Abstract
Research and policy initiatives are increasingly focused on the role of neighborhood food environment in children’s diet and obesity. However, existing evidence relies on observational data that is limited by neighborhood selection bias. The Military Teenagers’ Environments, Exercise, and Nutrition Study (M-TEENS) leverages the quasi-random variation in neighborhood environment generated by military personnel’s assignment to installations to examine whether neighborhood food environments are associated with children’s dietary behaviors and BMI. Our results suggest that neither the actual nor the perceived availability of particular food outlets in the neighborhood is associated with children’s diet or BMI. The availability of supermarkets and convenience stores in the neighborhood was not associated with where families shop for food or children’s dietary behaviors. Further, the type of store that families shop at was not associated with the healthiness of food available at home. Similarly, availability of fast food and restaurants was unrelated to children’s dietary behaviors or how often children eat fast food or restaurant meals. However, the healthiness of food available at home was associated with healthy dietary behaviors while eating at fast food outlets and restaurants were associated with unhealthy dietary behaviors in children. Further, parental supervision, including limits on snack foods and meals eaten as a family, was associated with dietary behaviors. These findings suggest that focusing only on the neighborhood food environment may ignore important factors that influence children’s outcomes. Future research should also consider how families make decisions about what foods to purchase, where to shop for foods and eating out, how closely to monitor their children’s food intake, and, ultimately how these decisions collectively impact children’s outcomes.
Keywords: USA, Body mass index, Childhood obesity, Food environments, Diet
Introduction
Childhood obesity remains a leading health concern with 34.5% of children aged 12–19 years overweight or obese and 20.5% obese in the U.S. in 2012(Ogden, Carroll, Kit, & Flegal, 2014). Obesity results when energy consumption exceeds energy expenditure, but the factors that influence this energy imbalance are complex and still not well understood. Given the high and increasing rates of child obesity over the past three decades (Fryar, Carroll, & Ogden, 2012), there is growing interest in population-level prevention and the role of social and environmental contexts (N. Larson & Story, 2009) (Carroll-Scott et al., 2013; Ding, Sallis, Kerr, Lee, & Rosenberg, 2011). One potential contextual driver that has received substantial attention recently is the role of neighborhood food environments.
Several federal and local policy initiatives are attempting to address the role of neighborhood food environment by improving access to healthy foods and restricting access to unhealthy foods. For example, the $400 million Healthy Food Financing Initiative, the Pennsylvania Fresh Food Financing Initiative, and New York City’s Food Retail Expansion to Support Health include funding to encourage the introduction of supermarkets in underserved areas. Another approach focuses on regulating the opening of new fast food outlets through zoning laws (Sturm & Wu, 2012). The premise behind these initiatives is that greater access to supermarkets and less access to fast food outlets will translate into improvements in diets and health.
Despite the growing attention focused on the role of the neighborhood food environment, our understanding of the empirical relationship between the neighborhood food environment and children’s diet and obesity is limited and primarily based on cross-sectional studies (N. Larson & Story, 2009). The limitations of the existing research include a focus on a single food industry (e.g., fast food or supermarkets)(Lee, 2012), use of only objective or perceived measures of the environment (Caspi, Sorensen, Subramanian, & Kawachi, 2012), and lack of insight into the mechanisms underlying findings (Casagrande, Whitt-Glover, Lancaster, Odoms-Young, & Gary, 2009; Odoms-Young, Zenk, & Mason, 2009). Moreover, cross-sectional studies may produce biased estimates if families self-select into neighborhoods based on their preferences for certain types of foods and other health-related behaviors that influence the risk of obesity. Therefore, one cannot assume that neighborhoods are randomly or exogenously assigned and residential selection may confound estimates of how those neighborhood characteristics affect behaviors and health. Results from a limited number of longitudinal studies provide little evidence of a significant relationship between the neighborhood food environment and children’s BMI and obesity. One longitudinal study that assessed outlet availability with two different measures at the county-level found a significant association between increased supermarket outlets per 10 square miles and lower childhood BMI but did not find any significant associations for supermarket outlets per 10,000 capita or for availability of other food outlets (L. M. Powell & Bao, 2009). Another longitudinal study concludes that differential exposure to food outlets (measured as density in their home census tract) does not explain weight gain in children followed from kindergarten through 5th grade (Lee, 2012).
This study uses data from the Military Teenagers Environments, Exercise, and Nutrition Study (M-TEENS) to first examine the association of the neighborhood food environment (both objective and perceived) with children’s dietary behaviors and BMI. An important advantage of studying children in military families is that the relocation of military personnel provides unique variation in their families’ neighborhood environments. These relocations assign military personnel to new installations based on military’s needs and are typically not influenced by family preferences (Lleras-Muney, 2010). Therefore, even cross-sectional data are valuable because the neighborhood food environment among these Army families is not subject to the same level of residential selection that undermines typical observational studies. Moreover, these environments on and around military installations are likely to vary considerably, in large part because of the significant variation in geographic location and size of the installations. Other contributions include examining the potential mechanisms through which neighborhood food environment might influence children’s diet/BMI to gain insight into the relationships between the neighborhood food environment, where families shop for food, the home food environment, how often families eat out, and children’s diet/BMI. Rather than focusing on just one aspect of the food environment like most previous papers, this study provides a more complete understanding of the neighborhood food environment using this rich set of data on where families purchase food, the home food environment, children’s consumption, and children’s and families’ covariates. In summary, periodic military relocations of these families combined with our rich set of data provide a unique and innovative opportunity to examine the associations and mechanisms between neighborhood food environments and children’s dietary behaviors and BMI.
Conceptual framework
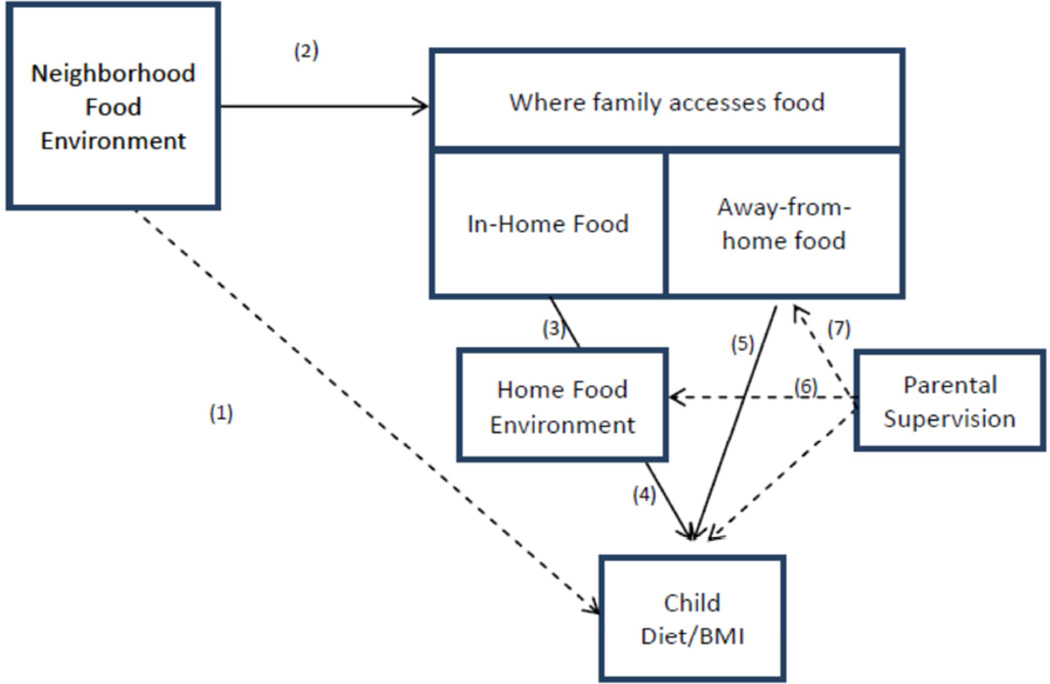
Figure 1 depicts our conceptual framework for understanding how neighborhood food environment can influence children’s diet and BMI (relationship 1). The availability of food outlets in the neighborhood is likely to influence children’s diet and consequently BMI through its influences on where the family purchases food for the home and how often the family eats away from home (relationship 2). Greater availability of supermarkets or convenience stores close to a family’s home might increase the likelihood that the family shops for food at those outlets. Similarly, greater availability of fast food outlets or restaurants might increase the frequency that the family eats outside the home. However, these mechanisms may be weaker among children because children have limited autonomy to purchase food and go out for food. Instead of shopping close to home, parents may shop at food outlets that are close to or en route to their work, children’s school or other routine activities. Furthermore, parents may influence the relationships between neighborhoods and children’s diet by making choices about what to purchase for the home, setting limits on what the child is allowed to eat and influencing what the child orders when eating out.
