Abstract
Adult-onset Still’s disease (AOSD) is a multisystem inflammatory disease of unknown etiology. It is characterized by arthritis, hectic fever, transient rash and visceral lesions such as pleuropericarditis, lymphadenopathy and hepato splenomegaly. Although kidney involvement may appear in some cases of AOSD, minimal glomerular lesion (MGL) has not been described. We describe a female patient, who presented with multisystemic manifestations, including high spiking fever, arthralgias, striking hyperferritinemia, and proteinuria. Renal biopsy showed classic MGL. A diagnosis of AOSD was made on the basis of Yamaguchi’s criteria. The patient was treated with steroids, resulting in remission of the rheumatological condition closely paralleled by remission of proteinuria, thereby strongly suggesting a causative link between AOSD and MGL in this patient. Renal involvement in the AOSD was rarely reported in the literature. MGL may be a cause of unexplained proteinuria in AOSD. In this situation, renal biopsy is necessary to establish a definitive diagnosis.
Keywords: Kidney involvement, minimal glomerular lesion, Still’s disease, proteinuria
Introduction
Adult-onset Still’s disease (AOSD) is a multisystem inflammatory disease of unknown etiology. It is characterized by arthritis, hectic fever, transient rash, and visceral lesions, such as pleuropericarditis, lymphadenopathy, and hepatosplenomegaly (1). Although kidney involvement may appear in some cases of AOSD, minimal glomerular lesion (MGL) has not been described. We present a patient diagnosed with AOSD who developed MGL.
Case Presentation
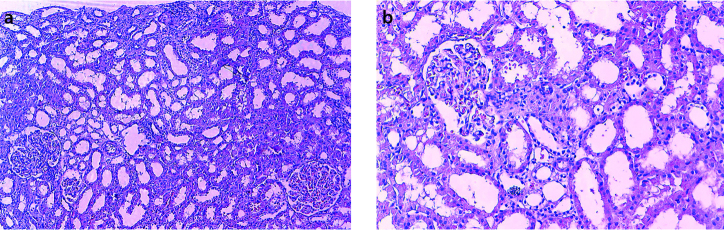
A 37-year-old woman with no notion of drug-taking presented with hectic fever, weight loss, polyarthritis, and nonitching maculopapular rash of the four limbs. Apart from fever, rash, and arthritis, the clinical examination was unremarkable. The laboratory evaluation revealed the following: hematocrit: 30.6%; hemoglobin: 10 g/dL; white blood cell count: 30 520/mm3 (neutrophils: 91.4%; lymphocytes: 5%; monocytes: 2.9%; eosinophils: 0.6%); normal platelet count; elevated erythrocyte sedimentation rate of 120 mm in the first hour; and C-reactive protein: 346 mg/L (normal, <6 mg/L). Biochemical values were as follows: urea: 0.39 g/L (14.11 mmol/L) (normal from 0.10 to 0.50 g/L [3 to 18 mmol/L]); creatinine: 8 mg/L (7040 μmol/L) (normal from 8 to 14mg/L [7040 to 12320 μmol/L]); albumin: 28.3 g/L (normal from 35 to 52 g/L); lactate dehydrogenase: 715 U/L (normal from 0 to 248 U/L); ferritin: 998 μg/L (normal from 50 to 80 μg/L); and normal liver function tests. Her coagulation profile was normal. Infectious and immunologic tests (rheumatoid factor, antinuclear antibody (ANA), anti-deoxyribonucleic acid (anti-DNA)) were negative. Proteinuria was positive on 2 occasions at 0.9 g/24 h, and urinary Bence Jones protein was absent. Kidney biopsy showed evidence of MGL (Figure 1). No other possible causes of MGL, especially hemopathy and infections, could be found in the investigations. Our patient was diagnosed as suffering from AOSD based on the criteria proposed by Yamaguchi et al. (1). She fulfilled five major criteria (fever of 39°C, arthritis, evanescent rash, leukocytosis, and pharyngitis). So, a diagnosis of AOSD with MGL nephropathy was established. The patient was treated by corticosteroids at a dose of 1 mg/kg per day with good improvement. Indeed, the arthritis and rash disappeared after 5 days. Moreover, biological inflammatory and hematological abnormalities and proteinuria normalized within 1 month and are still normal after 10 months of corticosteroids.
