Abstract
Introduction:
India is one of the countries with high prevalence of anemia during pregnancy. Anemia in pregnancy is multifactorial. Iron deficiency anemia is the most common conditions in a pregnant woman. As per ayurvedic classics, this condition occurs due to improper Rasa Dhatu in mother and continuously increasing fetal demands and is considered as Rasa Pradoshajavikara. A large number of Lauha preparations have been used widely for centuries to cure Anemia.
Aim:
To evaluate efficacy of Punarnava Mandura and Dhatri Lauha on Garbhini Pandu.
Materials and Methods:
A total 24 pregnant women with symptoms of Garbhini Pandu were randomly divided into two groups (A and B). In Group A (n = 15) Punarnava Mandura, two tablets (each of 500 mg) thrice a day with one cup (100 ml) of buttermilk and in Group B (n = 9) Dhatri Lauha, two tablets (each of 500 mg) thrice a day with luke warm water were administered for 90 days. The assessment was done with subjective parameters such as pallor, general weakness, dyspnea, etc., and objective parameters such as hematological parameters. Results were statistically analyzed using Student's t-test.
Results:
The results revealed that overall clinical improvement was better in Group A when compared to Group B. Hemoglobin was increased in patients of Group A, which was statistically significant. No adverse drug reaction was observed during the treatment period.
Conclusion:
Punarnava Mandura is more effective on Garbhini Pandu in comparison to Dhatri Lauha.
Keywords: Anemia, Dhatri Lauha, Garbhini Pandu, Punarnava Mandura
Introduction
Anemia is the most common nutritional deficiency disorder in the world. WHO has estimated that prevalence of anemia in pregnant women is 14% in developed and 51% in developing countries and among them, 65–75% are in India.[1] The prevalence of anemia in all the age groups is higher in India as compared to other developing countries.[1] India contributes to about 80% of the maternal deaths due to anemia in South Asia.[2] The high prevalence of anemia in pregnancy and serious adverse consequences in both mother and baby, the management of anemia in pregnancy was accorded a very high priority both in obstetric and public health practice.
There are no direct references of Garbhini Pandu (anemia in pregnancy) in Ayurveda, except Acharya Kashyapa has described Pandu as a symptom of Garbhini in the description of Rakta Gulma,[3] Acharya Harita has also described Vivarnatva as one of the eight complications of Garbha.[4]
Empirical use of different preparations of iron in the treatment of anemia from ancient times is evident. Lauha Bhasma and Mandura Bhasma are effective in Pandu Roga. On the basis of Pandughna (antianemic), Prinana (nourishing), Raktaprasadana (blood toner) properties and previous reports in Garbhini Pandu,[5] Dhatri Lauha was selected in this study. Punarnava Mandura is successfully used by Ayurvedic physicians for the management of all types of Pandu. Government of India has included it in ASHA drug kit for National Reproductive Health Care Programme.[6] In the previous study carried out on Pandu (iron deficiency anemia [IDA]), Punarnava Mandura and Dhatri Lauha,[7] both were given in dose of 500 mg thrice in a day, satisfactory results were not achieved. The reason noticed for this was low dose of drug. Thus, for the present study, the dose of both the drugs was increased and planned to evaluate the clinical efficacy of both the drugs with increased dose (3 g/day) on Garbhini Pandu.
Materials and Methods
Patients of Garbhini Pandu (n = 24) were selected from the outpatient department of Stree Roga and Prasooti Tantra of Institute for Post Graduate Teaching and Research in Ayurveda (IPGT and RA) Hospital, Jamnagar. Those patients fulfilling the criteria for selection were included into the study irrespective of caste, religion, etc. The study was started after getting approval by the Institutional Ethics Committee (No. PGT/7/-A/Ethics/2013-2014/1767; Date. 10/09/2013). Informed written consent was obtained from each patient before starting the treatment.
Inclusion criteria
Pregnant women, belonging to the age group of 18 to 40 years having clinical signs and symptoms of Garbhini Pandu, i.e., Panduta (pallor), Bhrama (giddiness), Daurbalya (general weakness), Shwasa (dyspnea)
Patients of second or third trimester of pregnancy with 6 g% to 10 g% of hemoglobin
Microcytic hypochromic appearance of red blood cells in peripheral smear.
Exclusion criteria of patient
First trimester of pregnancy
Patients suffering from pregnancy-related complications such as pregnancy-induced hypertension, hyper emesis gravidarum, pre eclampsia, etc.
