Summary
Background
Gastro-Intestinal bleeding remains a frequent clinical dilemma and common cause of hospitalization, morbidity and mortality.
Case Report
We report a case of pseudo aneurysm of splenic artery developed after an episode of acute on chronic pancreatitis which was treated by direct percutaneous puncture of pseudoaneurysm and embolization by coils.
Conclusions
The aim was to preserve the main splenic artery and avoid the complications of splenic artery embolization like infarcts and abscess.
MeSH Keywords: Embolization, Therapeutic; Pancreatitis, Chronic; Splenic Artery
Background
Pseudoaneurysm is a well-recognized complication of pancreatitis. Transcatheter embolization of pseudoaneurysm by coils is the treatment of choice [1] Percutaneous embolization is used as an alternative treatment when transcatheter embolization is not feasible [2,3].
Percutaneous embolization by direct needle puncture has been successfully employed to occlude pseudoaneurysm [2,3], aneurysm [4] and vascular malformations [5]. The available embolized materials for percutaneous technique are thrombin, glue, gelfoam and coils. Complications associated with glue for treatment of bleeding lesions include embolic events and equipment damage [6].
In this case, coils were preferred over glue and thrombin to embolize the splenic artery pseudoaneurysm to maintain the patency of the splenic artery. To our knowledge, this is the first case report where we directly punctured the pseudoaneurysm and embolized it by coils in the case of chronic calcific atrophic pancreatitis.
Case Report
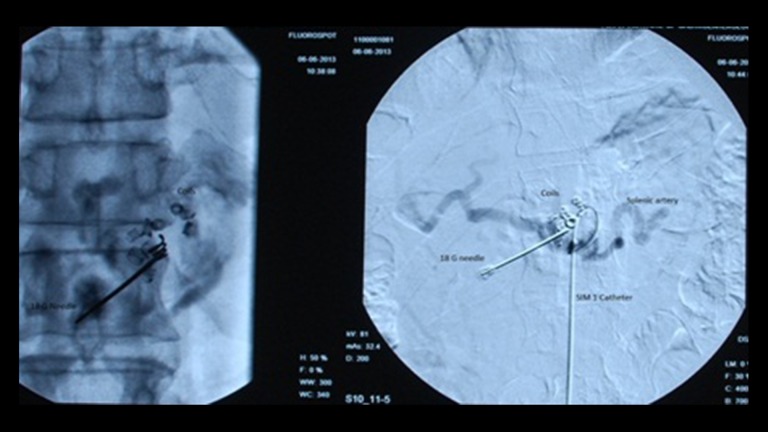
A 49-year-old male patient was admitted with complaints of pain in the epigastric region radiating to the back and two episodes of hematemesis on the day of admission. Patient was a known case of ethanol-related chronic pancreatitis for the last 2 years. Blood investigation showed anemia (7.9 gm/dL) with normal amylase and lipase levels. Upper GI endoscopy reveled grade 3 esophageal varices with an adherent clot along the lesser curvature. Triple-phase CT of the abdomen showed a pseudocyst with intracystic bleed and proximal splenic artery pseudoaneurysm of 23×18 mm in size (Figure 1), with thrombosed portal vein, splenic vein, and superior mesenteric vein with collaterals.
Figure 1.
CT image: Pseudoaneurysm arising from the proximal splenic artery.
Conventional angiography revealed proximal splenic artery pseudoaneurysm. We tried to embolize the pseudoaneurysm via the right femoral route but failed to cannulate the splenic artery because of its tortuosity. The other available options were percutaneous embolization by glue, thrombin and coils. A common complication after percutaneous embolization with glue is embolic events and equipment damage [6].
