Abstract
Background
The supraclavicular artery island flap (SAIF) has recently been re-popularized as a versatile and reliable option for reconstruction of oncological head and neck defects. Prior ipsilateral neck dissection or irradiation is considered a relative contraindication to its use. The aim of this study was to describe the safety and utility of the SAIF for head and neck reconstruction in the setting of neck dissection and radiation.
Methods
A retrospective chart review was performed of consecutive SAIF reconstructions at two institutions between May 2011 and 2014. In addition to demographic data, comorbidities, indications, surgical characteristics, data about radiation treatment and neck dissection were specifically recorded. Donor and recipient site complications were noted. Fisher exact test was performed to analyze if neck dissection or radiation were associated with complications.
Results
Twenty-two patients underwent SAIF reconstruction for an array of head and neck defects. Donor site infection was noted in 1 patient. Recipient site complications included, wound dehiscence (n=2), oro-cutaneous fistula (n=1), carotid blowout (n=1) and total flap loss (n=1). There was no association between prior neck dissection or radiation treatment and flap loss (p=1.00).
Conclusion
The SAIF is safe to use in patients who have had ipsilateral neck dissection involving level IV or V lymph nodes and/or radiation treatment to the neck. It can be used alone or in combination with other flaps for closure of a variety of head and neck defects.
Introduction
Due to the paucity of local flaps available in the head and neck region, the supraclavicular artery island flap (SAIF) has recently become re-popularized in light of its versatility and reliability.1-11 The SAIF is supplied by perforators of the supraclavicular artery, which originates in the anatomic posterior triangle of neck formed by the posterior border of the sternocleidomastoid muscle, external jugular vein and clavicle. Since head and neck cancer patients frequently have had prior radiotherapy or ipsilateral neck dissection, the patency of the supraclavicular and transverse cervical arteries cannot reliably be ensured. The safest option for the reconstructive surgeon is to use the SAIF from the uninvolved neck; however, this option may only be available for midline surgical defects such as following pharyngectomy. While preoperative imaging is a potential method of verifying supraclavicular artery patency, due to its small size, it's often unable to be visualized with CT scans or angiography.12
Prior radiotherapy or ipsilateral neck dissection may be considered relative contraindications to SAIF harvest. The aim of the current study is to describe use of the SAIF in this setting. The hypothesis is that the SAIF can be safely used in patients who have undergone either concurrent or previous neck dissection and/or prior radiotherapy. A secondary aim was to demonstrate the versatility of the SAIF in head and neck reconstruction.
Methods
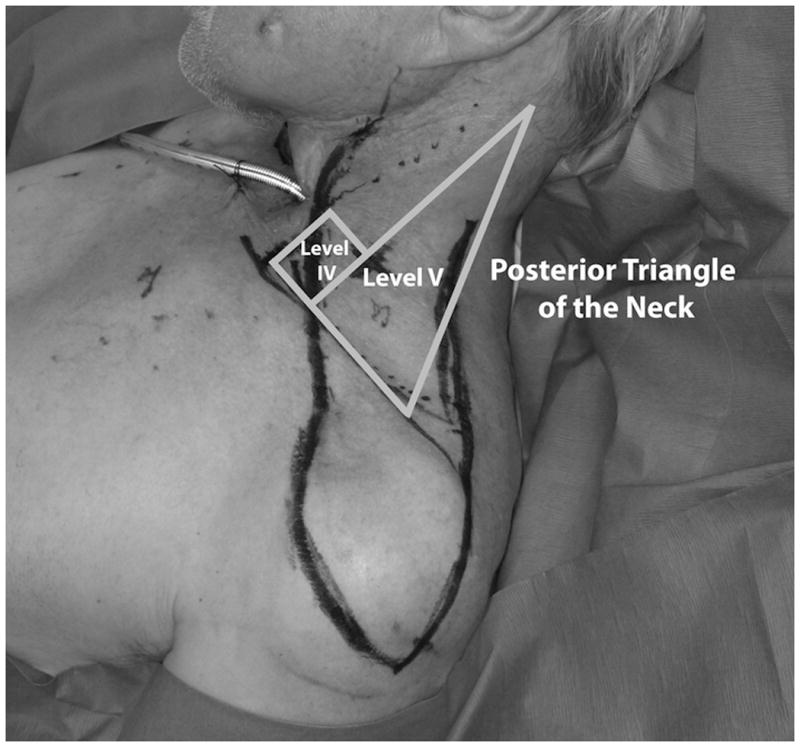
A retrospective chart review was performed of consecutive SAIF reconstructions between May 2011 and May 2014 for oncological head and neck defects at Memorial Sloan-Kettering Cancer Center and Montefiore Medical Center. Institutional review board approval was obtained at both institutions prior to initiation of the study. Demographic data were tabulated including socio-demographic/oncologic variables, surgical characteristics and postoperative complications. Information on previous radiation treatment as well as prior or concurrent level IV/V neck dissection was specifically sought from the medical records (Figure 1). Fisher's exact test was performed to calculate a correlation between history of radiation and/or neck dissection and recipient site complication using STATA statistical software (College Station, TX).