Figure 1.
Conceptual model of relationship between neighborhood food environment and child diet and BMI
With respect to foods eaten at home, it is hypothesized that greater access to supermarkets may support healthy home food environments (relationship 3) and consequently more healthful diets because they typically stock a wide range of healthy foods and make these items available at lower prices (N. I. Larson, Story, & Nelson, 2009). However, supermarkets may also stock a wider variety of junk foods than may be available in smaller stores because more total shelf space is devoted to junk foods (Farley et al., 2009). Greater access to convenience stores and fast food outlets may support unhealthy eating behaviors because they typically sell inexpensive energy-dense foods and soda (N. I. Larson, et al., 2009). However, the emerging empirical research from recent large and longitudinal studies suggests that the food outlets available in a family’s neighborhood are not associated with children’s diet, BMI and obesity (An & Sturm, 2012; Lee, 2012; L. M. Powell & Bao, 2009; Shier, An, & Sturm, 2012; Sturm & Datar, 2005).
In contrast to the research on the neighborhood food environment, there is mounting evidence that the home food environment – defined as the healthiness of foods available in the home– influences children’s diet and BMI (relationship 4) (Cullen et al., 2003; Ding et al., 2012; Ebbeling et al., 2006; Grimm, Harnack, & Story, 2004; Neumark-Sztainer, Wall, Perry, & Story, 2003; van Ansem, Schrijvers, Rodenburg, & van de Mheen, 2013). Access to fruits and vegetables (Cullen, et al., 2003; Ding, et al., 2012; Neumark-Sztainer, Wall, et al., 2003; van Ansem, et al., 2013), soft drinks (Ebbeling, et al., 2006; Grimm, et al., 2004), and snack foods at home have been associated with increased consumption among children. This suggests that readily available healthful foods are likely to enhance healthful dietary behaviors among families.
The empirical evidence is more consistent for away-from-home foods eaten at fast food outlets and full-service restaurants. Fast food consumption has been associated with more fat, sodium, sugars, and soda and less fruits, vegetables, fiber, and milk in child diets (relationship 5) (Bauer, Larson, Nelson, Story, & Neumark-Sztainer, 2009; Bowman, Gortmaker, Ebbeling, Pereira, & Ludwig, 2004; Lisa M Powell & Nguyen, 2013). Further, a study of children and adolescents finds that similar to fast food, full-service restaurant consumption is associated with increased daily total energy intake, sugar, fat, and soda (Lisa M Powell & Nguyen, 2013). Thus, away-from-home food consumption is associated with greater total calorie intake, which is particularly important because children are increasingly eating away-from-home foods (Poti & Popkin, 2011).
Finally, there may be certain types of parents with preferences for healthy family diets. A potential proxy for parental preferences for healthy diets is parental supervision of the children’s diets. Therefore, an important aspect of the framework is the role of parental supervision as a confounder to the influences of the home food environment and away-from-home food consumption (relationships 6 and 7). Parents with preferences for healthy diets (and parental supervision of diets) may have healthier home food environments, eat fewer meals out of the home, and have healthier child diet behaviors. Two measures of parent supervision are family meals and limits on child intake of junk foods. Parents who participate in family meals or set limits on children’s intake of junk foods may have healthier foods in the home or limit fast food intake and influence their children’s dietary choices overall. Frequency of family meals together has been positively associated with child consumption of fruits, vegetables, and grains, and less fried foods, soda, and fat (French, Story, Fulkerson, & Gerlach, 2003; Neumark-Sztainer, Hannan, Story, Croll, & Perry, 2003).
Empirical approach
The main objective of our study is to determine the association between the neighborhood food environment and children’s dietary behaviors, BMI, and overweight/obesity (relationship 1). We estimate this relationship using the multiple linear regression model in the equation below. The primary explanatory variable of interest is the neighborhood food environment (NFE).
The main coefficient of interest is β1, which captures the relationship between the neighborhood food environment and the child’s dietary behaviors, BMI and obesity (Y). The vector (X) includes contemporaneous child, family and contextual covariates that may influence diet and BMI. Standard errors are adjusted for clustering within installations. We examine this relationship using both objective and perceived measures of the neighborhood food environment separately.
An additional objective of the study is to unpack the potential mechanisms through which the neighborhood food environment might influence children’s diet/BMI as presented in the conceptual framework. We first examine how the neighborhood food environment is associated with where the family shops for or accesses food. For example, greater availability of certain types of food outlets in one’s neighborhood might increase the likelihood that the family shops or eats at those outlets. We test this hypothesis by estimating relationship (2) separately for food-at-home and away-from-home foods. For food-at-home, the dependent variable measures where the family primarily shops for grocery items. For away-from-home foods, the dependent variable measures the number of meals or snacks from fast food outlets and number of evenings the family eats at a restaurant or gets take out dinner per week.
For food-at-home, we then examine whether the family’s primary grocery food shopping source is associated with the family’s home food environment (relationship (3)). The home food environment measures the healthiness of food available in the home. We then examine how the home food environment is associated with children’s outcomes (relationship 4). Similarly, for away-from-home foods, we examine how the number of meals eaten at fast food outlets or restaurants influenced children’s outcomes (relationship (5)).
Finally, we examine how parental supervision influenced the relationship between the home food environment (relationship 6) and fast food/restaurant meals (relationship 7) on children’s outcomes.
Data
M-TEENS is a longitudinal study of families of Army-enlisted personnel located at 12 Army installations in the continental U.S. The 12 installations are distributed across all four Census regions: West (Joint Base Lewis-McChord, Fort Carson), Northeast (Fort Drum), South (Fort Bragg, Fort Benning, Fort Bliss, Fort Campbell, Fort Hood, Fort Polk, Fort Stewart) and Midwest (Fort Polk, Fort Riley, Fort Sill). Installations were selected to represent a majority of the Army active duty enlisted population with eligible children. Recruitment was conducted March to December 2013 via emails to the service members’ military email and mailings sent to their home address, which were obtained from the Defense Manpower Data Center. Due to concerns about outdated contact information of this mobile population and typically low response rates in this population (2014 Health Care Survey of DoD Beneficiaries; Tanielian T, Karney BR, Chandra A, & SO, 2014), 8545 families were initially contacted, of which 2106 completed the eligibility screener. Families were eligible to participate if: 1) the Army-enlisted parent intended to stay in the Army for the coming year; 2) the 12- or 13-year old child resided with the enlisted parent at least half-time; and 3) the child was enrolled in public or Department of Defense Education Activity school. Of those screened, 1794 were eligible and 1188 consented to participate. This study uses data from the baseline surveys conducted in 2013.
The eligible 12- or 13-year old child and a parent completed online or paper surveys. The child survey focused on the child’s dietary behaviors, food purchases at school, and physical activity. The parent survey focused on the family’s background, the residential neighborhood, the home environment, and the family’s dietary and exercise behaviors. A total of 1052 parents and 933 children completed the surveys with completed surveys for a total of 903 child/parent pairs. The child’s height, weight, and waist circumference were also measured by trained field staff during visits to the 12 installations.
The study leverages unique quasi-random variation in neighborhood environments generated by the assignment of military personnel to installations to serve the military’s needs. This assignment process renders even cross-sectional data valuable because the distribution of families across installations at any given point in time is potentially exogenous to the study outcomes.
The study was approved by the Institutional Review Boards at [Excluded for review] and [Excluded for review] and by the Army’s Human Research Protection Office.