Patients with high-risk pregnancy
Patients having Hb% count <6 g% and more than 10 g%.
Investigations
Hematological
Hemoglobin (Hb)%, total red blood corpuscles (TRBC), total leukocytes count (TLC), differential leukocytes count (DLC), platelet count, erythrocyte sedimentation rate (ESR), packed cell volume (PCV), mean cell volume (MCV), Mean corpuscular hemoglobin (MCH), Mean corpuscular hemoglobin concentration (MCHC), and peripheral blood picture.
Specific tests for assessing iron status
Serum ferritin, serum iron, total iron binding capacity (TIBC), and transferrin saturation percentage were carried out in all the patients before and after treatment. All the investigations were carried out before and after the treatment.
Grouping and posology
The selected patients were randomly divided by simple random sampling method into two groups, A and B.
Group A (n = 15): In this group, two tablets of Punarnava Mandura (500 mg each) thrice a day; before breakfast, lunch, and dinner with one cup of buttermilk were administered for 90 days
Group B (n = 9): In this group, two tablets of Dhatri Lauha (500 mg each) thrice a day; before breakfast, lunch, and dinner with one cup of lukewarm water were administered for 90 days.
All the ingredients of formulations were procured from the Pharmacy of Gujarat Ayurved University and authenticated in the Pharmacognosy Laboratory of IPGT and RA, Jamnagar. Gomutra was collected from local areas. The trial drugs Punarnava Mandura and Dhatri Lauha were prepared in Pharmacy of Gujarat Ayurved University by following classical guidelines.
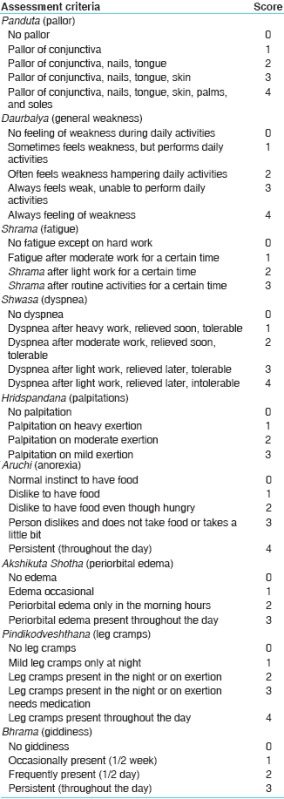
Assessment criteria
The effects of treatment after giving medications were assessed with regards to subjective and objective criteria before and after the treatment.
Subjective parameters
Objective parameters
Hematological parameters: Hb%, TRBC, PCV, MCV, MCH, MCHC
Specific markers of IDA: Serum ferritin, serum iron, serum TIBC, transferrin saturation %.
Assessment for overall effect of therapy
Complete remission: 100% relief in the signs and symptoms
Marked improvement: Above 76%
Moderate improvement: 51–75% relief in the signs and symptoms
Mild improvement: 26–50% relief in the signs and symptoms
Unchanged: Up to 25% relief.
Statistical analysis
Data were presented in terms of mean, standard deviation, standard error, and student t-test was considered at the level of P < 0.001 as highly significant, P < 0.05 or P < 0.01 as significant and P > 0.05 as insignificant.
Observations
In the present study, maximum number of patients, i.e., 51.85% belonged to age group of 23–27 years, 88.89% of patients were Hindu, 59.26% patients had primary education, 85.18% were housewives, 66.67% patients from lower middle class, 67.57% patients belonged to urban area, 62.96% patients were from joint family, and 48.14% were having 17–20 weeks of gestation. Maximum number of patients, i.e. 55.55% were of Vata-Pitta Prakriti.
Among the etiological factors, it was found that majority of the patients were vegetarians (59.26%) and having the habit of Vishamashana (62.96%). Most of the patients were taking excessive Lavana (92.59%), Amla Rasa (92.59%), Katu Rasa (81.48%), and Guru Guna dominant (66.67%) diet. Mandagni was found in 88.89% patients. Addiction of tea was found in 88.89% patients. In Viharaja Nidana, Diwaswapna was found in 100% of patients and habit of suppression of urination was found in 70.37% of patients. Majority of patients were suffering from Chinta (100%) and Bhaya (92.59%). Around 66.67% of patients have a normal menstrual history, 66.67% of patients were multigravida, while 59.26% were parous.
