Abstract
As two major non-operative methods, physiotherapy and acupuncture have been proved to be safe and effective in osteoarthritis (OA) treatment. However, only a little study focused on functions of both methods on cartilage repairing. The main goal of this research is to prove and compare effectiveness of acupuncture and physiotherapy on OA, and to explore their possible efficacy on cartilage repairing. One hundred knees of 50 participants with knee osteoarthritis (KOA) were randomly divided into acupuncture group and physiotherapy group. Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was used to evaluate the motor function of knee joints, followed by MRI scanning to measure T2 values in ten cartilage sub-regions in tibiofemoral joints. Significant lower scores of total WOMAC and three subscales on the 4th weekend were observed in both groups than those of the baseline (P < 0.01). For acupuncture group, scores of total WOMAC and three subscales for pain, stiffness and physical function on 4th weekend were significantly lower than those of the physiotherapy group (P < 0.01 and P < 0.05). T2 values in anterior medial tibial sub-region (MTa) and anterior lateral tibial sub-region (LTa) were significantly lower in acupuncture group on 4th weekend than those of the baseline (P < 0.05). No significant difference in T2 values was detected in physiotherapy group. These results indicate that acupuncture represents certain clinical effect on KOA which is superior compared with physiotherapy, and hint the possible roles of acupuncture in promoting cartilage repairing.
Keywords: Osteoarthritis, cartilage, acupuncture therapy, physiotherapy, magnetic resonance imaging
Introduction
As a kind of degenerate joint disease, osteoarthritis (OA) is characterized by cartilage degradation, which may occur in every joint, especially in those bearing loadings. Knee joint was considered to be the most commonly complained place in clinic. Two therapeutic methods now can be available to treat OA: operation and non-operative therapy. However, operation was reported to be appropriate for patients at late stage, and non-operative therapy is mainly for those at early or middle stage. As two major non-operative methods, physiotherapy and acupuncture have been proved to be safe and effective in OA treatment. Studies have reported that physiotherapy may have efficacy on diminishing inflammation and suppressing pain [1], and acupuncture can remarkably improve symptoms and motor function of knee joints for patients with knee osteoarthritis (KOA) [2,3]. However, only a little study focused on functions of both methods on cartilage repairing.
Previous studies reported that magnetic resonance imaging (MRI) may be more superior on displaying soft tissues than other imaging methods, and can detect cartilage degradation even at early stage of OA [4,5]. As the quantitative MRI method, T2 images have been considered to indirectly assess collagen content and orientation [6]. In the earliest stage of OA, collagen matrix of cartilage breaks down and cannot immobilize water protons, resulting in an elevation in T2 relaxation time [7]. Numerous reports have witnessed the wide use of T2 imaging in measuring water content of cartilage [8]. Study also revealed that T2 values may be the sensitive marker for early diagnosis and disease monitoring of OA [9].
In the present study, paticipants were treated by acupuncture and physiotherapy respectively and evaluated by Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scoring [10] followed by MRI examination of cartilage. WOMAC scores were compared to assess the clinical effect for each group, aiming to prove and compare effectiveness of acupuncture and physiotherapy on KOA. T2 values were detected to explore the possible efficacy of these two deferent therapy methods on cartilage repairing.
Material and methods
Trial design and subjects
This study was a prospective, randomized controlled clinical trial. Written informed consent to attend this study was obtained from all participants prior to inclusion in the study, as approved by the Ethics Committee of Peking Union Medical College Hospital. Full compliance with the Helsinki Declaration was applied during the study. Participants aged 30-80 were recruited by the Department of Orthopedic Surgery of Peking Union Medical College Hospital between Jan. 2010 and Jul. 2013, and clinically diagnosed as having KOA by experienced orthopedist according to the OA criteria proposed by American College of Rheumatology in 1995 [11]. The main exclusion criteria were: (1) acute knee injury; (2) had ever accepted therapy as hormone or injection in articulation cavity; (3) had ever accepted treatment as oral medicine, physiotherapy, acupuncture or massage during the passed three months; (4) anyone with cardiac pacemaker or any metal object in body; (5) other severe diseases such as heart, lung, liver, kidney or cerebrum failure, tumors, gastrointestinal hemorrhage and so on; (6) pregnant or lactating woman; (7) anyone unable to tolerate or cooperate with treatment. A total of 100 knees (n = 100) of 50 participants (12 males, 38 females) were included in the study. All the participants were randomly divided into acupuncture group (5 males, 20 females, n = 50) and physiotherapy group (7 males, 18 females, n = 50) based on the central stochastic system built in the SAS9.