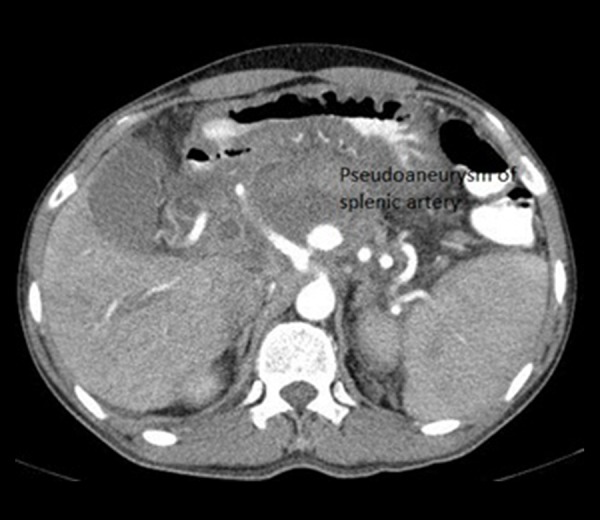
Under USG guidance, we directly punctured the pseudoaneurysm with an 18-gauge (VYGON 20 mm-18G-L.90 mm) needle and confirmed the position of the needle by injecting contrast under fluoroscopy (Siemans artis U) (Figure 2). Through this needle, IMWCE coils (of the following size: 35-3-3, by cook medical) and tornado coils (35-4/3 by cook medical) were placed in the pseudoaneurysm (Figure 3). During the procedure we simultaneously performed angiography by the transfemoral route via SIM 1 catheter (5 french-0.035 inch-100 cm by cook medical) to check the patency of the splenic artery (Figure 3). When we confirmed by angiogram that the pseudoaneurysm was embolized by coils, we injected 3 mL of glue and lipoidol combination to completely occlude the pseudoaneurysm (Figure 4). A follow-up angiogram revealed non-filling of the pseudoaneurysm with preservation of the splenic artery (Figure 5). The post-procedure period was uneventful. He improved symptomatically with stabilization of the hemoglobin level. Post-procedure color Doppler USG after 48 hrs revealed non-filling of pseudoaneurysm with normal splenic artery and no evidence of splenic infarcts. At the time of discharge vital parameters were stable with normal oral diet, bladder and bowel habits. We followed the patient for one year and no evidence of recurrence of pseudoaneurysm was noted.
Figure 2.
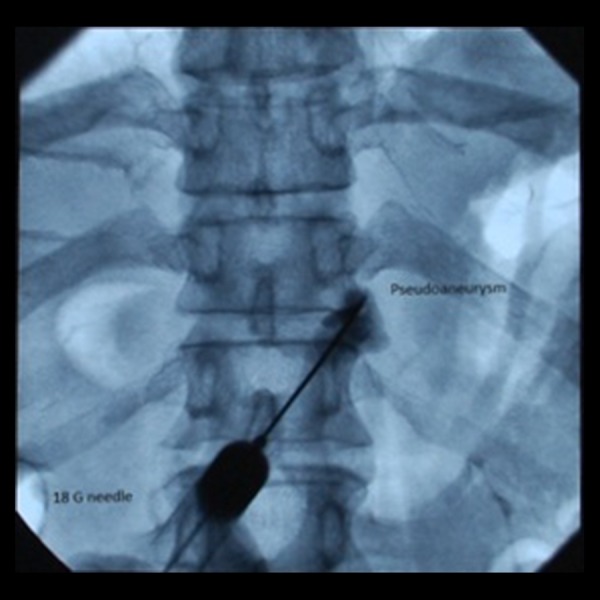
DSA image: Direct puncture of pseudoaneurysm by an 18-G needle.
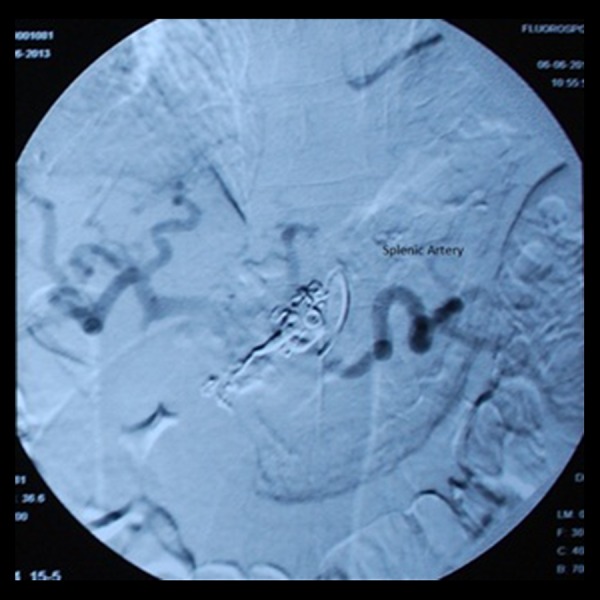
Figure 3.
DSA image: Coil embolization of pseudoaneurysm.
Figure 4.
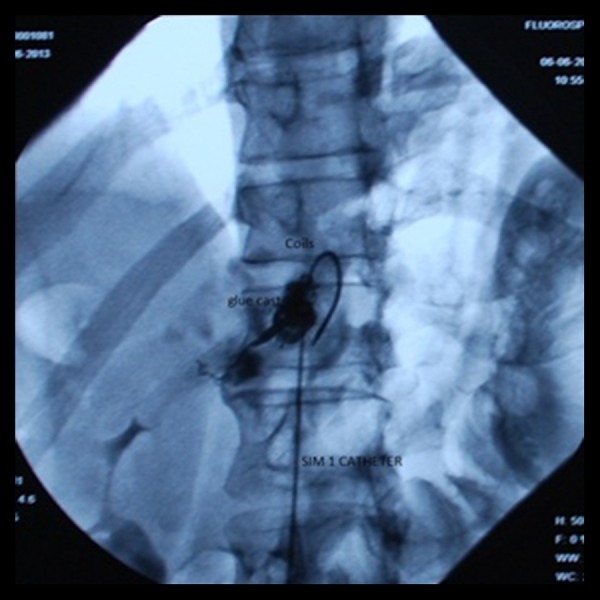
DSA image: Embolized pseudoaneurysm by coils and glue cast.