Measures
BMI and overweight/obesity
BMI and overweight/obesity are primary outcome measures. One important advantage of the M-TEENS is that height and weight measurements were not only reported by parents and children, but were also collected by trained study staff for a subsample of children (N=522) who were able to attend the onsite installation visits. Given that only 58% of the sample had height and weight measurements, we used these observations as a validation sample to estimate “correction models” that are a standard approach in the literature (Cawley, 2002, 2004). For boys and girls separately, the measured height (weight) was regressed on the corresponding self-reported and parent-reported height (weight), quadratic term of height (weight), age in months, and indicators of race-ethnicity. The regression estimates were used to predict corrected children’s height (weight) in the overall sample. These models yielded very high model-fit (Adjusted R2 =77.4 for height, 88.3 for weight) and low classification error for obesity (sensitivity, or true positive: 77–85%, specificity, or true negative: 96–99%). Detailed findings from these models are reported elsewhere (Excluded for review). There were no statistically significant differences between the measured and unmeasured children in terms of their self-reported BMI or overweight/obese status or in family background characteristics, with one exception - those who were measured were more likely to live on-installation, which is not surprising given that the measurement visits were hosted at an installation youth center. Using the predicted height and weight, we constructed age- and gender-specific BMI z-score and BMI percentile based on the 2000 BMI-for-age and gender growth charts issued by the Centers for Disease Control and Prevention. A child was classified as obese or overweight if the BMI percentile was greater than or equal to 85.
Dietary behaviors
We also examine outcomes measuring children’s dietary behaviors. These were collected via a modified version of the Beverage and Snack Questionnaire (Neuhouser, Lilley, Lund, & Johnson, 2009) which asks about frequency of consumption of fruits, vegetables, soda, and types of salty snacks and sweets, among other beverages and foods during the past 7 days. The survey response categories (never, 1–3 in past 7 days, 4–6 in past 7 days, 1 per day, 2 per day, 3 per day, 4+ per day) were converted into times per week (0, 2, 5, 7, 14, 21, 28+). We created a weekly measure of salty snacks and sweets by summing responses to the relevant questions: salty snacks (low-fat or non-fat chips; regular chips; other salty snacks) and sweets (candy; doughnuts or other pastries; cookies, brownies, pies and cakes; low fat or nonfat frozen desserts; regular ice cream and milkshakes). Children were also asked how often they ate a dinner that was ready-made in the past 7 days. Parents were asked how often the family had a dinner that was ready-made in the past week.
Objectively measured neighborhood food environment
Objective measures of the neighborhood food environment summarized the availability and number of various food outlets within certain radii from the family’s home. Home addresses provided by parents were geocoded to a position along the street network using the 10.0 U.S. Streets Address Locator within ArcGIS (ESRI, Redlands CA). Circular buffers around the family’s home were computed using 0.5-, 1- and 2-mile radii from each family’s home to generate counts of fast food outlets, restaurants, supermarkets, small grocery stores, and convenience stores within the buffers. The food outlet data were geocoded to latitude and longitude based on the 2012 release of InfoUSA, a dataset of all business establishments that includes the name, location, sales volume, and North American Industry Classification System (NAICS). Fast food outlets were identified as limited service restaurants (NAICS 722513). Our set of fast food outlets also includes the outlets from the National Restaurants Association list of top 100 fast-food chains. The NAICS were used to identify restaurants ( NAICS 7225511), supermarkets with annual sales greater than $2 million (NAICS 445100), small grocery stores with annual sales less than or equal to $2 million ( NAICS 445100), and convenience stores (NAICS 445120). We constructed a similar measure for warehouse/megastores, but there was almost no variation in the measure: 99% of families had no warehouse/megastore within 2 miles of the home. Commissaries are another shopping outlet alternative for military personnel, but were not identified in the data; moreover, we assumed that all military personnel have access the commissary during their time on the installation which implies no variation in this measure across families. Among the three distances, the 2- mile radius was selected as the main objective measure because it is consistent with the literature (Ball, Timperio, & Crawford, 2006) and provides sufficient variation.
Perceived neighborhood food environment
Parents completed the parent version of the Neighborhood Environment Walkability Scale – Youth version (NEWS-Y) (Adams et al., 2009; Saelens, Sallis, Black, & Chen, 2003). To correspond to the objective neighborhood food environment measures, individual questions from the NEWS-Y were utilized, including how long it would take the parent to walk from the home to the nearest convenience/corner store/small grocery store/bodega, supermarket, fast food restaurant, and non-fast food restaurant. Responses included: 1–5, 6–10, 11–20, 21–30, and 31+ minutes. Based on these data, we created indicator variables for whether there was a parent-reported store (of each type) within a 20 minute walk from home.
Where family accesses food
Regarding food-at-home, parents were asked where the family most often shops for each of the following grocery items: fruits and vegetables; meat, fish, eggs, beans; milk and dairy products; bread, rice, pasta, cereals, other grains. Indicator variables were constructed to indicate whether the family shops most often for groceries at the commissary, supermarket, convenience or small grocery store, warehouse or mega store, or other by selecting the modal food shopping location.
For away-from-home foods, children were asked how many times they ate a meal or snack from a fast food restaurant in the past 7 days. The survey response categories (never, 1–3 in past 7 days, 4–6 in past 7 days, 1 per day, 2 per day, 3 per day, 4+ per day) were converted into times per week (0, 2, 5, 7, 14, 21, 28+). Children who ate at least one fast food meal in the past 7 days were asked where they most often got it from (on-post or off-post). Parents were also asked, in a typical week, how many evenings their family eats out at a restaurant or gets take-out dinner (response categories were 0 to 7).
Home food environment
The home food environment variable measured the “healthiness” of the food available in the home by summarizing how much parents agree or disagree with the following statements about the food environment in their home: most of the food in the house is healthy; there are a lot of salty snacks in our house (reverse coded); there are a lot of sweets in our house (reverse coded); there are a lot of other high-fat foods in our house (reverse coded); there are a lot of sweetened beverages in our house (reverse coded); a variety of healthy foods is available to my child at each meal served at home. The response categories included strongly disagree, somewhat disagree, neutral, somewhat agree, and strongly agree.
These six items were summed to create an overall score for the home food healthiness. Higher scores indicated a healthier home food environment.
Parental supervision and children's dietary behaviors
Two sets of variables captured parental supervision on children’s dietary behaviors. First we created a measure of the parents’ rules for snack foods. Parents were asked what limits, if any, their family set on the child’s intake of the following foods and beverages: Sugary drinks, Salty snacks, and Sweets. Parent responses included No limit, 0–1 per week; 2–3 per week, 4–6 per week, 1 per day, 2 per day, 3 per day, and 4 or more per day. These items we recoded to dichotomous variables indicating whether the family had set a limit of three or fewer servings per week. Second, parents were asked separate questions about how many days per week the family eats breakfast and dinner together.
Other covariates
We included child, family and contextual covariates that may influence dietary and BMI outcomes such as the child’s age in months, gender, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic/Latino, other), education levels of both parents (less than high school, high school graduate or equivalent, some college, and college graduate or higher), household income (<=$40,000; $40,001–$50,000; $50,001–$75,000; $75,001 or higher), marital status, and number of children in household, whether the family lives on-post, and region (west, south, midwest, northeast, other). In addition, two measures of residential location preference (how important proximity to supermarkets and proximity to restaurants were to selection of family residence) were included in the regressions that examine the neighborhood food environment and dietary behaviors. These measures of residential location preference adjust for one aspect of self-selection.
Results
Descriptive statistics of the M-TEENS sample are presented in a previous paper (Excluded for review). The mean age of children was 13.2 years. Almost 41% of the sample were White, non-Hispanic (40.8%), 20.7% were Black, non-Hispanic, 24.6% were Hispanic/Latino, and 13.9% were other. Almost 44% had an income of less than or equal to $50,000. The 903 children in the M-TEENS sample lived in 408 Census Block Groups.
Approximately 26% of the children in the sample were obese or overweight. The average number of servings of fruits (8.9), vegetables (8.1), soda (3.1), sweets (12.5) and salty snacks (7.6) per week are reported in Table 1 as are the number of child- and parent-reported ready-made meals (1.3 and 0.9) per week. Most families shopped at the commissary (57.7%) followed by discount/big box/wholesale clubs (16.6%), supermarkets (15.3%), convenience/small grocery stores (1.9%) and other outlets (8.5%). Many families reported having limits on sugary drinks (64.4%), salty snacks (50.1%) and sweets (59.7%). On average, the families ate dinner together (5.5 times per week) twice as often as breakfast together (2.7 times).
Table 1.
