Abstract
Genu varus malalignment can lead to medial compartment overload and progression of ipsilateral compartment osteoarthritis. To slow this process, a medial opening wedge proximal tibial osteotomy (PTO) can be performed. This type of PTO is indicated in patients with genu varus malalignment and isolated medial compartment osteoarthritis of the knee, prior to or concurrent with medial compartment cartilage procedures or meniscal transplants, chronic posterolateral corner deficiency, or chronic anterior cruciate ligament deficiency. When treating ligamentous instability, a PTO can be performed in isolation, with simultaneous ligament reconstruction, or as a staged procedure with the osteotomy first, followed by ligament reconstruction if instability persists. Failure to address malalignment in cases of concurrent ligament reconstruction leads to increased stress on the graft and potential graft failure. One distinct advantage of this procedure is the ability to correct deformities in the sagittal and coronal planes. The purpose of this article was to describe our technique used to perform a medial opening wedge PTO.
Genu varus deformity can lead to medial compartment overload and a progression of ipsilateral compartment osteoarthritis.1 Some of the possible treatments for symptomatic malalignment include physical therapy, medial unloader bracing, and in-shoe heel wedges in an attempt to offload the medial compartment and delay the need for arthroplasty.2, 3 However, the predictability and durability of these treatment modalities may not meet the expectations and physical demands of young and active patients. In such cases, a valgus-producing medial opening wedge proximal tibial osteotomy (PTO) has been proposed to restore neutral mechanical alignment and alleviate excess load on the medial compartment.1, 3, 4, 5 This technique has been reported to produce significant improvement in subjective and objective clinical outcome scores when treating medial compartment overload.6, 7
Recently, the indications for this technique have expanded to include the treatment of chronic central and posterolateral ligamentous instability, and also to protect ligament reconstructions in the setting of varus malalignment.8 Studies have reported improved outcomes when used for these indications.8, 9, 10 An important aspect of the medial opening wedge PTO is the ability to perform corrections in the coronal and sagittal planes, which is commonly required to restore knee stability. We present our preferred technique and indications for medial opening wedge PTO using plate osteosynthesis and adjunctive bone allograft.
Surgical Technique
Objective Diagnosis
To determine the proper course of treatment, a thorough medical and surgical history is required. In cases of trauma with resultant instability, the mechanism of injury should be ascertained. The instability pattern is assessed with clinical examination, evaluation of gait pattern, stress radiographs, and magnetic resonance imaging (MRI) for concomitant injuries.
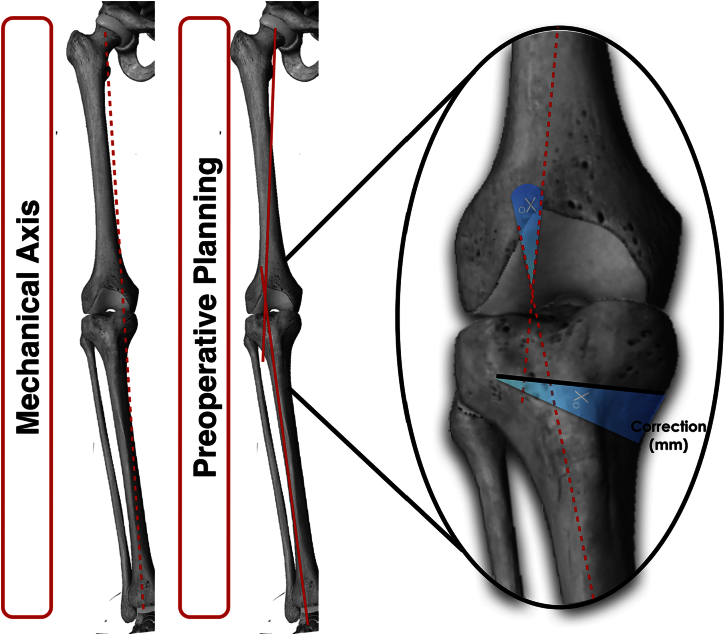
Weightbearing hip-knee-ankle radiographs are obtained to evaluate lower limb alignment. To determine the mechanical axis, a straight line is drawn from the center of the femoral head through the center of the talar dome (Fig 1). The preoperative mechanical axis is calculated as a percentage of the width across the tibial plateau, with the medial border considered 0% and the lateral border, 100%. Confirmation of varus malalignment occurs when the mechanical axis is situated medial to the apex of the medial tibial eminence, or more than 41% across the tibial plateau in the coronal plane.11
Fig 1.
Schematic representation of a right knee showing the methodology for measurement of both varus malalignment and proposed correction for a medial opening wedge osteotomy. To evaluate the amount of deformity in the mechanical axis, a line is drawn from the center of the femoral head to the center of the talar dome. Planning for surgical correction is made by measuring the angle created by a line drawn from the center of the femoral head to the center of the lateral tibial eminence and a line down the anatomic axis of the tibia. This angle is then transposed to the medial proximal tibia at the level of the desired correction. An anteriorly or posteriorly placed plate can later result in a biplanar correction by increasing or decreasing the tibial slope respectively.
Preoperative planning for patients with medial compartment osteoarthritis seeks to restore the mechanical axis through the apex of the lateral tibial eminence (56% across the tibial plateau).11 The required angle of correction in the coronal plane is calculated by drawing a line from the center of the femoral head through the apex of the lateral tibial eminence. Another line is drawn from the center of the talar dome through the same point on the tibia. The angle created by the intersection of these 2 lines provides the osteotomy correction angle needed to achieve the required correction. This angle is transposed to the location of the most lateral cut of the planned osteotomy on the proximal tibia and expanded to the medial proximal tibia. This calculated angulation creates a triangle, with the height (in millimeters) at the medial tibial cortex representing the required amount of correction for the osteotomy (Fig 1). When planning the osteotomy, it is important to leave approximately 1 cm of lateral cortex intact to avoid cortical fracture.
