Abstract
Objective
The goal of this study was to examine links between concerns about community violence and objective and subjective sleep parameters in an adolescent sample. Sex was considered as a moderator of effects.
Design
The study used a cross-sectional design.
Participants
The community-based sample included 252 adolescents (53% girls) with an average age of 15.79 years (SD = 0.81) from the Southeastern United States. The sample included 34% African American and 66% European American adolescents from a wide range of socioeconomic backgrounds.
Measurements
Adolescent-reported community violence concerns were assessed using a composite of 3 separate subscales that measured perceived community safety and threats of community and school violence. Sleep duration and quality were assessed using actigraphy, and subjective sleep problems and daytime sleepiness were measured with subscales of the School Sleep Habits Survey.
Results
Community violence predicted lower sleep efficiency, more long-wake episodes, and more sleep/wake problems and sleepiness. Sex-related moderation effects revealed that girls in the sample were more vulnerable to the effects of violence concerns on their objective sleep quality.
Conclusions
Findings highlight the role of community violence concerns on adolescents’ sleep, revealing that greater community violence concerns are linked with lower levels of actigraphy-based and subjective reports of sleep quality, particularly for adolescent girls. Consideration of the mechanisms by which violence concerns may affect sleep is discussed.
Keywords: Community violence, Adolescent, Sleep, Actigraphy
Exposure to community violence is a common experience for adolescents living in disadvantaged neighborhoods. Compared with adults, adolescents are at increased risk of exposure to community violence. The 2009 National Survey of Children’s Exposure to Violence found that more than 60% of youth ages 12–17 years reported exposure to violence and nearly 20% reported having witnessed an assault within their communities in the past year. Being a victim of, having witnessed, or even hearing about violence within the neighborhood may lead youth to develop concerns about their own safety.1 In a meta-analysis on the effects of exposure to community violence, Fowler and colleagues2 concluded that as a consequence of community violence exposure, adolescents often develop concerns for their safety that cause them to experience a state of chronic hyperarousal. Prior research has shown that youth who were victims or witnesses of violence were less likely to show the normal, expected drop in blood pressure at night (an indication of physiological hyperarousal), lending support to this pathway of effects.3
Links between concerns for safety and arousal raise questions about the possible effects of safety concerns on sleep for adolescents. A prominent framework articulated by Dahl4 suggests that sleep and arousal/vigilance are contradictory processes and that sufficient and good quality sleep is most likely to occur when vigilance is reduced. Concerns for one’s safety, therefore, may interfere with the initiation of sleep, reduce the total hours slept, and potentially have negative effects on sleep quality. The framework has been valuable to research examining links between violence in the home and children’s sleep,5 which has demonstrated that feelings of emotional insecurity and safety concerns mediate links between violence exposure and sleep.6
Several studies have demonstrated associations between poor neighborhood conditions, including exposure to violence and sleep disturbances in adolescents.7,8 There is also a body of research that considers violence exposure and sleep problems as part of a broader constellation of symptoms related to post-traumatic stress disorder (for review, see Spilsbury9). Still, few studies have explicitly examined the relations between worry about safety and sleep in adolescents. Worry or concerns about one’s safety may be a more proximal psychological variable linking violence exposure to sleep problems. General worry has been shown to be one of the strongest predictors of self-reported disrupted sleep after accounting for sleep disturbance the prior year, traumatic stress, alcohol use, and demographic variables in a sample of African-American youth living in impoverished, inner-city neighborhoods.10 Furthermore, there are a few notable empirical studies using adult samples that have shown that feelings of neighborhood safety are related to sleep. For example, in a large, national sample of adults in Argentina, self-reported sleep quality and duration were negatively associated with feelings of safety in one’s neighborhood and home, particularly for women.11 In another large international study across 6 countries, self-reported insomnia symptoms and reports of poor sleep quality were worse for those who reported feeling unsafe in their neighborhoods.12
The current study extends research conducted with adults to an adolescent sample by considering links between concerns about neighborhood safety and sleep. We examine these relations while accounting for general anxiety symptoms to mitigate potential confounds. Because prior research has often relied on self-report of both worry and sleep, the use of actigraphy-derived sleep in the current study reduces the effects of potential reporter bias on results. Consistent with the framework that vigilance interferes with the maintenance of sleep, we expected greater concerns for safety to be associated with poorer self-reported and objective sleep duration and quality. Sex is examined as a moderator, as prior research with adults11 has shown women to be more vulnerable to the effects of safety concerns on sleep.