Interventions
Electro-acupuncture treatment was given to the participants in acupuncture group by acupuncturists with practice experience of over twenty years, and was reported according to Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) [12] and New Standard International Acupuncture Nomenclature [13] as follows. The participants received treatment with a frequency of once every other day for four weeks. The needles were retained in acupoints for 20 min each time. Seven acupoints of each side were selected for needling: EX-LE4 Neixiyan, EX-LE5 Waixiyan, EX-LE2 Heding, SP10 Xuehai, SP11 Jimen, ST34 Liangqiu and ST36 Zusanli (see Figure 1). All acupoints were located according to the WHO standard acupuncture point locations in the Western Pacific Region. Disposable stainless steel acupuncture needles (φ 0.30 × 40 mm, Hanyi®, Tianjin Huahong medical Co. Ltd., Tianjin, China) were inserted to a depth of approximately 0.8-3.5 cm. Each acupuncture needle was manipulated until Deqi sensation occurred. Then the needles in EX-LE4 and EX-LE5 were connected with electric acupuncture apparatus (KWD-808II Multi-Purpose Health Device, Yingdi®, Changzhou, China), and continuous wave was selected with the stimulation of 20 HZ frequency and tolerated current strength by participants.
Figure 1.
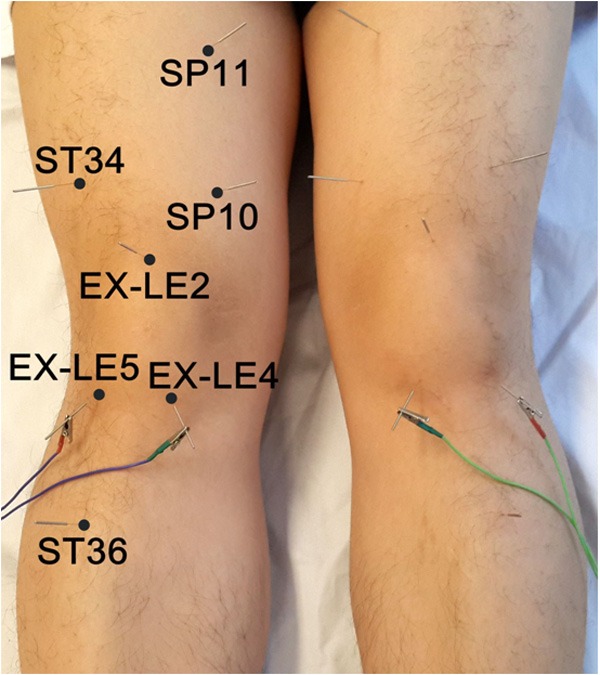
Acupoints of acupuncture treatment.
Participants in the physiotherapy group received physiotherapy treatment five times a week for four weeks. The treatment was given for 30 min each time. K824 Computer Intermediate Frequency Therapy Apparatus (Xiangyun®, Beijing, China) was used to give the No.9 prescription which alternately output sine, triangular and exponential wave with 3000 HZ intermediate frequency and 0.5-120 HZ low frequency. The maximum stimulation was given to participants based on their tolerance. Silica gel electrodes were put on the pain points around knee.
Outcome measures
WOMAC scoring: WOMAC was used to assess knee joint’s motor function. The scores of total WOMAC and three subscales for pain, stiffness and physical function were respectively acquired pre and posttreatment.
MRI acquisition: All participants underwent MRI scans on a clinical 1.5 T scanner (Signa EXCITE Twin Speed HD, GE Medical Systems, Milwaukee, WI, USA). Sagittal T2 Mapping images for the medial and lateral tibiofemoral joints were acquired pre and post-treatment according to the following parameters: Two-dimensional fast recovery fast spin echo (2D-FRFSE) sequence, repetition time/echo time (TR/TE) = 1340/(17.5-105) ms, echo train length (ETL) = 6, thickness = 4 mm, field of view (FOV) = 14 cm × 11 cm or 15 cm × 12 cm, matrix = 320 × 256; 3 times excitations; section = 7, acquisition time = 6.95 min, which lasted about 13.9 min to acquire the images in an individual subject.