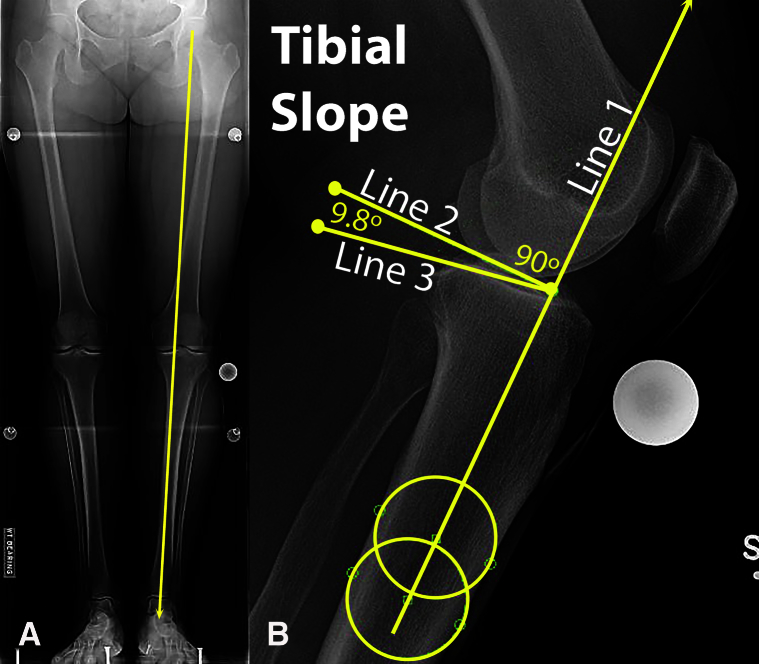
Standard anteroposterior (AP), standing AP 45° flexion radiographs (Rosenberg view), and lateral knee radiographs are obtained to evaluate tibial slope and the amount of joint space narrowing. It is essential to calculate the sagittal plane tibial slope preoperatively because medial opening wedge PTO has been reported to change the proximal tibial slope, and plate positioning can affect the degree of slope change (Fig 2).12
Fig 2.
(A) Long-length standing radiograph of the bilateral lower extremities showing the left lower limb mechanical axis with varus malalignment. (B) Lateral radiograph of a left knee with associated measurement of the tibial slope by drawing 2 circles in the tibial shaft that are each tangent to the anterior to posterior cortices, and drawing a straight line extending between the central point of the circles to find the anteroposterior midpoint of the tibia (line 1). A second line (line 2) is drawn perpendicular to the first at the level of the tibial plateau, and a third line (line 3) is drawn along the tibial slope, using the medial femoral condyle. The angle measured between the second and third lines is the preoperative angle of the tibial slope.
Tibial slope is evaluated on the lateral radiograph by electronically drawing 2 circles in the tibial shaft that are each tangent to the anterior to posterior cortices, and drawing a straight line extending between the central point of the circles to find the anteroposterior midpoint of the tibia. A second line is drawn perpendicular to the first at the level of the tibial plateau, and a third line is drawn along the medial tibial slope. The angle measured between the second and third lines is the preoperative angle of the tibial slope.
For chronic posterolateral corner (PLC) injuries, clinical examination with varus stress test, reverse pivot shift test, dial test at 30° and 90° of knee flexion, and external rotation recurvatum test are performed. Clinical maneuvers typically have increased varus, external rotation, and recurvatum laxities.13
Varus malalignment in chronic PLC injuries should be addressed with a biplanar osteotomy before ligament reconstruction. Failure to address malalignment can lead to reconstruction graft failure.
Varus stress radiographs are performed at 20° to 30° of knee flexion. Stress radiographs are essential for the objective diagnosis of PLC lesions and have been shown to be a reliable and reproducible method to evaluate the severity of these injuries.14 Lateral gapping is obtained by measuring the shortest distance between the subchondral bone surface of the most distal aspect of the lateral femoral condyle and the corresponding tibial plateau. The current diagnostic algorithm of the senior author (blinded for review) for an isolated complete fibular collateral ligament tear is a side-to-side difference of 2.7 to 4.0 mm, whereas a difference greater than 4 mm represents an associated grade III PLC injury.
Medial opening wedge PTO can also be used to treat patients with chronic ACL tears. In these circumstances, patients with concurrent medial compartment osteoarthritis or those with an increased sagittal plane tibial slope may also benefit from a biplanar PTO that corrects both the varus malalignment and decreases the tibial slope concurrently.
In patients with concomitant posterior cruciate ligament (PCL) injuries, bilateral kneeling posterior stress radiographs to measure posterior tibial translation are performed preoperatively.15 In general, the literature reports that a complete isolated PCL tear has between 8 and 11 mm of increased posterior translation compared to the normal contralateral side. Furthermore, concurrent ligament injuries in addition to the PCL result in posterior tibial translation of 12 mm or more compared to the contralateral side.15 Medial opening wedge PTO can be used in PCL-deficient knees with medial compartment arthritis or those with a flat (decreased) sagittal plane tibial slope.