Summary statistics of the study sample
| % or Mean (SD) | |
|---|---|
| Child BMI z-score | 0.41 (1.02) |
| Child overweight or obese | 26.2% |
| Times per week | |
| Fruits | 8.9 (7.7) |
| Vegetables | 8.1 (7.1) |
| Soda | 3.1 (4.6) |
| Sweets | 12.5 (13.8) |
| Salty snacks | 7.6 (8.9) |
| Ready-made food (child-reported) | 1.3 (1.8) |
| Ready-made food (parent-reported) | 0.9 (1.1) |
| Objective measures: food outlets within 2-miles of home | |
| Fast food | |
| 0 | 22.1% |
| 1–2 | 17.3% |
| 3–4 | 13.0% |
| 5+ | 47.6% |
| Restaurants | |
| 0 | 14.4% |
| 1–2 | 17.1% |
| 3–4 | 19.1% |
| 5+ | 49.4% |
| Convenience stores | |
| 0 | 30.8% |
| 1–2 | 56.2% |
| 3–4 | 13.0% |
| 5+ | 0.0% |
| Small grocery stores | |
| 0 | 61.0% |
| 1–2 | 26.2% |
| 3–4 | 8.2% |
| 5+ | 4.6% |
| Supermarkets | |
| 0 | 61.4% |
| 1–2 | 32.8% |
| 3–4 | 5.6% |
| 5+ | 0.2% |
| Perceived measures: food outlets within 20-minute walk of home |
|
| Fast food | 44.2% |
| Restaurants | 31.9% |
| Convenience/small grocery stores | 72.4% |
| Supermarkets | 44.6% |
| Most shopping done at: | |
| Commissary | 57.7% |
| Supermarket | 15.3% |
| Convenience/small grocery store | 1.9% |
| Discount or big box store or Wholesale club | 16.6% |
| Other | 8.5% |
| Home food healthiness | 22.0 (4.5) |
| Limits on child intake (<=3 servings per week) | |
| Sugary drinks | 64.4% |
| Salty snacks | 50.1% |
| Sweets | 59.7% |
| Meals eaten as family per week | |
| Breakfast | 2.7 (2.1) |
| Dinner | 5.5 (1.7) |
Source: Military Teenagers’ Environments, Exercise and Nutrition Study, wave 1 (2013).
Notes: SD: Standard deviation
There was considerable variation across food outlet types and across families. The modal number of fast food outlets and restaurants was 5+, but almost one in four families had no fast food outlets and 14.4% had no restaurants within 2 miles of their home. Convenience stores, small grocery stores, and supermarkets were less common with modal responses of 1–2 convenience stores and 0 small grocery stores and supermarkets. Using parent-perceived measures of outlets within a 20-minute walk, convenience stores/small grocery stores were most common (72.4%) followed by supermarkets (44.6%), fast food outlets (44.2%) and restaurants (31.9%).
Neighborhood food environment and child BMI and dietary behaviors
Table 2 presents the estimated adjusted associations between the objective and parent-perceived neighborhood food environment and the child’s BMI and dietary behaviors.
Table 2.
Regression estimates of the association between objective and perceived neighborhood food environment and children’s BMI and dietary behaviors
| Times per week | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Overweight or obese Coef (SE) |
BMI z-score Coef (SE) |
Fruits Coef (SE) |
Vegetables Coef (SE) |
Soda Coef (SE) |
Sweet snacks Coef (SE) |
Salty snacks Coef (SE) |
Ready- made dinner Coef (SE) |
Ready- made dinner (parent) Coef (SE) |
|
| Objective Measures: Number of food outlets within 2 miles of home | |||||||||
| Fast food | 0.000 | −0.001 | 0.014 | 0.068* | 0.006 | −0.040 | −0.056* | 0.003 | 0.003 |
| (0.002) | (0.004) | (0.037) | (0.033) | (0.025) | (0.033) | (0.026) | (0.011) | (0.006) | |
| Restaurant | −0.001 | −0.001 | 0.001 | 0.016 | 0.005 | 0.023 | −0.014 | −0.003 | −0.002 |
| (0.001) | (0.002) | (0.011) | (0.012) | (0.009) | (0.017) | (0.008) | (0.004) | (0.003) | |
| Convenience store | −0.019 | 0.007 | −0.011 | 0.254 | 0.035 | −0.358 | −0.255 | 0.026 | −0.040 |
| (0.016) | (0.039) | (0.160) | (0.199) | (0.212) | (0.452) | (0.288) | (0.060) | (0.048) | |
| Small Grocery store | −0.001 | 0.004 | −0.014 | 0.033 | 0.007 | −0.110 | −0.027 | −0.019 | 0.016 |
| (0.004) | (0.010) | (0.043) | (0.080) | (0.054) | (0.168) | (0.051) | (0.025) | (0.011) | |
| Supermarket | 0.011 | 0.025 | −0.319* | 0.037 | −0.113 | −0.103 | −0.458* | −0.036 | −0.018 |
| (0.014) | (0.028) | (0.173) | (0.154) | (0.085) | (0.325) | (0.192) | (0.071) | (0.033) | |
| Perceived Measures: Parent reported whether food outlet within 20 minute walk of home | |||||||||
| Fast food | 0.020 | 0.020 | −0.416 | −0.736 | −0.432 | −0.912 | −0.092 | −0.110 | −0.057 |
| (0.030) | (0.051) | (0.926) | (0.763) | (0.271) | (1.388) | (0.594) | (0.148) | (0.063) | |
| Restaurant | 0.023 | −0.013 | −0.200 | −0.174 | −0.415 | −0.981 | −0.196 | −0.124 | −0.078 |
| (0.034) | (0.058) | (0.785) | (0.784) | (0.388) | (0.895) | (0.445) | (0.135) | (0.058) | |
| Convenience store | −0.018 | 0.010 | −0.423 | −0.234 | −0.184 | 0.744 | −0.157 | −0.238 | −0.059 |
| (0.033) | (0.088) | (1.121) | (0.739) | (0.296) | (0.829) | (0.544) | (0.154) | (0.056) | |
| Supermarket | −0.002 | 0.051 | −0.150 | −0.140 | −0.535* | −0.843 | −0.548 | −0.151 | −0.062 |
| (0.024) | (0.047) | (0.767) | (0.663) | (0.238) | (1.019) | (0.452) | (0.125) | (0.053) | |
p<0.01,
p<0.05
Source: Military Teenagers’ Environments, Exercise and Nutrition Study, wave 1 (2013). Sample size ranges from 778 to 941.
Notes: SE = Standard Error. Each cell represents a separate regression. All regressions controlled for child, family, and contextual covariates and how important proximity to supermarket or produce market and restaurants were in selecting family’s current residence.
The top panel presents the results using the objective measures of the neighborhood food environment using the 2-mile radius from the child’s home. Most of the estimated coefficients were close to zero and none were statistically significant. The bottom panel presents the results using the parent-perceived measures of the neighborhood food environment. Again, there were no significant associations between the neighborhood food environment and child’s dietary behaviors, BMI, or overweight/obese. Sensitivity analyses using alternative radii of 0.5 and 1 mile produced qualitatively similar findings.
The results thus far suggest that there are no significant relationships between the availability of fast food outlets, restaurants, convenience stores, small grocery stores, and supermarkets in the child’s neighborhood and their BMI, obesity or diet. These results are consistent with recent larger cross-sectional and longitudinal studies examining food availability and children’s outcomes (An & Sturm, 2012; Lee, 2012; L. M. Powell & Bao, 2009; Shier, et al., 2012; Sturm & Datar, 2005).
Neighborhood food environment and where family accesses food
Next, we provide insight into why living in neighborhoods with fewer supermarkets or more convenience stores or fast food outlets might not contribute to “unhealthy” diets among children. Specifically, we examined whether the availability of certain food outlets is related to where a family shops for or eats food.
