising that the joint contact center moves inferiorly on the glenoid during this range of motion. This finding is consistent with previous research by Millett and colleagues,42 who reported that the humeral head center translates 1 to 2 mm inferiorly during shoulder elevation in patients with a rotator cuff tear. Furthermore, this finding of inferior motion of the joint contact center at lower elevation angles is consistent with previously reported findings in patients who have had surgical rotator cuff repair.10 Consequently, these data suggest that the mechanical function of the supraspinatus that appears to be lost or diminished in patients with a painful rotator cuff tear is not adequately restored through surgical repair. However, it is important to acknowledge that electromyographic activity of the supraspinatus or other rotator cuff muscles was not measured in this study.
Another important finding from this study is that the mean joint contact center in the patients with a symptomatic rotator cuff tear is located near the equator of the glenoid (Figure 5). In contrast, previous research has shown that the mean joint contact center of patients with a surgically repaired (and intact) rotator cuff tear is located approximately 10% more superiorly on the glenoid.10 Taken together, these findings suggest that perhaps there is a significant difference in the GHJ mechanics between the patients in this study and those who eventually require surgery. Alternatively, these findings suggest that some aspect of surgery, either the surgical repair procedure or postoperative rehabilitation, results in the humerus being positioned more superiorly on the glenoid than the preoperative (ie, post-PT) condition. It is plausible to hypothesize that current surgical repair protocols place the repair tissues under excessive tension, which in turn translates the humerus into a position located more superiorly on the glenoid. This hypothesis about excessive repair tension is supported by a study by McCarron et al,38 who reported that tantalum markers implanted at the time of rotator cuff repair demonstrate substantial (15-20 mm) medial retraction of the repair, with most of that retraction occurring within the first 3 months after surgical rotator cuff repair. Although the only consequence of excessive repair tension in patients with a small rotator cuff tear may be altered GHJ mechanics, excessive repair tension may help explain the high incidence of recurrent tears in patients with a medium/large rotator cuff tear.
As with any study, this one was not without limitations. First, the individualized approach of delivering treatment made it difficult to ensure a uniform PT protocol among patients. Patient compliance with the home-based portion of the PT protocol was not measured, largely because no practical method exists yet for accurately and objectively assessing a patient’s home-based PT activities. Another limitation is that the radiography-based technique for measuring in vivo joint motion does not take cartilage into consideration, but Massimini et al37 reported that the location of the mean joint contact center is not significantly affected by the presence/absence of cartilage. It was also a limitation of this study that the data were confounded to some extent by changes in the patients’ ROM between the pre- and post-PT testing time points. For example, before PT, only 44% of patients were able to achieve 120° of humerothoracic elevation during in vivo joint motion testing, whereas 80% were able to meet or exceed this ROM at their post-PT visit. Since these inevitable differences made it difficult to select an ROM that was common to all study participants, we selected the ranges of 20° to 70° of glenohumeral elevation and 20° to 105° of humerothoracic motion to enable direct comparisons with previous research on postsurgical patients.10 Additional limitations included variability among patients in the number of supervised therapy visits and the duration of treatment, the use of a convenience sample, assessors who were not blinded to the study participants’ treatment groups, and inclusion of subjects with asymptomatic rotator cuff pathology in the control group.
In summary, this study demonstrated that there are appreciable differences in conventional clinical outcomes when comparing patients with a symptomatic rotator cuff tear to asymptomatic control subjects and that PT has a significant effect on clinical outcomes; however, physical therapy did not restore patients to the levels of controls. The differences in joint motion between patients and control subjects, or between pre- and post-PT time points, are much more subtle. Ongoing research is aimed at more precisely defining the relationship between rotator cuff integrity, joint motion, strength, and conventional clinical outcomes.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This research was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under award number AR051912.
