Abstract
The aim of this study was to evaluate current practice patterns on diagnosis and management of pediatric varicoceles. Questionnaires of approaches to diagnosis and management of pediatric varicoceles were sent electronically to pediatric urologists. Of the 70 questionnaires e-mailed, 37 (53%) responded to the survey. 10 respondents (27%) chose to operate on varicoceles, whereas 9 (24%) chose to observe, and 18 (49%) chose to decide upon treatment depending on the clinical situation. The most important indication for varicocelectomy was a decrease in ipsilateral testicular size (n=29, 78%) followed by testicular or scrotal pain (n=4, 11%) and varicocele grade (n=4, 11%). The optimal age for varicocelectomy was answered as 13.8±2.3 years mean. 32 respondents (86%) have used ultrasonography to aid in the diagnosis of varicoceles, and 26 respondents (70%) have considered repairing varicocele incidentally detected on ultrasonography. In an otherwise asymptomatic patient with varicocele, 17 respondents (46%) considered surgery for grade 3, but 15 respondents (41%) would not repair the varicocele. The most commonly used surgical approach was subinguinal microsurgical (n=19, 51%), followed by inguinal (n=9, 24%) and laparascopic (n=5, 14%) procedures. The most commonly experienced post-operative complication was recurrence (n=22, 59%) followed by persistence (n=13, 35%) and hydrocele (n=10, 27%). 28 respondents (76%) did not have long-term follow-up data including regarding fertility on their varicocele patients. Our survey demonstrates that there is lack of consensus on diagnosis and management of pediatric and adolescent varicoceles among pediatric urologists. A prospective randomized study of pediatric and adolescent varicoceles is needed to assess the outcomes and develop universal management guidelines.
Keywords: Varicocele, Adolescent, Surveys and Questionnaires, Infertility
INTRODUCTION
Varicoceles are abnormal dilations of the pampiniform plexus in the scrotum. Varicoceles occur in about 15% of the general male population and are diagnosed in 20% to 40% of men visiting infertility clinics.1 Varicoceles are also diagnosed in 15%-20% of adolescent boys.2 Varicoceles can affect testicular growth, semen parameters, and development of androgen deficiency. They are considered to be a major cause of male infertility.3,4 However, due to the unclear etiological effect of varicoceles on spermatogenesis and infertility in pediatric and adolescent males,5 the benefits of varicocele treatment and indications for treatment (surgery versus observation) are controversial.6,7,8
There have been two prior practice surveys regarding the approaches to the diagnosis and management of pediatric and adolescent varicocele in the United States in 20019 and 2014.10 However, to the best of our knowledge, such practice surveys have yet to be undertaken in other countries. Therefore, we surveyed pediatric urologists to determine the current practices for diagnosis and management of pediatric and adolescent varicoceles in Korea.
MATERIALS AND METHODS
A 21-point online questionnaire concerning the management of pediatric and adolescent varicoceles was distributed to 70 pediatric urologists in Korea. The Naver office service (http://office.naver.com) was used to format the survey, as well as to acquire and analyze the data. Additional data analysis was performed using Microsoft Excel and IBM SPSS statistics 21. The questionnaire was intended to evaluate diagnostic approachs, indications for varicocelectomy, surgical approaches, postoperative complications, and follow-up information. To better understand the current approach used by urologists with regard to pediatric and adolescent varicocele, two clinical scenarios were also investigated.
This study was approved by the institutional review board of our hospital (IRB No. 2016-01-036).
RESULTS
1. Respondent demographics
Out of the 70 distributed surveys, 37 responses (53%) were received. 29 respondents (78%) work in university hospitals, 3 respondents (8%) in general hospitals, and 5 respondents (14%) in private clinics. 23 respondents (61%) have been in practice for 6-15 years, 9 respondents (25%) for more than 16 years, and 5 respondents (14%) for 0-5 years. 34 respondents (97%) see at least 6-10 patients with varicocele annually, with 9 respondents (24%) having more than 30 cases annually.