Out of 24 pregnant women screened for the present study, all patients (100%) were having pallor and complaint of general weakness, fatigue, and anorexia. 77.78% had dyspnea on exertion, 74.07% had palpitation, 62.96% had leg cramps, 66.67% had giddiness, and 40.74% had periorbital edema.
Results
Effect of therapy on subjective parameters
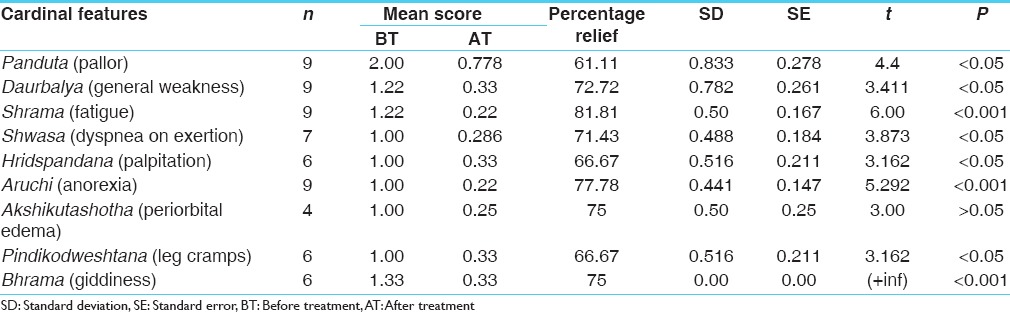
Group A provided highly significant (P < 0.001) result in Panduta, Daurbalya, Shrama, Shwasa, Hridspandana, Aruchi, Pindikodweshtana, and Bhrama whereas relief in Akshikuta Shotha was statistically significant (P < 0.05) [Table 1].
Table 1.
Effect on cardinal features of Garbhini Pandu in Group A

In Group B, statistically highly significant (P < 0.001) improvement was found on Shrama, Aruchi, and Bhrama while statistically significant (P < 0.05) improvement in Panduta, Daurbalya, Shwasa, Hridspandana, and Pindikodweshtana [Table 2].
Table 2.
Effect on cardinal features of Garbhini Pandu in Group B
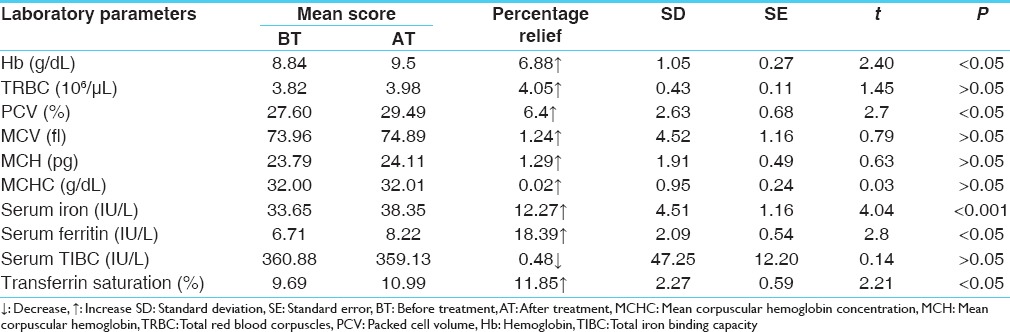
Effect of therapy on objective parameters
Group A provided improvement on all objective parameters of Garbhini Pandu. Increase in serum iron was highly significant (P < 0.001), whereas increase in Hb%, PCV, serum ferritin, and transferrin saturation was statistically significant (P < 0.05). Serum TIBC was decreased, but was statistically insignificant [Table 3].
Table 3.