Figure 5.
DSA Image: Post procedure check angiogram – embolized pseudoaneurysm and patent splenic artery.
Discussion
A bleeding pseudoaneurysm is a serious complication of chronic pancreatitis and has an incidence of up to 10% [7]. Mortality in a treated rupture of pseudoaneurysm ranges from 12 to 57%, or as high as 90–100% in untreated cases depending on the patient’s clinical condition, site and characteristics of the pseudoaneurysm [8].
Two available methods of embolization in post-pancreatitis pseudoaneurysm are transcathter [1] and percutaneous [2]. Coils, glue, PVA particle, thrombin and stent graft are used to control the bleeding. The choice of the embolic agent is based on the types of the bleeding artery, vascular anatomy, size of the vessel being occluded, level of vascular occlusion and catheter or needle position to be achieved during the procedure [1]. In post-pancreatitis pseudoaneurysm transcathter embolization by coils is the treatment of choice. Percutaneous embolization is used when transcathter embolisation is not feasible. Direct puncture and percutaneous embolization technique are commonly used in the peripheral vascular interventions, pulmonary, breast, lumbar, and renal pseudoaneurysms. Reports are available on post-pancreatitis pseudoaneurysm embolization by direct puncture of pseudoaneurysm and embolization by thrombin and glue [2,3]. We elected to use coils as the therapeutic agent to maintain the patency of the splenic artery. If the results were confirmed by larger experiences, the direct puncture of pseudoaneurysm and embolisation by coils can be consider treatment of choice when transcather embolization cannot be performed.
Conclusions
Direct puncture and percutaneous embolization of pseudoaneurysm by coils can be safely performed in abdomen situations where the accessibility and anatomy of the vessel is not favourable for transcatheter embolization and pseudoaneurysm is well visualized on USG. By this technique, we maintain the patency of the main artery and embolize the pseudoaneurysm and we can avoid the complications of splenic artery embolization like infarcts and abscess.
Footnotes
Conflict of interests
The authors do not have any disclosures or conflict of interests that they would like to declare in relation to their paper.
References
- 1.Shin JH. Recent update of embolization of upper gastrointestinal tract bleeding. Korean J Radiol. 2012;13(Suppl 1):S31–39. doi: 10.3348/kjr.2012.13.S1.S31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Puri S, Nicholson AA, Breen DJ. Percutaneous thrombin injection for the treatment of a post-pancreatitis pseudoaneurysm. Eur Radiol. 2003;13(Suppl 4):L79–82. doi: 10.1007/s00330-003-1836-5. [DOI] [PubMed] [Google Scholar]
- 3.Kreuger K, Zaehringer M, Lackner K. Percutaneous treatment of a splenic artery pseudoaneurysm by thrombin injection. J Vasc Interv Radiol. 2005;16:1023–25. doi: 10.1097/01.RVI.0000162167.54455.C0. [DOI] [PubMed] [Google Scholar]
- 4.Chan RP, David E. Reperfusion of splanchnic artery aneurysm following transcatheter embolization: treatment with percutaneous thrombin injection. Cardiovasc Intervent Radiol. 2004;27(3):264–67. doi: 10.1007/s00270-003-0092-z. [DOI] [PubMed] [Google Scholar]
- 5.Yakes WF, Pevsner P, Reed M, et al. Serial embolizations of an extremity arteriovenous malformation with alcohol via direct percutaneous puncture. Am J Roentgenol. 1986;146(5):1038–40. doi: 10.2214/ajr.146.5.1038. [DOI] [PubMed] [Google Scholar]
- 6.Petersen B, Barkun A, Carpenter S, et al. Tissue adhesives and fibrin glues. Gastrointest Endosc. 2004;60(3):327–33. doi: 10.1016/s0016-5107(04)01564-0. [DOI] [PubMed] [Google Scholar]
- 7.White AF, Baum S, Buranasiri S. Aneurysms secondary to pancreatitis. Am J Roentgenol. 1976;127(3):393–96. doi: 10.2214/ajr.127.3.393. [DOI] [PubMed] [Google Scholar]
- 8.Kapoor S, Pankaj R, Pal S, Chatopadhyay TK. Hemosuccus pancreaticus: An uncommon cause of gastrointestinal hemorrhage. A case report. JOP. 2004;5:373–76. [PubMed] [Google Scholar]