Surgical Indications
Medial opening wedge PTO is primarily indicated in relatively young active patients with genu varus malalignment with either (1) isolated medial compartment gonarthrosis of the knee or (2) chronic PLC or chronic ACL deficiencies. These patients might be considered for a staged procedure with the PTO being performed prior to ligament reconstruction.
Contraindications include lateral compartment osteoarthritis or meniscal deficiency, rheumatoid arthritis, open growth plates, severely limited range of motion (knee flexion less than 90° and a flexion contracture greater than 10°), severe patellofemoral symptoms, or patients with patella baja because an osteotomy may increase the forces on articular cartilage in these patients.12, 16 Of note, patients that use nicotine-derived products should be discouraged from undergoing this procedure because of the high risk of nonunion.15
Surgical Technique
A detailed demonstration of the surgical procedure is shown in Video 1.
Patient Positioning
When performed in isolation, the patient is placed supine on the operating table and induced with general anesthesia. A bilateral knee examination under anesthesia is performed. A well-padded high-thigh tourniquet (Zimmer, Warsaw, IN) is placed on the operative leg and then a bump is placed under the knee so that it rests at approximately 30° of flexion. The contralateral leg is secured to the table in full extension with a leg holder (Mizuho OSI, Union City, CA) and a pneumatic compression device (Covidien Medtronic, Irvine, CA) is placed around the lower leg. When performed with a concurrent arthroscopic procedure, the operative leg can be left hanging free during the arthroscopic procedure (Fig 3) and repositioned before starting the osteotomy.
Fig 3.

Intraoperative photograph of a patient sterilely prepared and draped positioned supine on the operating table with the operative leg secured in a leg holder and the foot of the bed lowered to allow for full mobility of the lower extremity. A marking pen is used to outline the proposed incision medial opening wedge proximal tibial osteotomy on the anteromedial aspect left knee (purple marks). The incision is performed midway between the tibial tubercle and posteromedial border of the tibia approximately 6 to 8 cm long.
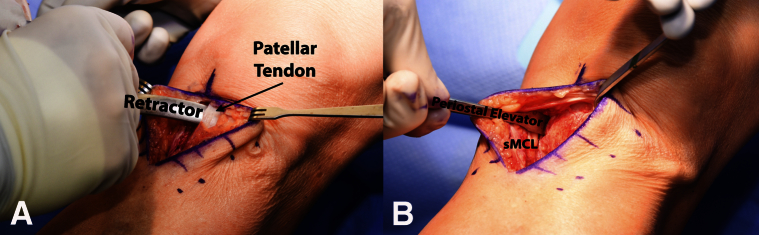
Surgical Approach
A proximal anteromedial incision is performed midway between the tibial tubercle and posteromedial border of the tibia approximately 6 to 8 cm long (Fig 3). Sharp dissection is carried down to the bone to avoid devascularization of the skin flaps. The distal aspect of the patellar tendon and superficial medial collateral ligaments are identified and protected. A subperiosteal dissection is performed anteriorly under the infrapatellar bursa and patellar tendon and then a retractor is inserted (Fig 4A). Posteromedially, a subperiosteal dissection is performed under the superficial medial collateral ligament and the popliteus musculature (Fig 4B) and a radiolucent retractor (Arthrex, Naples, FL) is placed to protect the neurovascular bundle.
Fig 4.
Intraoperative picture of a left knee following an anteromedial incision showing (A) the placement of a retractor to protect the patellar tendon from the sharp instruments used to perform the osteotomy and (B) the use of a periosteal elevator on the posteromedial aspect of the tibia to dissect the soft tissues and facilitate further protection by a radiolucent retractor. (sMCL, superficial medial collateral ligament.)
Tibial Osteotomy
Two guide pins (Arthrex) are inserted roughly parallel to the joint line, or angled slightly cephalad in the coronal plane, just distal to the tibial metaphyseal flare (Fig 5). In the sagittal plane, the guide pins approximate the desired tibial slope. Additionally, it is important to maintain a minimum of approximately 1.5 cm of bone between the articular cartilage and the osteotomy to minimize the risk of an intra-articular fracture and to leave sufficient bone stock for hardware fixation. An osteotomy guide (Arthrex) is inserted over the guide pins, creating a straight line to use for the osteotomy.
Fig 5.
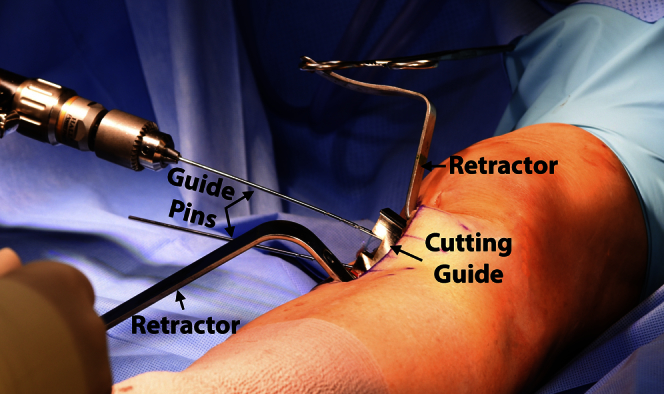
Intraoperative photograph of a left knee during the placement of guide pins to support the cutting guide for a medial opening wedge proximal tibial osteotomy. This procedure should be done under fluoroscopic control to ensure the correct placement of the guide and, ultimately, the correct direction of the osteotomy.