Effect on laboratory parameters of Garbhini Pandu in Group A (n=15)
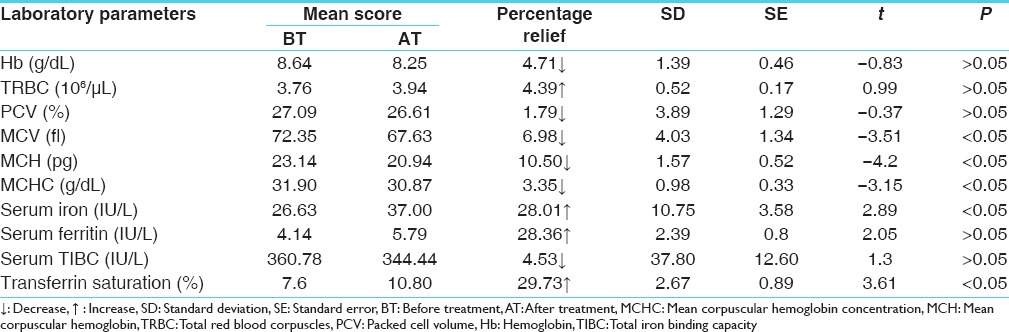
Group B provided statistically insignificant improvement on hematological parameters but serum iron and transferrin saturation were statistically improved (P < 0.05), whereas increase in serum ferritin and reduction in serum TIBC were statistically insignificant [Table 4].
Table 4.
Effect on laboratory parameters of Garbhini Pandu in Group B (n=9)
Comparative effect of therapies
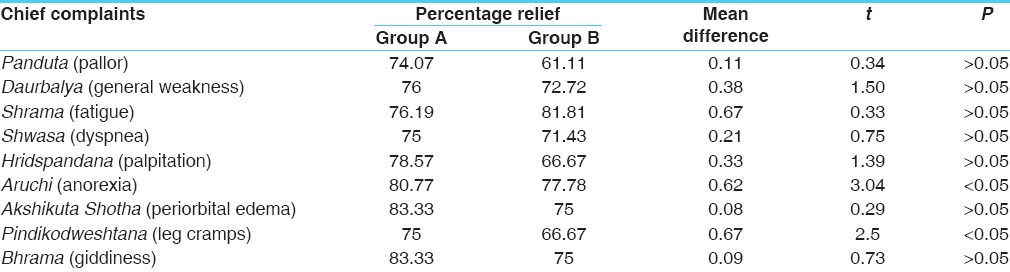
On subjective parameters
On comparing Group A and B statistically significant (P < 0.05) difference was found on Aruchi and Pindikodweshtana. It shows that on relieving Aruchi and Pindikodweshtana, Group A is better than Group B and on the rest of other symptoms, both groups are equally effective [Table 5].
Table 5.
Comparative effect of Group A and Group B on chief complaints
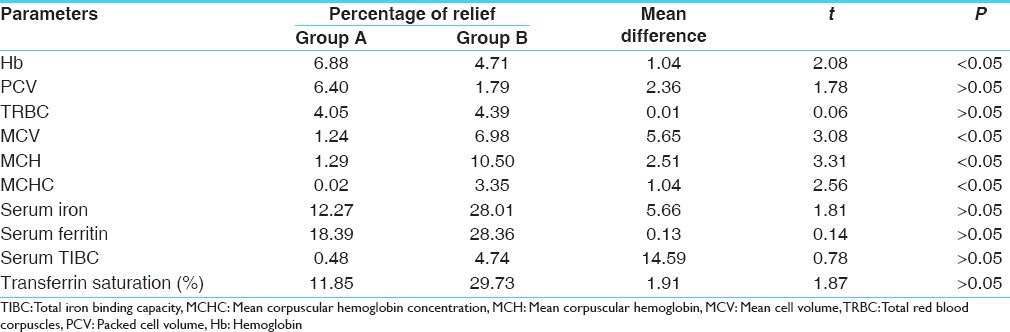
On objective parameters
On comparing Group A and B, statistically significant (P < 0.05) difference was noted in Hb%, MCV, MCH, and MCHC. It shows that Group A is better than Group B in relieving above parameters [Table 6].
Table 6.
Comparative effect of Group A and Group B on laboratory parameters
Overall effect of therapy
None of the patients showed complete remission or marked improvement in any of the groups. In Group A, 46.67% patients had moderate improvement while 44.44% patients had moderate improvement in Group B. Mild improvement was found in 40% patients in Group A while 33.33% patients in Group B. In Group A, 13.33% patients and 22.22% patients in Group B showed no improvement [Figure 1].
Figure 1.