2. Varicocele diagnosis (Table 1)
TABLE 1. Varicocele diagnosis.
32 respondents (86%) used an ultrasonography (US) and/or Doppler US for the diagnosis of varicocele with most of those respondents (n=25, 68%) using US in 76%-100% of all cases. 29 respondents (78%) used objective US criteria, including testicular volume discrepancy, as well as venous dilation and/or backflow, but 8 respondents (22%) answered that US findings did not influence their decision making process.
3. Treatment of pediatric and adolescent varicocele (Table 2)
TABLE 2. Varicocele treatment.
SD: standard deviation, US: ultrasonography.
36 respondents (97%) responded that they treat varicoceles by themselves, with only 1 respondent (3%) referring patients to fertility specialists. Overall, 10 respondents (27%) indicated that they decide to operate at the time of diagnosis, 9 respondents (24%) choose to observe, and 18 respondents (49%) choose to treat according to the given circumstances. The most important surgical indications answered, were (1) decrease in ipsilateral testicular size (n=29, 78%), (2) testicular or scrotal pain (n=4, 11%), and (3) varicocele grade (n=4, 11%). The adequate age for varicocelectomy answered was 13.8±2.3 years. Most respondents (n=26, 70%) answered to consider surgery for incidentally identified varicoceles on US. For a symptom-free adolescent with symmetric, adequate testis for their age, 17 respondents (46%) answered they would consider operation when the grade of varicocele is 3, whereas 15 respondents (41%) would not operate on any grade of varicocele.
Regarding the surgical approach, 19 respondents (51%) chose the subinguinal microsurgical approach, followed by the inguinal (n=9, 24%), the laparoscopic artery sparing (n=5, 14%) and the open retroperitoneal approach (n=4, 11%). Of those respondents who repair varicoceles with open approaches, 15 respondents (41%) used a microscope and 13 respondents (35%) used a loupe magnification, whereas only 9 respondents (24%) used neither of them.
4. Postoperative follow-up and complications (Table 3)
TABLE 3. Varicocelectomy complications.
28 respondents (76%) indicated that long-term follow-up (more than 6 months) data of their pediatric and adolescent varicocele patients was not available, whereas 9 respondents (24%) indicated that the data were available. 34 respondents (91%) indicated that they were not aware of the fertility status of their patients and 3 respondents (9%) who were aware of the fertility status, indicated that less than 10% of patients developed infertility.
Postoperative complications experienced after varicocelectomy were recurrence (n=22, 59%), persistence (n=13, 35%), hydrocele (n=10, 27%), chronic pain (n=8, 22%), hematoma (n=5, 14%), and paresthesia (n=3, 8%). Complications occurring for more than 5% of incidences were recurrence (n=15, 41%), persistence (n=12, 32%), hydrocele (n=6, 16%), and chronic pain (n=6, 16%).