An oscillating saw (ConMed, Utica, NY) is used to begin the osteotomy on the medial cortex. Next, osteotomes are used to advance the osteotomy (first, anteromedially with a small osteotome, continuing to the middle cortex with the use of a larger osteotome, and lastly the posteromedial cortex with the small osteotome again (Fig 6). To avoid damaging the lateral cortex, fluoroscopic imaging is used to frequently confirm the position and verify that a lateral bony hinge of approximately 1 cm is maintained.
Fig 6.
Intraoperative photographs of a left knee during the proximal tibial opening wedge osteotomy procedure. These images show the sequence of the osteotomy after the first cut with the saw on a left knee. (A) Anterior cortex, (B) middle aspect of the osteotomy, and (C) posterior cortex. Observe that in both extremities (anterior and posterior), the width of the osteotome lamina is narrower to better control the cuts near important structures.
A spreader device (Arthrex) is used to slowly distract the medial cortex (Fig 7). Lateral fluoroscopic imaging is then used to assess the tibial slope, while anteroposterior imaging is used to assess the coronal plane correction. Once the desired correction is obtained, the spreader is left in place for several minutes to allow for stress relaxation of the lateral cortex. If the lateral tibial cortex is damaged, a staple can be placed to prevent further propagation and stabilize the cortex.
Fig 7.
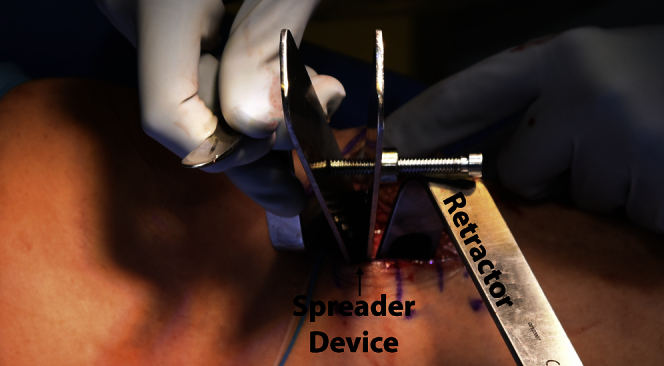
Intraoperative picture of a left knee following completion of the proximal tibial osteotomy. A spreader device used to separate the proximal and distal aspects of the medial osteotomy on a left knee. Once the desired correction is obtained, the spreader is left in place for several minutes to allow for stress relaxation of the lateral cortex.
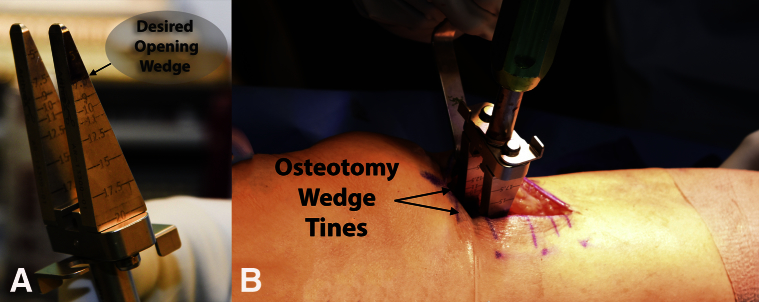
After accommodation of the lateral cortex, the spreader is removed and 2 calibrated osteotomy tines (Arthrex) (previously demarcated to the planned opening height with a surgical marking pen) attached to a handle are advanced into the osteotomy site using gentle mallet strikes to confirm and sustain the desired amount of medial opening prior to plate positioning (Fig 8). The handle and one of the tines are removed according to the desired placement of the plate.
Fig 8.
(A) Intraoperative photograph of the calibrated osteotomy wedge device after having the desired amount of opening wedge marked with a surgical pen. (B) Intraoperative photograph of a left knee with insertion of the osteotomy wedge into the site of the osteotomy on the anteromedial tibia to confirm and sustain the desired amount of opening.
An angled wedge plate (conventional Puddu plate; Arthrex) is secured along the medial cortex, with two 4.5-mm cortical screws (Synthes, West Chester, PA) distally and two 6.5-mm fully threaded cancellous screws (Synthes) proximally (Fig 9). After 1 screw is inserted proximally and distally, the remaining tine is removed, and the other 2 screws secured. The plate may need to be bent to properly conform to the tibia. After plate fixation, the knee is placed into hyperextension, and a large Richards staple is placed anteriorly to prevent the sagittal plane correction from altering postoperatively12 (Fig 10). Opteform allograft (RTI Biologics, Alachua, FL) previously heated to 120° F (to induce malleability of the graft, such that it can be easily packed into the osteotomy site) is then inserted (Fig 11). Pearls/pitfalls and advantages/disadvantages to this procedure are listed in Tables 1 and 2, respectively.
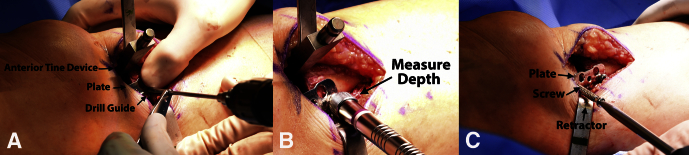
Fig 9.
Intraoperative images showing fixation of the proximal tibia osteotomy contoured plate into the osteotomy site on a left knee: (A) surgical image of a left knee showing drilling of the screw tunnel into the distal aspect of the plate, (B) image of the same surgical knee following drilling of the screw tunnel showing measurement of the appropriate screw length with a depth gage, and (C) intraoperative photo of the same surgical knee showing placement of a fully threaded nonlocking screw into the proximal aspect of the plate. Observe that one of the tine devices is kept in place to sustain the desired opening while the plate is initially fixed.