Figure 1. Preoperative photo showing SAIF design with overlay of anatomic level IV and V nodal dissection.
Results
Twenty-two patients were identified from the two centers. Eighteen (82%) were male and four (18%) were female patients. The mean age of patients was 68 years (Range: 51 – 83 years). Medical comorbidities and pathologic diagnosis for the patient cohort is given in Table 1. The SAIF was most commonly performed for partial laryngectomy or pharyngectomy closure in approximately half (13/22) the patients. The remainder of surgical indications for reconstruction is given in Table 2. Twelve flaps (55%) were performed from the patient's right side whereas 10 (45%) flaps were harvested from the left side. There were no thoracic duct injuries in any of the left-sided flap harvests. Fifteen patients (68%) had a history of previous neck irradiation and seventeen patients (77%) underwent an ipsilateral neck dissection. Mean dose of radiation given to the neck was 7000 cGy. Of the patients who had ipsilateral neck dissection, 6 (40%) had Level IV without Level V, 1 (7%) had Level V without IV and 8 (53%) had both level IV and V dissections. Eleven (65%) patients had SAIF harvest performed in the same setting as the ipsilateral neck dissection. The mean flap size was 6 × 18 cm with primary donor site closure in 82% of patients and split thickness skin graft in the remainder (Table 3).
Table 1. Patient demographics and diagnosis.
| Variable | |
|---|---|
|
| |
| Age in years, mean (range) | 68 (51 – 83) |
| Gender, n (%) | |
| Male | 18 (82%) |
| Female | 4 (18%) |
| Medical comorbidities, n (%) | |
| CAD | 3 (14%) |
| DM | 5 (23%) |
| Smoking History, n (%) | 15 (68%) |
| Diagnosis, (n) | |
| SCC Larynx | 8 |
| SCC Pharynx | 5 |
| Oro-mandible Cancer | 4 |
| SCC Temporal Bone | 1 |
| Melanoma of Mastoid Skin | 1 |
| Lung Cancer | 1 |
| Esophageal Cancer | 1 |
| Parotid Metastasis | 1 |
CAD: Coronary Artery Disease, DM: Diabetes Mellitus, SCC: Squamous Cell Carcinoma
Table 2. Indications for reconstruction.
| Indication | No. of patients |
|---|---|
| A) Hypopharynx Defect | |
| i) Circumferential | 1 |
| ii) Partial | 4 |
| B) Fistula | |
| i) Pharyngocutaneous | 2 |
| ii) Tracheoesophageal | 2 |
| C) Skin | |
| i) Cervical | 8 |
| ii) Mastoid | 1 |
| D) Oral Cavity | |
| i) Hemimandible | 1 |
| ii) Floor of mouth defect | 2 |
| E) Other | |
| i) Skull base defect | 1 |
Table 3. Surgical characteristics.