One optimal image was chosen in the medial and lateral tibiofemoral joint respectively at each knee, and the AW 4.2/Functool software (GE Medical Systems, Milwaukee, WI, USA) was used to generate the T2 pseudocolor map with 95% confidence interval after deleting volumes acquired during the first spin echo [14]. Ten sub-regions of interest including central medial femoral region (MFc), posterior medial femoral region (MFp), central lateral femoral region (LFc), posterior lateral femoral region (LFp), anterior medial tibial region (MTa), central medial tibial region (MTc), posterior medial tibial region (MTp), anterior lateral tibial region (LTa), central lateral tibial region (LTc) and posterior lateral tibial region (LTp) were then selected according to the Whole-Organ Magnetic Resonance Imaging Score (WORMS) [15] (see Figure 2 [16]). T2 values were measured three times in each region and the mean values were then acquired. Images with much translation or rotation or with T2 values of > 200 ms would be excluded in the processing.
Figure 2.
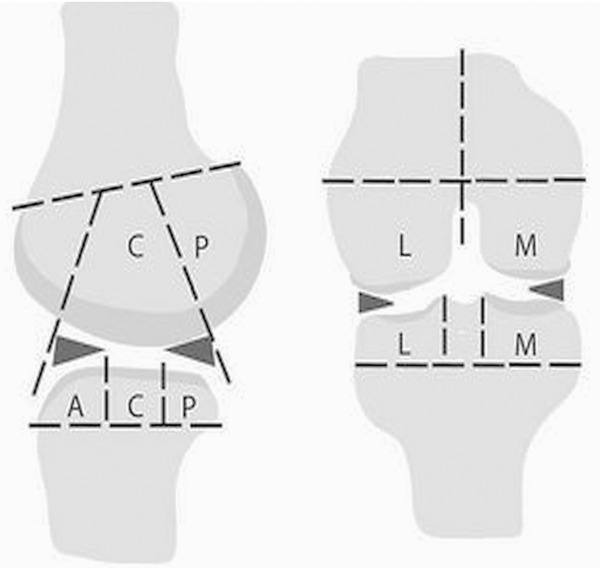
Regions selected in the tibiofemoral joint.
Data analysis
All the continuous variables were presented as mean ± SD. T-test including Paired-samples T-test and Independent-samples T-test was respectively and appropriately used to analyze the difference within each group and between two groups. The nonparametric Mann-Whitney test would be performed in case of abnormal distribution. All tests were performed assuming a significance level of α = 5%. Analysis was performed by using SPSS 13.0 (SPSS Inc., Chicago IL).
Results
Baseline characteristics
One hundred and twenty-six participants were approached and screened for their eligibility to enroll in this study. Fifty participants consented and were eligible for the study and were given their informed consent for participation. One hundred knees of 50 participants (n = 100) were randomly divided into acupuncture group and physiotherapy group, and 50 knee joints were included in each group (n = 50). Three participants dropped-out for their personal reason (one from acupuncture group and two from physiotherapy group). Forty-seven participants with 94 knees completed the trials (n = 94), 24 participants in acupuncture group (n = 48) and 23 in physiotherapy group (n = 46) (see Figure 3). The characteristics of the two groups are not significantly different at baseline and are given in Table 1.
Figure 3.