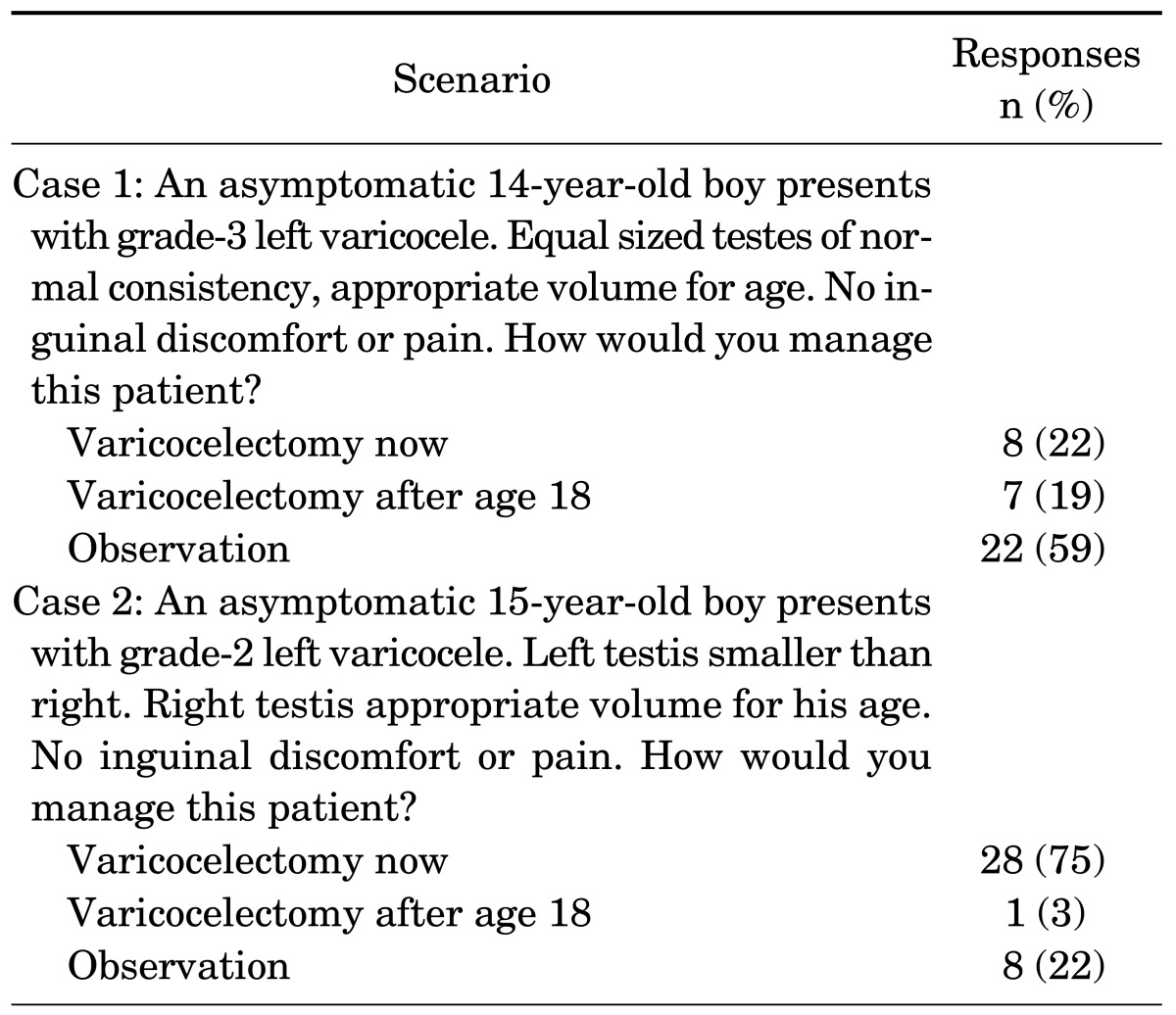
5. Clinical case scenarios (Table 4)
TABLE 4. Clinical case scenarios.
In an effort to better understand the practice patterns of physicians that diagnose and treat pediatric and adolescent varicoceles, we presented two clinical case scenarios that require integration of clinical principles. In the first scenario reflecting an adolescent with grade 3 varicocele and symmetric testes appropriate for age, 22 respondents (59%) indicated that they would observe the patient, whereas 15 respondents (41%) indicated that they would treat the varicocele. In contrast, in the second scenario reflecting a grade 2 varicocele with ipsilateral testicular hypoplasia, 28 respondents (75%) indicated that they would treat the varicocele, whereas 9 respondents (25%) indicated that they would continue to observe the patient.