| Laterality of SAIF, n (%) | |
| Right | 12 (55%) |
| Left | 10 (45%) |
|
| |
| Flap Size (mean) | |
| Length | 6 cm |
| Width | 18 cm |
|
| |
| History of Radiotherapy (XRT), n (%) | |
| Yes | 15 (68%) |
| No | 7 (32%) |
|
| |
| History of Ipsilateral Neck Dissection (ND), n (%) | |
| Yes | 17 (77%) |
| No | 5 (23%) |
|
| |
| History of: | |
| Both XRT and Ipsilateral ND | 12 (55%) |
| Either XRT or Ipsilateral ND | 8 (36%) |
| Neither XRT or Ipsilateral ND | 2 (9%) |
|
| |
| Level of Ipsilateral Neck Dissection,* n (%) | |
| IV without V | 6 (40%) |
| V without IV | 1 (7%) |
| IV and V | 8 (53%) |
|
| |
| Timing of Neck Dissection with respect to SAIF harvest,* n (%) | |
| Simultaneous | 11 (65%) |
| Prior to Operation | 6 (35%) |
|
| |
| Donor Site Closure, n (%) | |
| Primary | 18 (82%) |
| Split-Thickness Skin Graft | 4 (18%) |
Five patients did not have any neck dissection and two patients did not have an ipsilateral neck dissection.
One patient (4.5%) had a donor site infection that responded to conservative management. Five (23%) patients had recipient site complications: wound dehiscence (n=2), oro-cutaneous fistula (n=1), carotid blowout (n=1) and total flap loss (n=1). Both cases of wound dehiscence responded to dressing changes. The case of oro-cutaneous fistula led to adhesion of tongue to the floor of mouth and responded to release of adhesions in the operating room. The carotid blowout necessitated emergency surgery. The only total flap loss occurred in a patient with an anterior cervical skin defect following laryngectomy with jejunal flap reconstruction. This patient had a concurrent level II-IV ipsilateral neck dissection and previous radiotherapy. Salvage with a pectoralis myocutaneous flap was required for soft tissue coverage. There was no statistical association between prior neck irradiation and / or ipsilateral neck dissection and flap loss (p = 1.00).
Discussion
Previous ipsilateral neck irradiation or nodal dissection at the time of current or prior surgery may be considered a relative contraindication for use of the SAIF in head and neck reconstruction. Radiotherapy is a possible source of vascular compromise such as thrombosis, to either the transverse cervical artery or supraclavicular perforator. Ipsilateral nodal dissection, specifically at level IV or V, is a second potential source of injury to the flap blood supply. Furthermore, even if the transverse cervical artery is preserved in the process of neck dissection, often the skin in the posterior triangle is elevated or retracted harming the skin perforators. In the current series, the majority of patients had either neck dissection or irradiation yet only one patient had clinically relevant flap loss (Table 3); therefore, previous neck irradiation or a nodal dissection of the ipsilateral neck should not be considered a contraindication for SAIF use. The single patient who experienced a flap loss received both radiation and ipsilateral nodal dissection so perhaps these patients should be approached with the most caution and counseled about the risk for flap loss. Although the current report supports the safety of the SAIF, it remains preferable to harvest the flap from a side without prior intervention when possible. Finally, because the thoracic duct enters the subclavian vein on the left, this may be an additional consideration when choosing the side of flap harvest. With this background in mind, surgeons are urged to approach each case individually evaluating the entire medical and surgical background of the patient. If a patient has a radiation-crippled neck with extensive prior nodal harvest, the potential for SAIF loss can never be eliminated so other reconstructive alternatives should be considered including preparation for possible free or pectoralis myocutaneous (PM) flap.13,14
The SAIF is not without donor site morbidity. Flaps wider than approximately 5-6 cm may require a skin graft for closure that are frequently associated with delayed healing. This can be particularly problematic for women when wearing a brasserie. The one donor site infection in the current series was the result of a communication between a contaminated tracheoesophageal fistula defect and the donor site. Surgical defects in contaminated spaces, such as the pharynx, larynx and oral cavity can always be a source of infection tracking between the tunnel of the donor and recipient site.