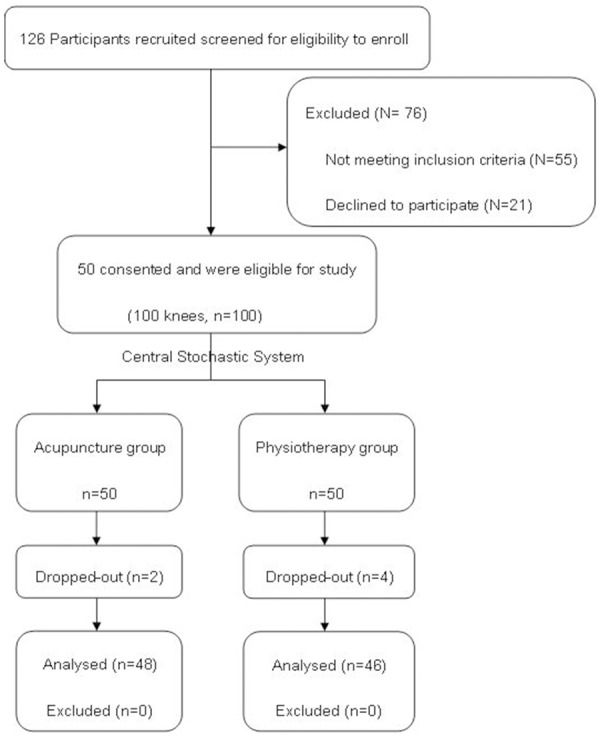
Participants flow diagram.
Table 1.
Baseline characteristics of two groups
| Variables n = 94 | Acupuncture n = 48 | Physiotherapy n = 46 | p Value |
|---|---|---|---|
| Age (years) | 54.38±8.05 | 55.26±9.07 | 0.617 |
| Gender | 0.553 | ||
| Male | 10 (20.8%) | 12 (26.1%) | - |
| Female | 38 (79.2%) | 34 (73.9%) | - |
| Course (years) | 6.90±5.65 | 6.00±4.29 | 0.391 |
| Total WOMAC | 34.44±22.38 | 35.70±20.58 | 0.778 |
| Pain | 6.96±4.25 | 7.41±4.33 | 0.608 |
| Stiffness | 2.38±1.70 | 2.43±1.53 | 0.858 |
| Physical function | 23.73±15.86 | 24.46±14.22 | 0.816 |
Outcomes
Table 2 showed the scores of total WOMAC and three subscales on the day 0 (baseline) and 4th weekend. Significant lower values of the measurement were observed after 4 weeks treatment in both groups when compared with the baseline values (P < 0.01). For acupuncture group, scores of total WOMAC and each subscale on 4th weekend were significantly lower than those of the physiotherapy group (P < 0.01 and P < 0.05).
Table 2.
Scores of total WOMAC and three subscales
| Index | Acupuncture group n = 48 | Physiotherapy group n = 46 | ||
|---|---|---|---|---|
|
| ||||
| Baseline | 4th Weekend | Baseline | 4th Weekend | |
| Total WOMAC | 34.44±22.38 | 13.63±12.06*,† | 35.70±20.58 | 24.11±16.60* |
| Pain | 6.96±4.25 | 2.71±2.32*,Δ | 7.41±4.33 | 4.00±3.09* |
| Stiffness | 2.38±1.70 | 0.83±0.95*,†† | 2.43±1.53 | 1.78±1.15* |
| Physical function | 23.73±15.86 | 9.58±8.43*,‡ | 24.46±14.22 | 17.37±11.99* |
P = 0.000, compared with the baseline.
P = 0.001, compared with physiotherapy group;
P = 0.000, compared with physiotherapy group;
P = 0.000, compared with physiotherapy group;
P = 0. 024, compared with physiotherapy group.
Figure 4A and 4B showed the T2 grey-scale image and T2 pseudocolor image of the tibiofemoral joint from one patient. Table 3 listed T2 values in the ten sub-regions of the cartilage of tibiofemoral joints. For the acupuncture group, T2 values in MTa and LTa on 4th weekend were significantly lower than the baseline values (P < 0.05). However, no significant difference was observed in other eight sub-regions (P > 0.05). For the physiotherapy group, none sub-region showed significant difference of T2 value on 4th weekend when compared with the baseline (P > 0.05).
Figure 4.
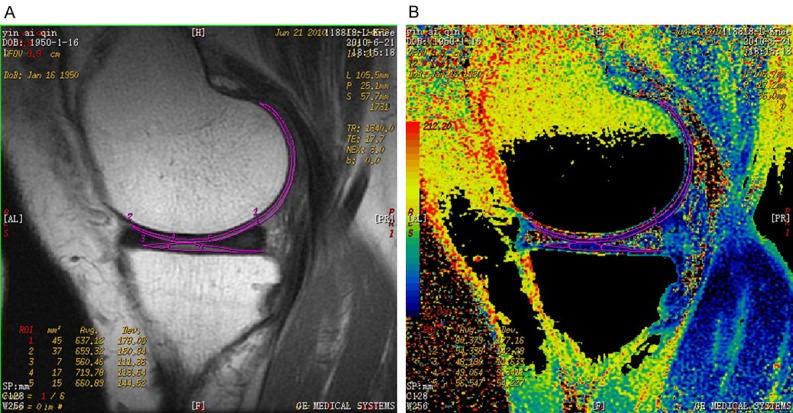
Sub-regions of the cartilage of tibiofemoral joint and T2 values measurements. A. T2 grey-scale image. B. T2 pseudocolor image.