Figure 1.
a, b. HES ×100 (a) HES ×200 (b) glomeruli and tubes are optically normal, surrounded by a discretely interstitial inflammatory infiltrate with polymorphic elements. There is no endo- or extracapillary proliferation or abnormal deposits
Discussion
Adult-onset Still’s disease is a relatively rare multisystem disorder of unknown etiology characterized by spiking fever, arthralgias, and maculopapular evanescent rash. There are no pathognomonic signs or laboratory investigations for its diagnosis, and it is essentially a diagnosis of exclusion. Our patient was diagnosed as suffering from AOSD based on the criteria proposed by Yamaguchi et al. (1). Five criteria, including at least two major ones, after a strict exclusion process, yielded a diagnosis with 96.2% sensitivity and 92.1% specificity (1). The patient presented with all of the clinical criteria, and the exhaustive workup reasonably excluded any other diagnosis. She also had marked hyperferritinemia, which was also suggested as minor criteria, although this was later excluded due to lack of data (1). Mert et al. (2) recently reviewed 20 patients with AOSD and noted striking hyperferritinemia in 88% of the patients. Our case also met the criteria of Cush et al. (3) for diagnosing AOSD.
Kidney involvement has been rarely reported in AOSD. Mesangial glomerulonephritis, disseminated intravascular coagulation, thrombocytopenic purpura, and renal amyloidosis leading to renal insufficiency have been reported in patients with AOSD (4–8). To our knowledge, the occurrence of MGL in AOSD has not been reported previously.
Minimal glomerular lesion means normal or minimally altered glomeruli with no or minimal immune deposit. For the most part, in MGL, glomeruli appear normal, but MGL may be accompanied by a slight increase of mesangial matrix or by mesangial proliferation and thickening of the basement membrane, and there is a history of upper respiratory infection, allergy, and immunization in most cases. This lesion may be difficult to differentiate from the lesions of early stages of other forms of glomerulonephritis, including mesangioproliferative glomerulonephritis (MsPGN) and membranous glomerulonephritis, but it is regarded as a distinct entity by virtue of the characteristic age distribution, symptoms, glomerular morphology, and good response to steroids. MGL frequently occurs in children and is reported to be associated with nephrotic syndrome in 53.6% to 88% of children and 10% to 43% of all persons (9).
Clinically, MGL is typically characterized by more or less abrupt onset of nephrotic-range proteinuria with rapid progression to end-stage renal failure. Laurinavicius et al. (10) reported nephrotic-range proteinuria at the time of initial presentation in 89% of patients, with a median renal survival of 13 to 16 months. Most cases of MGL are idiopathic (or primary) and not clearly associated with an underlying disease or event. With secondary MGL, the onset of nephrotic syndrome occurs concurrently or following an extraglomerular or glomerular disease process. MGL is associated with the following: drugs, neoplasms, infections, allergy, and other glomerular diseases.
Therapeutic decisions should be based upon the extent and severity of organ system involvement. The principal options for treatment are nonsteroidal anti-inflammatory drugs (NSAIDs), glucocorticoids, biologic agents, and disease-modifying antirheumatic drugs (DMARDs). Salicylates, once a mainstay of juvenile idiopathic arthritis therapy, are now seldom used to treat AOSD, because their therapeutic index is narrower than that of most NSAIDs.
As a general approach, we suggest starting treatment with an NSAID but moving quickly to glucocorticoids, followed by biologic agents, if AOSD does not come under control (10). Patients who are on the sicker end of the AOSD spectrum should be treated with glucocorticoids from the outset of therapy, followed by biologic agents if the disease proves refractory. DMARDs now generally play an adjunctive role in the treatment of AOSD. Methotrexate is often used in conjunction with biologic therapies. To date, no therapy has been shown to be effective in this condition. So far, the published literature is limited and is in the form of retrospective and uncontrolled analyses. Variable outcomes with respect to renal survival have been observed, with regimens consisting of steroids, with or without cyclophosphamide or cyclosporine (10).
