Abstract
Background:
Revision anterior cruciate ligament (ACL) reconstruction surgery occurs in 5% to 15% of individuals undergoing ACL reconstruction. Identifying predictors for revision ACL surgery is of essence in the pursuit of creating adequate prevention programs and to identify individuals at risk for reinjury and revision.
Purpose:
To determine predictors of revision ACL surgery after failed primary ACL reconstruction.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
A total of 251 participants (mean age ± SD, 26.1 ± 9.9 years) who had undergone primary ACL reconstruction 1 to 5 years earlier completed a comprehensive survey to determine predictors of revision ACL surgery at a mean 3.4 ± 1.3 years after the primary ACL reconstruction. Potential predictors that were assessed included subject characteristics (age at the time of surgery, time from injury to surgery, sex, body mass index, preinjury activity level, return to sport status), details of the initial injury (mechanism; concomitant injury to other ligaments, menisci, and cartilage), surgical details of the primary reconstruction (Lachman and pivot shift tests under anesthesia, graft type, femoral drilling technique, reconstruction technique), and postoperative course (length of rehabilitation, complications). Univariate and multivariate logistic regression analyses were performed to identify factors that predicted the need for revision ACL surgery.
Results:
Overall, 21 (8.4%) subjects underwent revision ACL surgery. Univariate analysis showed that younger age at the time of surgery (P = .003), participation in sports at a competitive level (P = .023), and double-bundle ACL reconstruction (P = .024) predicted increased risk of revision ACL surgery. Allograft reconstructions also demonstrated a trend toward greater risk of revision ACL surgery (P = .076). No other variables were significantly associated with revision ACL surgery. Multivariate analysis revealed that revision ACL surgery was only predicted by age at the time of surgery and graft type (autograft vs allograft).
Conclusion:
The overall revision ACL surgery rate after primary unilateral ACL reconstruction was 8.4%. Univariate predictors of revision ACL reconstruction included younger age at the time of surgery, competitive baseline activity level, and double-bundle ACL reconstruction. However, multivariable logistic regression analysis indicated that age and reconstruction performed with allograft were the only independent predictors of revision ACL reconstruction.
Keywords: anterior cruciate ligament, ACL, surgery, revision, graft failure
The occurrence of anterior cruciate ligament (ACL) injuries has significantly increased in recent years. It is estimated that approximately 250,000 to 300,000 ACL injuries occur in the United States annually.11 Approximately 75,000 to 100,000 ACL reconstructions are performed,12 which makes it one of the most common procedures in orthopaedic surgery.7 The surgical technique has evolved considerably since its inception; however, the rates of clinical success in terms of knee stability and abnormal International Knee Documentation Committee (IKDC) scores are still between 80% and 95%.12 Even though research on ACL reconstruction is extensive, the optimal surgical technique is yet not universally accepted.
An important clinical outcome after ACL reconstruction is graft failure, and according to recent studies, varying rates of graft failure and revision ACL surgery have been reported (0%-14%).13,26,28,31 Factors that predict revision ACL surgery after failed primary ACL reconstruction are not well defined, and there is inconsistency in terms of these factors in the literature. Some factors that predict revision ACL surgery have been identified by other researchers. These include lower age, smoking, and activity level at the time of initial injury.1,3
The main purpose of this study was to identify predictors of revision ACL surgery after failed primary ACL reconstruction. We hypothesized that younger individuals and higher activity level will predict graft failure.
Methods
This study was approved by the University of Pittsburgh Institutional Review Board using an expedited review process (IRB Protocol Number PRO11120006).