Method
Participants
Data for the current study are drawn from the fourth wave (collected from 2012 to 2013) of the Family Stress Study; community violence and actigraphic sleep measures were not collected at earlier waves. Recruited through flyers distributed to elementary schools in the Southeastern United States, children were eligible for the study if their parents had been living together for at least 2 years and if they were not diagnosed with the following: attention deficit/hyperactivity disorder, developmental delays, clinical sleep disorder, or a chronic illness. At T1, 251 school-aged children participated, and 79% (n = 199) of those children participated at T4. To increase the sample size, an additional 53 families were recruited at T4 from the same schools as the original sample using the same inclusion/exclusion criteria. The participants recruited at T4 did not differ from those recruited at T1 on demographic or primary study variables.
The final analytic sample consisted of 252 adolescents (118 boys, 134 girls; 66% European American, 34% African American; Mage = 15.79 years, SD = 0.81). Income-to-needs ratio (annual family income divided by federal poverty threshold for a given family size13) indicated that families in the current wave were from a wide range of socioeconomic backgrounds. Approximately 42% of families were living in or near the poverty line (ratio ≤ 2), 22%were of lower middle class (ratio > 2 and < 3), and 36%were of middle class (ratio ≥ 3). The majority (82%) of adolescents lived in a 2-parent household, 14% lived in a single-parent household, and 4% lived with a legal guardian(s).
Procedure
The study was approved by the university’s institutional review board. Consent and assent for participation were obtained from parents and adolescents, respectively. Objective sleep data were collected during the regular school year, excluding holidays and obtained from actigraphs worn on adolescents' nondominant wrist at bedtime for 7 consecutive nights. Sleep diaries were used to corroborate actigraphy data.14 Nights during which medication was used (reported in sleep diary)were excluded from analyses. Families visited the laboratory 3.96 days (SD = 12.25) following the last night of actigraphy to complete questionnaires.
Measures
Community violence concerns
Adolescents completed the 6-item crime safety subscale of the Neighborhood Walkability Scale.15 Items (eg, “There is high crime in my neighborhood”; “I am worried about being outside alone around my home because I am afraid of being taken or hurt by a stranger”) were rated on a 4-point scale (1 = strongly disagree to 4 = strongly agree; α = .89). Items from the Community Experiences Questionnaire16 were adapted to assess adolescents' perceptions of threats of violence in their community and schools. Threats of community violence were assessed with 7 items (eg, "How worried are you that someone will break in or force their way into your home?”; α = .94), and school violence was assessed with 8 items (eg, "How worried are you that someone will break in your locker?”; α = .90). Items were rated on a 5-point scale (0 = not at all to 4 = a whole lot).
Adolescent reports of crime safety (M = 7.97, SD = 3.26) and threats of community (M = 2.37, SD = 4.28) and school (M = 2.44, SD = 3.95) violence were moderately to highly correlated (rs ranged from.43 to .62, Ps < .001). Scores for each measure were standardized and averaged to create a composite score, hereafter referred to as community violence.
Objective sleep
Sleep data were obtained through Motionlogger Octagonal Basic actigraphs (Ambulatory Monitoring Inc, Ardsley, NY17), and Sadeh’s scoring algorithm was used to score each epoch.18 On average, participants had 5.44 nights (SD = 1.77) of usable actigraphy data; missing data were due to forgetting to wear the watch, mechanical problems, or exclusion of nights with medication use. Because of poor estimation of regular sleep,19 sleep data for adolescents with fewer than 5 nights of actigraphy data (23%) were not included in analyses. The following well-established sleep parameters were derived by averaging actigraphy data across all available nights: (a) sleep minutes—the number of minutes from sleep onset to wake time; (b) sleep efficiency—percentage of epochs scored as sleep between sleep onset and wake time; and (c) long-wake episodes—the number of wake episodes of 5 minutes or more. Night-to-night stability during the week was high for all sleep parameters (αs ranged from .75 to .92).
