Abstract
Impulsivity is posited to be a key part of the externalizing spectrum during childhood, but this idea has received minimal empirical attention. The goal of the present investigation was to utilize network analysis to determine whether behavioral impulsivity symptoms are key components of the externalizing network across several developmental periods from preschool into adolescence. Participants were 109 preschoolers (64% male) ages 3 to 6, 237 children (59% male) ages 6 to 9, 372 children (59% male) ages 10 to 13, and 357 adolescents (59% male) ages 13 to 17 and their parents. Parents completed ratings of Attention-Deficit/Hyperactivity Disorder (ADHD) and Oppositional Defiant Disorder (ODD) symptoms on a well-validated rating scale. Network analyses indicated that ADHD and ODD were somewhat differentiated in preschool, becoming united by behavioral impulsivity symptoms during early childhood, and then differentiating into inattention versus externalizing clusters later during childhood and in adolescence. Behavioral impulsivity symptoms were core to the externalizing spectrum across most developmental periods, but core inattentive and ODD symptoms were also identified in line with progressive differentiation. These results suggest the increasing importance of impulsivity symptoms across development, explaining externalizing comorbidity and potentially serving as a viable target for childhood interventions for externalizing problems.
Keywords: Impulsivity, externalizing disorder, child development, adolescence
Network analysis provides a new paradigm for understanding psychopathology. It shifts the field of psychology dramatically away from a latent variable approach to the conceptualization of psychopathology, which suggests that a latent variable causes a set of manifest symptoms, consistent with a disease model of psychopathology (Borsboom & Cramer, 2013). Instead, network analysis suggests that symptoms themselves may be causally related at a symptom level, allowing for additional modeling of complexity among symptoms (Borsboom & Cramer, 2013). Therefore, network analysis provides a complex way of thinking of disorders as conceptualized as systems of causally related symptoms rather than assuming that symptoms are merely downstream effects of a causal latent disorder.
Network analysis may thus provide an innovative and promising means by which to test symptom interrelations across development in order to evaluate models of potential causality as they unfold over time. That is, network analytic approaches might extend our understanding of psychopathology gleaned from a latent factor approach by evaluating potential causal networks of symptoms rather than assuming that disorders arise from a common cause (as in a disease model; Borsboom & Cramer, 2013). This type of analysis provides insight into how symptoms of a disorder relate to each other and which symptoms might be at the core of the disorder. Therefore, network analysis (a) allows for the examination of how individual symptoms across age ranges change across developmental age groups and (b) provides information on which of these symptoms are at the core of the symptom network (Borsboom & Cramer, 2013). Thus, it is possible to test if there are common core symptoms (such as behavioral impulsivity) across developmental time periods. This type of analysis is impossible using other statistical methods, such as latent variable analyses, which weights each of the symptoms equally.
Such an approach could potentially be useful for examination of the development of the externalizing spectrum. Latent variable approaches have suggested that the externalizing spectrum in adulthood consists of conduct problems, substance abuse, antisocial behavior, and aggression (Krueger et al., 2002; Krueger, Markon, Patrick, Benning, & Kramer, 2007; Krueger, Markon, Patrick, & Iacono, 2005). Yet, the developmental precursors to this externalizing spectrum have been less well-studied (Tackett, 2010). It is theorized that oppositional-defiance and hyperactivity-impulsivity may form such an externalizing spectrum during childhood (Burt, McGue, Krueger, & Iacono, 2005; Lahey et al., 2004). However, this theory has only been minimally tested at present, with two latent variable studies finding support for a bifactor structure of a general externalizing factor with co-existing specific factors of Oppositional Defiant Disorder (ODD) and Attention-Deficit/Hyperactivity Disorder (ADHD; e.g., Burns, Moura, Beauchaine, & McBurnett, 2014; Lee, Burns, Beauchaine, & Becker, 2015).
Beauchaine's trait impulsivity theory suggests impulsivity may be an underlying liability factor for the externalizing spectrum in childhood and adulthood that can explain heterotypic continuity across common externalizing problems across development (Beauchaine, Hinshaw & Pang, 2010). During childhood, externalizing behavior exhibits prominent developmental change over time with hyperactivity peaking early, and oppositional-defiance appearing soon thereafter, followed by inattention at school entry (Hart, Lahey, Loeber, Applegate, & Frick, 1995; Olson, 2002). Most conduct problems do not emerge until near or during adolescence (Moffitt, 1993). This developmental progression of problems across the externalizing spectrum is referred to as heterotypic continuity, or different manifestations of the same underlying liability (reviewed by Beauchaine et al., 2010). Theoretical work suggests that such an externalizing spectrum may be underpinned by impulsivity (Beauchaine et al., 2010), which is related to the trait of daring (Lahey et al., 2008) and similar to an adult disinhibition factor (Young et al., 2009), also known as constraint (Krueger et al., 2002). Like adulthood disinhibition, this impulsivity factor is also thought to be largely influenced by genetic factors (Krueger et al., 2002). Yet, other work suggests prominent shared environmental influences on this shared externalizing spectrum (Burt et al., 2005). Therefore, such a factor seems to be influenced by both genetic and environmental influences.
