Abstract
We present a case of a 17-year-old football player who had previously received multiple facet joint injections for presumed secondary osteoarthritis. 99mTc-methylene diphosphonate single-photon emission computed tomography/computed tomography imaging of the cervical spine demonstrated focal increased radiopharmaceutical activity in the right C2 lamina, which was associated with an osteolytic lesion with a central irregular sclerotic nidus. Surgical pathology confirmed an osteoid osteoma.
Keywords: Accuracy, computed tomography, osteoid, osteoma, single-photon emission computed tomography
INTRODUCTION
Hybrid single-photon emission computed tomography/computed tomography (SPECT/CT) offers the diagnostic advantage of combining both anatomical and functional information in a single imaging session. 99mTc-methylene diphosphonate (99mTc-MDP) SPECT/CT scintigraphy has previously demonstrated superior accuracy in diagnosing osteoid osteoma (OO) compared to three-phase bone scintigraphy, which lacks specificity.[1] CT alone has also shown inferior diagnostic accuracy compared to SPECT/CT.[1] The following case demonstrates the utility of SPECT/CT in the diagnosis of OO in a young athlete participating in contact sports.
CASE REPORT
A 17-year-old male football player presented with 2 years of right-sided upper cervical pain. The pain was constant, radiating, throbbing, worse at night, and initially relieved with nonsteroidal anti-inflammatory drugs (NSAIDs). The patient had undergone a partial work-up at an outside institution and was treated symptomatically for presumed right-sided C1–C2 facet synovitis including physical therapy, chiropractic manipulation, muscle relaxants, and multiple occipital nerve and facet joint injections, all of which provided only temporary relief.
Physical examination revealed mild tenderness to palpation of the right upper cervical region. Neurological examination was negative.
Initial cervical radiographs were normal and without evidence of facet joint osteoarthritis. 99mTc-MDP planar [Figure 1] and SPECT/CT [Figures 2 and 3] scintigraphy of the cervical spine were then performed and demonstrated focal increased radiopharmaceutical accumulation associated with a lucency within the right C2 lamina, consistent with OO.
Figure 1.
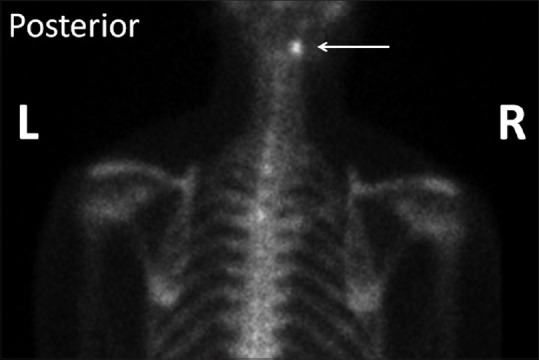
Posterior planar 99mTc-methylene diphosphonate scintigraphy demonstrates increased uptake at the nidus (arrow)
Figure 2.
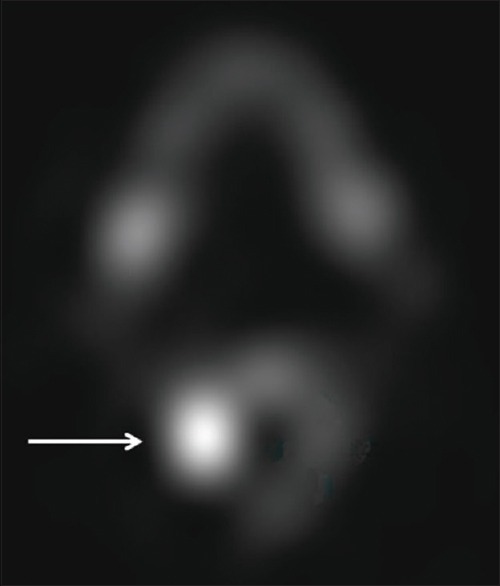
Axial 99mTc-methylene diphosphonate single-photon emission computed tomography image demonstrates focal increased activity (arrow) at the nidus
Figure 3.