Fig 10.
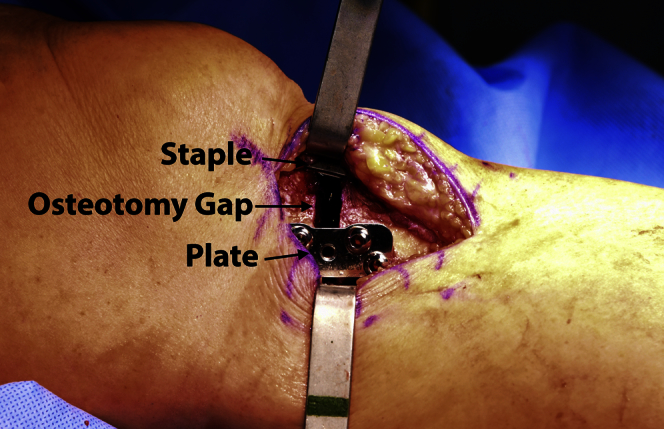
Intraoperative image of the anteromedial aspect of a left knee following proximal tibial osteotomy with placement of the osteotomy plate. The plate has been contoured to fit the tibia, and is placed in the posteromedial aspect. A Richards staple has been placed on the anteromedial aspect of the tibia to prevent future migration or movement of the bone.
Fig 11.
Use of bone allograft to fill the gap left by the medial opening wedge osteotomy. (A) Photograph of the bone allograft in its original packaging as it comes from the manufacturer. This allograft has been warmed to 120° F to ensure malleability for later packing into the proximal tibial defect. (B) Intraoperative image of the anteromedial aspect of a left knee after proximal tibial osteotomy. The previously prepared allograft is packed into the osteotomy site.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| The use of a radiolucent retractor to protect the posterior neurovascular structures allows the surgeon to fluoroscopically access the osteotomy without having to remove the retractor to verify pin or osteotome position. | Opening proximal tibial osteotomy has been reported to increase the posterior tibial slope. Measuring the sagittal slope preoperatively helps planning the best position for the plate |
| Slow progression in the opening of the osteotomy using a specific spreader device and leaving it in place for 5 minutes to allow for stress relaxation of the lateral cortex can minimize the risk of an undesired fracture | Intra-articular tibial fracture is a possible complication. Keeping at least 1.5 cm of bone between the osteotomy and the cartilage on the coronal view minimizes this risk |
| The fixation plate may need to be bent to better conform to the tibia surface | Extra-articular fracture extending to the lateral tibial cortex may happen. Leave 1 cm of bone bridge on the lateral side to avoid this complication. |
| Be aware of the bowl shape of the medial tibial plateau when placing the proximal screws to avoid damage to the joint. | If the lateral tibial cortex is damaged, a staple can be placed to prevent further propagation and stabilize the cortex |
| Placing a large Richards staple anteriorly while hyperextending the knee prevents the sagittal plane correction from altering postoperatively | Consolidation problems may happen with opening wedge osteotomies. Preserving local biology and filling the gap with bone graft when it is greater than 10 mm minimizes the risk of this complication. |
| Place an immobilizer brace after surgery to prevent loss of correction but begin early assisted knee mobilization to prevent adhesions. | Advise your patient to avoid smoking and the use of nicotine products to prevent consolidation problems. |
Table 2.
Advantages and Limitations
| Advantages | Limitations |
|---|---|
| Prevents stretching and failure of the grafts in cases of concomitant chronic PLC or ACL instabilities and varus malalignment | Risk of tibial fracture |
| Possibility to perform a biplanar correction, which can be adjusted according to the instability | Need for an 8-week period of nonweightbearing |
| In some patients, the correction of varus malalignment reduces the instability complaint | Risk of consolidation problems is higher in opening osteotomies, when compared with lateral closing osteotomies. |
| Opening wedge osteotomies allow for better control of the correction | Big corrections may be better addressed with a distraction opening technique or double osteotomy |
| For treatment of early degenerative disease of the medial compartment, proximal tibial osteotomy can delay the need for a joint replacement procedure. | Big changes in bony anatomy can challenge future conversion to a knee replacement |
ACL, anterior cruciate ligament; PLC, posterolateral corner.
Grafting and Closure
Autologous bone graft may also be used alternatively to allograft. Fluoroscopic images are obtained to verify if the screws are of appropriate length, the osteotomy site is thoroughly packed with bone graft, and the lateral cortex remains intact (Fig 12). Finally, the wound is irrigated with normal saline, closed in layers, and placed into an immobilizer brace.
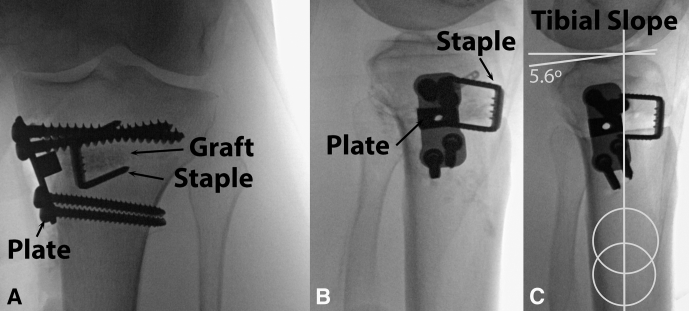
Fig 12.