Alternatively conceptualized as behavioral impulsivity (Beauchaine et al., 2010), affective impulsivity (Whiteside & Lynam, 2001), disinhibition (Nigg, 2000; Young et al., 2009), or affective/reactive control (Martel, 2009; Wehmeier, Schacht, & Barkley, 2010), such bottom-up facets of impulsivity may explain comorbidity among externalizing problems across development. Bottom-up facets of impulsivity may exhibit particularly salient linkages to hyperactivity-impulsivity, as well as oppositional-defiance and conduct problems, compared to inattention which may be more closely linked to executive dysfunction or effortful control (i.e., top-down control: Martel, Nigg & von Eye, 2009; Nigg & Casey, 2005). Recent empirical work using a latent variable approach is consistent with such theory, suggesting that a single general latent factor underlies ADHD and ODD, with such a factor accounting for all of the variance in hyperactivity-impulsivity scores, and over half of the variance in oppositional-defiance and inattention scores (Burns et al., 2014). Furthermore, the sluggish cognitive tempo factor, related to ADHD inattention, exhibited discriminant validity by loading onto its own factor and predicting academic impairment (Lee et al., 2015).
Isolation of factors underpinning such an externalizing spectrum is of critical importance to determine etiological or risk factor(s) accounting for the high levels of comorbidity among these disorders (i.e., ADHD, ODD). Although some work has evaluated such ideas using a latent variable approach (Burns et al., 2014; Lee et al., 2015), no work to date has utilized a network analytic approach to determine core symptoms of the externalizing spectrum across childhood development. Yet, a network analysis approach can provide a critical test of whether behavioral impulsivity symptoms are in fact core, or central, to the network of externalizing symptoms across development periods. The current study will be the first to test whether behavioral impulsivity symptoms are core to externalizing symptoms across developmental age ranges from preschool into late adolescence using network analysis, and it is hypothesized that behavioral impulsivity symptoms will be core, or central, to the externalizing network across development.
METHOD
Participants
Overview
Preschoolers, children, and adolescents, along with their parents and teachers participated in the current study. Participants were recruited from the community and completed a multistage screening and diagnostic procedure including informed consent consistent with APA, NIH, and IRB guidelines.
Preschool sample
Preschool participants were 109 young children between the ages of three and six and their primary caregivers, hereafter referred to as parents. Sixty-four percent of the sample was male, and 36% of the sample was non-White (28% African American and 8% other including Latino, American Indian, and mixed race children). Annual family income exhbited a wide range (from below $20,000 to over $100,000 US dollars. Based on multistage and comprehensive diagnostic screening procedures (detailed below), children were recruited into two groups: ADHD (n = 61) and typically developing non-ADHD children (n = 48). The non-ADHD group included children with subthreshold symptoms, consistent with research suggesting that ADHD may be better captured by continuous dimensions than categorical diagnosis (Haslam et al., 2006; Marcus & Barry, 2011).
Early childhood sample
There were 237 child participants (59% male; 24% ethnic minority) between the ages of 6 and 9. Annual family income exhibited a wide range from below $20,000 to over $500,000 US dollars. Children were initially included in one of two groups: ADHD (n = 130) and typically developing non-ADHD comparison youth (i.e., controls, n = 107), though those with situational or sub-threshold ADHD were included to parallel the preschool selection strategy.
Middle Childhood Sample
There were 372 children (59% male; 26% ethnic minority) between the ages of 10 and 13. Annual family income exhibited a wide range from below $20,000 to over $500,000 US dollars. Children were included in one of two groups: ADHD (n = 205) and typically developing non-ADHD comparison youth (controls, n = 167), including those with situational or sub-threshold ADHD in order to parallel the preschool selection strategy.
Adolescent sample
Adolescent sample participants were 357 youth (59% male) between ages 13 and 17. Twenty-two percent identified themselves as ethnic minorities. Families exhibited a wide range of incomes. Participants included those who met research criteria for ADHD (n = 144) and typically developing non-ADHD youth, including subthreshold cases (n = 213) in order to parallel the preschool selection strategy.
Identification and Recruitment
All participants were recruited using a diverse set of recruitment strategies including radio, newspaper, and movie theater advertisements and general mailings or flyers targeting individuals who thought they or their children might have attention problems and/or advertising a study of the development of attention, as well as mailings to local clinics (although less than 10% of the sample came from clinic advertisements), in order to recruit a representative sample of community volunteers. Prospective participants then underwent a standard multi-gate screening process to identify cases eligible for the study. At stage 1, parents of participants completed a telephone screen to assess eligibility. To be eligible to participate in the study, participants were required to be a native English speaker and without a sensorimotor disability, neurological illness, or a current prescription for antidepressant, antipsychotic, or anticonvulsant medication. These eligibility criteria were chosen to ensure study participants could adequately understand task instructions and to eliminate the confounds of comorbid conditions and medication use that could affect cognitive performance. Participants who passed this stage of screening went on to a second stage of screening.
At stage 2, parents completed semi-structured interviews and standardized normative rating scales, described below, to ascertain ADHD and comorbid psychopathology. Parents completed either the Diagnostic Interview Schedule for Children (DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000), the Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS-E; Puig-Antich & Ryan, 1986), or the Kiddie Disruptive Behavior Disorders Schedule (K-DBDS: Leblanc et al., 2008). In addition, parents and teachers completed the following standardized rating scales: Child Behavior Checklist /Teacher Report Form (CBCL/TRF; Achenbach, 1991) and the ADHD Rating Scale (ADHD-RS; DuPaul, Power, Anastopolous, & Reid, 1998).