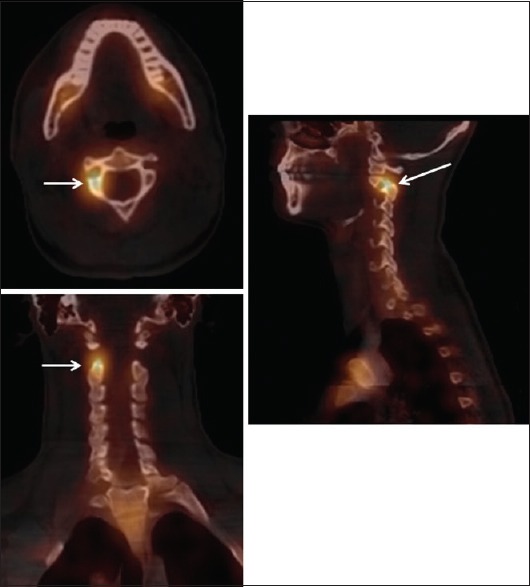
Axial, coronal, and sagittal 99mTc-methylene diphosphonate single-photon emission computed tomography/computed tomography fusion images demonstrate focal increased activity (arrows) within the right C2 lamina
Diagnostic CT of the cervical spine [Figure 4] confirmed an osteolytic lesion with a central irregular sclerotic nidus within the right C2 lamina. The facet joints, central canal, and neural foramina were unremarkable. Imaging findings were consistent with OO.
Figure 4.
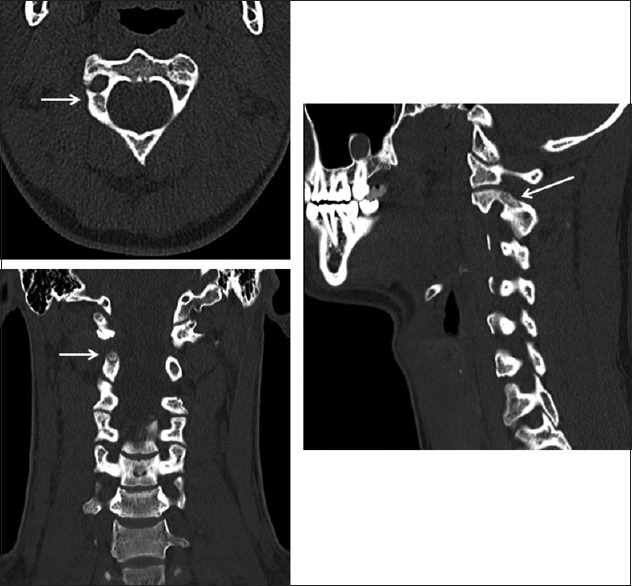
Axial, coronal, and sagittal unenhanced computed tomography images in bone windows demonstrate a predominantly radiolucent nidus (arrows) with internal mineralization and subtle surrounding reactive sclerosis
Neurosurgery recommended intra-lesional resection and curettage as opposed to radiofrequency ablation due to anatomic location. The patient underwent an uncomplicated image-guided partial hemi-laminectomy at C2. Surgical pathology evaluated the intra-laminar lesion and confirmed OO [Figure 5]. The patient recovered uneventfully with only mild postoperative pain.
Figure 5.