References
- 1. American Academy of Orthopaedic Surgeons. Optimizing the Management of Rotator Cuff Problems: Guidelines and Evidence Report. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2010. [DOI] [PubMed] [Google Scholar]
- 2. Analan PD, Leblebici B, Adam M. Effects of therapeutic ultrasound and exercise on pain, function, and isokinetic shoulder rotator strength of patients with rotator cuff disease. J Phys Ther Sci. 2015;27:3113–3117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bang MD, Deyle GD. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. J Orthop Sports Phys Ther. 2000;30:126–137. [DOI] [PubMed] [Google Scholar]
- 4. Baumer TG, Giles JW, Drake A, Zauel R, Bey MJ. Measuring three-dimensional thorax motion via biplane radiographic imaging: technique and preliminary results. J Biomech Eng. 2016;138(1). doi:10.1115/1.4032058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Baydar M, Akalin E, El O, et al. The efficacy of conservative treatment in patients with full-thickness rotator cuff tears. Rheumatol Int. 2009;29:623–628. [DOI] [PubMed] [Google Scholar]
- 6. Beaudreuil J, Dhenain M, Coudane H, Mlika-Cabanne N. Clinical practice guidelines for the surgical management of rotator cuff tears in adults. Orthop Traumatol Surg Res. 2010;96:175–179. [DOI] [PubMed] [Google Scholar]
- 7. Bey MJ, Brock SK, Beierwaltes WN, Zauel R, Kolowich PA, Lock TR. In vivo measurement of subacromial space width during shoulder elevation: technique and preliminary results in patients following unilateral rotator cuff repair. Clin Biomech (Bristol, Avon). 2007;22:767–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bey MJ, Kline SK, Zauel R, Kolowich PA, Lock TR. In vivo measurement of glenohumeral joint contact patterns. EURASIP J Adv Signal Process. 2010;2010(162136):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bey MJ, Kline SK, Zauel R, Lock TR, Kolowich PA. Measuring dynamic in-vivo glenohumeral joint kinematics: technique and preliminary results. J Biomech. 2008;41:711–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bey MJ, Peltz CD, Ciarelli K, et al. In vivo shoulder function after surgical repair of a torn rotator cuff: glenohumeral joint mechanics, shoulder strength, clinical outcomes, and their interaction. Am J Sports Med. 2011;39:2117–2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bey MJ, Zauel R, Brock SK, Tashman S. Validation of a new model-based tracking technique for measuring three-dimensional, in vivo glenohumeral joint kinematics. J Biomech Eng. 2006;128:604–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Boyer PJ, Massimini DF, Gill TJ, et al. In vivo articular cartilage contact at the glenohumeral joint: preliminary report. J Orthop Sci. 2008;13:359–365. [DOI] [PubMed] [Google Scholar]
- 13. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19:641–661. [DOI] [PubMed] [Google Scholar]
- 14. Camargo PR, Alburquerque-Sendin F, Avila MA, Haik MN, Vieira A, Salvini TF. Effects of stretching and strengthening exercises with and without manual therapy on scapular kinematics, function, and pain in individuals with shoulder impingement: a randomized controlled trial. J Orthop Sports Phys Ther. 2015;45:984–997. [DOI] [PubMed] [Google Scholar]
- 15. Cools AM, Dewitte V, Lanszweert F, et al. Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sports Med. 2007;35:1744–1751. [DOI] [PubMed] [Google Scholar]
- 16. Escamilla RF, Yamashiro K, Paulos L, Andrews JR. Shoulder muscle activity and function in common shoulder rehabilitation exercises. Sports Med. 2009;39:663–685. [DOI] [PubMed] [Google Scholar]
- 17. Gebremariam L, Hay EM, Koes BW, Huisstede BM. Effectiveness of surgical and postsurgical interventions for the subacromial impingement syndrome: a systematic review. Arch Phys Med Rehabil. 2011;92:1900–1913. [DOI] [PubMed] [Google Scholar]