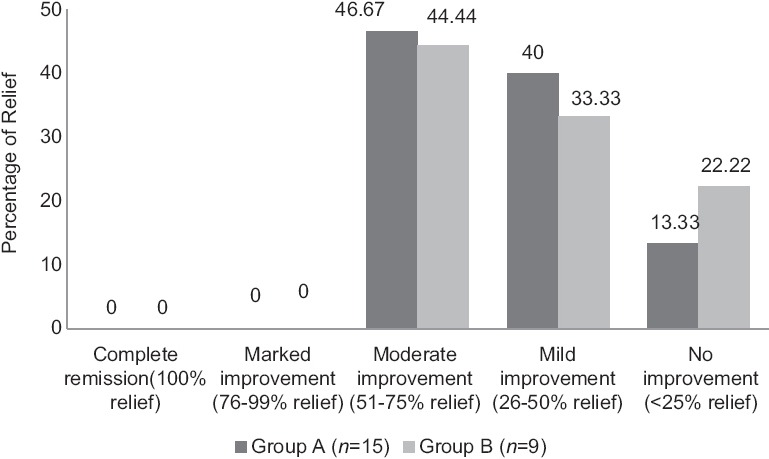
Overall effect of therapies
Discussion
Garbhini Pandu (anemia in pregnancy) is not a Vyadhi; it is described as a complication of Garbha. In pregnant woman, Rasa Nadi is compressed by the growing fetus, due to which Rasa does not flow freely in to the body resulting in Pandu. After 3 months of pregnancy, due to Dauhridavastha, if Garbhini is taking excessive Amla (sour) Lavana (salty) and Katu (pungent) Rasa (taste) or indulging in Vishamashana (improper diet), Diwaswapa (day time sleep), Vegavidharana, etc., and/or suffers from Manasika Bhava (psychological factors) it may cause Garbhini Pandu.
In the present study, majority of patients (59.26%) were having vegetarian diet. Iron supplied from vegetarian diet is mainly nonheam iron and its bioavailability is only about 1–10%. Thus, vegetarians are more prone for IDA. Most of the patients were habituated for consumption of excessive Lavana Rasa (92.59%) and Guru (heavy) Ahara (66.67), which hampers the proper Rasa Dhatu formation and leads to Ama production. It is the foremost step in the development of Pandu. 88.89% were habituated to tea. Tannins in tea can cause iron absorption to drop by 60%.[7] All patients were suffering from Chinta and had habit of Diwaswapa. Chronicity of the Chinta weakens digestive power and that ultimately is responsible for vitiation of Rasavaha Srotas resulting in Aruchi, Angamarda etc., symptoms.[8] Diwaswapa has been known to vitiate all three Doshas as per Sushruta[9] and especially Kapha and Pitta as per Acharya Charaka[10] which then pin down the normal functioning of Agni. Majority of the patients 64.86% were multigravida, and 48.65% were parous. Repeated pregnancies and excessive blood loss during deliveries predispose for Anemia.[11]
Punarnava Mandura provided a significant improvement on all subjective parameters of Garbhini Pandu, due to its Pitta-Kapha Shamaka, Pandughna, Rasayana (rejuvinative), Deepana-Pachana (digestive), Raktavardhaka, and Anulomana (laxative) properties which leads to the correction of metabolism, increase iron absorption, and improves blood formation. Dhatri Lauha provided relief on subjective parameters and serum iron, serum ferritin, serum TIBC, and transferrin saturation due to its Pandughna, Prinana, Rakta Prasadana properties as well as antioxidant, immunomodulator, hepatoprotective, and hematinic properties, which increase Dhatu Poshana as well as Iron absorption. There was decrease in hematological parameters, may be due to lack of Ushna Veerya Dravyas in Dhatri Lauha, hence it did not corrected the Bhutagni (enzymes responsible for metabolism).
Probable mode of action of Punarnava Mandura in Garbhini Pandu
Contents of Punarnava Mandura are Kashaya (astringent), Laghu (light), Ruksha (dry), Shita (cold), Katu, and Pittakapha Shamaka. Punarnava is Anulomana, Mutrala (diuretic) and has been proved as hepatoprotective and antioxidant.[12,13,14,15] Mandura Bhasma possesses significant hematinic and cytoprotective, hepatoprotective activity.[16,17] Triphala, an Ayurvedic Rasayana, is antianemic and anti-oxidant. It contains Amalaki (Emblica officinalis Gaertn.) that is Rochana, Deepana, and Anulomana having a role in the digestion, absorption, and motility of digestive materials in the gut. As it is Hridya, Yakrututtejaka, and Shonita Sthapana, it has a direct action on Rasavaha and Raktavaha Srotas. It has been considered as a potent Rasayana enhancing the essence of all the Dhatus. Amalaki is a rich source of iron and Vitamin C. Trikatu is a known bioavailability enhancer.[18] Gomutra (cow urine) is an important ingredient of the drug and proved for its antimicrobial, antioxidant,[19] and antianemic due to its erythropoietin stimulating factor.[20] Anupana of buttermilk is digestive due to the presence of probiotics,[21] Pandughna,[22] and rich source of minerals and Vitamin B12.[23] The significant results obtained in the subjective parameters, as well as laboratory parameters, could be attributed to these properties.