Reconstructive advantages leading to popularity of the SAIF are its reliable vascular supply, wide arc of rotation, short harvest time, thinness, and excellent color match to head and neck region. Due to a lack of vascular anastomosis, the flap is an attractive option for vessel depleted necks due to previous surgeries and also doesn't require microsurgical training. Prior to the recent expansion in its use over the last 7 years, the only regional flaps widely used in the head and neck area were the deltopectoral (DP), internal mammary artery perforator (IMAP) and PM flaps. Some differences between the SAIF and other regional flaps are worth highlighting. The SAIF should not be considered superior to the PM flap, but rather a complementary alternative. For example the PM flap is excellent for providing bulk and obliterating surgical dead-space such as following a laryngectomy with bilateral neck dissections. If the SAIF donor area can be closed primarily, it may be a superior alternative to either the IMAP or DP flap that are considered relatively thin flaps. The DP flap has disadvantages such as the need for skin grafting of the donor areas as well as a limited arc of rotation because of its broad base. While both the SAIF and IMAP flap have narrow bases with wide arcs of rotation as well as ability for primary donor site closure, the IMAP flap lies farther away from the head and neck area so cannot reliably reach oral cavity or mastoid defects. Finally, the SAIF can be harvested from each arm/neck without placing tension on the opposite side donor site closure. This is unlikely for a PM flap where tension closure on one side is likely to compromise the other.
A comparison of the SAIF with traditional reconstructions including free flaps for various oncological defects in the head and neck region is performed here in order to demonstrate its widespread utility. For circumferential pharyngeal defects, standard reconstructions involve tubularized free flaps such as the anterolateral thigh (ALT) flaps or jejunal flaps. The thin nature of the SAIF is an alternative option for use in patients who are poor candidates for free tissue transfer or absent recipient vessels following prior radiation treatment or neck dissection (Figure 2).1,2 For circumferential pharyngeal defects with absent overlying skin, the SAIF is a simple pedicle flap to resurface the neck following free tissue transfer. Although the double island ALT flap is well described, inadequate perforator position and presence make this option unpredictable.15 For partial pharyngeal defects the principle considerations are the amount of surgical dead space present and whether or not overlying neck skin needs replacement. Whereas PM flap adequately fills dead space and easily closes the pharyngeal defect, the bulk sometimes precludes primary skin closure because of poorly compliant radiated skin, thus necessitating skin grafting. Further the bulk of the PM flap may cause overhanging of the tracheostoma with airway obstruction. The single or double island radial forearm flap (RFF) or ALT flap can be used depending upon need for external skin. Alternatively, the SAIF can be combined with the RFF or ALT flap as a second flap. Tracheoesophageal or pharyngocutaneous fistulas are traditionally reconstructed with free flaps, or regional flaps such as PM or IMAP flap. The close vicinity of the SAIF makes it equally useful without the need for free flaps when only a small amount of vascularized tissue is required in a tight space. Oral cavity defects involving either the floor of mouth or mandible while traditionally reconstructed with free flaps, the facial artery musculomucosal (FAMM) flap or PM flap can also be closed with the SAIF, if of limited size (Figure 3). Skull base or radical parotid defects are generally closed with buried free flaps, but have also been successfully closed with the SAIF in minimal time and with low donor site morbidity.3,4 Soft tissue skin defects of the face and neck not amenable to cervicofacial flaps, can also be closed with the SAIF, DP flap or PM flap (Figure 4). Finally, while the trapezius flap is considered the workhorse flap for posterior cervical defects, recently the SAIF was reported as an alternative when soft tissue bulk is not required.11
Figure 2. Circumferential hypopharynx defect.



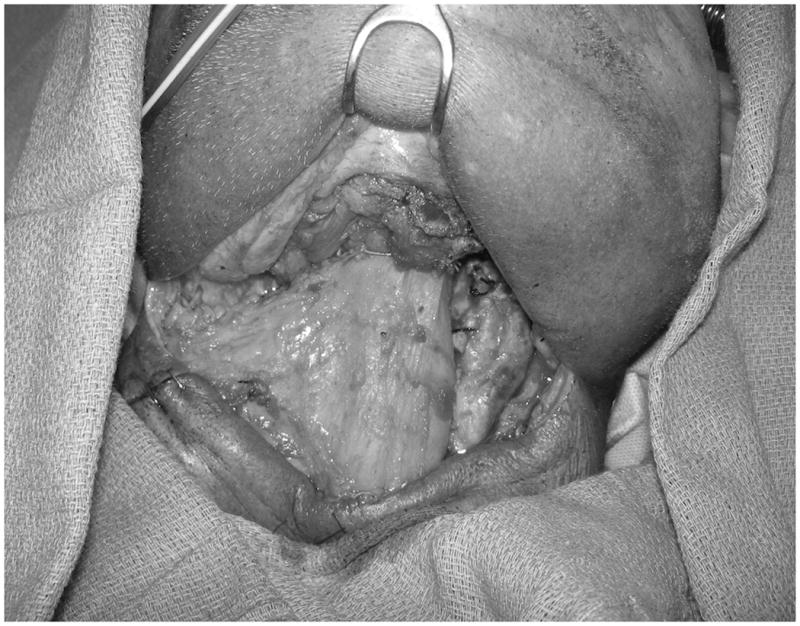
(a) Post-resection image, (b) SAIF elevated, (c) Flap tubularized around a syringe, (d) Flap inset to oropharynx and cervical esophagus.