Subjects
A medical records review between January 1, 2007 and April 30, 2011 was performed to identify skeletally mature eligible subjects between 14 and 50 years of age at the time of primary unilateral ACL reconstruction. Subjects with concomitant meniscus (medial, 33%; lateral, 43%), ligament (medical collateral, 8%; lateral collateral, 1%; posterior cruciate, 0%), or cartilage (patella, 13%; trochlea, 8%; medial femur, 16%; lateral femur, 14%; medial tibia, 7%; lateral tibia, 9%) injury were included and surgically addressed according to the surgeon’s opinion. Subjects who had prior injury or surgery to either knee were excluded. All surgeries were performed by 5 expert surgeons.
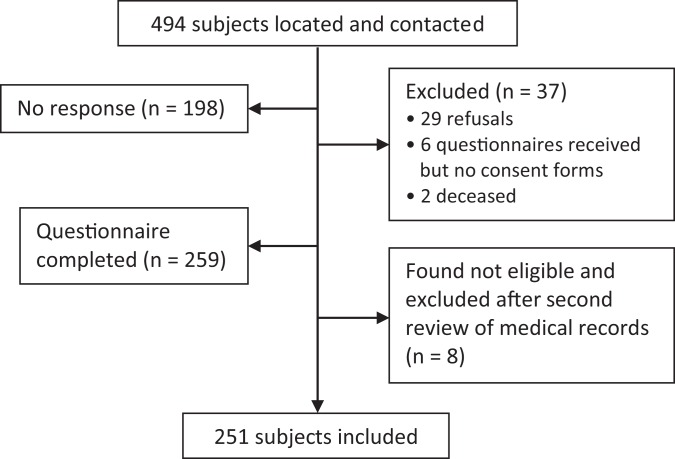
Of the 797 potential subjects identified by the medical records, we were able to locate and contact 494 subjects, of which 251 were included in this survey (Figure 1).
Figure 1.
Flow diagram of subject recruitment process.
Nonresponders were younger (21.1 ± 8.3 years) than those who responded (26.1 ± 9.9 years; P < .001) and more likely to be male (60% male vs 40% female) (P < .001) (Table 1).
TABLE 1.
Demographics for Those Who Did and Did Not Respond to the Questionnairea
| Nonresponders (n = 206)b | Responders (n = 251) | Refused (n = 29) | P | |
|---|---|---|---|---|
| Age at surgery, y | 21.1 ± 8.3 | 26.1 ± 9.9 | 27.6 ± 11.5 | <.001 |
| Female patients | 83 (40.3) | 139 (55.4) | 17 (58.6) | <.001 |
| Follow-up, y | 2.9 ± 1.1 | 3.4 ± 1.3 | 3.1 ± 1.1 | .269 |
aValues are presented as mean ± SD or n (%).
bNonresponder group includes no response to invitation, returned questionnaire without consent, and deceased.
The mean age (±SD) of included subjects at the time of surgery was 26.1 ± 9.9 years; 139 subjects were female, and their mean length of follow-up was 3.4 ± 1.3 years (Table 1). The median time from injury to surgery was approximately 2 months.
Participants were arbitrarily placed into different subgroups based on their age at the time of surgery: ≤18 years, 19 to 23 years, or ≥24 years. Competitive sports participation was operationally defined as participation in strenuous sports activities that involve jumping, cutting, and hard pivoting (eg, football, soccer, basketball, volleyball, and gymnastics) or moderate sports activities that involve running, twisting, and turning (eg, tennis, racquetball, handball, ice hockey, field hockey, skiing, and wrestling) 4 to 7 times per week, with a minimum total Marx Activity Scale score of 12.
Procedures
Letters of invitation along with a consent form and survey were sent to all potential subjects using a 3-phase mailing procedure. To maximize response rate, invitation letters were followed by a postcard reminder, 2 additional letters, and 2 phone calls to nonrespondents. Subjects were asked to report their pre- and postsurgical levels of sports activity and participation. Predictors of revision ACL surgery were identified from subject characteristics (age at time of surgery, time from injury to surgery, sex, body mass index [BMI], preinjury activity level, return to sport status), details of the initial injury (mechanism; concomitant injury to other ligaments, menisci, and cartilage), surgical details of the primary reconstruction (Lachman and pivot shift tests under anesthesia, graft type, femoral drilling technique, reconstruction technique), and postoperative course (length of rehabilitation, complications) that were extracted from the questionnaire and medical records. All patients followed a standardized postoperative rehabilitation program, and return to sports occurred 9 to 12 months after surgery.