Probable mode of action of Dhatri Lauha in Garbhini Pandu
Contents of Dhatri Lauha are Kashaya, Ruksha, Sheeta, and Tridoshashamaka specially Kapha-Pitta Shamaka. Dhatri is Rasayana and Yakrututtejaka and has been proved as antioxidant, immunomodulator, and hepatoprotective.[24] Yashtimadhu (Glycyrrhiza glabra L.) is Rasayana and active bio-availability enhancer.[25] Amruta (Tinospora cordifolia [Willd.] Miers.) is also Rasayana and hepatoprotective. All these drugs have action on Rasavaha and Raktavaha Srotas and enhance the essence of all the Dhatus. Lauha Bhasma possesses a significant hematinic and Deepana-Pachana property. Amalaki[26] and Amruta[27] is a rich source of Vitamin C which enhances the iron absorption.
Thus, cumulative effects of all the drugs lead to the correction of metabolism, increase iron absorption, improved blood formation, and improves the subjective and objective parameters of Garbhini Pandu.
No adverse effects were reported during the entire period of the study.
Conclusion
Punarnava Mandura provided better results against the symptoms of Garbhini Pandu. Dhatri Lauha showed better results on subjective parameters only. With increased dose, both drugs were able to break the disease pathogenesis. Hence, better results were found. Punarnava Mandura and Dhatri Lauha are effective and safe at increased dose on Garbhini Pandu, but Punarnava Mandura is comparatively better in Garbhini Pandu.
Financial support and sponsorship
IPGT and RA, Gujarat Ayurved University, Jamnagar, Gujarat, India.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors are thankful to the staff of Pathology and Biochemistry laboratories, Hospital staff, especially Department of SRPT for their help, Pharmacy of Gujarat Ayurved University for in time preparation of drugs and support of patients for participating in this study.
References
- 1.DeMaeyer E, Adiels-Tegman M. The prevalence of anaemia in the world. World Health Stat Q. 1985;38:302–16. [PubMed] [Google Scholar]
- 2.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 3.Sharma H. Commentator. Kashyapa Samhita of Kashyapa, Khila Sthana. Reprinted ed. Ch. 9, Ver. 46-49. Varanasi: Chaukhambha Sanskrit Sansthan; 2009. p. 289. [Google Scholar]
- 4.Tripathi HP, editor. Harita Samhita of Harita, Trutiya Sthana. 1st ed. Ch. 51, Ver. 1. Varanasi: Chaukhambha Krishnadas Academy; 2005. p. 456. [Google Scholar]
- 5.Rupapara AV, Donga SB, Dei L. A comparative study on the effect of Pandughnivati and Dhatrilauhavati in the management of Garbhinipandu (Iron Deficiency Anemia) Ayu. 2013;34:276–80. doi: 10.4103/0974-8520.123120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.List of Drugs Being Provided in ASHA Kit – Government of India. [Last updated on 2014 Aug 21; Last cited on 2015 March 04]. Available from: http://www.india.gov.in .
- 7.Hargreaves C. Is your daily cuppa leaving you lower in iron? Camberley, Surrey GU15 3YL: Nutritionist Resource. 2013. [Last cited on 2015 Mar 15]. Available from: http://www.nutritionist-resource.org.uk/nutritionist-articles/is-your-daily-cuppaleaving-you-lower-in-iron .