Our patient, who was maintained on low-dose prednisone, continues to be in remission with respect to renal function and AOSD. Interestingly, steroid therapy for AOSD resulted in the induction of remission of AOSD, as well as of the proteinuria, in our patient with MGL, which otherwise has an aggressive course and poor prognosis, thereby strongly suggesting a causal link between AOSD and MGL. Both AOSD and MGL are relatively uncommon diseases with an unclear etiopathogenesis.
As a conclusion, renal involvement in AOSD id rarely reported in the literature. MGL may be a cause of the unexplained proteinuria in AOSD. In this situation, renal biopsy is necessary to establish a definitive diagnosis.
Footnotes
Ethics Committee Approval: N/A.
Informed Consent: Written informed consent was obtained from the patient.
Peer-review: Externally peer-reviewed.
Author contributions: Concept - I.E., F.A.; Design - I.E.; Supervision - F.A.; Resource - F.A.; Materials - I.E.; Data Collection&/or Processing - I.E.; Analysis&/or Interpretation - F.A.; Literature Search - I.E.,N.G.; Writing - I.E.; Critical Reviews - T.H.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y, Kashiwagi H, et al. Preliminary criteria for classification of adult Still’s disease. J Rheumatol. 1992;19:424–30. [PubMed] [Google Scholar]
- 2.Mert A, Ozaras R, Tabak F, Bilir M, Ozturk R, Ozdogan H, et al. Fever of unknown origin: a review of 20 patients with adult-onset Still’s disease. Clin Rheumatol. 2003;22:89–93. doi: 10.1007/s10067-002-0680-3. http://dx.doi.org/10.1007/s10067-002-0680-3. [DOI] [PubMed] [Google Scholar]
- 3.Cush JJ, Medsger TA, Jr, Christy WC, Herbert DC, Cooperstein LA. Adult-onset Still’s disease. Clinical course and outcome. Arthritis Rheum. 1987;30:186–94. doi: 10.1002/art.1780300209. http://dx.doi.org/10.1002/art.1780300209. [DOI] [PubMed] [Google Scholar]
- 4.Wendling D, Humbery Ph, Hory B, Blanc D, Dupond JL, Guidet M. The kidney in Still’s disease in adults. Rev Rheum Mal Osteoartic. 1989;56:325–7. [PubMed] [Google Scholar]
- 5.Portolés J, de Tomás E, Espinosa A, Gallego E, Nieva GS, Blanco J. Thrombotic thrombocytopenic purpura and acute renal failure in adult Still’s disease. Nephrol Dial Transplant. 1997;12:1471–3. doi: 10.1093/ndt/12.7.1471. http://dx.doi.org/10.1093/ndt/12.7.1471. [DOI] [PubMed] [Google Scholar]
- 6.Diamond JR. Hemolytic uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP) complicating adult Still’s disease: Remission induced with intravenous immunoglobulin G. J Nephrol. 1997;10:253–7. [PubMed] [Google Scholar]
- 7.Perez MG, Rodwig FR., Jr Chronic relapsing thrombotic thrombocytopenic purpura in adult onset Still’s disease. South Med J. 2003;96:46–9. doi: 10.1097/01.SMJ.0000047763.56451.F0. http://dx.doi.org/10.1097/01.SMJ.0000047763.56451.F0. [DOI] [PubMed] [Google Scholar]
- 8.Rivera F, Gill CM, Gill MT, Battle-Gualda E, Trigueros M, Olivares J. Vascular renal AA amyloidosis in adult Still’s disease. Nephrol Dial Transplant. 1997;12:1714–6. doi: 10.1093/ndt/12.8.1714. http://dx.doi.org/10.1093/ndt/12.8.1714. [DOI] [PubMed] [Google Scholar]
- 9.Zollinger HU, Mihatsch MJ. Renal Pathology in biopsy. Springer-Verlag; Berlin: 1978. Glomerular minimal change; pp. 367–79. http://dx.doi.org/10.1007/978-3-642-66731-2. [Google Scholar]
- 10.Laurinavicius A, Hurwtiz S, Renke HG. Collapsing glomerulopathy in HIV and non-HIV patients: A clinicopathological and follow up study. Kidney Int. 1999;56:2203–13. doi: 10.1046/j.1523-1755.1999.00769.x. http://dx.doi.org/10.1046/j.1523-1755.1999.00769.x. [DOI] [PubMed] [Google Scholar]