- 18. Harris JD, Pedroza A, Jones GL. Predictors of pain and function in patients with symptomatic, atraumatic full-thickness rotator cuff tears: a time-zero analysis of a prospective patient cohort enrolled in a structured physical therapy program. Am J Sports Med. 2012;40:359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hibberd EE, Oyama S, Spang JT, Prentice W, Myers JB. Effect of a 6-week strengthening program on shoulder and scapular-stabilizer strength and scapular kinematics in division I collegiate swimmers. J Sport Rehabil. 2012;21:253–265. [DOI] [PubMed] [Google Scholar]
- 20. Kalra NS AL, Boardman ND, 3rd, Michener LA. Effect of posture on acromiohumeral distance with arm elevation in subjects with and without rotator cuff disease using ultrasonography. J Orthop Sports Phys Ther. 2010;40:633–640. [DOI] [PubMed] [Google Scholar]
- 21. Karduna AR, Kerner PJ, Lazarus MD. Contact forces in the subacromial space: effects of scapular orientation. J Shoulder Elbow Surg. 2005;14:393–399. [DOI] [PubMed] [Google Scholar]
- 22. Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘Scapular Summit’. Br J Sports Med. 2013;47:877–885. [DOI] [PubMed] [Google Scholar]
- 23. Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2003;11:142–151. [DOI] [PubMed] [Google Scholar]
- 24. Kibler WB, McMullen J, Uhl T. Shoulder rehabilitation strategies, guidelines, and practice. Orthop Clin North Am. 2001;32:527–538. [DOI] [PubMed] [Google Scholar]
- 25. Kibler WB, Sciascia A. Current concepts: scapular dyskinesis. Br J Sports Med. 2010;44:300–305. [DOI] [PubMed] [Google Scholar]
- 26. Kim HM, Dahiya N, Teefey SA, et al. Location and initiation of degenerative rotator cuff tears: an analysis of three hundred and sixty shoulders. J Bone Joint Surg Am. 2010;92:1088–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kirkley A, Alvarez C, Griffin S. The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: The Western Ontario Rotator Cuff Index. Clin J Sport Med. 2003;13:84–92. [DOI] [PubMed] [Google Scholar]
- 28. Kuhn JE. Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elbow Surg. 2009;18:138–160. [DOI] [PubMed] [Google Scholar]
- 29. Kuhn JE, Dunn WR, Sanders R, et al. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg. 2013;22:1371–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lawrence RL, Braman JP, Laprade RF, Ludewig PM. Comparison of 3-dimensional shoulder complex kinematics in individuals with and without shoulder pain, part 1: sternoclavicular, acromioclavicular, and scapulothoracic joints. J Orthop Sports Phys Ther. 2014;44:636–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lawrence RL, Braman JP, Staker JL, Laprade RF, Ludewig PM. Comparison of 3-dimensional shoulder complex kinematics in individuals with and without shoulder pain, part 2: glenohumeral joint. J Orthop Sports Phys Ther. 2014;44:646–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ludewig PM, Borstad JD. Effects of a home exercise programme on shoulder pain and functional status in construction workers. Occup Environ Med. 2003;60:841–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ludewig PM, Braman JP. Shoulder impingement: biomechanical considerations in rehabilitation. Man Ther. 2011;16:33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276–291. [PubMed] [Google Scholar]
- 35. MacDermid JC, Ramos J, Drosdowech D, Faber K, Patterson S. The impact of rotator cuff pathology on isometric and isokinetic strength, function, and quality of life. J Shoulder Elbow Surg. 2004;13:593–598. [DOI] [PubMed] [Google Scholar]
- 36. Maenhout AG, Mahieu NN, De Muynck M, De Wilde LF, Cools AM. Does adding heavy load eccentric training to rehabilitation of patients with unilateral subacromial impingement result in better outcome? A randomized, clinical trial. Knee Surg Sports Traumatol Arthrosc. 2013;21:1158–1167. [DOI] [PubMed] [Google Scholar]
- 37. Massimini DF, Warner JJ, Li G. Glenohumeral joint cartilage contact in the healthy adult during scapular plane elevation depression with external humeral rotation. J Biomech. 2014;47:3100–3106. [DOI] [PubMed] [Google Scholar]