DISCUSSION
Varicocele is the most common cause of surgically correctable infertility in men and is a progressive disease that causes deterioration in the testicular function and semen parameters.1,11 In contrast, the management of pediatrics and adolescents with varicocele remains controversial, as the study of Bogaert et al. suggests that treatment of the varicocele at diagnosis does not appear to improve later chances of paternity.5 However, many investigators believe that the duration of exposure to varicocele results in progressive worsening of the testicular function.12 In adolescents, varicocele treatment is typically performed with testicular asymmetry. Some studies supported the concept of early varicocelectomy to allow "catch-up-growth" of the affected testis, although the impact of this treatment on fertility is unknown.13,14 However, other studies reported a significant testicular catch-up growth without surgery.15 Moursy et al.16 reported that a catch-up testicular growth was observed in 70% of surgical patients and 50% of nonsurgical patients. Such conflicting data make it difficult to define clear indications for treatment.
Paduch and Niedzielski17 reported that varicoceles have been associated with a significant decrease in sperm motility and vitality in untreated men aged 17-19 years. Although semen analysis is the most objective test to assess testicular function, it is difficult to be done in children and young adolescents.
In several studies, it has been shown that a repair of a varicocele increased serum testosterone,18,19 resulting in testicular growth correlating with increased serum testosterone.20 These studies support a relationship between varicocele and the development of hypogonadism or androgen deficiency.
In this survey, all respondents have seen pediatric and adolescent patients with varicoceles on their routine practice with the majority of them working in academic hospitals, and a significant proportion having practiced for >10 years. The study by Richter et al.9 in 2001 surveyed both pediatric urologists as well as adult urologists having interest in infertility, and the study by Alexander et al.10 in 2014 surveyed only pediatric urologists. This study surveyed 37 members of Korean Society of Pediatric Urology. In this survey 97% of respondents treat varicoceles by themselves. This is in accordance with the previous surveys.9,10
The most common indication for surgical intervention was testicular size discrepancy. This is in accordance with previously published studies in 2001 and 2014.9,10 However, our questionnaire did not specifically evaluate the criteria for any specific testicular size discrepancy which may prompt the decision for surgical repair. According to a recent survey study that examined the approach to asymptomatic grade 2 and 3 varicoceles by pediatric urologists,21 85% of respondents defined a "significant" testicular size discrepancy as >20% which prompts surgical management and 59% of respondents would repeat measurements in 6 to 12 months.
In this survey, only 76% of urologists used optical magnification during surgical repair, while 90% of United States' urologists on the 2001 survey and 100% of United States' pediatric urologists on the 2014 survey used optical magnification with a microscope or optical loupes during surgical repair.
Cayan et al.22 analyzed 36 studies and they concluded that microsurgical varicocelectomy is associated with higher spontaneous pregnancy rates and less postoperative recurrence compared with other varicocelectomy techniques including the Palomo technique, laparoscopic varicocelectomy techniques, radiologic embolization, and macroscopic inguinal (Ivanissevich) varicocelectomy. Similarly, Diegidio et al.23 reviewed 33 studies, and they concluded that the pregnancy rate was highest for microsurgical subinguinal (45%) or microsurgical inguinal technique (42%).
According to the 2001 survey, the most common surgical approach was inguinal (36%), followed by subinguinal (30%), retroperitoneal (Palomo; 21%), and laparoscopic (10%). In a 2014 study, the most common surgical approach was the laparascopic approach (38%), followed by the subinguinal (33%), inguinal (14%), and retroperitoneal (13%). It reflects that laparoscopic surgery has gained popularity in U.S. In our survey, however, the most common surgical approach was subinguinal microsurgical (52%), followed by inguinal, laparoscopic (artery sparing), and open retroperitoneal (Palomo). There is a trend toward less invasive surgery including laparoscopic ones in many fields of medicine, but we are not sure which surgery is less invasive between the microscopic (sub)inguinal varicocelectomy and laparoscopic varicocelectomy, given that microscopic varicocelectomy requires a single small incision as long as it affords testis delivery.