ACL Revision Outcome
The outcome of revision ACL surgery was determined by asking subjects to report any additional injuries or surgeries to the reconstructed knee, including revision ACL surgery. A reported revision ACL surgery was confirmed by evaluating the subject’s medical records.
Data Analysis
Descriptive statistics were calculated and summarized for all variables. This included frequency counts and percentages for nominal variables and measures of central tendency (means, medians) and dispersion (standard deviations, ranges) for continuous variables. Independent t tests and chi-square tests were used to evaluate the differences in demographic variables between subjects who responded and those who did not respond to the invitations to participate in the study. Univariate logistic regression analyses were performed for all variables to identify factors that increased the risk of revision ACL surgery. Variables with P value <.25 (rule of thumb) were entered in a multivariate stepwise logistic regression model to determine the best predictors for revision ACL surgery taking into account other predictor variables in the model. Odds ratios (ORs) and 95% CIs were estimated. An alpha level of <0.05 was considered statistically significant. All statistical analyses were performed using SPSS (version 22.0; IBM Corp).
Results
Of the 251 subjects, 21 (8.4%) reported that they had undergone revision ACL surgery after their primary unilateral ACL reconstruction. Of those, 18 subjects were injured during sports participation. Predictors of revision surgery after ACL reconstruction, such as age, sex, BMI, time from injury to surgery, baseline activity level, graft type, and surgical technique, are described in Table 2.
TABLE 2.
Univariate Logistic Regression Model for Predictors of Revision ACL Surgery After Primary ACL Reconstructiona
| Predictor | Revision ACL Surgery, n (%) | OR | 95% CI | P |
|---|---|---|---|---|
| Age at surgery | ||||
| ≤18 y (n = 78) | 11 (14.1) | 9.52 | 2.05-44.26 | .004 |
| 19-23 y (n = 55) | 8 (14.5) | 9.87 | 2.02-48.22 | .005 |
| ≥24 yb (n = 118) | 2 (1.7) | |||
| Sex | ||||
| Femaleb (n = 139) | 13 (9.4) | |||
| Male (n = 112) | 18 (16.1) | 1.34 | 0.54-3.36 | .527 |
| BMI, kg/m2 (mean ± SD) | 25.15 ± 4.47 | 0.96 | 0.86-1.07 | .434 |
| Time from injury to surgery | ||||
| <6 mob (n = 210) | 20 (9.5) | 0.27 | 0.04-2.08 | .129 |
| ≥6 mo (n = 41) | 1 (2.4) | |||
| Baseline activity level | ||||
| Competitive (n = 147) | 17 (11.6) | 3.27 | 1.07-10.02 | .023 |
| Otherb (n = 104) | 4 (3.9) | |||
| Graft type | ||||
| Autograftb (n = 131) | 7 (4.7) | |||
| Allograft (n = 110) | 13 (11.1) | 2.37 | 0.91-6.18 | .076 |
| Mixed (n = 10) | 1 (10) | .189 | ||
| Surgical technique | ||||
| Single-bundleb (n = 196) | 11 (5.6) | |||
| Double-bundle (n = 55) | 9 (16.4) | 3 | 1.19-7.55 | .024 |
| Return to sports | ||||
| Nob (n = 42) | 2 (4.8) | 2 | 0.45-8.93 | .324 |
| Yes (n = 209) | 19 (9.1) |
aBoldfaced P values indicate statistical significance. ACL, anterior cruciate ligament; BMI, body mass index; OR, odds ratio.
bReference group for each predictor.