Final fluoroscopic images following medial opening wedge proximal tibial osteotomy on a left knee. (A) Anteroposterior view showing the plate, the screws, the staple, and the bone graft packed into the gap. (B) Lateral view of the same knee and (C) measurement of the tibial slope.
Postoperative Rehabilitation
Postoperatively, the patient is nonweightbearing for 8 weeks and a knee immobilizer brace (Össur, Foothill Ranch, CA) is worn during this period. Starting on postoperative day 1, a supervised physical therapy program is initiated. Particular emphasis is placed on quadriceps activation. Quadriceps sets and straight leg raises are to be performed 3 to 5 times daily. Passive range of motion should be limited from 0° to 90° of knee flexion during the first 2 weeks. After 8 weeks, weightbearing is gradually increased based on clinical and radiographic evidence of bone healing. An example of the rehabilitation protocol can be found in Figure 13.
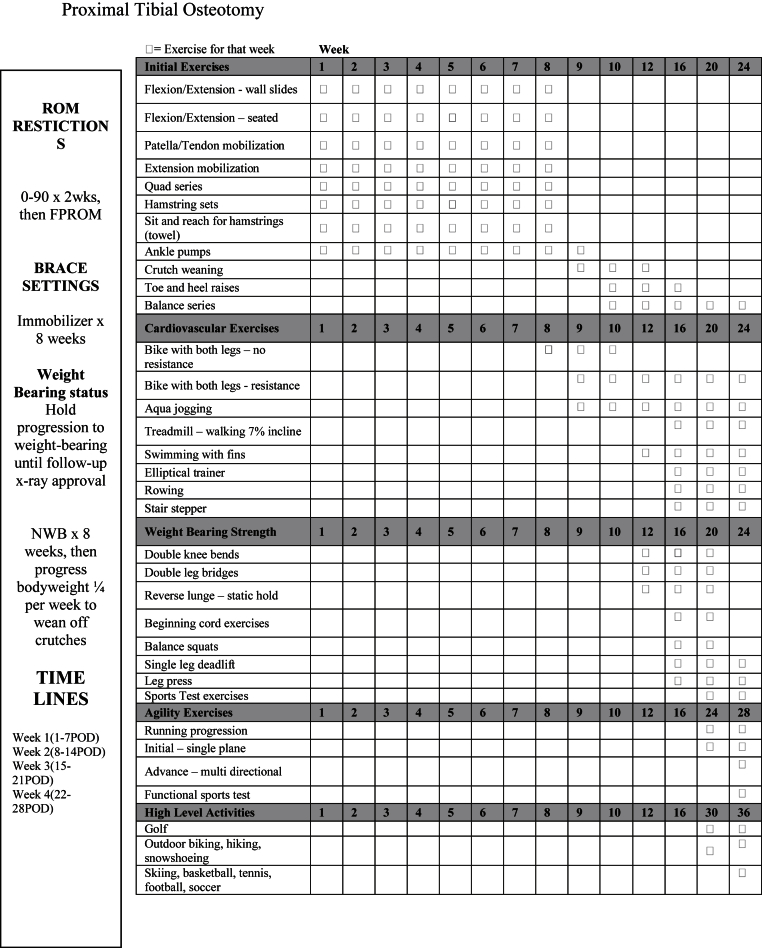
Fig 13.
Physical therapy protocol example. (FPROM, full passive range of motion; NWB, non–weight bearing; POD, postoperative day; ROM, range of motion.)
Discussion
The proximal tibial opening wedge osteotomy technique has been reported to produce significant improvement in subjective and objective clinical outcome scores when treating medial compartment overload and chronic instabilities.8 PTO has recently expanded its indications for treatment to include medial compartment overload or early degenerative changes,17 chronic instabilities (such as PLC instability),8 ligament reconstruction failure due to malalignment,17 and finally to protect a concurrent ligament reconstruction.18
It has been reported that performing a PTO to treat symptomatic medial compartment osteoarthritis in selected patients has a survival rate of 94% at 3.6 years postoperatively.11 The mean preoperative modified Cincinnati Knee Score improved from 42.9 (range, 8 to 63) to 65.1 (range, 10 to 100); significant differences were also observed in International Knee Documentation Committee scores both for effusions and for the single-leg hop. A recent systematic review reported that PTO reduces pain and improves knee function in patients with medial compartmental osteoarthritis of the knee with no difference between osteotomy techniques. Moreover, there was no evidence of whether an osteotomy is more effective than an alternative surgical treatment such as unicompartmental knee replacement or nonoperative treatment.1
When treating ligamentous instability, PTO can be performed in isolation, with simultaneous ligament reconstruction or as a staged procedure with PTO first followed by ligament reconstruction in cases of persistent instability. A recent systematic review19 reported favorable outcomes of combined PTO and ligamentous procedures. Studies with combined ACL reconstruction and PTO tended to report higher postoperative activity levels when compared with PTO alone. A prospective study of 21 patients with combined grade III PLC injuries and varus malalignment by Arthur et al.8 reported that 38% of patients did not require ligament reconstruction after PTO.