Table 3.
Changes of T2 values (ms)
| Regions | Acupuncture group n = 48 | Physiotherapy group n = 46 | ||
|---|---|---|---|---|
|
| ||||
| Baseline | 4th Weekend | Baseline | 4th Weekend | |
| MFc | 55.77±16.19 | 56.63±13.58 | 53.41±7.01 | 54.39±7.56 |
| MFp | 64.17±13.71 | 62.29±11.29 | 64.83±12.18 | 63.61±10.45 |
| MTa | 52.04±11.44 | 49.90±8.86* | 54.54±6.70 | 55.48±8.90 |
| MTc | 52.42±14.30 | 52.38±12.04 | 51.46±6.86 | 52.87±9.79 |
| MTp | 47.98±5.48 | 47.75±5.32 | 52.85±11.47 | 53.17±8.57 |
| LFc | 51.75±5.21 | 52.44±6.52 | 53.83±7.84 | 55.28±9.61 |
| LFp | 68.25±13.53 | 66.88±13.58 | 67.30±11.92 | 68.17±13.56 |
| LTa | 55.83±11.31 | 53.96±9.07▲ | 54.37±10.89 | 55.70±9.99 |
| LTc | 51.98±15.81 | 51.40±13.48 | 58.28±10.99 | 59.07±13.06 |
| LTp | 47.83±4.32 | 47.65±4.27 | 54.89±7.40 | 55.50±9.88 |
P = 0.040, compared with the baseline;
P = 0.030, compared with the baseline.
Safety and tolerability
Physiotherapy is a conventional therapy method for OA. It’s safe and painless during treatment process, so it’s easy to be accepted by participants. Acupuncture is widely used in China with history of thousands years. It does harmless to body. Although needling sensation or sometimes tiny bleeding occurs, it’s popularly recognized and tolerated by Chinese people, and is being accepted by more people all over the world. Both acupuncture and physiotherapy were well tolerated in this study, and all the participants completed the trial except three for their personal reasons.
Discussion
Clinical effect of acupuncture on OA
OA is a common disease in the middle-aged and elderly population. Each joint such as joint of hand, hip-joint, spine and especially knee-joint could be involved. Clinically KOA is characterized by pain, arthrocele, limited movement. It is considered that operations such as arthroscopic debridement and total knee arthroplasty could be applied to patients with severe and end-stage KOA only. For most early-stage and mid-stage patients, safe and effective early intervention is considered to prevent and postpone OA development. Compared with the hormone, non-steroid anti-inflammatory and antalgic drugs, physiotherapy is believed to be a safer conventional non-operative treatment whose antalgic and repercussive roles have been proved in clinic practice.
According to the theory of Traditional Chinese Medicine (TCM), OA is classified into category of arthralgia. Deficiency of liver and kidney, energy and nutrition results in wind, cold and damp staying in the week joints. Furthermore, meridians are obstructed which may lead to unsmooth flowing of energy and nutrition. As a result, joints lose being nourished and pain occurs. As a kind of external therapy in TCM for arthralgia treatment, acupuncture is widely used in China due to its nice clinical effect in analgesia, detumescence as well as its roles in improving physical function with advantages of safety and non-toxic effect. Previous studies have proved anti-inflammatory action of acupuncture [17,18] and hinted its possible roles in protecting and repairing cartilage [19-21].