There were no significant relationships between the availability of particular food outlets and where the family shops for groceries (Table 3). In fact, families with a supermarket within 2 miles of home were no more likely to shop at a supermarket than those who have without (Table 3). These findings may be because families are willing to travel further than two miles from their home to grocery shop. Families may shop for groceries at stores close to the parents’ work, their children’s schools, or other convenient locations. In our sample, most families shopped at the on-post Commissary (i.e., where at least one parent works and items are sold at lower prices) or a discount, big box store, or wholesale club even though many families live off-post and almost none live within 2 miles of a wholesale club. This suggests that affordability may be an important consideration. Relatedly, a recent nationally representative survey of households found that households do not shop at the nearest supermarket, even if they walk, bike, or use public transportation to get to the store (Ver Ploeg, Mancino, Todd, Clay, & Scharadin, 2015). A study of residents in a food desert also found that they did not rely on the neighborhood stores, but bypassed closer stores to shop at a preferred supermarket (Dubowitz, Ncube, Leuschner, & Tharp-Gilliam, 2015).
Table 3.
Regression estimates of the association between objective neighborhood food environment and where families shop for food
| Family shops for food at: | ||||
|---|---|---|---|---|
| Food stores available within 2 mile of home |
Commissary Coef (SE) |
Supermarket Coef (SE) |
Small grocery/conv store Coef (SE) |
Warehouse/ Mega store Coef (SE) |
| Has at least one Supermarket | −0.021 | 0.014 | −0.001 | −0.006 |
| (0.047) | (0.032) | (0.011) | (0.026) | |
| Has at least one Small grocery store | 0.011 | −0.001 | 0.011 | −0.028 |
| (0.042) | (0.019) | (0.009) | (0.042) | |
| Has at least one convenience store | −0.027 | 0.051 | −0.009 | −0.023 |
| (0.043) | (0.025) | (0.012) | (0.038) | |
p<0.01,
p<0.05
Source: Military Teenagers’ Environments, Exercise and Nutrition Study, wave 1 (2013). Sample size is 945.
Notes: SE = Standard Error. Reference group is no food store. Each column represents a separate regression.
All regressions controlled for child, family, and contextual covariates.
The results were similar when we examined the relationships for food outlets offering prepared foods. Children with fast food outlets or restaurants did not consume more fast food meals/snacks or restaurant and take-out meals per week (Table 4), respectively. Further, most children reported that they most often got fast food from locations off-post even if they lived on-post.
Table 4.
Regression estimates of the association between objective neighborhood food environment and fast food outlet and restaurant meals
| Food outlets available within 2 mile of home |
Number of fast food meals/snacks Coef (SE) |
Number of restaurant or take-out dinners Coef (SE) |
|---|---|---|
| Has at least one restaurant |
0.022 | −0.035 |
| (0.158) | (0.103) | |
| Has at least one fast food outlet |
0.210 | 0.0432 |
| (0.100) | (0.085) |
p<0.05,
p<0.10
Source: Military Teenagers’ Environments, Exercise and Nutrition Study, wave 1 (2013). Sample size ranges from 815 to 945.
Notes: SE = Standard error. Reference group is no food outlet. Each column represents a separate regression. All regressions controlled for child, family, and contextual covariates.
Food-at-home: home food environment and children’s diet and BMI
Next, we examined whether the type of food outlet the family shops at was related to the healthiness of foods available at home, children’s diet, and BMI. The regressions indicate that where the family shops for groceries is not associated with the healthiness of food available at home (Table 5). In particular, even shopping at a supermarket was not associated with healthier food environment at home. The estimated relationships with children’s diet were also small and non-significant with one exception. Compared to shopping at the Commissary, shopping at convenience/small grocery stores was associated with children eating fewer ready-made dinners (−0.993). While these results may initially seem counterintuitive, most families shopped at supermarkets or the Commissary that may provide greater opportunity for junk food purchases given that all food outlets devote more shelf space to unhealthy items than healthy items and supermarkets offer more total shelf space (Farley, et al., 2009).
Table 5.
Regression estimates of the association between where families shop for food and home food environment/child’s dietary behaviors
| Times per week | ||||||||
|---|---|---|---|---|---|---|---|---|
| Home food healthiness Coef (SE) |
Fruits Coef (SE) |
Vegetables Coef (SE) |
Soda Coef (SE) |
Sweet snacks Coef (SE) |
Salty snacks Coef (SE) |
Ready-made dinner Coef (SE) |
Ready–made dinner (parent) Coef (SE) |
|
| Supermarket | −0.406 | −0.083 | 0.515 | 0.680 | 1.205 | 0.994 | 0.123 | 0.149 |
| (0.451) | (0.846) | (0.777) | (0.504) | (1.524) | (0.964) | (0.191) | (0.112) | |
| Small grocery/ convenience |
−0.865 | 0.662 | 0.744 | −1.556 | −4.430 | −4.345 | −0.993* | −0.244 |
| (1.137) | (2.016) | (1.845) | (1.194) | (3.530) | (2.361) | (0.456) | (0.277) | |
| Warehouse/ Mega store |
0.059 | −0.399 | −0.046 | 0.677 | 1.833 | 0.059 | −0.137 | 0.209 |
| (0.435) | (0.804) | (0.735) | (0.477) | (1.420) | (0.919) | (0.182) | (0.108) | |
| Other | 0.990 | 1.766 | 0.512 | −0.184 | 1.928 | 0.675 | −0.035 | 0.005 |
| (0.556) | (0.980) | (0.902) | (0.580) | (1.746) | (1.114) | (0.223) | (0.137) | |
p<0.01,
p<0.05
Source: Military Teenagers’ Environments, Exercise and Nutrition Study, wave 1 (2013). Sample size ranges from 786 to 950.
Notes: SE = Standard error. Reference group is shopping at the Commissary. Each column represents a separate regression.
Home food healthiness is a summary score of 6 parent questions about food in the home. Higher score indicates healthier home food environment.
All regressions controlled for child, family, and contextual covariates.
We found evidence of significant relationships between the home food environment and children’s diet. Healthier home food environments as reported by the parents were significantly associated with higher consumption of fruits and vegetables, less consumption of soda, salty snacks, and sweet snacks, and fewer dinners of ready-made food among children (Appendix). Although we found no significant association with BMI and overweight or obese, these results underscore the importance of the role that parents can play in contributing to the obesogenic environment at home.
Away-from-home foods: fast food and restaurant meals and child dietary behaviors and BMI
Consistent with the existing literature (Bauer, et al., 2009; Bowman, et al., 2004; Lisa M Powell & Nguyen, 2013), we also found evidence of significant relationships between fast food and restaurant consumption and children’s diet (Appendix). An additional fast food meal/snack per week was associated with lower frequency of eating fruit (−0.580) and vegetables (−0.442) and higher frequency of drinking soda (0.489), eating sweet snacks (1.056) and eating salty snacks (0.430). An additional restaurant meal per week was associated with eating vegetables fewer times per week (−0.611), drinking more soda more times (0.362) and eating ready-made dinners (0.249) more times per week. However, these results are more likely to be biased due to endogeneity since the same factors may contribute to the choice to eat at a fast food outlet and the choice of what to eat overall. Children who eat a lot of fast food or restaurant meals may also eat lower quality foods at home. We found no significant relationships with BMI or the probability of being overweight or obese.
Parental supervision and children’s diet and BMI
Finally, we examined the role of parental supervision defined as limits on sugary drinks, salty snacks, and sweets and the number of breakfast meals and dinner meals eaten together. With few exceptions, the significant relationships between the home food environment and children’s diet and between fast food meals/snacks and diet were robust to the addition of parental supervision covariates (Appendix and Table 6) suggesting that parental supervision has a separate influence on dietary behaviors. In both food-at-home (Table 6, Panel A) and away-from-home regressions (Table 6, Panel B), setting limits was significantly associated with children consuming fewer sugary drinks and salty snacks, but not sweet snacks. Finally, eating an additional dinner, but not breakfast, together as a family was associated with children eating fewer ready-made dinners. These results confirm a strong relationship between parental supervision and children’s diet.
Table 6.