According to clinical scenarios of previous study in 2014 in United States,10 93% of respondents chose to observe grade 3 adolescent varicocele with symmetric testes, and 44% of respondents chose to observe grade 2 adolescent varicocele with ipsilateral testicular hypoplasia. Our survey, on the other hand, showed 59% and 22% of respondents chose to observe in the similar clinical scenarios indicating more physicians in Korea treat rather than observe.
Although the response rate of this study was more than 50%, a drawback of this study is that the responses do not reflect the practice patterns of all pediatric urologists. Furthermore, because our survey targeted only pediatric urologists, we could not compare with other urologists who treat varicocele. Besides, there is a degree of selection bias in this study. The response rate from academicians (n=29, 78%) was overrepresented and likely contributes to the results, such as the usages of US and Doppler US in the diagnosis of varicocele. Despite these limitations, our study is the first survey to evaluate the diagnosis and management of pediatric and adolescent varicoceles outside of United States. Due to limited and conflicting data regarding pediatric and adolescent varicocele, evidence-based guidelines for management of pediatric and adolescent varicocele are lacking. We believe that initiating a discussion about the management of pediatric and adolescent varicoceles is important, and this study provides a valuable reference for studies about pediatric and adolescent varicoceles not just in Korea but also in other countries.
In conclusion, our survey demonstrates that there is lack of consensus on diagnosis and management of pediatric and adolescent varicocele among pediatric urologists in Korea, except indication for varicocelectomy deriving from a decrease in ipsilateral testicular size. A prospective randomized study of pediatric and adolescent varicoceles is needed to assess the outcomes and develop universal management guidelines.
Footnotes
CONFLICT OF INTEREST STATEMENT: None declared.
References
- 1.Akbay E, Cayan S, Doruk E, Duce MN, Bozlu M. The prevalence of varicocele and varicocele-related testicular atrophy in Turkish children and adolescents. BJU Int. 2000;86:490–493. doi: 10.1046/j.1464-410x.2000.00735.x. [DOI] [PubMed] [Google Scholar]
- 2.Meacham RB, Townsend RR, Rademacher D, Drose JA. The incidence of varicoceles in the general population when evaluated by physical examination, gray scale sonography and color Doppler sonography. J Urol. 1994;151:1535–1538. doi: 10.1016/s0022-5347(17)35295-3. [DOI] [PubMed] [Google Scholar]
- 3.Kass EJ. Adolescent varicocele: current concepts. Semin Urol. 1988;6:140–145. [PubMed] [Google Scholar]
- 4.Dabaja A, Wosnitzer M, Goldstein M. Varicocele and hypogonadism. Curr Urol Rep. 2013;14:309–314. doi: 10.1007/s11934-013-0339-4. [DOI] [PubMed] [Google Scholar]
- 5.Bogaert G, Orye C, De Win G. Pubertal screening and treatment for varicocele do not improve chance of paternity as adult. J Urol. 2013;189:2298–2303. doi: 10.1016/j.juro.2012.12.030. [DOI] [PubMed] [Google Scholar]
- 6.Sawczuk IS, Hensle TW, Burbige KA, Nagler HM. Varicoceles: effect on testicular volume in prepubertal and pubertal males. Urology. 1993;41:466–468. doi: 10.1016/0090-4295(93)90510-h. [DOI] [PubMed] [Google Scholar]
- 7.Gorenstein A, Katz S, Schiller M. Varicocele in children: "to treat or not to treat"--venographic and manometric studies. J Pediatr Surg. 1986;21:1046–1050. doi: 10.1016/0022-3468(86)90005-9. [DOI] [PubMed] [Google Scholar]