For all participants, a clinical diagnostic team consisting of a board certified psychiatrist and licensed clinical psychologist then used this information to arrive at a “best estimate” diagnosis (Faraone, 2000). Each member reviewed ADHD symptoms counts and impairment ratings from the semi-structured interviews and raw scores and t-scores from the rating scales completed by parents and teachers to judge whether ADHD was present or absent, ADHD subtype (if applicable), and comorbid disorders. Each member reviewed information individually to reach a diagnostic decision based on aggregation of all aforementioned information, and then these decisions were compared. In the case of disagreement, consensus was reached by discussion. Inter-rater agreement was satisfactory on presence or absence of ADHD and ODD (κ≥.80).
Measures
ADHD and ODD Symptoms
The 18 ADHD symptoms and 8 ODD symptoms used in primary analyses were rated by parents using a 0 (rarely or never) to 3 (always or very often) rating scale on the DSM-IV-TR ADHD Rating Scale for preschoolers, children, and adolescents, a reliable and valid measure (Barkley & Murphy, 1998; DuPaul et al., 1998). Internal reliability in the current study exhibited alpha of .8 or above for all subscales. Parents were instructed to rate behavior off medication. There was no missing data for symptoms because symptom ratings were required for study participation. Means and standard deviations for individual symptoms were around 1 for all symptoms and all samples.
Data Analytic Plan
A series of networks were computed using the R package qgraph (Epskamp, Cramer, Waldorp, Schmittmann, & Borsboom, 2012). We used the portion of the script and followed procedures provided in the supplemental materials from Borsboom and Cramer (2013). Networks were not specified to be directional, nor did we set a predetermined number of paths or strength of correlations. For each age group (i.e., preschool, early childhood, middle childhood, and adolescence), networks were computed and visualized using different colors to represent inattention, hyperactivity, impulsivity, and ODD. Line thickness in figures represents the strength of the correlation, so the thicker the line, the more strongly related the symptoms. Networks can be visually inspected to show tight clustering of individual symptoms and potential bridge symptoms. Bridge nodes are symptoms that link adjacent symptoms together and are theorized to constitute pathways that could causally connect symptoms or behaviors (pending longitudinal data analysis and experimental design), and these are qualitatively determined based on visual inspection of the network.
Statistical indices, called measures of centrality, were also calculated to quantify aspects of the network, particularly node centrality, using the tnet package in R (Freeman, 1979; Opsahl, Agneessens, & Skvoretz, 2010). We used two indices of centrality: Closeness and Degree. Closeness represents the inverse of the sum of distance to all other nodes; higher numbers indicating that a node is more central to the network relative to the other items. Degree represents the sum of the weights of the relations with which a node is involved and captures the strength of the relations that a node has with all other nodes (Opsahl & Panzarasa, 2009). Again, higher numbers indicate higher centrality. There are as-of-yet no guidelines for how to interpret the relative magnitude of these numbers or how to interpret differences between numbers, with the exception that higher numbers indicate higher centrality relative to the other symptoms. The indices of centrality were used to identify which symptoms are core to the externalizing network.
RESULTS
Preschool Network of Externalizing Spectrum
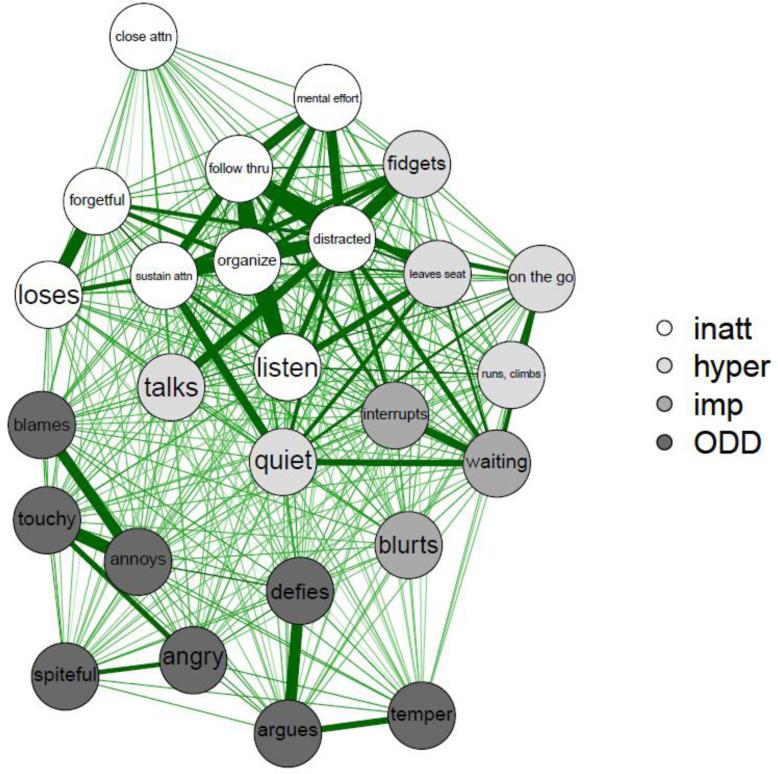
During preschool, as can be seen in Figure 1, there are two clusters of symptoms falling into ADHD and ODD categories, although symptoms are relatively evenly dispersed aside from the diagnostic distinction. ADHD symptoms are evenly distributed with an inattentive/distracted cluster toward the center, and impulsivity symptoms toward one edge with those symptoms most seeming to bridge the ADHD and ODD space. Easily distracted is a central inattentive symptom (closeness=.04, degree=12.97), and Often defies is a central ODD symptom (closeness=.043, degree=12.73), as shown in Table 1. Often interrupts is the core network symptom based on highest indices of closeness (.043) and degree (13.04), consistent with the idea that a behavioral impulsivity symptom is central to the preschool externalizing spectrum.