- 8.Acharya JT, editor. Charaka Samhita of Agnivesha, Vimana Sthana. Reprint Edition. Ch. 5, Ver. 12. Varanasi: Chaukhamba Sanskrit Sansthana Varanasi; 2013. p. 251. [Google Scholar]
- 9.Shastri AD, editor. Sushruta Samhita of Sushruta, Sharira Sthana. 2nd ed. Ch. 4, Ver. 37. Varanasi: Chaukhamba Sanskrit Sansthana; 2010. p. 45. [Google Scholar]
- 10.Acharya JT, editor. Charaka Samhita of Agnivesha, Sutra Sthana. Reprint Edition. Ch. 21, Ver. 44. Varanasi: Chaukhamba Sanskrit Sansthana Varanasi; 2013. p. 118. [Google Scholar]
- 11.Datta DC. Text Book of Obstetrics. 7th ed. Culcutta: New Central Book Agency; 2011. p. 262. [Google Scholar]
- 12.Chandan BK, Sharma AK, Anand KK. Boerhaavia diffusa: A study of its hepatoprotective activity. J Ethnopharmacol. 1991;31:299–307. doi: 10.1016/0378-8741(91)90015-6. [DOI] [PubMed] [Google Scholar]
- 13.Mungantiwar AA, Nair AM, Shinde UA, Dikshit VJ, Saraf MN, Thakur VS, et al. Studies on the immunomodulatory effects of Boerhaavia diffusa alkaloidal fraction. J Ethnopharmacol. 1999;65:125–31. doi: 10.1016/s0378-8741(98)00153-6. [DOI] [PubMed] [Google Scholar]
- 14.Rawat AK, Mehrotra S, Tripathi SC, Shome U. Hepatoprotective activity of Boerhaavia diffusa L. roots- A popular Indian ethnomedicine. J Ethnopharmacol. 1997;56:61–6. doi: 10.1016/s0378-8741(96)01507-3. [DOI] [PubMed] [Google Scholar]
- 15.Agrawal B, Das S, Pandey A. Boerhaavia diffusa Linn: A review on its phytochemical and pharmacological profile. Asian J Appl Sci. 2011;4:663–84. [Google Scholar]
- 16.Kanase B, Patil S, Thorat B. Curative effects of mandur bhasma on liver and kidney of albino rats after induction of acute hepatitis by CCl4. Indian J Exp Boil. 1997;35:754–64. [PubMed] [Google Scholar]
- 17.Sarkar PK, Prajapati PK, Chaudhary AK, Shukla VJ, Ravishankar B. Haematinic evaluation of Lauha bhasma and Mandura bhasma on HgCl 2 -Induced anemia in rats. Indian J Pharm Sci. 2007;69:791. [Google Scholar]
- 18.Kesarwani K, Gupta R. Bioavailability enhancers of herbal origin: An overview. Asian Pac J Trop Biomed. 2013;3(4):253–66. doi: 10.1016/S2221-1691(13)60060-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jarald E, Edwin S, Tiwari V, Garg R, Toppo E. Antioxidant and Antimicrobial Activities of Cow Urine. Global Journal of Pharmacology. 2008;2:20–2. [Google Scholar]
- 20.Randhawa GK. Cow urine distillate as bioenhancer. J Ayurveda Integr Med. 2010;1:240–41. doi: 10.4103/0975-9476.74089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. [Last cited on 2015 Mar 15]. Available from: http://www.Buttermilk%20Nutrition%20Facts%20%20Calories%20in%20Buttermilk%20Health%20Benefits.html .
- 22.Gupta AD, editor. Ashtanga Samgraha of Vagbhatta, Sutra Sthana. Reprinted ed. Ch. 6, Ver. 69. Varanasi: Chaukhamba Prakashana; 2005. p. 54. [Google Scholar]
- 23. [Last cited on 2016 Mar 15]. Available from: http://www.benefits-of-buttermilk-benefits-of.html .
- 24.Bhaskarmurthy DH, Velusami CC, Dethe S, Mundkinajeddu D, Pandre MK, Balachandran J, et al. Hepatoprotective and antioxidant activity of standardized herbal extracts. Pharmacogn Mag. 2012;8:116–23. doi: 10.4103/0973-1296.96553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drabu S, Khatri S, Babu S, Lohani P. Use of herbal bioenhancers to increase the bioavailability of drugs. Res J Pharm Biol Chem Sci. 2011;2:107–1. [Google Scholar]
- 26.Yadav V, Duvey B, Sharma S, Devi B. Amla (Emblica officinalis) - Medicinal food and pharmacological activity. Int J Pharm Chem Sci. 2014;3:616–9. [Google Scholar]
- 27.Deshmukh A, Usha D. In vitro Effect of Tinospora cordifolia on PMN Function Update Ayurveda-94, Bombay, India; 24th-26th February. 1994:63. [Google Scholar]


