Abstract
Tuberculosis remains one of the most common infectious diseases in the world. Vertebral tuberculosis is the commonest form of bone and joint tuberculosis; however, isolated sacral tuberculosis is rare. This atypical presentation may lead to a delay in diagnosis and treatment. We report three cases of sacral tuberculosis diagnosed in young women, aged 30, 23, and 35 years old, respectively. Lombosciatic pain was the main symptom in all cases. All patients had a biological assessment, plain radiographs, and CT scan. However, magnetic resonance imaging was done in only two cases. All patients underwent surgical sacral biopsy, and the diagnosis of tuberculosis was confirmed by histology in all cases. The evolution was satisfactory with the adjunction of antituberculous chemotherapy in all cases. Spinal tuberculosis should be the first and foremost differential diagnosis in the presence of atypical clinical and radiological features of a sacral lesion, particularly in developing countries. Early diagnosis and treatment could prevent or minimize the neurological morbidity in such cases.
Keywords: Sacral, tuberculosis, antibacillary chemotherapy
Introduction
Tuberculosis can affect any bone and joint structures of the body. Osteoarticular tuberculosis (OAT) represents 2% to 5% of all cases of tuberculosis and 11% to 15% of extrapulmonary tuberculosis (1). The principal location of the OAT is the spinal cord, which represents approximately 50% of cases affecting more often dorsolumbar vertebrae (2). Isolated tuberculosis of the sacrum is rarely reported in the literature, which leads to a delay in diagnosis and subsequently persistence of a normally curable disease. We report three cases.
Case Presentations
Case 1
A 30-year-old woman presented with right inflammatory lombo-sciatic pain that worsened 2 months before, with an undetermined weight loss. Clinical examination revealed stiffness of the lumbosacral spine without neurological deficit. Laboratory tests showed an ESR at 90 mm at the first hour and C-reactive protein (CRP) at 45 mg/L. Other biologic parameters were normal. The tuberculin skin test was positive at 15 mm. The search for Koch’s bacillus in the sputum and urine was negative. Chest x-ray was normal. The pelvis radiographs showed an osteolytic lesion of the sacrum that extended to the right sacroiliac joint. Computed tomography confirmed the existence of an osteolytic lesion with a pelvic collection. Magnetic resonance imaging (MRI) showed the presence of sacroiliitis with fluid collection localized in the sacral and iliac bones and adjacent soft gluteal tissues (Figure 1). Histological study of the sacral biopsy found caseo-follicular tuberculosis. The patient was treated with antibacillary chemotherapy for a period of 9 months. After achieving treatment, the evolution was marked by clinical and biological improvement, with normalization of inflammatory parameters.
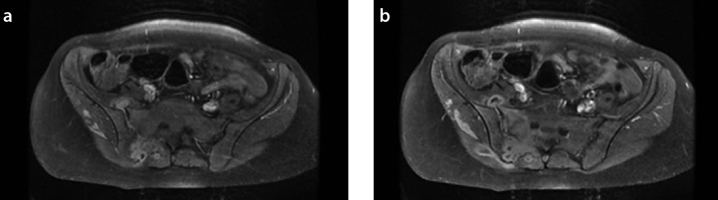
Figure 1.
a, b. T1-weighted axial MR images of the pelvic after gadolinium injection show sacral and presacral abscess
Case 2
A 23-year-old woman had complained since 5 months of left S1 lombosciatic pain, fever, night sweats, and weight loss of 20 kg. Clinical examination found lumbar stiffness with no signs of neurological deficit. Laboratory tests showed an ESR at 75 mm at the first hour and CRP at 60 mg/L. Other biologic parameters were normal. The tuberculin skin test was positive at 18 mm. The search for Koch’s bacillus in the sputum was negative. Chest x-ray was normal. Radiographs of the pelvis were unremarkable. CT scan revealed pre-sacral and retro-acetabular abscessed collections with lytic lesions of the vertebral body of S2. Pelvic MRI objectived collections fusing to the sacral and left buttock (Figure 2). The patient underwent surgical drainage of the collections and a sacral biopsy. Histological examination showed an epithelioid granuloma with giant cells and caseous necrosis. Anti-bacillary chemotherapy was prescribed for a period of 9 months. The evolution after 4 months of treatment was marked by the regression of low back pain, radicular pain, and normalization of biologic parameters.
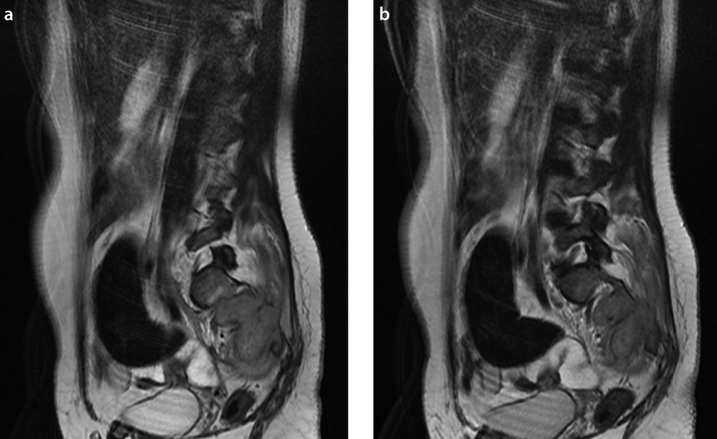
Figure 2.