Univariate Analyses
In the univariate logistic regression model, participants who had revision ACL surgery had a significantly increased risk of being 18 years or younger (OR, 9.5; P = .004) or 19 to 23 years of age (OR, 9.9; P = .005) compared with 24 years or older. Time from injury to primary ACL reconstruction was divided into 2 categories: less than 6 months (n = 210) and 6 months or longer (n = 41). No difference was found in reported graft failure frequency between the 2 groups. Moreover, BMI and sex were not significantly associated with increased risk of revision ACL surgery. Based on graft type, the difference in the risk for revision ACL surgery (autograft, 4.7%; allograft, 11.1%; mixed, 10%) was not significant (autograft vs allograft, P = .076; autograft vs mixed, P = .189). There were no differences in revision ACL rate between those who returned to sports and those who did not (Table 2).
Subjects were divided into 2 groups with regard to activity level: competitive athletes (n = 147) and other (n = 104). Those who participated in competitive sports activities prior to surgery had a significant increased risk of undergoing revision ACL surgery compared with those who participated at other activity levels prior to surgery (OR, 3.3; P = .023).
Patients who underwent primary double-bundle ACL reconstruction (n = 55) had a significantly increased risk of undergoing revision ACL reconstruction compared with those who underwent primary single-bundle ACL reconstruction (n = 196) (OR, 3.0; P = .024) (Table 2). In further analysis, the combination of use of allograft and double-bundle ACL reconstruction had the highest frequency of revision (18.4%) (Table 3).
TABLE 3.
Correlation Between Graft Type and Surgical Technique by Revision ACL Surgerya
| Graft Type | Surgical Technique | Total | |
|---|---|---|---|
| Single-Bundle | Double-Bundle | ||
| Autograft | 7/135 (5.2) | 0/6 (0) | 7/141 |
| Allograft | 4/61 (6.6) | 9/49 (18.4) | 13/110 |
| Total | 11/196 | 9/55 | |
aData are presented as n/total (%). ACL, anterior cruciate ligament.
Furthermore, patients who had double-bundle ACL reconstruction were predominantly of younger age, and a higher proportion participated at a competitive baseline activity level (Table 4); the same applies for patients who underwent double-bundle ACL reconstruction with allograft (Table 5).
TABLE 4.
Correlation Between Age at Surgery, Surgical Technique, and Baseline Activity Level by Revision ACL Surgerya
| Baseline Activity Level | Age at Surgery | Total | ||
|---|---|---|---|---|
| ≤18 y | 19-23 y | ≥24 y | ||
| Competitive | ||||
| Single-bundle | 6/54 (9.3) | 4/35 (11.4) | 0/25 (0) | 10/114 (8.8) |
| Double-bundle | 5/21 (23.8) | 2/9 (22.2) | 0/3 (0) | 7/33 (21.2) |
| Other | ||||
| Single-bundle | 0/2 (0) | 1/9 (11.1) | 1/71 (1.4) | 2/82 (2.4) |
| Double-bundle | 0/1 (0) | 1/2 (50) | 1/19 (5.3) | 2/22 (9.1) |
aData are presented as n/total (%). ACL, anterior cruciate ligament.
TABLE 5.
Correlation Between Age at Surgery, Surgical Technique, and Baseline Activity Level by Revision ACL Surgery in Subjects With Allograft Reconstructiona
| Baseline Activity Level | Age at Surgery | Total | ||
|---|---|---|---|---|
| ≤18 y | 19-23 y | ≥24 y | ||
| Competitive | ||||
| Single-bundle | 2/8 (25) | 2/5 (40) | 0/9 (0) | 4/22 (18.2) |
| Double-bundle | 5/17 (29.4) | 2/9 (22.2) | 0/3 (0) | 7/29 (24.1) |
| Other | ||||
| Single-bundle | 0/1 (0) | 0/2 (0) | 0/36 (0) | 0/39 (0) |
| Double-bundle | 0/1 (0) | 1/2 (50) | 1/17 (5.3) | 2/20 (10) |
aData are presented as n/total (%). ACL, anterior cruciate ligament.