Regression estimates of the association between home food healthiness, eating out, parent supervision, and child dietary behaviors and BMI
| Times per week | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Overweight or Obese Coef (SE) |
BMI z- score Coef (SE) |
Fruits Coef (SE) |
Vegetables Coef (SE) |
Soda Coef (SE) |
Sweet snacks Coef (SE) |
Salty snacks Coef (SE) |
Ready-made dinner Coef (SE) |
Ready-made dinner (parent) Coef (SE) |
|
| Panel A: Food-at-home | |||||||||
| Home food healthiness |
−0.002 | 0.003 | 0.328** | 0.288** | −0.121** | −0.275* | −0.139 | −0.025 | −0.055** |
| (0.004) | (0.009) | (0.068) | (0.062) | (0.038) | (0.116) | (0.076) | (0.015) | (0.009) | |
| Limits on soda | 0.040 | 0.108 | 0.087 | 0.525 | −1.598** | −2.329 | −0.787 | −0.181 | 0.022 |
| (0.041) | (0.092) | (0.696) | (0.633) | (0.393) | (1.204) | (0.783) | (0.153) | (0.090) | |
| Limits on salty snacks |
−0.040 | −0.089 | 0.505 | 0.914 | 0.102 | 0.365 | −2.125** | −0.061 | −0.103 |
| (0.041) | (0.093) | (0.702) | (0.642) | (0.398) | (1.218) | (0.794) | (0.155) | (0.092) | |
| Limits on sweet snacks |
−0.029 | −0.105 | −0.724 | −0.727 | 0.263 | −1.550 | 0.593 | −0.191 | 0.076 |
| (0.044) | (0.100) | (0.750) | (0.685) | (0.424) | (1.306) | (0.847) | (0.166) | (0.098) | |
| Days family eats breakfast together |
−0.014 | −0.020 | 0.078 | 0.082 | −0.079 | 0.125 | −0.047 | −0.007 | −0.013 |
| (0.008) | (0.018) | (0.138) | (0.126) | (0.078) | (0.240) | (0.156) | (0.030) | (0.018) | |
| Days family eats dinner together |
0.017* | 0.012 | 0.143 | 0.301 | −0.059 | −0.505 | 0.084 | −0.168** | −0.141** |
| (0.010) | (0.023) | (0.173) | (0.157) | (0.097) | (0.298) | (0.195) | (0.038) | (0.022) | |
| Panel B: Away-from home foods | |||||||||
| Number of fast food meals/snacks |
−0.000 | 0.011 | −0.532** | −0.388* | 0.427** | 0.922** | 0.352 | 0.186** | 0.008 |
| (0.010) | (0.022) | (0.165) | (0.151) | (0.095) | (0.287) | (0.189) | (0.036) | (0.023) | |
| Number of restaurant or take-out dinners |
0.005 | −0.015 | 0.070 | −0.524 | 0.208 | 0.428 | 0.098 | 0.032 | 0.202** |
| (0.018) | (0.040) | (0.301) | (0.273) | (0.173) | (0.521) | (0.345) | (0.066) | (0.041) | |
| Limits on soda | 0.042 | 0.122 | 0.149 | 0.515 | −1.625** | −2.563* | −0.670 | −0.137 | −0.040 |
| (0.041) | (0.093) | (0.693) | (0.628) | (0.397) | (1.196) | (0.789) | (0.152) | (0.095) | |
| Limits on salty snacks |
−0.040 | −0.070 | 0.741 | 1.117 | 0.042 | −0.214 | −2.307** | −0.049 | −0.208* |
| (0.041) | (0.093) | (0.697) | (0.634) | (0.401) | (1.208) | (0.798) | (0.154) | (0.096) | |
| Limits on sweet snacks |
−0.035 | −0.107 | −0.039 | −0.259 | 0.202 | −1.082 | 0.687 | −0.166 | 0.034 |
| (0.044) | (0.100) | (0.747) | (0.678) | (0.429) | (1.296) | (0.854) | (0.165) | (0.103) | |
| Days family eats breakfast together |
−0.014 | −0.020 | 0.153 | 0.106 | −0.118 | −0.021 | −0.080 | −0.005 | −0.017 |
| (0.008) | (0.018) | (0.135) | (0.123) | (0.078) | (0.234) | (0.154) | (0.030) | (0.019) | |
| Days family eats dinner together |
0.015 | 0.010 | 0.251 | 0.400** | −0.051 | −0.363 | 0.095 | −0.161** | −0.154** |
| (0.010) | (0.023) | (0.170) | (0.154) | (0.097) | (0.292) | (0.195) | (0.037) | (0.023) | |
p<0.01,
p<0.05
Source: Military Teenagers’ Environments, Exercise and Nutrition Study, wave 1 (2013). Sample size ranges from 764 to 913.
Note: SE = Standard Error. Each column within the panel represents a separate regression.
Home food healthiness is a summary score of 6 parent questions about food in the home. Higher score indicates healthier home food environment.
All regressions controlled for child, family, and contextual covariates.
Conclusion
Several recent federal and local policies and programs focus on promoting access to supermarkets and restricting access to fast food outlets despite growing evidence that availability of particular food outlets may not be associated with diet and BMI among children and adolescents (An & Sturm, 2012; Lee, 2012; Shier, et al., 2012). This study adds to the growing body of evidence that the availability of supermarkets close to home is not associated with positive children’s dietary outcomes, lower BMI and lower probability of overweight/obesity and, similarly, that the availability of fast food outlets and convenience stores is not associated with negative outcomes among children. These confirmatory findings are noteworthy given that our sample of military families, whose relocation generates unique variation in neighborhood environments, is not subject to the same level of residential selection that undermines typical observational studies and that we examine both perceived and objective measures of multiple aspects of the environment.
Our additional contributions are a rich exploration of 1) the potential reasons for these null findings and 2) the role of the home environment and parental supervision on children’s dietary behaviors. The availability of grocery food outlets was not associated with where a family shopped for groceries and the family’s choice of outlet was not associated with the healthiness of the food in the home nor children’s diet. Likewise, the availability of fast food outlets was not associated with how often children eat fast food meals. However, we did find significant associations between both the healthiness of food available at home and consumption of fast food and restaurant meals as well as measures of parental supervision on children’s diet.
An important limitation of this study is the quality of the InfoUSA business dataset, as field observations have been found to have only fair to good agreement with commercial data(Bader, Ailshire, Morenoff, & House, 2010; Lisa M Powell et al., 2011) which increases the noise and the probability of a null finding. However, we also found no association between whether the parent-perceived food outlets were close to home and children’s diet. Another option would have been field observations, but that would be infeasible for such a large and geographically-dispersed sample of participants. Second, neighborhoods were defined using Euclidean distance to measure the 2-mile buffer, but a street network distance might provide better measure of travel distance or time. Third, there may be remaining selection bias because families can choose where to live around their assigned installation. However, two measures of residential location preference were included in the analyses that examined the neighborhood food environment, which adjust for one aspect of self-selection. Finally, our data focuses on families with an Army-enlisted parent in an effort to address the common concern regarding neighborhood selection, but, as a result, our findings may not be completely generalizable. These families exhibit similar patterns of obesity and related behaviors as civilian populations and the availability of a commissary may provide a similar affordable shopping option to big box or discount stores available to civilian families, which suggests that our findings may provide some insights for civilian populations living in similar environments.
The main take-away from our analyses is that focusing only on the availability of particular food outlets in the neighborhood may ignore other important factors, including how families make decisions about food purchases and where to shop for foods, availability of healthy foods at home, consumption of fast food and restaurant meals, and parental limits, that may collectively impact children’s obesity and dietary behaviors. However, we caution that our models examining the healthiness of the home food environment, consumption of fast food and restaurant meals, and parental limits and children’s outcomes are vulnerable to bias from potential endogeneity because unobserved individual characteristics may be correlated with the explanatory variables and children’s outcomes. Given the current research and policy emphasis on the neighborhood food environment, policy initiatives and interventions could focus greater attention on the home food environment and the role of parents. Parents have a central role in helping to shape their children’s dietary habits (Savage, Fisher, & Birch, 2007). Parents can help promote healthy eating behaviors through the types and amounts of foods available in the home (Cullen, et al., 2003; Jago, Baranowski, & Baranowski, 2007; Kratt, Reynolds, & Shewchuk, 2000) and accessibility of foods in home (e.g., having fruits on the counter) (Cullen, et al., 2003). Modeling healthy food consumption (Arcan et al., 2007; Orlet Fisher, Mitchell, WRIGHT, & Birch, 2002; Young, Fors, & Hayes, 2004) is also important. Parent fruit and vegetable intake has been associated with fruit and vegetable intake among children (Hanson, Neumark-Sztainer, Eisenberg, Story, & Wall, 2005; Orlet Fisher, et al., 2002). Child dietary behaviors may also be influenced by parenting practices. Authoritative parenting styles that are firm but warm (likely to set limits for children based on reasoning rather than intimidation) have been associated with greater intake of fruit and vegetables and lower intake of junk food (Gable & Lutz, 2000; Lytle et al., 2003), while authoritarian (firm and likely to set rigid limits with punishment) and permissive (warm but not firm and less likely to set limits) parenting styles may not have the intended effect and lower intakes of fruits and vegetables (Cullen et al., 2000; De Bourdeaudhuij, 1997; Patrick & Nicklas, 2005). The home environment can either facilitate or inhibit healthy eating among children and parents play a key role in maintaining and supporting the home environment. Future research and interventions should address the complexity of the role of the home environment and familial influences on child diet and obesity.