Figure 1.
Preschool Impulsivity Network
Note. Inatt=Inattention. Hyper=Hyperactivity. Imp=Impulsivity. ODD=Oppositional-Defiance.
Table 1.
Network Indices of Centrality
| Preschool | Early Childhood | Middle Childhood | Adolescence | |||||
|---|---|---|---|---|---|---|---|---|
| Closeness | Degree | Closeness | Degree | Closeness | Degree | Closeness | Degree | |
| Close attn. | .040 | 11.57 | .040 | 13.61 | .039 | 13.99 | .040 | 11.57 |
| Sustain attn. | .039 | 11.03 | .041 | 14.36 | .040 | 14.48 | .039 | 11.03 |
| Listen | .038 | 10.27 | .042 | 14.80 | .041 | 15.15 | .038 | 10.27 |
| Follow thru | .040 | 11.93 | .041 | 14.64 | .040 | 14.90 | .040 | 11.93 |
| Organize | .039 | 11.47 | .039 | 13.65 | .040 | 14.51 | .039 | 11.47 |
| Mental effort | .039 | 11.29 | .040 | 13.82 | .040 | 14.52 | .039 | 11.29 |
| Loses | .040 | 11.86 | .040 | 13.85 | .039 | 14.41 | .040 | 11.86 |
| Distracted | .043 | 12.97 | .039 | 12.94 | .039 | 13.52 | .043 | 12.97 |
| Forgetful | .041 | 12.28 | .041 | 14.43 | .039 | 13.70 | .041 | 12.28 |
| Fidgets | .036 | 9.04 | .040 | 13.77 | .041 | 14.86 | .036 | 9.04 |
| Leaves seat | .035 | 8.37 | .041 | 14.11 | .041 | 14.75 | .035 | 8.37 |
| Runs, climbs | .034 | 8.34 | .036 | 10.90 | .038 | 12.96 | .034 | 8.34 |
| Quiet | .038 | 9.84 | .039 | 12.92 | .039 | 14.12 | .038 | 9.84 |
| On the go | .039 | 10.28 | .042 | 14.46 | .040 | 14.49 | .039 | 10.28 |
| Talks | .040 | 11.38 | .039 | 12.87 | .040 | 14.06 | .040 | 11.38 |
| Blurts | .040 | 11.43 | .041 | 14.09 | .041 | 15.01 | .040 | 11.43 |
| Waiting | .041 | 11.64 | .043 | 15.20 | .041 | 14.94 | .041 | 11.64 |
| Interrupts | .043 | 13.04 | .041 | 13.73 | .040 | 14.19 | .043 | 13.04 |
| Temper | .039 | 11.00 | .037 | 11.49 | .038 | 13.49 | .039 | 11.00 |
| Touchy | .039 | 11.35 | .039 | 12.88 | .040 | 13.99 | .039 | 11.35 |
| Angry | .040 | 11.62 | .037 | 11.62 | .039 | 14.10 | .040 | 11.62 |
| Argues | .040 | 11.86 | .037 | 11.66 | .039 | 13.74 | .040 | 11.86 |
| Defies | .043 | 12.73 | .042 | 14.28 | .042 | 15.36 | .042 | 12.73 |
| Annoys | .038 | 10.45 | .040 | 13.39 | .041 | 14.80 | .038 | 10.45 |
| Blames | .040 | 11.45 | .038 | 11.90 | .040 | 14.49 | .039 | 11.45 |
| Spiteful | .037 | 10.10 | .033 | 9.44 | .036 | 12.20 | .037 | 10.10 |
Note. Closeness represents the distance between each singe node and all other nodes; degree represents the strength of the relationship each node has with all other nodes. Higher numbers are more central to the network. Bolded numbers represent the most central symptoms in each network, and bolded symptoms denote impulsive symptoms.