a, b. Axial (a) and coronal (b) T1-weighted MR images of the pelvic show a hyperintense sacral lesion
Case 3
A 35-year-old woman complained of right lombosciatic pain lasting for 1 year without neurological deficit on clinical examination. Laboratory tests showed hemoglobin at 8.7 g/dL, ESR at 25 mm at the first hour, and CRP at 20 mg/L. No other biologic anomaly was noted. The tuberculin skin test was positive at 16 mm. Chest x-ray was normal. CT scan of the pelvis showed a right sacral lytic lesion that extended to the sacral canal (Figure 3). Histological examination revealed a caseous granuloma and multinucleated giant cells. The patient received anti-bacillary chemotherapy for a period of 1 year, with significant clinical and biological improvement.
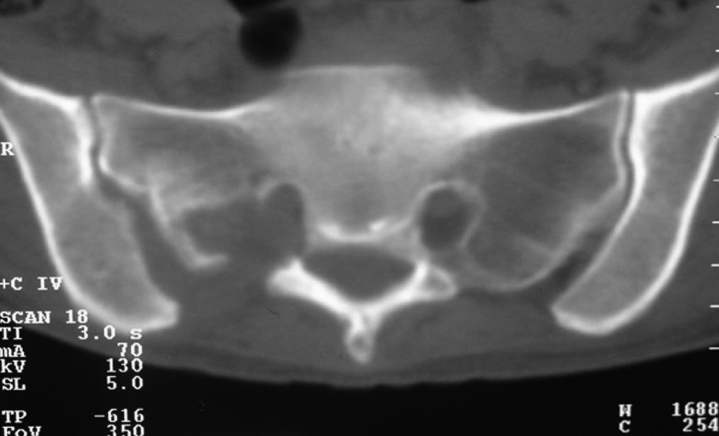
Figure 3.
Contrasted-enhanced CT scan of the sacrum showing destruction of the first right sacral foramen with abscess surrounding the lesion
Discussion
Tuberculosis is a major health problem in Morocco and other developing countries. Tuberculosis of the spine is a disease of antiquity but was not fully described until 1779 by Percival Pott (3). OAT represents about 3% of all tuberculosis and 15% of extrapulmonary tuberculosis (1). Spinal location is at least 50% of cases and sits at the thoracolumbar spine in 80% of cases (4). Isolated tuberculosis of the sacrum is rarely reported in the literature, with a frequency estimated at 5% by Pertuiset et al. (5). In a review of 63 cases of spinal tuberculosis by Lindahl et al. (6), sacral involvement was found in just four cases, while none was involved in 107 patients in the series of Lifeso et al. (7). Spinal tuberculosis is often due to hematogenous spread of mycobacteria from primary foci in the lung and/or genitourinary tract (3). It is widely believed that the paravertebral venous plexus of Batson provides the primary pathway for dissemination of the tuberculous bacilli into the vertebral column. It is also possible that lymphatic drainage of the pleura or kidney may involve the para-aortic lymph nodes, which may secondarily involve the vertebrae (3, 4). Clinical manifestations of sacral tuberculosis depend primarily on the age of the patient. Young individuals tend to present with discharging sinuses and abscesses, while backache is a dominant clinical feature in adults. The deficit and radicular symptoms are less common, because the sacral nerve roots are protected by bone (3, 8). Magnetic resonance imaging is the most sensitive diagnostic radiologic imaging, and the radiological spectrum of spinal tuberculosis has been well reported in the literature. MRI of the sacrum usually reveals diffuse marrow edema that is hypointense on T1- and hyperintense on T2-weighted images (9, 10). The tubercular lesions may be misinterpreted with other infectious diseases or neoplasms in MRI. This can be a source of diagnostic delays and errors (10, 11). CT is useful for imaging cortical bone. However, the early marrow changes in the vertebrae that precede the more gross erosive changes are difficult to visualize. Plain radiographs are extremely insensitive and do not detect vertebral involvement until at least 50% of a vertebra is destroyed. Similarly, bone scans are notably prone to miss this disease (3, 10).
Surgical biopsy poses diagnosis of certainty tuberculosis by a pathological study. This surgical biopsy was performed in all our patients (8, 10). Regarding treatment of spinal tuberculosis, various chemotherapy protocols have been proposed; many workers prescribe chemotherapy for 6 months, while some continue it for 9 to 12 months (12). Excellent response of vertebral tuberculosis to multi-drug therapy prevents the need for surgical management.
Surgery may be necessary because of signs of neurological compression during extensive destruction of several vertebral bodies with spinal deformity or to evacuate an abscess that is resistant to medical treatment. The prognosis of sacral tuberculosis is good, if a rapid and correct diagnosis is made and adequate treatment is provided (13, 14). This pathology should always be suspected in any process of the lytic sacrum, especially in endemic areas of tuberculosis, to prevent or at least reduce the morbidity of this disease, which is generally curable.