Highlights.
Examine link between the food environment and children’s outcomes in Army families.
Finds that focusing only on the neighborhood may ignore other important factors.
Home environment, eating out, and parent supervision may impact children’s outcomes.
Appendix
Appendix Table.
Regression estimates of the association between home food healthiness, eating out, and child dietary behaviors and BMI
| Times per week | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Overweight or Obese Coef (SE) |
BMI z- score Coef (SE) |
Fruits Coef (SE) |
Vegetables Coef (SE) |
Soda Coef (SE) |
Sweet snacks Coef (SE) |
Salty snacks Coef (SE) |
Ready-made dinner Coef (SE) |
Ready-made dinner (parent) Coef (SE) |
|
| Panel A: Food-at-home | |||||||||
| Home food healthiness |
−0.003 | −0.002 | 0.345** | 0.339** | −0.159** | −0.390** | −0.204** | −0.053** | −0.068** |
| (0.004) | (0.008) | (0.061) | (0.056) | (0.035) | (0.105) | (0.069) | (0.014) | (0.008) | |
| Panel B: Away-from home foods | |||||||||
| Number of fast food meals/snacks |
0.001 | 0.016 | −0.580** | −0.442** | 0.489** | 1.056** | 0.430* | 0.203** | 0.025 |
| (0.010) | (0.022) | (0.163) | (0.150) | (0.096) | (0.284) | (0.186) | (0.037) | (0.023) | |
| Number of restaurant or take-out dinners |
0.005 | −0.008 | −0.052 | −0.611* | 0.362* | 0.697 | 0.159 | 0.082 | 0.249** |
| (0.017) | (0.040) | (0.292) | (0.268) | (0.172) | (0.509) | (0.337) | (0.066) | (0.041) | |
p<0.01,
p<0.05
Source: Military Teenagers’ Environments, Exercise and Nutrition Study, wave 1 (2013). Sample size ranges from 776 to 932.
Notes: SE: Standard error. Each column within the panel represents a separate regression.
Home food healthiness is a summary score of 6 parent questions about food in the home. Higher score indicates healthier home food environment.
All regressions controlled for child, family, and contextual covariates.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Victoria Shier, Email: vshier@prgs.edu, Pardee RAND Graduate School, 1776 Main St, Santa Monica CA 90401 310-393-0411 x 6657.
Nancy Nicosia, Email: nicosia@rand.org, RAND Corporation, 20 Park Plaza #920, Boston, MA 02116 617-338-2059.
Ashlesha Datar, Email: adatar@usc.edu, Center for Economic and Social Research, University of Southern California 635 Downey Way, Los Angeles CA 90089, 212-821-1850.
References
- 2014 Health Care Survey of DoD Beneficiaries: Adult Technical Manual. Washington DC: Mathematica Policy Research Inc.; 2014. Aug, [Google Scholar]
- Adams MA, Ryan S, Kerr J, Sallis JF, Patrick K, Frank LD, Norman GJ. Validation of the Neighborhood Environment Walkability Scale (NEWS) items using geographic information systems. Journal of physical activity & health. 2009;6(1):S113. doi: 10.1123/jpah.6.s1.s113. [DOI] [PubMed] [Google Scholar]
- An R, Sturm R. School and residential neighborhood food environment and diet among California youth. American journal of preventive medicine. 2012;42(2):129–135. doi: 10.1016/j.amepre.2011.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcan C, Neumark-Sztainer D, Hannan P, van den Berg P, Story M, Larson N. Parental eating behaviours, home food environment and adolescent intakes of fruits, vegetables and dairy foods: longitudinal findings from Project EAT. Public health nutrition. 2007;10(11):1257–1265. doi: 10.1017/S1368980007687151. [DOI] [PubMed] [Google Scholar]
- Bader MD, Ailshire JA, Morenoff JD, House JS. Measurement of the local food environment: a comparison of existing data sources. American journal of epidemiology. 2010;171(5):609–617. doi: 10.1093/aje/kwp419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball K, Timperio AF, Crawford DA. Understanding environmental influences on nutrition and physical activity behaviors: where should we look and what should we count? International Journal of Behavioral Nutrition and Physical Activity. 2006;3(1):33. doi: 10.1186/1479-5868-3-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer KW, Larson NI, Nelson MC, Story M, Neumark-Sztainer D. Fast food intake among adolescents: secular and longitudinal trends from 1999 to 2004. Preventive medicine. 2009;48(3):284–287. doi: 10.1016/j.ypmed.2008.12.021. [DOI] [PubMed] [Google Scholar]
- Bowman SA, Gortmaker SL, Ebbeling CB, Pereira MA, Ludwig DS. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics. 2004;113(1):112–118. doi: 10.1542/peds.113.1.112. [DOI] [PubMed] [Google Scholar]
- Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, Peters SM, McCaslin C, Joyce R, Ickovics JR. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: The role of built, socioeconomic, and social environments. Social Science & Medicine. 2013;95:106–114. doi: 10.1016/j.socscimed.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casagrande SS, Whitt-Glover MC, Lancaster KJ, Odoms-Young AM, Gary TL. Built environment and health behaviors among African Americans: a systematic review. American journal of preventive medicine. 2009;36(2):174–181. doi: 10.1016/j.amepre.2008.09.037. [DOI] [PubMed] [Google Scholar]
- Caspi CE, Sorensen G, Subramanian S, Kawachi I. The local food environment and diet: a systematic review. Health & Place. 2012;18(5):1172–1187. doi: 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawley J. Addiction and the consumption of calories: Implications for obesity. Unpublished manuscript. 2002 [Google Scholar]
- Cawley J. The impact of obesity on wages. Journal of Human Resources. 2004;39(2):451–474. [Google Scholar]
- Cullen KW, Baranowski T, Owens E, Marsh T, Rittenberry L, de Moor C. Availability, accessibility, and preferences for fruit, 100% fruit juice, and vegetables influence children's dietary behavior. Health Education & Behavior. 2003;30(5):615–626. doi: 10.1177/1090198103257254. [DOI] [PubMed] [Google Scholar]
- Cullen KW, Baranowski T, Rittenberry L, Cosart C, Owens E, Hebert D, de Moor C. Socioenvironmental influences on children's fruit, juice and vegetable consumption as reported by parents: reliability and validity of measures. Public health nutrition. 2000;3(03):345–356. doi: 10.1017/s1368980000000392. [DOI] [PubMed] [Google Scholar]
- Datar A, Nicosia N, Wong E, Shier V. Neighborhood Environment and Children's Physical Activity and Body Mass Index: Evidence from Military Personnel Installation Assignments. Childhood Obesity. 2015 doi: 10.1089/chi.2014.0094. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bourdeaudhuij I. Family food rules and healthy eating in adolescents. Journal of health psychology. 1997;2(1):45–56. doi: 10.1177/135910539700200105. [DOI] [PubMed] [Google Scholar]
- Ding D, Sallis JF, Kerr J, Lee S, Rosenberg DE. Neighborhood environment and physical activity among youth: a review. American journal of preventive medicine. 2011;41(4):442–455. doi: 10.1016/j.amepre.2011.06.036. [DOI] [PubMed] [Google Scholar]
- Ding D, Sallis JF, Norman GJ, Saelens BE, Harris SK, Kerr J, Glanz K. Community food environment, home food environment, and fruit and vegetable intake of children and adolescents. Journal of nutrition education and behavior. 2012;44(6):634–638. doi: 10.1016/j.jneb.2010.07.003. [DOI] [PubMed] [Google Scholar]
- Dubowitz T, Ncube C, Leuschner K, Tharp-Gilliam S. A Natural Experiment Opportunity in Two Low-Income Urban Food Desert Communities Research Design, Community Engagement Methods, and Baseline Results. Health Education & Behavior. 2015;42(1 suppl):87S–96S. doi: 10.1177/1090198115570048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebbeling CB, Feldman HA, Osganian SK, Chomitz VR, Ellenbogen SJ, Ludwig DS. Effects of decreasing sugar-sweetened beverage consumption on body weight in adolescents: a randomized, controlled pilot study. Pediatrics. 2006;117(3):673–680. doi: 10.1542/peds.2005-0983. [DOI] [PubMed] [Google Scholar]