None of the other variables, including mechanism of injury (sport vs other) (P = .476); concomitant injury to the meniscus, other ligaments, or cartilage (P = .366); Lachman (P = .757) and pivot shift under anesthesia (P = .793); femoral drilling technique (transtibial [16%] vs medial portal [84%]) (P = .585); length of rehabilitation (P = .118); and complications after primary ACL reconstruction surgery (P = .677) were found to be predictors for revision ACL surgery.
Multivariate Analyses
In the multivariate logistic regression model, participants who were 18 years or younger had a significantly increased risk of revision ACL surgery compared with individuals 24 years or older (OR, 11.5; P = .001). Moreover, there was a significantly increased risk of revision ACL surgery in patients between 19 and 23 years of age compared with 24 years or older (OR, 12.9; P = .003) (Table 6).
TABLE 6.
Multivariate Logistic Regression Model for Predictors of Revision ACL Surgery After Primary ACL Reconstructiona
| Predictor | β | SE | OR | 95% CI | P Value |
|---|---|---|---|---|---|
| Age at surgery | |||||
| ≤18 vs ≥24b y | 2.44 | 0.84 | 11.46 | 2.24-58.87 | .001 |
| 19-23 vs ≥24b y | 2.56 | 0.88 | 12.94 | 2.32-72.07 | .003 |
| Graft type | |||||
| Autograftb vs allograft | 1.32 | 0.51 | 3.75 | 1.38-10.22 | .010 |
aACL, anterior cruciate ligament; OR, odds ratio; SE, standard error.
bReference group for each predictor.
Additionally, the multivariate logistic regression model indicated that when other variables in the model were also considered, participants who underwent primary ACL reconstruction with allograft in comparison with autograft had a significantly increased risk for revision ACL (OR, 3.8; P = .010) (Table 6).
Discussion
The main finding of this study was that younger individuals at the time of primary ACL reconstruction and ACL reconstruction with allograft predicted significantly increased risk of revision ACL surgery. This is consistent with previous studies where young age has been associated with a greater risk of revision surgery.2,15,17–19,22,37 In addition to the assumed increased activity in younger patients, the reason for this could also be that they are less compliant in terms of rehabilitation and had an earlier return to pivoting sports. These active lifestyle differences are difficult to assess and evaluate if they are true confounders, and there is no available evidence to date to support or negate these often used suggestions. However, it appears reasonable that subjects who are younger have a different active lifestyle compared with subjects who are a decade older, have full-time employment, and may have started a family.
The overall revision ACL rate after primary ACL reconstruction in the present study was 8.4%, which is in the reported range found in the literature (0%-14%).5,13,26 Newer registry studies from Scandinavia that included a large number of individuals, however, report relatively low frequencies of revision ACL reconstruction (1.6%-5.16%).15,22,24 The reason for the greater revision frequencies in this study is a potential selection bias in the included cohort and general differences in activity level and patient cohorts between this cross-sectional study and the cohorts used in the Scandinavian Knee Ligament Register reports.
Baseline activity level appears to be a predictor of revision ACL surgery in the present study. Patients who participated in competitive sports activities prior to primary ACL reconstruction had an increased risk of undergoing revision compared with those who were noncompetitive athletes. This is both reasonable and logical due to the fact that competitive sports not only means that the subject might exercise more often but is also exposed to more intense situations.
