Abstract
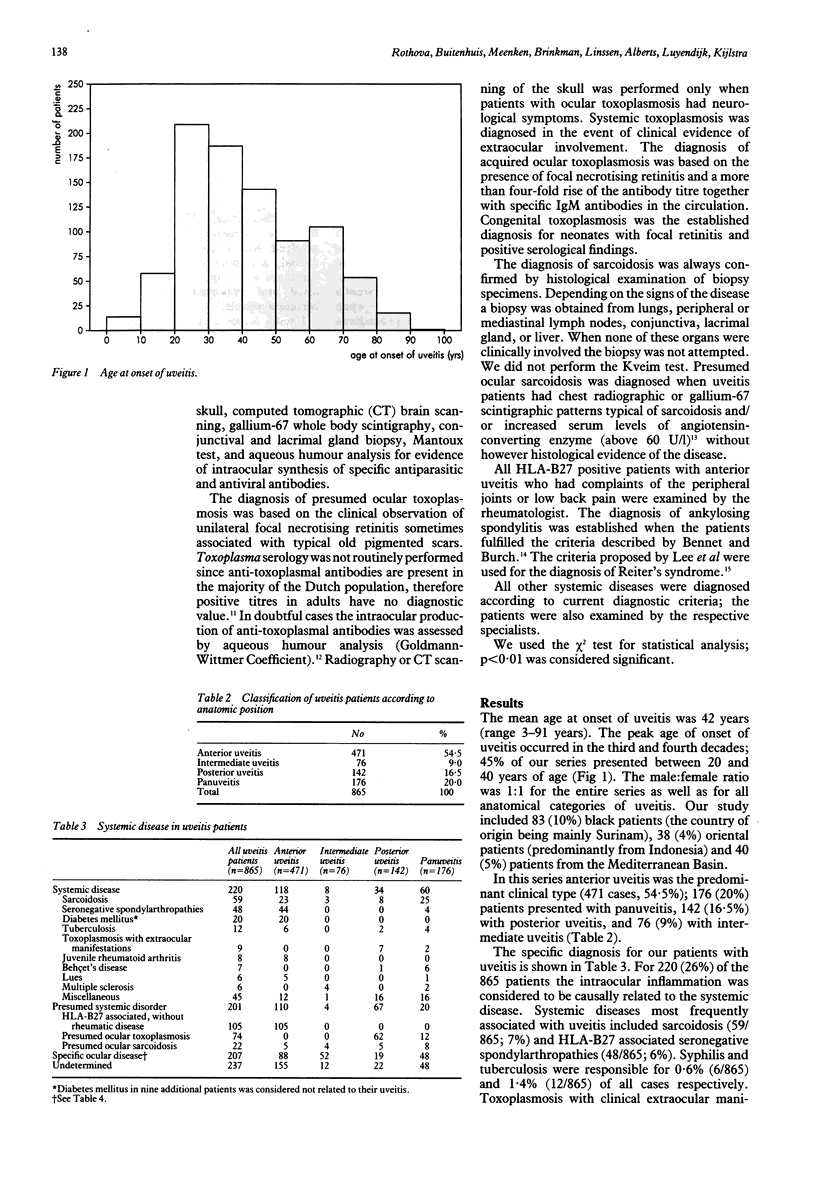
A prospective study was conducted of 865 patients with uveitis to determine the frequency of associated systemic diseases and to assess the value of limited laboratory screening of these patients. All patients underwent a standard diagnostic protocol followed--when indicated--by special tests and procedures performed in order of likelihood ('tailored approach'). For 628 patients (73%) a specific diagnosis was established based on history, ophthalmologic examination, and laboratory and radiographic studies. A definite association with systemic disease was determined for 220 patients (26%). A relationship with a subclinical systemic disorder could be presumed in 201 cases (23%) and a well-established clinical uveitis entity without a recognisable systemic disorder was present in 207 cases (24%). For 237 patients (27%) a diagnosis could not be determined. The most frequently observed systemic diseases were sarcoidosis (7%) and HLA-B27-associated seronegative spondylarthropathies (6%). Presumed or definite toxoplasmosis was encountered in 10% of cases. HLA-B27-associated acute anterior uveitis was the most common clinical entity (17%). In the majority of cases the presence of a systemic disease was not suspected prior to eye involvement and was only recognised after the subsequent diagnostic procedures.