Figure 3. Oral cavity defect.
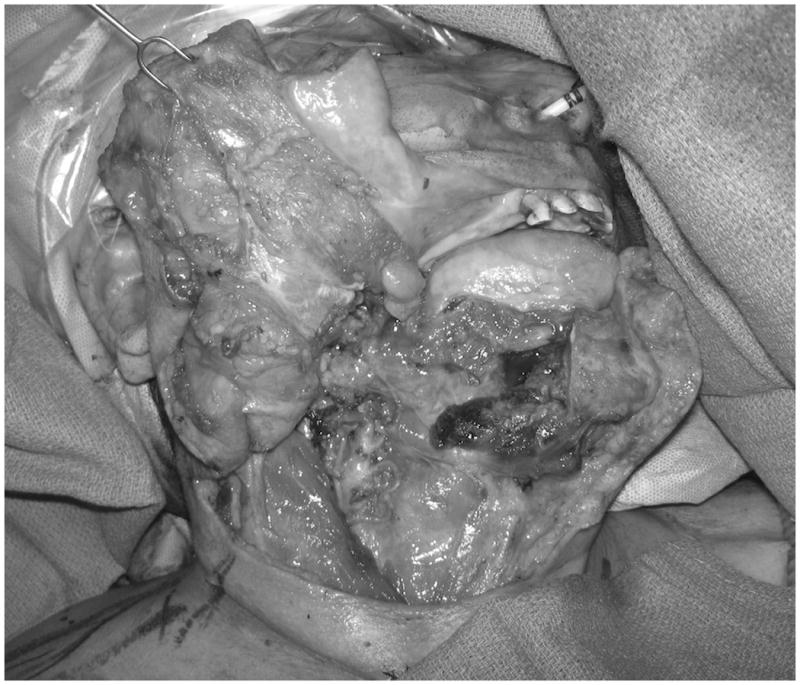



(a) Right hemi-mandible with floor of mouth and gingiva defect, (b) SAIF elevated with portions de-epithelialized, (c) SAIF brought through neck tunnel prior to insetting, (d) Flap inset into oral cavity.
Figure 4. Mastoid skin defect.



(a) Surgical defect, (b) SAIF elevated and transposed, (c) Final flap inset.
Conclusion
The SAIF is a safe and versatile flap that can be used to reconstruct a wide array of head and neck oncologic defects. A prior history of neck irradiation or ipsilateral neck dissection should not be a deterrent for flap use.
Acknowledgments
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748.