A multivariate logistic regression model found that allograft was an inferior graft choice in terms of revision ACL frequency compared with autograft. This is not only in line with most previous studies in this area27 but also biomechanically and histologically reasonable. Moreover, previous studies found that ACL reconstruction with allograft combined with an early return to sports was a risk factor for graft failure.6,14,30
A little surprising, the univariate analysis showed that double-bundle ACL reconstruction was associated with a greater risk of revision ACL reconstruction. This finding is not consistent with other high-quality studies reporting the outcome of double-bundle ACL reconstruction. For instance, Tiamklang et al34 found 6 studies presenting data on graft failure in their Cochrane meta-analysis, and there was no significant difference between double- and single-bundle ACL reconstruction. Moreover, Björnsson et al5 found a trend toward fewer reruptures, and Suomalainen et al32,33 found significantly fewer graft failures and subsequent revision ACL surgery after double-bundle ACL reconstruction than after single-bundle surgeries at 5-year follow-up.
Further analysis of the results in the present study revealed that the increased risk for revision ACL surgery for those undergoing double-bundle ACL reconstruction was likely confounded by the fact that a larger proportion of patients who underwent double-bundle reconstruction underwent surgery with allograft compared with those who underwent single-bundle reconstruction. Additionally, those who underwent double-bundle ACL reconstruction were also younger and had an increased baseline activity level. All these factors could have contributed to the increased risk of revision ACL reconstruction for those who underwent double-bundle ACL reconstruction. This contention is supported by the findings of the multivariable analysis, which indicated that after controlling for the effects of age and graft type, double-bundle ACL reconstruction was no longer an independent predictor of revision ACL reconstruction.
An increased risk of primary ACL injuries in women has been reported in several earlier studies.9,23,25,35 In the present study, there was no effect for sex with respect to the risk of revision, which is in accordance with previous studies.# It is possible that different anatomy, biomechanics, and neuromuscular control20,21 after ACL reconstruction overrule the effect of sex that is associated with primary ACL injury.
Using data from the Danish Knee Ligament Reconstruction Register, Rahr-Wagner et al24 found an increased risk of revision ACL surgery when the femoral tunnel was drilled through a medial portal compared with transtibial drilling. In the present study, there were no differences in terms of graft failure when drilling the femoral tunnel through a medial portal versus transtibial.
There are only a few studies in the current literature about the effect of BMI on revision ACL surgery. In the present study, there was no relationship between BMI and revision ACL surgery. Similar findings were reported by Hettrich et al.10 However, Persson et al22 found greater risk of revision in patients with a BMI of <25 kg/m2 compared with patients with a BMI of >25 kg/m2. Similarly, van Eck et al36 found that greater body weight was associated with graft failure. Based on data from this study and other high-quality studies, it appears as though BMI has no effect on the frequency of revision, and if it does, it might be a confounder, for instance, for activity level.
Retrospective case control studies are often used to identify potential risk factors for adverse outcomes. However, there are several limitations to the present study. First, low follow-up is a severe limitation. Also, nonresponders to the study invitation were younger than those that responded. Since younger individuals in the current study as well as previous reports were more likely to undergo revision surgery, missing data from younger individuals could affect the prevalence of revision ACL surgery and result in an underestimation of the true overall revision surgery rate. Moreover, objective outcome measurements (eg, Lachman test, pivot-shift test, and KT-1000 arthrometer measurements) not being included at follow-up and limited information about reinjury are additional obvious limitations. Finally, revision surgery was used as a measure of graft failure, and it is likely that some individuals who experienced graft failure choose not to undergo revision surgery, which probably underestimates the graft failure rate. A strength of the study was that patients were asked to report all subsequent surgeries, not only evidence of revision ACL reconstruction. Given the significance of surgery to a patient, it is not likely that they would under-report revision ACL surgery. Moreover, the determination of revision surgery was not solely dependent on the patient returning to the Center for Sports Medicine, which minimizes the risk of underestimating the true rate of revision ACL surgery because patients may elect to go to another provider for their revision surgery.