Isolated sacral tuberculosis is exceptional and often causes a delay in diagnosis. It should always be suspected in any process of the lytic sacrum, especially in endemic areas of tuberculosis, to prevent or at least reduce the morbidity of this disease, which is generally curable.
Footnotes
Ethics Committee Approval: N/A.
Informed Consent: Written informed consent was obtained from the patient.
Peer-review: Externally peer-reviewed.
Author contributions: Concept - F.L., F.E.E.; Design - F.L.; Supervision - F.E.A.; Resource - F.E.; Materials - M.B.; Data Collection&/or Processing - F.L.; Analysis&/or Interpretation - F.E.A., M.B.; Literature Search - F.L., F.E.E.; Writing - F.L.; Critical Reviews - T.H.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Pertuiset E. Peripheral bone and joint tuberculosis. EMC-Rhumatologie Orthopédie. 2004;1:463–86. http://dx.doi.org/10.1016/j.emcrho.2004.08.00. [Google Scholar]
- 2.Shantanu K, Sharma V, Kumar S, Jain S. Tuberculosis of sacrum mimicking as malignancy. BMJ Case Rep. 2012 doi: 10.1136/bcr.07.2011.4505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patankar T, Krishnan A, Patkar D, Kale H, Prasad S, Shah J, et al. Imaging in isolated sacral tuberculosis: a review of 15 cases. Skeletal Radiol. 2000;29:392–6. doi: 10.1007/s002560000229. http://dx.doi.org/10.1007/s002560000229. [DOI] [PubMed] [Google Scholar]
- 4.Bezer M, Kucukdurmaz F, Aydin N, Kocaoglu B, Guven O. Tuberculous spondylitis of the lumbosacral region: long-term follow-up of patients treated by chemotherapy, transpedicular drainage, posterior instrumentation, and fusion. J Spinal Disord Tech. 2005;18:425–9. doi: 10.1097/01.bsd.0000171627.11171.6f. http://dx.doi.org/10.1097/01.bsd.0000171627.11171.6f. [DOI] [PubMed] [Google Scholar]
- 5.Pertuiset E, Beaudreuil J, Lioté F, Horusitzky A, Kemiche F, Richette P, et al. Spinal tuberculosis in adults: A study of 103 cases in a developed country, 1980–1994. Medicine. 1999;78:309–20. doi: 10.1097/00005792-199909000-00003. http://dx.doi.org/10.1097/00005792-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Lindahl S, Nyman RS, Brismar J, Hugosson C, Lundstedt C. Imaging of tuberculosis. IV. spinal manifestations in 63 patients. Acta Radiol. 1996;37:506–11. doi: 10.1177/02841851960373P215. http://dx.doi.org/10.3109/02841859609175433. [DOI] [PubMed] [Google Scholar]
- 7.Lifeso RM, Weaver P, Harder EH. Tuberculosis spondylitis in adults. J Bone Joint Surg Am. 1985;67:1405–13. [PubMed] [Google Scholar]
- 8.Kumar A, Varshney MK, Trikha V. Unusual presentation of isolated sacral tuberculosis. Joint Bone Spine. 2006;73:751–2. doi: 10.1016/j.jbspin.2006.01.016. http://dx.doi.org/10.1016/j.jbspin.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 9.Kim NH, Lee HM, Suh JS. Magnetic resonance imaging for the diagnosis of tuberculous spondylitis. Spine. 1994;19:2451–5. doi: 10.1097/00007632-199411000-00016. http://dx.doi.org/10.1097/00007632-199411000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Wellons JC, Woods CW, Eastwood JD, Woods CW, Lawson WT, Eastwood JD. Sacral tuberculosis: a case report and review of the literature. Surg Neurol. 2004;61:136–41. doi: 10.1016/s0090-3019(03)00265-9. http://dx.doi.org/10.1016/S0090-3019%2803%2900265-9. [DOI] [PubMed] [Google Scholar]
- 11.Burrill J, Williams C, Bain G, Conder G, Hine AL, Misra RR. Tuberculosis: a radiologic review. Radiographics. 2007;27:1255–73. doi: 10.1148/rg.275065176. http://dx.doi.org/10.1148/rg.275065176. [DOI] [PubMed] [Google Scholar]
- 12.Punia VPS, Kumar S. Atypical manifestation of sacral tuberculosis as cauda-conus syndrome. JIACM. 2008;9:57–60. [Google Scholar]
- 13.Bouajina E, Harzallah L, Hachfi W, Slama KB, Rammeh N, Ghannouchi M, et al. Tuberculous sacro-iliitis: a series of twenty-two cases. Rev Med Interne. 2005;26:690–4. doi: 10.1016/j.revmed.2005.03.009. http://dx.doi.org/10.1016/j.revmed.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 14.López-Sánchez MC, CalvoArrojo G, Vázquez-Rodríguez TR. Tuberculousspondylodiskitis with lumbar tumor. Reumatol Clin. 2012;08:292–3. doi: 10.1016/j.reuma.2011.10.011. http://dx.doi.org/10.1016/j.reuma.2011.10.011. [DOI] [PubMed] [Google Scholar]