- Farley TA, Rice J, Bodor JN, Cohen DA, Bluthenthal RN, Rose D. Measuring the food environment: shelf space of fruits, vegetables, and snack foods in stores. Journal of Urban Health. 2009;86(5):672–682. doi: 10.1007/s11524-009-9390-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French SA, Story M, Fulkerson JA, Gerlach AF. Food environment in secondary schools: a la carte, vending machines, and food policies and practices. American journal of public health. 2003;93(7):1161–1168. doi: 10.2105/ajph.93.7.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fryar CD, Carroll MD, Ogden CL. Prevalence of obesity among children and adolescents: United States, trends 1963–1965 through 2009–2010. National Center for Health Statistics. 2012 [Google Scholar]
- Gable S, Lutz S. Household, Parent, and Child Contributions to Childhood Obesity*. Family relations. 2000;49(3):293–300. [Google Scholar]
- Ghosh-Dastidar B, Haas A, Nicosia N, Datar A. Accuracy of BMI Correction Using Mutiple Reports in Children. Under Review. 2015 doi: 10.1186/s40608-016-0117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimm GC, Harnack L, Story M. Factors associated with soft drink consumption in school-aged children. Journal of the American Dietetic Association. 2004;104(8):1244–1249. doi: 10.1016/j.jada.2004.05.206. [DOI] [PubMed] [Google Scholar]
- Hanson NI, Neumark-Sztainer D, Eisenberg ME, Story M, Wall M. Associations between parental report of the home food environment and adolescent intakes of fruits, vegetables and dairy foods. Public health nutrition. 2005;8(01):77–85. doi: 10.1079/phn2005661. [DOI] [PubMed] [Google Scholar]
- Jago R, Baranowski T, Baranowski JC. Fruit and vegetable availability: a micro environmental mediating variable? Public health nutrition. 2007;10(07):681–689. doi: 10.1017/S1368980007441441. [DOI] [PubMed] [Google Scholar]
- Kratt P, Reynolds K, Shewchuk R. The role of availability as a moderator of family fruit and vegetable consumption. Health Education & Behavior. 2000;27(4):471–482. doi: 10.1177/109019810002700409. [DOI] [PubMed] [Google Scholar]
- Larson N, Story M. A review of environmental influences on food choices. Annals of Behavioral Medicine. 2009;38(1):56–73. doi: 10.1007/s12160-009-9120-9. [DOI] [PubMed] [Google Scholar]
- Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. doi: S0749-3797(08)00838-6 [pii] 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- Lee H. The role of local food availability in explaining obesity risk among young school-aged children. Social Science & Medicine. 2012;74(8):1193–1203. doi: 10.1016/j.socscimed.2011.12.036. [DOI] [PubMed] [Google Scholar]
- Lleras-Muney A. The Needs of the Army Using Compulsory Relocation in the Military to Estimate the Effect of Air Pollutants on Children’s Health. Journal of Human Resources. 2010;45(3):549–590. [Google Scholar]
- Lytle LA, Varnell S, Murray DM, Story M, Perry C, Birnbaum AS, Kubik MY. Predicting adolescents' intake of fruits and vegetables. Journal of nutrition education and behavior. 2003;35(4):170–178. doi: 10.1016/s1499-4046(06)60331-x. [DOI] [PubMed] [Google Scholar]
- Neuhouser ML, Lilley S, Lund A, Johnson DB. Development and validation of a beverage and snack questionnaire for use in evaluation of school nutrition policies. Journal of the American Dietetic Association. 2009;109(9):1587–1592. doi: 10.1016/j.jada.2009.06.365. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Hannan PJ, Story M, Croll J, Perry C. Family meal patterns: associations with sociodemographic characteristics and improved dietary intake among adolescents. Journal of the American Dietetic Association. 2003;103(3):317–322. doi: 10.1053/jada.2003.50048. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Perry C, Story M. Correlates of fruit and vegetable intake among adolescents: Findings from Project EAT. Preventive medicine. 2003;37(3):198–208. doi: 10.1016/s0091-7435(03)00114-2. [DOI] [PubMed] [Google Scholar]
- Odoms-Young AM, Zenk S, Mason M. Measuring food availability and access in African-American communities: implications for intervention and policy. American journal of preventive medicine. 2009;36(4):S145–S150. doi: 10.1016/j.amepre.2009.01.001. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orlet Fisher J, Mitchell DC, WRIGHT HS, Birch LL. Parental influences on young girls’ fruit and vegetable, micronutrient, and fat intakes. Journal of the American Dietetic Association. 2002;102(1):58–64. doi: 10.1016/s0002-8223(02)90017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick H, Nicklas TA. A review of family and social determinants of children’s eating patterns and diet quality. Journal of the American College of Nutrition. 2005;24(2):83–92. doi: 10.1080/07315724.2005.10719448. [DOI] [PubMed] [Google Scholar]
- Poti JM, Popkin BM. Trends in energy intake among US children by eating location and food source, 1977–2006. Journal of the American Dietetic Association. 2011;111(8):1156–1164. doi: 10.1016/j.jada.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LM, Bao Y. Food prices, access to food outlets and child weight. Econ Hum Biol. 2009;7(1):64–72. doi: 10.1016/j.ehb.2009.01.004. doi: S1570-677X(09)00007-0 [pii] 10.1016/j.ehb.2009.01.004. [DOI] [PubMed] [Google Scholar]
- Powell LM, Han E, Zenk SN, Khan T, Quinn CM, Gibbs KP, Myllyluoma J. Field validation of secondary commercial data sources on the retail food outlet environment in the US. Health & Place. 2011;17(5):1122–1131. doi: 10.1016/j.healthplace.2011.05.010. [DOI] [PubMed] [Google Scholar]
- Powell LM, Nguyen BT. Fast-food and full-service restaurant consumption among children and adolescents: effect on energy, beverage, and nutrient intake. JAMA pediatrics. 2013;167(1):14–20. doi: 10.1001/jamapediatrics.2013.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saelens BE, Sallis JF, Black JB, Chen D. Neighborhood-based differences in physical activity: an environment scale evaluation. American journal of public health. 2003;93(9):1552–1558. doi: 10.2105/ajph.93.9.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: conception to adolescence. The Journal of Law, Medicine & Ethics. 2007;35(1):22–34. doi: 10.1111/j.1748-720X.2007.00111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shier V, An R, Sturm R. Is there a robust relationship between neighbourhood food environment and childhood obesity in the USA? Public health. 2012;126(9):723–730. doi: 10.1016/j.puhe.2012.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public health. 2005;119(12):1059–1068. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]
- Sturm R, Wu H. What's on the menu? A review of the energy and nutritional content of US chain restaurant menus. Public Health Nutr. 2012 May 11;:1–10. doi: 10.1017/S136898001200122X. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanielian T, Karney BR, Chandra A, SO M. The Deployment Life Study: Methodological Overview and Baseline Sample Description: RAND Corporation. 2014 [Google Scholar]
- van Ansem WJ, Schrijvers C, Rodenburg G, van de Mheen D. Is there an association between the home food environment, the local food shopping environment and children's fruit and vegetable intake? Results from the Dutch INPACT study. Public health nutrition. 2013;16(07):1206–1214. doi: 10.1017/S1368980012003461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ver Ploeg M, Mancino L, Todd JE, Clay DM, Scharadin B. Where Do Americans Usually Shop for Food and How Do They Travel To Get There? Initial Findings From the National Household Food Acquisition and Purchase Survey: Washington, DC. 2015 [Google Scholar]
- Young EM, Fors SW, Hayes DM. Associations between perceived parent behaviors and middle school student fruit and vegetable consumption. Journal of nutrition education and behavior. 2004;36(1):2–12. doi: 10.1016/s1499-4046(06)60122-x. [DOI] [PubMed] [Google Scholar]