Future studies that prospectively evaluate the incidence of revision ACL surgeries are necessary to more accurately determine the rate of revision ACL surgery after primary ACL reconstruction as well as the factors associated with revision ACL surgery. The validity of these prospective studies will be dependent on achieving adequate long-term follow-up (>80% over 5 or more years) to determine the true estimate of revision ACL reconstruction. In addition to determining the incidence of revision ACL surgery, to determine the true rate of ACL graft failure, other indicators of graft failure that should be considered are complaints of knee instability, pathological laxity (both anterior and anterolateral), and magnetic resonance imaging evidence of graft failure.
Conclusion
The overall rate of revision ACL surgery after primary unilateral ACL reconstruction was 8.4%. Univariate predictors of revision ACL reconstruction included younger age at the time of surgery, competitive baseline activity level, and double-bundle ACL reconstruction. However, multivariable logistic regression analysis indicated that age and reconstruction performed with allograft were the only independent predictors of revision ACL reconstruction.
Footnotes
References
- 1. Ahlden M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40:2230–2235. [DOI] [PubMed] [Google Scholar]
- 2. Andernord D, Björnsson H, Petzold M, et al. Surgical predictors of early revision surgery after anterior cruciate ligament reconstruction: results from the Swedish National Knee Ligament Register on 13,102 patients. Am J Sports Med. 2014;42:1574–1582. [DOI] [PubMed] [Google Scholar]
- 3. Andernord D, Desai N, Björnsson H, Ylander M, Karlsson J, Samuelsson K. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015;43:121–127. [DOI] [PubMed] [Google Scholar]
- 4. Barber-Westin SD, Noyes FR, Andrews M. A rigorous comparison between the sexes of results and complications after anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25:514–526. [DOI] [PubMed] [Google Scholar]
- 5. Björnsson H, Desai N, Musahl V, et al. Is double-bundle anterior cruciate ligament reconstruction superior to single-bundle? A comprehensive systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:696–739. [DOI] [PubMed] [Google Scholar]
- 6. Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009;37:2362–2367. [DOI] [PubMed] [Google Scholar]
- 7. Buoncristiani AM, Tjoumakaris FP, Starman JS, Ferretti M, Fu FH. Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2006;22:1000–1006. [DOI] [PubMed] [Google Scholar]
- 8. Ferrari JD, Bach BR, Bush-Joseph CA, Wang T, Bojchuk J. Anterior cruciate ligament reconstruction in men and women. Arthroscopy. 2001;17:588–596. [DOI] [PubMed] [Google Scholar]
- 9. Gwinn D, Wilckens J, McDevitt E, Ross G, Kao T. The relative incidence of ACL injury in men and women at the United States Naval Academy. Am J Sports Med. 2000;28:98–102. [DOI] [PubMed] [Google Scholar]
- 10. Hettrich CM, Dunn WR, Reinke EK, Spindler KP. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41:1534–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hofbauer M, Muller B, Murawski CD, van Eck CF, Fu FH. The concept of individualized anatomic anterior cruciate ligament (ACL) reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22:979–986. [DOI] [PubMed] [Google Scholar]
- 12. Hofbauer M, Valentin P, Kdolsky R, et al. Rotational and translational laxity after computer-navigated single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1201–1207. [DOI] [PubMed] [Google Scholar]
- 13. Jarvela T. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc. 2007;15:500–507. [DOI] [PubMed] [Google Scholar]
- 14. Krych AJ, Jackson JD, Hoskin TL, Dahm DL. A meta-analysis of patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction. Arthroscopy. 2008;24:292–298. [DOI] [PubMed] [Google Scholar]
- 15. Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40:1551–1557. [DOI] [PubMed] [Google Scholar]