An additional advantage of this osteotomy is the possibility to perform biplanar corrections, which is vital to restore knee stability in certain cases. Opening wedge PTO has been reported to increase the tibial slope.8, 12 The degree of slope change also depends on the positioning of the plate: anteriorly placed plates increase the sagittal plane slope, and posteriorly placed plates decrease the slope.12
Regarding the material used to fill the gap created by the osteotomy, several compounds have been used such as autograft, allograft, synthetic bone substitutes (hydroxyapatite, β-tricalcium phosphate, a combination of both and bone cement) with or without platelet-rich plasma, growth factors, and bone marrow aspirate concentrate.20, 21 To date, bone graft is considered the gold standard bone filling material because of its osteoconductive, osteoinductive, and osteogenic properties.21 Bone substitute avoids donor site morbidity associated with bone autograft; however, bone substitute provides weaker resistance to compressive loading forces.20, 22 It has been reported that gaps of less than 10 mm can be left unfilled because no pseudarthrosis or loss of correction was observed in a series of 112 patients.23
There are several technical considerations as well as advantages and drawbacks in using this technique, and these are highlighted in Tables 1 and 2. Further studies are needed to assess the long-term outcomes when using PTO to help correct ligamentous instability. Nevertheless, we recommend our approach for medial opening wedge PTO and encourage further studies by other groups to evaluate our surgical technique and long-term subjective and objective patient outcomes for both medial compartment overload and treatment of chronic instability.
Footnotes
The authors report the following potential conflict of interest or source of funding: R.F.L. receives support from Arthrex; Ossur; Siemens, Smith & Nephew; Health East, Norway; and an NIH R13 grant for biologics.
Supplementary Data
The patient is placed supine on the operating table and induced with general anesthesia. A well-padded high-thigh tourniquet is placed on the operative leg and then a bump is placed under the knee so that it rests at approximately 30° of flexion. A proximal anteromedial incision is performed. A subperiosteal dissection is performed anteriorly under the infrapatellar bursa and patellar tendon and then a retractor is inserted. Posteromedially, a subperiosteal dissection is performed under the superficial medial collateral ligament and the popliteus musculature and a radiolucent retractor is placed to protect the neurovascular bundle. Two guide pins are inserted parallel to the joint line in the coronal plane, just distal to the tibial metaphyseal flare. An osteotomy guide is inserted over the guide pins, creating a straight line to use for the osteotomy. An oscillating saw is used to begin the osteotomy on the medial cortex, which is then followed by osteotomes. A spreader device is inserted and slowly opened until the desired correction is obtained, at which point the spreader is left in place for several minutes to allow for stress relaxation of the lateral cortex. The spreader is removed and 2 wedged tines attached to a handle are inserted into the osteotomy site. After re-establishing the desired degree of correction, the handle and one of the tines are removed. An angled wedge plate is then secured along the medial cortex, with two 4.5-mm cortical screws distally and two 6.5-mm fully threaded cancellous proximally. After 1 screw is inserted proximally and distally, the remaining tine is removed, and the other 2 screws secured. After plate fixation, a large staple is placed anteriorly while hyperextending the knee to prevent the sagittal plane correction from altering postoperatively. Opteform allograft is then packed into the osteotomy site. Anteroposterior and lateral fluoroscopic imaging is used to verify the hardware position and degree of correction.
References
- 1.Brouwer R.W., Huizinga M.R., Duivenvoorden T. Osteotomy for treating knee osteoarthritis. Cochrane Database Syst Rev. 2014;12:CD004019. doi: 10.1002/14651858.CD004019.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wolfe S.A., Brueckmann F.R. Conservative treatment of genu valgus and varum with medial/lateral heel wedges. Indiana Med. 1991;84:614–615. [PubMed] [Google Scholar]
- 3.Asik M., Sen C., Kilic B., Goksan S.B., Ciftci F., Taser O.F. High tibial osteotomy with Puddu plate for the treatment of varus gonarthrosis. Knee Surg Sports Traumatol Arthrosc. 2006;14:948–954. doi: 10.1007/s00167-006-0074-1. [DOI] [PubMed] [Google Scholar]
- 4.Wright J.M., Crockett H.C., Slawski D.P., Madsen M.W., Windsor R.E. High tibial osteotomy. J Am Acad Orthop Surg. 2005;13:279–289. doi: 10.5435/00124635-200507000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Giuseffi S.A., Replogle W.H., Shelton W.R. Opening-wedge high tibial osteotomy: Review of 100 consecutive cases. Arthroscopy. 2015;31:2128–2137. doi: 10.1016/j.arthro.2015.04.097. [DOI] [PubMed] [Google Scholar]
- 6.DeMeo P.J., Johnson E.M., Chiang P.P., Flamm A.M., Miller M.C. Midterm follow-up of opening-wedge high tibial osteotomy. Am J Sports Med. 2010;38:2077–2084. doi: 10.1177/0363546510371371. [DOI] [PubMed] [Google Scholar]
- 7.Bode G., von Heyden J., Pestka J. Prospective 5-year survival rate data following open-wedge valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2015;23:1949–1955. doi: 10.1007/s00167-013-2762-y. [DOI] [PubMed] [Google Scholar]
- 8.Arthur A., LaPrade R.F., Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: A prospective clinical study. Am J Sports Med. 2007;35:1844–1850. doi: 10.1177/0363546507304717. [DOI] [PubMed] [Google Scholar]