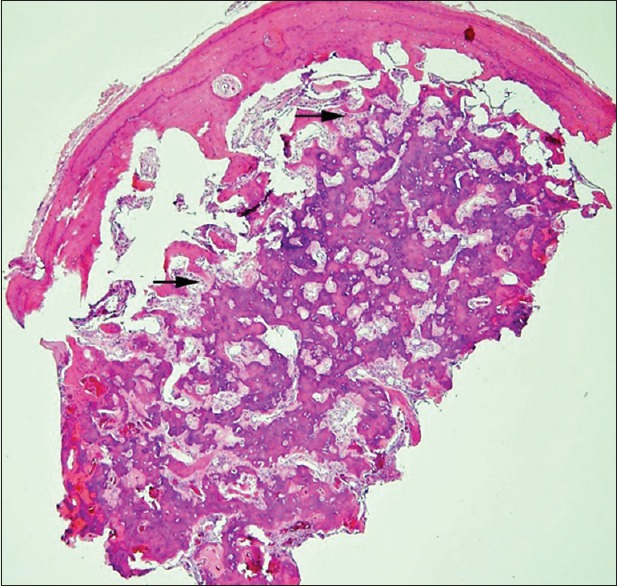
Photomicrograph of the osteoid osteoma, characterized by haphazardly anastomosing bony trabeculae with a sclerotic peripheral rim. The trabeculae are lined by a single layer of osteoblasts (arrows) (H and E)
Follow-up imaging demonstrated no definite recurrence of OO; however, there was reactive bone formation adjacent to the surgical site.
DISCUSSION
OOs are benign osteoblastic neoplasms primarily affecting children and adolescents.[1] OO comprise 10–12% of all benign osseous neoplasms and 2–3% of all primary bone tumors.[2] Clinically, OO present with intermittent pain worse at night and relieved by aspirin/NSAIDs. These tumors rarely exceed 1.5 cm and are pathologically characterized by an osteoid rich nidus surrounded by vascular connective tissue.[3]
Diagnostic imaging modalities include radiography, scintigraphy, CT, and magnetic resonance imaging. Three-phase scintigraphy has excellent sensitivity but lacks specificity.[1] Radiography and CT can accurately diagnose OO when the typical appearance of a radiolucent nidus surrounded by reactive sclerosis is present. However, the diagnosis can be equivocal when OO occur in atypical locations or have a nonspecific or misleading appearance on conventional modalities.[3] Hybrid SPECT/CT for bone imaging combines functional and anatomical information, which significantly improve specificity. Furthermore, the diagnostic accuracy of SPECT/CT in the detection of OO has been shown to be superior to planar scintigraphy or CT alone.[1]
This case demonstrates the value of SPECT/CT in diagnosing OO in an athlete participating in contact sports. The patient underwent a partial work-up at an outside institution and was treated symptomatically for presumed facet synovitis. While initial radiography failed to detect the lesion, 99mTc-MDP SPECT/CT scintigraphy accurately diagnosed OO and re-directed treatment to curative surgery instead of futile palliative therapies.
Hybrid SPECT/CT has proven to increase sensitivity and specificity of 99mTc-MDP scintigraphy in both benign and malignant bone disease.[4] SPECT/CT improves diagnostic accuracy in the detection of OO and can be utilized when other imaging modalities are equivocal.[1] Furthermore, clinicians should consider OO in the differential diagnosis even in patients with more likely diagnoses or those presenting with atypical signs, symptoms, or histories.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sharma P, Mukherjee A, Karunanithi S, Nadarajah J, Gamanagatti S, Khan SA, et al. 99m Tc-Methylene diphosphonate SPECT/CT as the one-stop imaging modality for the diagnosis of osteoid osteoma. Nucl Med Commun. 2014;35:876–83. doi: 10.1097/MNM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 2.Iyer RS, Chapman T, Chew FS. Pediatric bone imaging: Diagnostic imaging of osteoid osteoma. AJR Am J Roentgenol. 2012;198:1039–52. doi: 10.2214/AJR.10.7313. [DOI] [PubMed] [Google Scholar]
- 3.Laurence N, Epelman M, Markowitz RI, Jaimes C, Jaramillo D, Chauvin NA. Osteoid osteomas: A pain in the night diagnosis. Pediatr Radiol. 2012;42:1490–501. doi: 10.1007/s00247-012-2495-y. [DOI] [PubMed] [Google Scholar]
- 4.Horger M, Bares R. The role of single-photon emission computed tomography/computed tomography in benign and malignant bone disease. Semin Nucl Med. 2006;36:286–94. doi: 10.1053/j.semnuclmed.2006.05.001. [DOI] [PubMed] [Google Scholar]