Early Childhood Network of Externalizing Spectrum
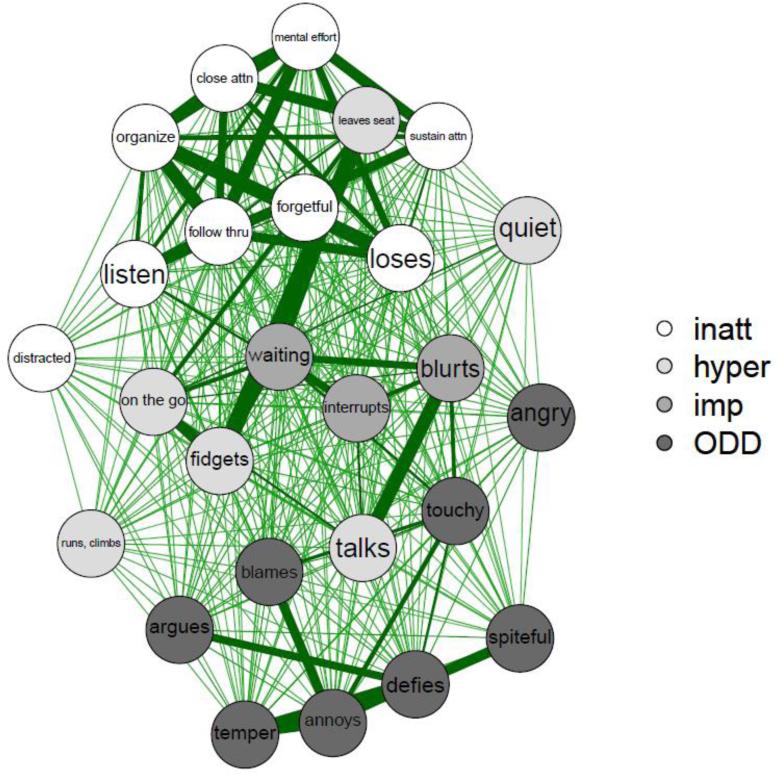
During early childhood, shown in Figure 2, impulsivity symptoms (e.g., Often interrupts; Often blurts; Often has difficulty waiting), as well several hyperactive symptoms (Talks excessively; Often fidgets), fall between the ADHD and ODD clusters. Impulsive symptoms fall at the center of the network. In particular, Difficulty waiting was the core network symptom with closeness of .043 and degree of 15.20. Does not seem to listen was a core inattentive symptoms (closeness=.042, degree=14.80), and Often defies was again the central ODD symptom (closeness=.042, degree=14.28). Again, impulsivity (and hyperactivity) seem to be core to the inattentive and ODD clusters.
Figure 2.
Early Childhood Impulsivity Network
Note. Inatt=Inattention. Hyper=Hyperactivity. Imp=Impulsivity. ODD=Oppositional-Defiance.
Middle Childhood Network of Externalizing Spectrum
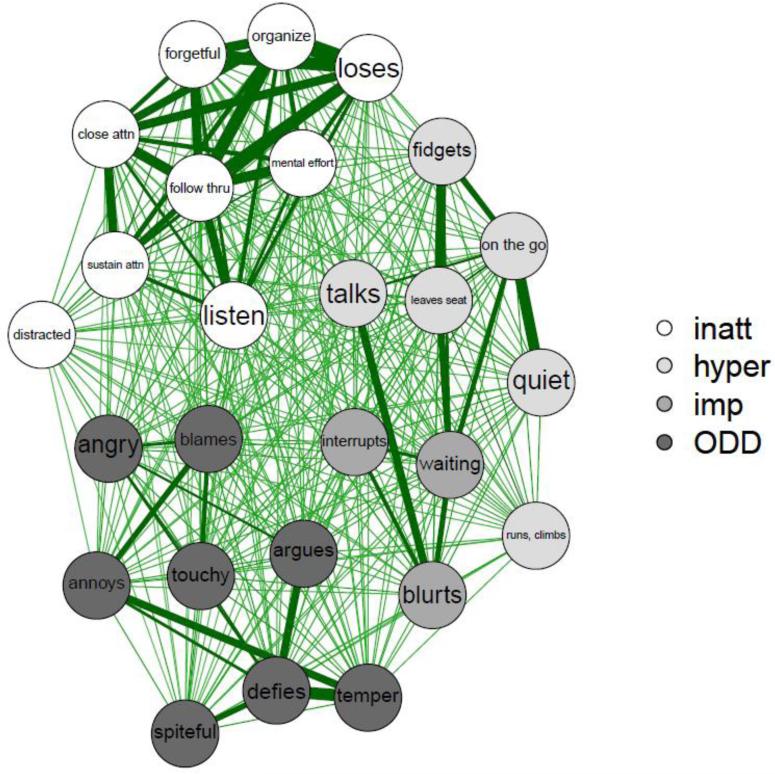
In middle childhood, shown in Figure 3, inattention separates out into its own cluster, ODD forms its own cluster, and hyperactivity-impulsivity forms a third cluster. Impulsivity symptoms fall in between the ODD and hyperactivity clusters. Often blurts out an answer is a core symptom with closeness of .041 and degree of 15.01. However, the inattentive symptom Does not seem to listen and the ODD symptom Often defies exhibit slightly higher closeness (.041 and .042) and degree (15.15 and 15.36 respectively) indices.
Figure 3.
Middle Childhood Impulsivity Network
Note. Inatt=Inattention. Hyper=Hyperactivity. Imp=Impulsivity. ODD=Oppositional-Defiance.