References
- 1.Chiu ES, Liu PH, Baratelli R, Lee MY, Chaffin AE, Friedlander PL. Circumferential pharyngoesophageal reconstruction with a supraclavicular artery island flap. Plast Reconstr Surg. 2010;125(1):161–166. doi: 10.1097/PRS.0b013e3181c4951e. [DOI] [PubMed] [Google Scholar]
- 2.Chiu ES, Liu PH, Friedlander PL. Supraclavicular artery island flap for head and neck oncologic reconstruction: indications, complications, and outcomes. Plast Reconstr Surg. 2009;124(1):115–123. doi: 10.1097/PRS.0b013e3181aa0e5d. [DOI] [PubMed] [Google Scholar]
- 3.Levy JM, Eko FN, Hilaire HS, Friedlander PL, Melgar MA, Chiu ES. Posterolateral skull base reconstruction using the supraclavicular artery island flap. J Craniofac Surg. 2011;22(5):1751–1754. doi: 10.1097/SCS.0b013e31822e62e9. [DOI] [PubMed] [Google Scholar]
- 4.Emerick KS, Herr MW, Lin DT, Santos F, Deschler DG. Supraclavicular artery island flap for reconstruction of complex parotidectomy, lateral skull base, and total auriculectomy defects. JAMA Otolaryngol Head Neck Surg. 2014;140(9):861–866. doi: 10.1001/jamaoto.2014.1394. [DOI] [PubMed] [Google Scholar]
- 5.Kokot N, Mazhar K, Reder LS, Peng GL, Sinha UK. The supraclavicular artery island flap in head and neck reconstruction: applications and limitations. JAMA Otolaryngol Head Neck Surg. 2013;139(11):1247–1255. doi: 10.1001/jamaoto.2013.5057. [DOI] [PubMed] [Google Scholar]
- 6.Granzow JW, Suliman A, Roostaeian J, Perry A, Boyd JB. The supraclavicular artery island flap (SCAIF) for head and neck reconstruction: surgical technique and refinements. Otolaryngol Head Neck Surg. 2013;148(6):933–940. doi: 10.1177/0194599813484288. [DOI] [PubMed] [Google Scholar]
- 7.Granzow JW, Suliman A, Roostaeian J, Perry A, Boyd JB. Supraclavicular artery island flap (SCAIF) vs free fasciocutaneous flaps for head and neck reconstruction. Otolaryngol Head Neck Surg. 2013;148(6):941–948. doi: 10.1177/0194599813476670. [DOI] [PubMed] [Google Scholar]
- 8.Pallua N, Wolter T. Defect classification and reconstruction algorithm for patients with tracheostomy using the tunneled supraclavicular artery island flap. Langenbecks Arch Surg. 2010;395(8):1115–1119. doi: 10.1007/s00423-010-0654-x. [DOI] [PubMed] [Google Scholar]
- 9.Vinh VQ, Ogawa R, Van Anh T, Hyakusoku H. Reconstruction of neck scar contractures using supraclavicular flaps: retrospective study of 30 cases. Plast Reconstr Surg. 2007;119(1):130–135. doi: 10.1097/01.prs.0000244843.49596.e5. [DOI] [PubMed] [Google Scholar]
- 10.Nthumba PM. The supraclavicular artery flap: a versatile flap for neck and orofacial reconstruction. J Oral Maxillofac Surg. 2012;70(8):1997–2004. doi: 10.1016/j.joms.2011.08.043. [DOI] [PubMed] [Google Scholar]
- 11.Razdan SN, Ro T, Albornoz CR, Bilsky MH, Matros E. Case report of a supraclavicular artery island flap for reconstruction of a nonhealing cervical spine wound. J Reconstr Microsurg. 2014 Nov 11; doi: 10.1055/s-0034-1393693. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Adams AS, Wright MJ, Johnston S, et al. The use of multislice CT angiography preoperative study for supraclavicular artery island flap harvesting. Ann Plast Surg. 2012;69(3):312–315. doi: 10.1097/SAP.0b013e31822afaba. [DOI] [PubMed] [Google Scholar]
- 13.Teo KG, Rozen WM, Acosta R. The pectoralis major myocutaneous flap. J Reconstr Microsurg. 2013;29(7):449–456. doi: 10.1055/s-0033-1343832. [DOI] [PubMed] [Google Scholar]
- 14.Chao JW, Spector JA, Taylor EM, et al. Pectoralis major myocutaneous flap versus free fasciocutaneous flap for reconstruction of partial hypopharyngeal defects: What should we be doing? J Reconstr Microsurg. 2014 Nov 11; doi: 10.1055/s-0034-1395417. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 15.Yu P, Selber J, Liu J. Reciprocal dominance of the anterolateral and anteromedial thigh flap perforator anatomy. Ann Plast Surg. 2013;70(6):714–716. doi: 10.1097/SAP.0b013e318241446c. [DOI] [PubMed] [Google Scholar]