- 16. Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91:2321–2328. [DOI] [PubMed] [Google Scholar]
- 17. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28:526–531. [DOI] [PubMed] [Google Scholar]
- 18. Maletis GB, Inacio MC, Desmond JL, Funahashi TT. Reconstruction of the anterior cruciate ligament: association of graft choice with increased risk of early revision. Bone Joint J. 2013;95-B:623–628. [DOI] [PubMed] [Google Scholar]
- 19. Maletis GB, Inacio MC, Funahashi TT. Analysis of 16,192 anterior cruciate ligament reconstructions from a community-based registry. Am J Sports Med. 2013;41:2090–2098. [DOI] [PubMed] [Google Scholar]
- 20. Nyland J, Klein S, Caborn DN. Lower extremity compensatory neuromuscular and biomechanical adaptations 2 to 11 years after anterior cruciate ligament reconstruction. Arthroscopy. 2010;26:1212–1225. [DOI] [PubMed] [Google Scholar]
- 21. Ortiz A, Olson S, Trudelle-Jackson E, Rosario M, Venegas HL. Landing mechanics during side hopping and crossover hopping maneuvers in noninjured women and women with anterior cruciate ligament reconstruction. PM R. 2011;3:13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Persson A, Fjeldsgaard K, Gjertsen JE, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42:285–291. [DOI] [PubMed] [Google Scholar]
- 23. Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23:1320–1325.e6. [DOI] [PubMed] [Google Scholar]
- 24. Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind MC. Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy. 2013;29:98–105. [DOI] [PubMed] [Google Scholar]
- 25. Rozzi S, Lephart S, Gear W, Fu FH. Knee joint laxity and neuromuscular characteristics of male and female soccer and basketball players. Am J Sports Med. 1999;27:312–319. [DOI] [PubMed] [Google Scholar]
- 26. Salmon L RV, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:948–957. [DOI] [PubMed] [Google Scholar]
- 27. Samuelsson K, Andersson D, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy. 2009;25:1139–1174. [DOI] [PubMed] [Google Scholar]
- 28. Shah AA, McCulloch PC, Lowe WR. Failure rate of Achilles tendon allograft in primary anterior cruciate ligament reconstruction. Arthroscopy. 2010;26:667–674. [DOI] [PubMed] [Google Scholar]
- 29. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246–251. [DOI] [PubMed] [Google Scholar]
- 30. Singhal MC, Gardiner JR, Johnson DL. Failure of primary anterior cruciate ligament surgery using anterior tibialis allograft. Arthroscopy. 2007;23:469–475. [DOI] [PubMed] [Google Scholar]
- 31. Snow M, Campbell G, Adlington J, Stanish WD. Two to five year results of primary ACL reconstruction using doubled tibialis anterior allograft. Knee Surg Sports Traumatol Arthrosc. 2010;18:1374–1378. [DOI] [PubMed] [Google Scholar]
- 32. Suomalainen P, Järvelä T, Paakkala A, Kannus P, Järvinen M. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 5-year results. Am J Sports Med. 2012;40:1511–1518. [DOI] [PubMed] [Google Scholar]
- 33. Suomalainen P, Moisala AS, Paakkala A, Kannus P, Järvelä T. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: randomized clinical and magnetic resonance imaging study with 2-year follow-up. Am J Sports Med. 2011;39:1615–1622. [DOI] [PubMed] [Google Scholar]
- 34. Tiamklang T, Sumanont S, Foocharoen T, Laopaiboon M. Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2012;11:CD008413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31:831–842. [DOI] [PubMed] [Google Scholar]
- 36. van Eck CF, Schkrohowsky JG, Working ZM, Irrgang JJ, Fu FH. Prospective analysis of failure rate and predictors of failure after anatomic anterior cruciate ligament reconstruction with allograft. Am J Sports Med. 2012;40:800–807. [DOI] [PubMed] [Google Scholar]
- 37. Wasserstein D, Khoshbin A, Dwyer T, et al. Risk factors for recurrent anterior cruciate ligament reconstruction: a population study in Ontario, Canada, with 5-year follow-up. Am J Sports Med. 2013;41:2099–2107. [DOI] [PubMed] [Google Scholar]
- 38. Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35:1131–1134. [DOI] [PubMed] [Google Scholar]