Subjective sleep
Adolescents completed the School Sleep Habits Survey,20 which measures how often participants experienced sleep/wake problems and sleepiness during the past 2 weeks. The Sleep/Wake problem scale (10 items) assesses problems such as irregular sleep times, unscheduled sleep, staying up late at night, oversleeping, and satisfaction with one’s sleep. Items were rated on 5-point scale (1 = never to 5 = every day/night; α = .77). The Sleepiness scale (9 items) assesses whether participants struggled to stay awake during various activities (eg, watching TV, taking a test); 1 item regarding sleepiness while driving was excluded. Items were rated on a 4-point scale (1 = no to 4 = struggled to stay awake and fallen asleep; α = .71).
Control variables
Some variables were associated with primary study variables and were controlled in analyses, including child sex (0 = girls, 1 = boys), race/ethnicity (0 = European American, 1 = African American), chronic illness such as allergies (0 = no, 1 = yes; 7% yes), age- and sex-standardized body mass index (zBMI), age of adolescent, family income-to-needs ratio, and general anxiety.21
Plan of analysis
Data were checked for outliers, and study variables that exceeded 4 SDs were winsorized22 as the next values within 4 SDs (in total, 3 values were recoded). Data were normally distributed and the amount of missing data across study variables was within an acceptable range (7%–23%).23
Cross-sectional path models were fitted in AMOS24 and used full information maximum likelihood estimation to handle missing data.25 Models examined the effects of community violence on adolescents' sleep and the moderating role of adolescents’ sex. Separate models were fitted for each sleep parameter, and all predictor variables were mean-centered for tests of moderation. Adolescent sex, race/ethnicity, age, income-to-needs ratio, chronic illness, zBMI, and anxiety were included as controls and allowed to covary, yielding a fully saturated model; thus, fit statistics are not reported. Significant interactions were graphed to illustrate associations between the predictor (community violence) and outcome (sleep) for girls and boys–simple slopes were tested.26
Results
Preliminary analyses
On average, adolescent girls and boys reported relatively low levels of community violence concerns, although a wide range was endorsed. On average, girls and boys slept 6.98 and 6.53 hours per night, respectively, and experienced moderate to high levels of sleep efficiency and few long-wake episodes as well as modest levels of sleep/wake problems and sleepiness (Table 1). Among control variables (not depicted in Table 1), higher zBMI was linked with more sleep/wake problems among girls (r = .18, P < .05). Among boys, higher sleep efficiency was associated higher income-to-needs ratio (r = .23, P < .05) and lower chronic illness (r = −.28, P < .01). For girls and boys, anxiety was correlated with community violence (r = .30, P < .01 and r = .31, P < .01, respectively), more sleep/wake problems (r = .30, P < .01; r = .34, P < .001, respectively), and more sleepiness (r = .32, P < .001; r = .27, P < .01, respectively). In addition, t tests examining sex and race/ethnicity differences revealed that, compared with boys, girls reported higher anxiety (Mgirls = 10.75, SD = 7.44; Mboys = 6.93, SD = 7.17; t = 4.00, P < .001) and community violence, and had longer sleep duration, higher sleep efficiency, and fewer long-wake episodes (Table 1). Compared with AAs, EAs reported lower community violence (MEA = −.08, SD = .71; MAA=.16, SD = 1.04; t = −1.84, P < .10) and had longer sleep duration (MEA = 413.52, SD = 50.27; MAA = 387.97, SD = 61.93; t = 2.96, P < .01).
Table 1.