- 8.Fontana D, Fasolis G, Rolle L, Bellina M. [Indications for correction of varicocele] Arch Ital Urol Nefrol Androl. 1990;62:171–175. [PubMed] [Google Scholar]
- 9.Richter F, Stock JA, LaSalle M, Sadeghi-Nejad H, Hanna MK. Management of prepubertal varicoceles-results of a questionnaire study among pediatric urologists and urologists with infertility training. Urology. 2001;58:98–102. doi: 10.1016/s0090-4295(01)01118-9. [DOI] [PubMed] [Google Scholar]
- 10.Pastuszak AW, Kumar V, Shah A, Roth DR. Diagnostic and management approaches to pediatric and adolescent varicocele: a survey of pediatric urologists. Urology. 2014;84:450–455. doi: 10.1016/j.urology.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 11.Lemack GE, Uzzo RG, Schlegel PN, Goldstein M. Microsurgical repair of the adolescent varicocele. J Urol. 1998;160:179–181. [PubMed] [Google Scholar]
- 12.Vasavada S, Ross J, Nasrallah P, Kay R. Prepubertal varicoceles. Urology. 1997;50:774–777. doi: 10.1016/S0090-4295(97)00332-4. [DOI] [PubMed] [Google Scholar]
- 13.Kass EJ, Belman AB. Reversal of testicular growth failure by varicocele ligation. J Urol. 1987;137:475–476. doi: 10.1016/s0022-5347(17)44072-9. [DOI] [PubMed] [Google Scholar]
- 14.Laven JS, Haans LC, Mali WP, te Velde ER, Wensing CJ, Eimers JM. Effects of varicocele treatment in adolescents: a randomized study. Fertil Steril. 1992;58:756–762. doi: 10.1016/s0015-0282(16)55324-2. [DOI] [PubMed] [Google Scholar]
- 15.Kolon TF, Clement MR, Cartwright L, Bellah R, Carr MC, Canning DA, et al. Transient asynchronous testicular growth in adolescent males with a varicocele. J Urol. 2008;180:1111–1114. doi: 10.1016/j.juro.2008.05.061. [DOI] [PubMed] [Google Scholar]
- 16.Moursy EE, ElDahshoury MZ, Hussein MM, Mourad MZ, Badawy AA. Dilemma of adolescent varicocele: long-term outcome in patients managed surgically and in patients managed expectantly. J Pediatr Urol. 2013;9:1018–1022. doi: 10.1016/j.jpurol.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 17.Paduch DA, Niedzielski J. Semen analysis in young men with varicocele: preliminary study. J Urol. 1996;156:788–790. doi: 10.1097/00005392-199608001-00063. [DOI] [PubMed] [Google Scholar]
- 18.Tanrikut C, Goldstein M, Rosoff JS, Lee RK, Nelson CJ, Mulhall JP. Varicocele as a risk factor for androgen deficiency and effect of repair. BJU Int. 2011;108:1480–1484. doi: 10.1111/j.1464-410X.2010.10030.x. [DOI] [PubMed] [Google Scholar]
- 19.Su LM, Goldstein M, Schlegel PN. The effect of varicocelectomy on serum testosterone levels in infertile men with varicoceles. J Urol. 1995;154:1752–1755. [PubMed] [Google Scholar]
- 20.Sathya Srini V, Belur Veerachari S. Does varicocelectomy improve gonadal function in men with hypogonadism and infertility? Analysis of a prospective study. Int J Endocrinol. 2011;2011:916380. doi: 10.1155/2011/916380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coutinho K, McLeod D, Stensland K, Stock JA. Variations in the management of asymptomatic adolescent grade 2 or 3 left varicoceles: a survey of practitioners. J Pediatr Urol. 2014;10:430–434. doi: 10.1016/j.jpurol.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 22.Cayan S, Shavakhabov S, Kadioğlu A. Treatment of palpable varicocele in infertile men: a meta-analysis to define the best technique. J Androl. 2009;30:33–40. doi: 10.2164/jandrol.108.005967. [DOI] [PubMed] [Google Scholar]
- 23.Diegidio P, Jhaveri JK, Ghannam S, Pinkhasov R, Shabsigh R, Fisch H. Review of current varicocelectomy techniques and their outcomes. BJU Int. 2011;108:1157–1172. doi: 10.1111/j.1464-410X.2010.09959.x. [DOI] [PubMed] [Google Scholar]