Full text
PDF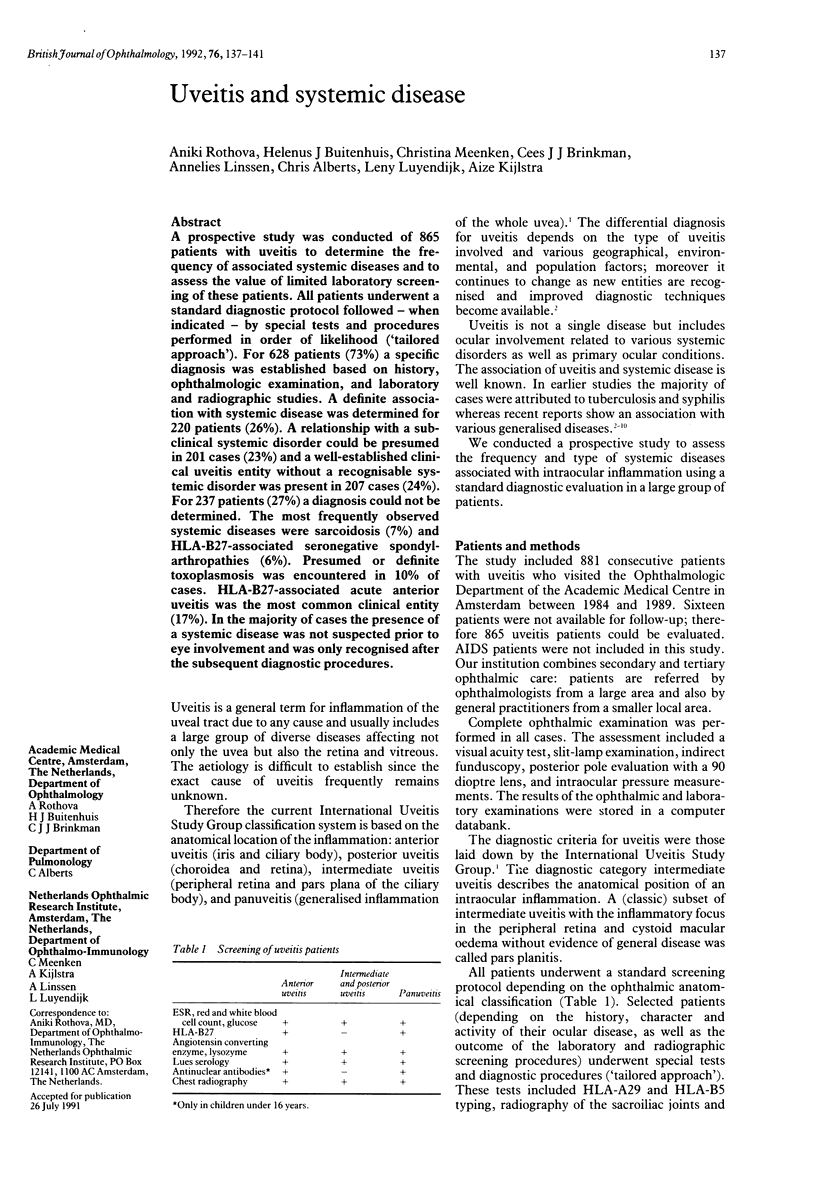


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baarsma G. S., La Hey E., Glasius E., de Vries J., Kijlstra A. The predictive value of serum angiotensin converting enzyme and lysozyme levels in the diagnosis of ocular sarcoidosis. Am J Ophthalmol. 1987 Sep 15;104(3):211–217. doi: 10.1016/0002-9394(87)90406-5. [DOI] [PubMed] [Google Scholar]
- Bloch-Michel E., Nussenblatt R. B. International Uveitis Study Group recommendations for the evaluation of intraocular inflammatory disease. Am J Ophthalmol. 1987 Feb 15;103(2):234–235. doi: 10.1016/s0002-9394(14)74235-7. [DOI] [PubMed] [Google Scholar]
- Chung Y. M., Yeh T. S., Liu J. H. Endogenous uveitis in Chinese--an analysis of 240 cases in a uveitis clinic. Jpn J Ophthalmol. 1988;32(1):64–69. [PubMed] [Google Scholar]
- Henderly D. E., Genstler A. J., Smith R. E., Rao N. A. Changing patterns of uveitis. Am J Ophthalmol. 1987 Feb 15;103(2):131–136. doi: 10.1016/s0002-9394(14)74217-5. [DOI] [PubMed] [Google Scholar]
- James D. G., Friedmann A. I., Graham E. Uveitis. A series of 368 patients. Trans Ophthalmol Soc U K. 1976 Apr;96(1):108–112. [PubMed] [Google Scholar]
- Kijlstra A., Luyendijk L., Baarsma G. S., Rothova A., Schweitzer C. M., Timmerman Z., de Vries J., Breebaart A. C. Aqueous humor analysis as a diagnostic tool in toxoplasma uveitis. Int Ophthalmol. 1989 Dec;13(6):383–386. doi: 10.1007/BF02306485. [DOI] [PubMed] [Google Scholar]
- Kijlstra A., Rothova A., Baarsma G. S., Zaal M. J., Fortuin M. E., Schweitzer C., Glasius E., de Jong P. T. Computer registration of uveitis patients. Doc Ophthalmol. 1987 Sep-Oct;67(1-2):139–143. doi: 10.1007/BF00142708. [DOI] [PubMed] [Google Scholar]
- Lee D. A., Barker S. M., Su W. P., Allen G. L., Liesegang T. J., Ilstrup D. M. The clinical diagnosis of Reiter's syndrome. Ophthalmic and nonophthalmic aspects. Ophthalmology. 1986 Mar;93(3):350–356. doi: 10.1016/s0161-6420(86)33747-3. [DOI] [PubMed] [Google Scholar]