According to the characters of deficiency and stasis of energy and nutrition, the therapeutic principle for OA should be promoting energy to activate circulation, so as to acquire efficacy of dredging meridians and easing pain. Three principles should be complied for the acupoints selection-local selection, selecting distant points along meridians, and point selection by identification. Since KOA presents as a local lesion, and the previous animal experiment hinted that acupuncture achieved curative effect on KOA mainly through local action [20], the local acupoints around knee like EX-LE4, EX-LE5 and EX-LE2 were then selected as the main points in order to regulate local energy and circulation of joint. In addition, decreased tension of soft tissues was considered to be associated with KOA, points near knee joint like SP10, SP11 and ST34 were thus supplementally selected to adjust tension of soft tissues. Furthermore, based on principle of selecting distant points along meridians, an important point of stomach meridian of foot-Yangming whose characteristic is full of energy and nutrition, ST36 was selected to invigorate Channel qi. All the seven acupoints contribute to dredge meridians and ease pain. In addition, electric pulse stimulation was used on EX-LE4 and EX-LE5, mainly for enhancing and maintaining stimulation.
This study revealed that both acupuncture and physiotherapy improved the clinical symptoms of pain, morning stiffness and joint dysfunction. However, acupuncture treatment showed better curative effect than physiotherapy, suggesting that acupuncture may be a superior non-operative treatment for KOA compared with physiotherapy.
Impact of acupuncture on T2 value
OA is characterized by articular cartilage degradation and is considered as a degenerative disease. With the influence of age, wearing, biochemical and genetic factors, natural extracellular environment no longer exist because of damaged collagen scaffold and degraded proteoglycans in the chondrocyte matrix, leading to decreased cell counts and abnormal distribution. Attenuated cartilaginous layers, bony cleft and even bone defect will then appear along with biomechanics changes. Previous image examination such as X ray and computed tomography (CT) scans can only report the morphological changes for the moderate and end-stage OA. Early matrix degradation could not be detected because of non-obvious cartilage changes. It was reported that MRI could distinguish different histological layers and reflect early degradation of articular cartilage, which made it possible for the diagnosis of early-stage OA [22]. As the quantitative MRI method, increased T2 values, to some extent, could represent damages of the cartilage collagen scaffold [23]. T2 image could thus be used for the discrimination of the OA severities, which has been considered to be a sensitive method for detecting articular cartilage changes and curative effect evaluation in OA patients [24,25].
Abnormal high stress was considered as an important factor contributing to the degeneration of articular cartilage, so cartilage damage often occurred in weight-bearing area. Previous study has also revealed that differences in T2 values could be found in the weight-bearing areas, and T2 values increase with the severity of OA disease [26]. As two of the main weight-bearing areas in knee joint, MTa and LTa were the very places that the pinpoints could reach to when EX-LE4, EX-LE5 were selected as the acupoints. This study revealed significant differences in T2 values before and after acupuncture in MTa and LTa, while no significant difference in T2 value was detected in the physiotherapy group. Previous studies have proved anti-inflammatory action of acupuncture by influencing expression of interleukin-1β, tumor necrosis factor-α, matrix metalloproteinase and tissue inhibitor [17-19]. Additionally, acupuncture may play roles in improving cartilage repairing by influencing expression of transforming growth factor-β1 and basic fibroblast growth factor [20,21]. Further, acupuncture allows needles getting into articular cavity, and then pinpoints reached to the cartilage surface, while physiotherapy acts only at the superficial location of knee joint. This might contribute to the significant differences in T2 values in MTa and LTa. However, farther studies are inspired to explore the mechanism of both acupuncture and physiotherapy on KOA. Especially, studies with amended prescription focusing on other weight-bearing areas, larger sample size and longer-term observation are required to identify roles of acupuncture on cartilage repairing.
Conclusion
In summary, this study indicates that acupuncture is a feasible alternative therapy for KOA patients. Acupuncture shows an impact on T2 value in cartilage, which may suggest a superior clinical effect when compared with physiotherapy.
Acknowledgements
This study was supported by Traditional Chinese Medicine Science & Technology Research Program (NO. 06-07LP01) and National “Twelfth Five-Year” Plan for Science & Technology Support Program (NO. 2012BAI10B02), which was respectively funded by State Administration of Traditional Chinese Medicine and National Natural Science Foundation of China. We are grateful to Dr. Daohai Wang for his contribution to acupuncture treatment. Na Hu and Min Sheng assisted to MRI scans. Tao Xu performed statistical analysis.
Disclosure of conflict of interest
None.