Adolescent Network of Externalizing Spectrum
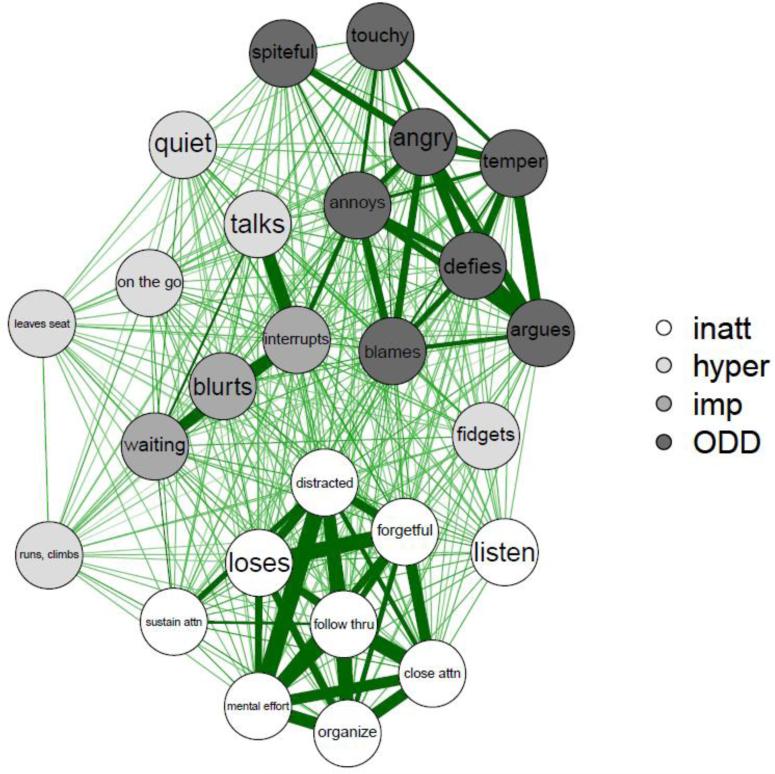
Finally, in adolescence, shown in Figure 4, inattention again is seen as its own cluster with impulsivity items central to the network, connecting hyperactivity and ODD symptoms. Often interrupts is the core symptom of the externalizing spectrum with closeness of .043 and degree of 13.04. Easily distracted is a core symptom in the inattentive cluster (closeness=.043, degree=12.97), and Often defies is the core symptom in the ODD cluster (closeness=.042, degree=12.73).
Figure 4.
Adolescence Impulsivity Network
Note. Inatt=Inattention. Hyper=Hyperactivity. Imp=Impulsivity. ODD=Oppositional-Defiance.
DISCUSSION
The current study was the first study to use network analysis to test whether behavioral impulsivity symptoms are core to the externalizing spectrum across four developmental age ranges from preschool to late adolescence. Behavioral impulsivity symptoms, particularly Often interrupts and Difficulty waiting, appeared to be core to the externalizing spectrum across most of early development with the possible exception of middle childhood. Behavioral impulsivity symptoms were particularly salient as visually central to the externalizing spectrum during early childhood and adolescence. Inattention clustered tightly throughout development and separated from the externalizing cluster later during childhood and into adolescence. Overall, results suggest that targeting behavioral impulsivity symptoms during early childhood might decrease risk for adolescent and adult externalizing problems.
These results are in line with Beauchaine's (2010) theory and consistent with prior work using a latent variable approach (Burns et al., 2014; Lee et al., 2015) suggesting that impulsivity is the core of the externalizing spectrum in childhood. In line with study hypotheses, behavioral impulsivity symptoms appeared to be core, or central, to the externalizing spectrum across developmental periods from preschool to adolescence. Yet, different impulsive symptoms were central at different ages. Often interrupts was key in preschool, difficulty waiting was important during early childhood, often blurts out an answer was core during middle childhood, and often interrupts was again central during adolescence. During middle childhood, impulsivity symptoms were not the core of the externalizing spectrum, but rather defiance appeared to be, and often defies was a core symptom across developmental periods. In addition, easily distracted was a core inattentive symptom during preschool and adolescence, and does not seem to listen was a core inattentive symptom during early and middle childhood. Therefore, defiance may be a relatively central and stable part of the externalizing spectrum across development as well, and the behavioral manifestation of inattention may change across developmental periods. Network analysis provides a critical extension of prior work by allowing for examination of such changes in individual symptom associations within the externalizing spectrum over time (Borsboom & Cramer, 2013).
This finding appears to be in line with progressive differentiation, or fragmentation, of externalizing disorders across development, with inattention splitting off from the externalizing spectrum in older samples, but particularly by late childhood when such inattention may be particularly noticeable (Bauermeister, Barkley, Bauermeister, Martinez, & McBurnett, 2012; Milich, Balentine & Lynam, 2002; Shaw et al., 2007). Thus, from early on, and perhaps increasingly in older populations, there may be notable core symptoms within inattentive, hyperactive-impulsive, and ODD clusters, as well as core symptoms that bridge these clusters, most typically impulsive symptoms.
Network analysis provides a critical extension over latent variable approaches in allowing for complexity to be modeled by a focus on lower-order symptoms (vs. higher-order factors which obscure symptom-level changes). Although results overall suggested that symptoms tended to become relatively more differentiated over time, there was a somewhat discontinuous progression. During preschool, ADHD and ODD formed somewhat distinct clusters; whereas, during early childhood, symptoms were slightly less differentiated, although impulsivity symptoms were the clear center. During later childhood and adolescence, inattention split off, and there was also some distinction between hyperactivity and ODD with impulsive items clearly in the center of the spectrum. Thus, although impulsivity symptoms seemed core across these developmental periods, the structure of the externalizing spectrum itself may change.