- 9.Marriott K., Birmingham T.B., Kean C.O., Hui C., Jenkyn T.R., Giffin J.R. Five-year changes in gait biomechanics after concomitant high tibial osteotomy and ACL reconstruction in patients with medial knee osteoarthritis. Am J Sports Med. 2015;43:2277–2285. doi: 10.1177/0363546515591995. [DOI] [PubMed] [Google Scholar]
- 10.McNamara I., Birmingham T.B., Fowler P.J., Giffin J.R. High tibial osteotomy: Evolution of research and clinical applications—A Canadian experience. Knee Surg Sports Traumatol Arthrosc. 2013;21:23–31. doi: 10.1007/s00167-012-2218-9. [DOI] [PubMed] [Google Scholar]
- 11.Laprade R.F., Spiridonov S.I., Nystrom L.M., Jansson K.S. Prospective outcomes of young and middle-aged adults with medial compartment osteoarthritis treated with a proximal tibial opening wedge osteotomy. Arthroscopy. 2012;28:354–364. doi: 10.1016/j.arthro.2011.08.310. [DOI] [PubMed] [Google Scholar]
- 12.LaPrade R.F., Oro F.B., Ziegler C.G., Wijdicks C.A., Walsh M.P. Patellar height and tibial slope after opening-wedge proximal tibial osteotomy: A prospective study. Am J Sports Med. 2010;38:160–170. doi: 10.1177/0363546509342701. [DOI] [PubMed] [Google Scholar]
- 13.LaPrade R.F., Wentorf F. Diagnosis and treatment of posterolateral knee injuries. Clin Orthop Relat Res. 2002;(402):110–121. doi: 10.1097/00003086-200209000-00010. [DOI] [PubMed] [Google Scholar]
- 14.LaPrade R.F., Heikes C., Bakker A.J., Jakobsen R.B. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. J Bone Joint Surg Am. 2008;90:2069–2076. doi: 10.2106/JBJS.G.00979. [DOI] [PubMed] [Google Scholar]
- 15.Jackman T., LaPrade R.F., Pontinen T., Lender P.A. Intraobserver and interobserver reliability of the kneeling technique of stress radiography for the evaluation of posterior knee laxity. Am J Sports Med. 2008;36:1571–1576. doi: 10.1177/0363546508315897. [DOI] [PubMed] [Google Scholar]
- 16.Kolb W., Guhlmann H., Windisch C., Kolb K., Koller H., Grutzner P. Opening-wedge high tibial osteotomy with a locked low-profile plate. J Bone Joint Surg Am. 2009;91:2581–2588. doi: 10.2106/JBJS.H.01047. [DOI] [PubMed] [Google Scholar]
- 17.Bonasia D.E., Governale G., Spolaore S., Rossi R., Amendola A. High tibial osteotomy. Curr Rev Musculoskelet Med. 2014;7:292–301. doi: 10.1007/s12178-014-9234-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zaffagnini S., Bonanzinga T., Grassi A. Combined ACL reconstruction and closing-wedge HTO for varus angulated ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc. 2013;21:934–941. doi: 10.1007/s00167-013-2400-8. [DOI] [PubMed] [Google Scholar]
- 19.Cantin O., Magnussen R.A., Corbi F., Servien E., Neyret P., Lustig S. The role of high tibial osteotomy in the treatment of knee laxity: A comprehensive review. Knee Surg Sports Traumatol Arthrosc. 2015;23:3026–3037. doi: 10.1007/s00167-015-3752-z. [DOI] [PubMed] [Google Scholar]
- 20.Chahla J., Arroquy D., Rodriguez G.G. Osteotomía Valguizante Tibial Alta: Comparación de Resultados con el Uso de Aloinjerto y Sustituto Óseo. Artrosc (B Aires) 2014;21:89–94. [Google Scholar]
- 21.Amendola A., Bonasia D.E. Results of HTO in medial OA of the knee. In: Bonnin M., Amendola N.A., Bellemans J., MacDonald S.J., Menetrey J., editors. The knee joint. Springer; Paris: 2012. pp. 633–641. [Google Scholar]
- 22.Aryee S., Imhoff A.B., Rose T., Tischer T. Do we need synthetic osteotomy augmentation materials for opening-wedge high tibial osteotomy. Biomaterials. 2008;29:3497–3502. doi: 10.1016/j.biomaterials.2008.05.027. [DOI] [PubMed] [Google Scholar]
- 23.Lobenhoffer P., Agneskirchner J.D. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2003;11:132–138. doi: 10.1007/s00167-002-0334-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed supine on the operating table and induced with general anesthesia. A well-padded high-thigh tourniquet is placed on the operative leg and then a bump is placed under the knee so that it rests at approximately 30° of flexion. A proximal anteromedial incision is performed. A subperiosteal dissection is performed anteriorly under the infrapatellar bursa and patellar tendon and then a retractor is inserted. Posteromedially, a subperiosteal dissection is performed under the superficial medial collateral ligament and the popliteus musculature and a radiolucent retractor is placed to protect the neurovascular bundle. Two guide pins are inserted parallel to the joint line in the coronal plane, just distal to the tibial metaphyseal flare. An osteotomy guide is inserted over the guide pins, creating a straight line to use for the osteotomy. An oscillating saw is used to begin the osteotomy on the medial cortex, which is then followed by osteotomes. A spreader device is inserted and slowly opened until the desired correction is obtained, at which point the spreader is left in place for several minutes to allow for stress relaxation of the lateral cortex. The spreader is removed and 2 wedged tines attached to a handle are inserted into the osteotomy site. After re-establishing the desired degree of correction, the handle and one of the tines are removed. An angled wedge plate is then secured along the medial cortex, with two 4.5-mm cortical screws distally and two 6.5-mm fully threaded cancellous proximally. After 1 screw is inserted proximally and distally, the remaining tine is removed, and the other 2 screws secured. After plate fixation, a large staple is placed anteriorly while hyperextending the knee to prevent the sagittal plane correction from altering postoperatively. Opteform allograft is then packed into the osteotomy site. Anteroposterior and lateral fluoroscopic imaging is used to verify the hardware position and degree of correction.