- Lesser R. L., Kornmehl E. W., Pachner A. R., Kattah J., Hedges T. R., 3rd, Newman N. M., Ecker P. A., Glassman M. I. Neuro-ophthalmologic manifestations of Lyme disease. Ophthalmology. 1990 Jun;97(6):699–706. doi: 10.1016/s0161-6420(90)32519-8. [DOI] [PubMed] [Google Scholar]
- Miettinen R. Incidence of uveitis in Northern Finland. Acta Ophthalmol (Copenh) 1977 Apr;55(2):252–260. doi: 10.1111/j.1755-3768.1977.tb01306.x. [DOI] [PubMed] [Google Scholar]
- Perkins E. S., Folk J. Uveitis in London and Iowa. Ophthalmologica. 1984;189(1-2):36–40. doi: 10.1159/000309382. [DOI] [PubMed] [Google Scholar]
- Rosenbaum J. T. Uveitis. An internist's view. Arch Intern Med. 1989 May;149(5):1173–1176. doi: 10.1001/archinte.149.5.1173. [DOI] [PubMed] [Google Scholar]
- Rothova A., Meenken C., Michels R. P., Kijlstra A. Uveitis and diabetes mellitus. Am J Ophthalmol. 1988 Jul 15;106(1):17–20. doi: 10.1016/s0002-9394(14)76381-0. [DOI] [PubMed] [Google Scholar]
- Rothova A., van Knapen F., Baarsma G. S., Kruit P. J., Loewer-Sieger D. H., Kijlstra A. Serology in ocular toxoplasmosis. Br J Ophthalmol. 1986 Aug;70(8):615–622. doi: 10.1136/bjo.70.8.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SMITH C., ASHTON N. Studies on the aetiological problem of uveitis. Br J Ophthalmol. 1955 Sep;39(9):545–556. doi: 10.1136/bjo.39.9.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- STANWORTH A., MCINTYRE H. Aetiology of uveitis. Br J Ophthalmol. 1957 Jul;41(7):385–420. doi: 10.1136/bjo.41.7.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakefield D., Dunlop I., McCluskey P. J., Penny R. Uveitis: aetiology and disease associations in an Australian population. Aust N Z J Ophthalmol. 1986 Aug;14(3):181–187. doi: 10.1111/j.1442-9071.1986.tb00034.x. [DOI] [PubMed] [Google Scholar]
- Winward K. E., Smith J. L., Culbertson W. W., Paris-Hamelin A. Ocular Lyme borreliosis. Am J Ophthalmol. 1989 Dec 15;108(6):651–657. doi: 10.1016/0002-9394(89)90856-8. [DOI] [PubMed] [Google Scholar]