References
- 1.Page CJ, Hinman RS, Bennell KL. Physiotherapy management of knee osteoarthritis. Int J Rheum Dis. 2011;14:145–151. doi: 10.1111/j.1756-185X.2011.01612.x. [DOI] [PubMed] [Google Scholar]
- 2.Plaster R, Vieira WB, Alencar FA, Nakano EY, Liebano RE. Immediate effects of electroacupuncture and manual acupuncture on pain, mobility and muscle strength in patients with knee osteoarthritis: a randomised controlled trial. Acupunct Med. 2014;32:236–241. doi: 10.1136/acupmed-2013-010489. [DOI] [PubMed] [Google Scholar]
- 3.Manyanga T, Froese M, Zarychanski R, Abou-Setta A, Friesen C, Tennenhouse M, Shay BL. Pain management with acupuncture in osteoarthritis: a systematic review and meta-analysis. BMC Complement Altern Med. 2014;14:312. doi: 10.1186/1472-6882-14-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dam EB, Loog M, Christiansen C, Byrjalsen I, Folkesson J, Nielsen M, Qazi AA, Pettersen PC, Garnero P, Karsdal MA. Identification of progressors in osteoarthritis by combining biochemical and MRI-based markers. Arthritis Res Ther. 2009;11:R115. doi: 10.1186/ar2774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsushima H, Okazaki K, Takayama Y, Hatakenaka M, Honda H, Izawa T, Nakashima Y, Yamada H, Iwamoto Y. Evaluation of cartilage degradation in arthritis using T1rho magnetic resonance imaging mapping. Rheumatol Int. 2012;32:2867–2875. doi: 10.1007/s00296-011-2140-3. [DOI] [PubMed] [Google Scholar]
- 6.Ross KA, Williams RM, Schnabel LV, Mohammed HO, Potter HG, Bradica G, Castiglione E, Pownder SL, Satchell PW, Saska RA, Fortier LA. Comparison of Three Methods to Quantify Repair Cartilage Collagen Orientation. Cartilage. 2013;4:111–120. doi: 10.1177/1947603512461440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baum T, Joseph GB, Karampinos DC, Jungmann PM, Link TM, Bauer JS. Cartilage and meniscal T2 relaxation time as non-invasive biomarker for knee osteoarthritis and cartilage repair procedures. Osteoarthr Cartilage. 2013;21:1474–1484. doi: 10.1016/j.joca.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Apprich S, Mamisch TC, Welsch GH, Stelzeneder D, Albers C, Totzke U, Trattnig S. Quantitative T2 mapping of the patella at 3.0T is sensitive to early cartilage degeneration, but also to loading of the knee. Eur J Radiol. 2012;81:e438–443. doi: 10.1016/j.ejrad.2011.03.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blumenkrantz G, Majumdar S. Quantitative magnetic resonance imaging of articular cartilage in osteoarthritis. Eur Cell Mater. 2007;13:76–86. doi: 10.22203/ecm.v013a08. [DOI] [PubMed] [Google Scholar]
- 10.Faik A, Benbouazza K, Amine B, Maaroufi H, Bahiri R, Lazrak N, Aboukal R, Hajjaj-Hassouni N. Translation and validation of Moroccan Western Ontario and McMaster Universities (WOMAC) osteoarthritis index in knee osteoarthritis. Rheumatol Int. 2008;28:677–683. doi: 10.1007/s00296-007-0498-z. [DOI] [PubMed] [Google Scholar]
- 11.Hochberg MC, Altman RD, Brandt KD, Clark BM, Dieppe PA, Griffin MR, Moskowitz RW, Schnitzer TJ. Guidelines for the medical management of osteoarthritis. Part II. Osteoarthritis of the knee. American College of Rheumatology. Arthritis Rheum. 1995;38:1541–1546. doi: 10.1002/art.1780381104. [DOI] [PubMed] [Google Scholar]
- 12.MacPherson H, Altman DG, Hammerschlag R, Li Y, Wu T, White A, Moher D STRICTA Revision Group. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. Acupunct Med. 2010;28:83–93. doi: 10.1136/aim.2009.001370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jenkins M. A new standard international acupuncture nomenclature. Acupunct Med. 1990;7:21–23. [Google Scholar]