- 38. McCarron JA, Derwin KA, Bey MJ, et al. Failure with continuity in rotator cuff repair “healing”. Am J Sports Med. 2013;41:134–141. [DOI] [PubMed] [Google Scholar]
- 39. McClure PW, Bialker J, Neff N, Williams G, Karduna A. Shoulder function and 3-dimensional kinematics in people with shoulder impingement syndrome before and after a 6-week exercise program. Phys Ther. 2004;84:832–848. [PubMed] [Google Scholar]
- 40. Michener LA, Walsworth MK, Burnet EN. Effectiveness of rehabilitation for patients with subacromial impingement syndrome: a systematic review. J Hand Ther. 2004;17:152–164. [DOI] [PubMed] [Google Scholar]
- 41. Milgrom C, Schaffler M, Gilbert S, van Holsbeeck M. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J Bone Joint Surg Br. 1995;77:296–298. [PubMed] [Google Scholar]
- 42. Millett PJ, Giphart JE, Wilson KJ, Kagnes K, Greenspoon JA. Alterations in glenohumeral kinematics in patients with rotator cuff tears measured with biplane fluoroscopy. Arthroscopy. 2016;32:446–451. [DOI] [PubMed] [Google Scholar]
- 43. Muir SW, Corea CL, Beaupre L. Evaluating change in clinical status: reliability and measures of agreement for the assessment of glenohumeral range of motion. N Am J Sports Phys Ther. 2010;5:98–110. [PMC free article] [PubMed] [Google Scholar]
- 44. Pedowitz RA, Yamaguchi K, Ahmad CS, et al. Optimizing the management of rotator cuff problems. J Am Acad Orthop Surg. 2011;19:368–379. [DOI] [PubMed] [Google Scholar]
- 45. Reinold MM, Escamilla RF, Wilk KE. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009;39:105–117. [DOI] [PubMed] [Google Scholar]
- 46. Roddey TS, Cook KF, O’Malley KJ, Gartsman GM. The relationship among strength and mobility measures and self-report outcome scores in persons after rotator cuff repair surgery: impairment measures are not enough. J Shoulder Elbow Surg. 2005;14(1 Suppl S):95S–98S. [DOI] [PubMed] [Google Scholar]
- 47. Saraswat MK, Styles-Tripp F, Beaupre LA, et al. Functional outcomes and health-related quality of life after surgical repair of full-thickness rotator cuff tears using a mini-open technique: a concise 10-year follow-up of a previous report. Am J Sports Med. 2015;43:2794–2799. [DOI] [PubMed] [Google Scholar]
- 48. Seida JC, LeBlanc C, Schouten JR, et al. Systematic review: nonoperative and operative treatments for rotator cuff tears. Ann Intern Med. 2010;153:246–255. [DOI] [PubMed] [Google Scholar]
- 49. Seitz AL, McClure PW, Lynch SS, Ketchum JM, Michener LA. Effects of scapular dyskinesis and scapular assistance test on subacromial space during static arm elevation. J Shoulder Elbow Surg. 2012;21:631–640. [DOI] [PubMed] [Google Scholar]
- 50. Silverstein B, Kalat J. Work-related musculoskeletal disorders of the neck, back, and upper extremity in Washington State, 1992-2000. Technical Report No. 40-6-2002 http://www.lni.wa.gov/sharp/WMSD2002Summary.pdf. Accessed January 1, 2003. [DOI] [PubMed]
- 51. Struyf F, Nijs J, Mollekens S, et al. Scapular-focused treatment in patients with shoulder impingement syndrome: a randomized clinical trial. Clin Rheumatol. 2013;32:73–85. [DOI] [PubMed] [Google Scholar]
- 52. Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 2009;18:927–932. [DOI] [PubMed] [Google Scholar]
- 53. Tate AR, McClure PW, Young IA, Salvatori R, Michener LA. Comprehensive impairment-based exercise and manual therapy intervention for patients with subacromial impingement syndrome: a case series. J Orthop Sports Phys Ther. 2010;40:474–493. [DOI] [PubMed] [Google Scholar]
- 54. Vitale MA, Vitale MG, Zivin JG, Braman JP, Bigliani LU, Flatow EL. Rotator cuff repair: an analysis of utility scores and cost-effectiveness. J Shoulder Elbow Surg. 2007;16:181–187. [DOI] [PubMed] [Google Scholar]
- 55. Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19:116–120. [DOI] [PubMed] [Google Scholar]