Of course, these findings need to be replicated in similar developmental age periods to determine if these networks are a product of the particular samples utilized or of actual developmental periods and changes over time. These illustrative patterns in cross-sectional samples suggest the need for longitudinal work following children over time in order to rule out possible sample artifacts and to test for potential causal relationships between symptoms. Longitudinal work could map how networks among symptoms change within individuals over time and might suggest personalized intervention approaches aimed at more central symptoms, at particular developmental periods (e.g., targeting impulsive symptoms during adolescence). Future work evaluating richer measures of impulsivity (e.g., performance-based measures of impulsivity; control vs. emotion-based impulsivity such as urgency; Whiteside & Lynam, 2001) should be conducted. Finally, we are limited by the current capabilities of network analysis, such as having no current clear guidelines on the strength of indices of centrality. We hope that future methodological work will provide more insight and even greater utility of such analysis. However, these findings represent an important first step in identifying core symptoms to the externalizing spectrum during childhood.
The current study suggests that behavioral impulsivity symptoms are a potent core of the externalizing spectrum during most of early development. Thus, behavioral impulsivity symptoms (and perhaps also defiance) might be useful targets of early interventions. For example, interventions which teach behavioral parenting and cognitive approaches to managing impulse control and defiance might decrease other externalizing symptoms. Such interventions could decrease later risk for other later-developing externalizing problems.
Acknowledgements
We are indebted to the study participants and staff who made this study possible. This research was supported by NIH National Institute of Mental Health Grant R01-MH63146 and MH3759105 to Joel Nigg and 5R03 HD062599-02 and K12 DA 035150 to Michelle Martel.
This research was supported by NIH National Institute of Mental Health Grant R01-MH63146 and MH3759105 to Joel Nigg and 5R03 HD062599-02 and K12 DA 035150 to Michelle Martel. The authors declare no conflicts of interest. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Footnotes
Compliance with Ethical Standards
The authors declare no conflicts of interest.
Contributor Information
Michelle M. Martel, Psychology Department, University of Kentucky
Cheri A. Levinson, Department of Psychiatry, Washington University in St. Louis
Christine A. Lee, Psychology Department, University of Kentucky
Tess E. Smith, Psychology Department, University of Kentucky
References
- Achenbach T. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. University of Vermont Department of Psychiatry; Burlington, VT.: 1991. [Google Scholar]
- Barkley RA, Murphy KR. Attention-Deficit Hyperactivity Disorder: A clinical workbook. 2nd Ed. Guilford Press; New York: 1998. [Google Scholar]
- Bauermeister JJ, Barkley RA, Bauermeister JA, Martínez JV, McBurnett K. Validity of the sluggish cognitive tempo, inattention, and hyperactivity symptom dimensions: Neuropsychological and psychosocial correlates. Journal of Abnormal Child Psychology. 2012;40:683–697. doi: 10.1007/s10802-011-9602-7. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Hinshaw SP, Pang KL. Comorbidity of Attention-Deficit/Hyperactivity Disorder and early-onset conduct disorder: Biological, environmental, and developmental mechanisms. Clinical Psychology: Science and Practice. 2010;17:327–336. [Google Scholar]
- Borsboom D, Cramer AOJ. Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Burns LG, Moura MA, Beauchaine TP, McBurnett K. Bifactor latent structure of ADHD/ODD symptoms: Predictions of dual-pathway/trait-impulsivity etiological models of ADHD. Journal of Child Psychology and Psychiatry. 2014;55:393–401. doi: 10.1111/jcpp.12165. [DOI] [PubMed] [Google Scholar]
- Burt SA, McGue M, Krueger RF, Iacono WG. Sources of covariation among the child-externalizing disorders: Informant effects and the shared environment. Psychological Medicine. 2005;35:1133–1144. doi: 10.1017/S0033291705004770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Jones RM, Hare TA. The adolescent brain. Annals of the New York Academy of Sciences. 2008;1124:111–126. doi: 10.1196/annals.1440.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuPaul GJ, Power TJ, Anastopolous AD, Reid R. ADHD Rating Scale—IV: Checklists, norms, & clinical interpretation. Guilford Press; New York: 1998. [Google Scholar]
- Epskamp S, Cramer AOJ, Waldorp LJ, Schmittman VD, Borsboom D. Qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software. 2012;48:1–18. [Google Scholar]
- Faraone SV. Attention Deficit Hyperactivity Disorder in adults: Implications for theory of diagnosis. Current Directions in Psychological Science. 2000;9:33–36. [Google Scholar]
- Freeman LC. Centrality in social networks conceptual clarification. Social Networks. 1979;1:215–239. [Google Scholar]
- Hart EL, Lahey BB, Loeber R, Applegate B, Frick PJ. Developmental change in Attention-Deficit Hyperactivity Disorder in boys: A four-year longitudinal study. Journal of Abnormal Child Psychology. 1995;23:729–749. doi: 10.1007/BF01447474. [DOI] [PubMed] [Google Scholar]