- 14.Maier CF, Tan SG, Hariharan H, Potter HG. T2 quantitation of articular cartilage at 1.5 T. J Magn Reson Imaging. 2003;17:358–364. doi: 10.1002/jmri.10263. [DOI] [PubMed] [Google Scholar]
- 15.Peterfy CG, Guermazi A, Zaim S, Tirman PF, Miaux Y, White D, Kothari M, Lu Y, Fye K, Zhao S, Genant HK. Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthr Cartilage. 2004;12:177–190. doi: 10.1016/j.joca.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Lajeunesse D, Reboul P. Subchondral bone in osteoarthritis: a biologic link with articular cartilage leading to abnormal remodeling. Curr Opin Rheumatol. 2003;15:628–633. doi: 10.1097/00002281-200309000-00018. [DOI] [PubMed] [Google Scholar]
- 17.Wang DH, Bao F, Wu ZH, Sun H, Zhang YX. Influence of acupuncture on IL-1β and TNF-α expression in the cartilage of rats with knee osteoarthritis. Chin J Orthop Trauma. 2011;24:775–778. [PubMed] [Google Scholar]
- 18.Qin Y, He J, Xia L, Guo H, He C. Effects of electro-acupuncture on oestrogen levels, body weight, articular cartilage histology and MMP-13 expression in ovariectomised rabbits. Acupunct Med. 2013;31:214–221. doi: 10.1136/acupmed-2012-010289. [DOI] [PubMed] [Google Scholar]
- 19.Bao F, Sun H, Wu ZH, Wang DH, Zhang YX. Effect of acupuncture on expression of matrix metalloproteinase and tissue inhibitor in cartilage of rats with knee osteoarthritis. Zhongguo Zhen Jiu. 2011;31:241–246. [PubMed] [Google Scholar]
- 20.Bao F, Wang DH, Wang FQ, Sun H, Li B, Zhang YX, Wu ZH. Effect of electro-acupuncture on expression of transforming growth factor-β1 in the cartilage of experimental rats with knee osteoarthritis. Chin J Rehabil Theory Pract. 2008;14:345–346. [Google Scholar]
- 21.Wang DH, Sun H, Bao F, Wu ZH, Wang FQ, Zhang YX. Influence of electro-acupuncture on b-FGF expression in the cartilage of knee osteoarthritic rats. J Med Res. 2010;39:106–109. [Google Scholar]
- 22.Hannila I, Raina SS, Tervonen O, Ojala R, Nieminen MT. Topographical variation of T2 relaxation time in the young adult knee cartilage at 1.5 T. Osteoarthr Cartilage. 2009;17:1570–1575. doi: 10.1016/j.joca.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 23.Blumenkrantz G, Stahl R, Carballido-Gamio J, Zhao S, Lu Y, Munoz T, Hellio Le Graverand-Gastineau MP, Jain SK, Link TM, Majumdar S. The feasibility of characterizing the spatial distribution of cartilage T(2) using texture analysis. Osteoarthr Cartilage. 2008;16:584–590. doi: 10.1016/j.joca.2007.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kornaat PR, Ceulemans RY, Kroon HM, Riyazi N, Kloppenburg M, Carter WO, Woodworth TG, Bloem JL. MRI assessment of knee osteoarthritis: Knee Osteoarthritis Scoring System (KOSS)--inter-observer and intra-observer reproducibility of a compartment-based scoring system. Skeletal Radiol. 2005;34:95–102. doi: 10.1007/s00256-004-0828-0. [DOI] [PubMed] [Google Scholar]
- 25.Nishioka H, Hirose J, Nakamura E, Okamoto N, Karasugi T, Taniwaki T, Okada T, Yamashita Y, Mizuta H. Detecting ICRS grade 1 cartilage lesions in anterior cruciate ligament injury using T1rho and T2 mapping. Eur J Radiol. 2013;82:1499–1505. doi: 10.1016/j.ejrad.2013.04.038. [DOI] [PubMed] [Google Scholar]
- 26.David-Vaudey E, Ghosh S, Ries M, Majumdar S. T2 relaxation time measurements in osteoarthritis. Magn Reson Imaging. 2004;22:673–682. doi: 10.1016/j.mri.2004.01.071. [DOI] [PubMed] [Google Scholar]