- Haslam N, Williams B, Prior M, Haslam R, Graetz B, Sawyer M. The latent structure of Attention-Deficit/Hyperactivity Disorder: A taxometric analysis. Australian and New Zealand Journal of Psychiatry. 2006;40:639–647. doi: 10.1080/j.1440-1614.2006.01863.x. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Iacono WG. Externalizing psychopathology in adulthood: A dimensional-spectrum conceptualization and its implications for DSM-V. Journal of Abnormal Psychology. 2005;114:537–550. doi: 10.1037/0021-843X.114.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Chronis AM, Jones HA, Williams SH, Loney J, Waldman ID. Psychometric characteristics of a measure of emotional dispositions developed to test a developmental propensity model of conduct disorder. Journal of Clinical Child & Adolescent Psychology. 2008;37(4):794–807. doi: 10.1080/15374410802359635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: Generating new hypotheses. Journal of Abnormal Psychology. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Lee SS, Willcutt E. Instability of the DSM-IV subtypes of ADHD from preschool through elementary school. Archives of General Psychiatry. 2005;62:896–902. doi: 10.1001/archpsyc.62.8.896. [DOI] [PubMed] [Google Scholar]
- Leblanc N, Boivin M, Dionne G, Brendgen M, Vitaro F, Tremblay RE, Pérusse D. The development of hyperactive–impulsive behaviors during the preschool years: The predictive validity of parental assessments. Journal of Abnormal Child Psychology. 2008;36:977–987. doi: 10.1007/s10802-008-9227-7. [DOI] [PubMed] [Google Scholar]
- Lee SY, Burns GL, Beauchaine TP, Becker SP. Bifactor latent structure of Attention-Deficit/Hyperactivity Disorder (ADHD)/Oppositional Defiant Disorder (ODD) symptoms and first-order latent structure of sluggish cognitive tempo symptoms. Psychological Assessment. 2015 doi: 10.1037/pas0000232. Advanced online publication. [DOI] [PubMed] [Google Scholar]
- Marcus DK, Barry TD. Does Attention-Deficit/Hyperactivity Disorder have a dimensional latent structure? A taxometric anlaysis. Journal of Abnormal Psychology. 2011;120:427–442. doi: 10.1037/a0021405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM. Research Review: A new perspective on Attention-Deficit/Hyperactivity Disorder: Emotion dysregulation and trait models. Journal of Child Psychology and Psychiatry. 2009;50:1042–1051. doi: 10.1111/j.1469-7610.2009.02105.x. [DOI] [PubMed] [Google Scholar]
- Martel MM, Nigg JT, von Eye A. How do trait dimensions map onto ADHD symptom domains? Journal of Abnormal Child Psychology. 2009;37:337–348. doi: 10.1007/s10802-008-9255-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milich R, Balentine AC, Lynam DR. The predominately inattentive subtype—not a subtype of ADHD. The ADHD Report. 2002;10:1–6. [Google Scholar]
- Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: A developmental taxonomy. Psychological Review. 1993;100:674–701. [PubMed] [Google Scholar]
- Nigg JT. On inhibition/disinhibition in developmental psychopathology: Views from cognitive and personality psychology and a working inhibition taxonomy. Psychological Bulletin. 2000;126:220–246. doi: 10.1037/0033-2909.126.2.220. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Casey BJ. An integrative theory of attention-deficit/hyperactivity disorder based on the cognitive and affective neurosciences. Development and Psychopathology. 2005;17(3):785–806. doi: 10.1017/S0954579405050376. [DOI] [PubMed] [Google Scholar]
- Olson SL. Developmental perspectives. In: Sandberg S, editor. Hyperactivity and attention disorders of childhood. Cambridge monographs in child and adolescent psychopathology (2nd Ed.) Cambridge University Press; Cambridge: 2002. [Google Scholar]
- Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: Generalizing degrees and shortest paths. Social Networks. 2010;32:245–251. [Google Scholar]
- Opsahl T, Panzarasa P. Clustering in weighted networks. Social Networks. 2009;31:155–163. [Google Scholar]
- Puig-Antich J, Ryan N. Kiddie Schedule for Affective Disorders and Schizophrenia. Western Psychiatric Institute; Pittsburgh, PA.: 1986. [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Shaw P, Eckstrand K, Sharp W, Blumenthal J, Lerch JP, Greenstein D, Rapoport JL. Attention-Deficit/Hyperactivity Disorder is characterized by a delay in cortical maturation. Proceedings of the National Academy of Sciences. 2007;104:19649–19654. doi: 10.1073/pnas.0707741104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tackett JL. Toward an externalizing spectrum in DSM–V: Incorporating developmental concerns. Child Development Perspectives. 2010;4:161–167. [Google Scholar]
- Wehmeier PM, Schacht A, Barkley RA. Social and emotional impairment in children and adolescents with ADHD and the impact on quality of life. Journal of Adolescent Health. 2010;46:209–217. doi: 10.1016/j.jadohealth.2009.09.009. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. [Google Scholar]
- Young SE, Friedman NP, Miyake A, Willcutt EG, Corley RP, Haberstick BC, Hewitt JK. Behavioral disinhibition: Liability for externalizing spectrum disorders and its genetic and environmental relation to response inhibition across adolescence. Journal of Abnormal Psychology. 2009;118:117–130. doi: 10.1037/a0014657. [DOI] [PMC free article] [PubMed] [Google Scholar]