Descriptive statistics and correlations among community violence and indices of sleep.
| 1 | 2 | 3 | 4 | 5 | 6 | Mean (SD) | |
|---|---|---|---|---|---|---|---|
| 1. Community violence | – | .14 | .03 | .02 | .33** | .25* | −.10 (.77)a |
| 2. Sleep minutes | −.20* | – | .59*** | −.37*** | .00 | −.08 | 391.88 (53.24)b |
| 3. Sleep efficiency | −.34** | .59*** | – | −.91*** | .10 | .04 | 89.50 (6.90)c |
| 4. Long-wake episodes | .32** | −.42*** | −.92*** | – | −.12 | −.11 | 2.36 (1.67) d |
| 5. Sleep/wake problems | .22* | −.17+ | −.09 | .04 | – | .44*** | 19.73 (6.99) |
| 6. Sleepiness | .18+ | −.14 | −.08 | .02 | .37*** | – | 13.40 (4.15) |
| Mean (SD) | .10 (.88) | 418.78 (53.36) | 92.07 (6.40) | 2.05 (1.76) | 20.13 (6.57) | 14.24 (3.59) |
Associations and descriptive statistics reported below the diagonal for girls and above the diagonal for boys. The composite of community violence includes standardized indices of neighborhood crime (Mgirls = 8.30, SD = 3.39; Mboys = 7.59, SD = 3.08), community violence (Mgirls = 3.00, SD = 5.07; Mboys = 1.78, SD = 3.69), and school violence (Mgirls = 2.73, SD = 4.18; Mboys = 2.34, SD = 4.81).
Superscripts denote differences between boys and girls.
t = 1.81, P < .10;
t = 3.49, P < .01;
t = 2.69, P < .01;
t = −2.33.
P < .10,
P < .05,
P < .01,
P < .001.
Community violence predicting adolescent sleep
Results from path models for objective and subjective sleep parameters are presented in Tables 2 and 3, respectively. Central to this investigation, after controlling for demographic and anxiety variables, community violence predicted lower sleep efficiency, more frequent long-wake episodes (Table 2), and more subjective sleep/wake problems and sleepiness (Table 3), explaining approximately 3.9%, 6.5%, 2.6%, and 1.5% of unique variance, respectively. Furthermore, analyses examining sex-related moderation effects revealed significant findings for sleep minutes, sleep efficiency, and long-wake episodes, explaining an additional 3.1%, 1.3%, and 0.3% of variance, respectively, but no moderation effects emerged for the subjective sleep parameters.
Table 2.
Path coefficients linking demographic variables and community violence with objective sleep parameters.
| Sleep minutes | Sleep efficiency | Long-wake episodes | |||||||
|---|---|---|---|---|---|---|---|---|---|
| B (SE) | β | R2 | B (SE) | β | R2 | B (SE) | β | R2 | |
| Step 1 | 16.8% | 9.0% | 6.0% | ||||||
| Sex | −29.13*** (7.74) | −.26*** | −2.71** (.99) | −.20** | .58* (.26) | .17* | |||
| Ethnicity | −25.58** (8.01) | −.22** | −.98 (1.03) | −.07 | .08 (.27) | .02 | |||
| Age | −.44 (.39) | −.08 | .06 (.05) | .09 | −.02 (.01) | −.10 | |||
| Income-to-needs ratio | 4.54 (2.94) | .11 | .71+ (.38) | .14+ | −.18+ (.10) | −.14 | |||
| Chronic illness | −31.17* (14.10) | −.15* | −3.75* (1.80) | −.15* | .48 (.47) | .07 | |||
| zBMI | −.05 (3.91) | −.00 | −.28 (.50) | −.04 | .05 (.13) | .03 | |||
| Anxiety | −.79 (.51) | −.11 | −.01 (.07) | −.01 | −.01* (.02) | −.04* | |||
| Step 2 | 16.8% | 12.9% | 12.5% | ||||||
| Community violence | .87 (4.80) | .01 | −1.68** (.60) | −.21** | .66*** (.16) | .30*** | |||
| Step 3 | 20.2% | 14.2% | 12.8% | ||||||
| Community violence × sex | 29.02** (9.04) | .28** | 2.98** (1.15) | .24** | −.59* (.30) | −.18* | |||
Sex coded: 0 = girls, 1 = boys; ethnicity coded: 0 = European American, 1 = African American; chronic illness coded: 0 = no, 1 = yes.
P < .10,
P < .05,
P < .01,
P < .001.
Table 3.
Path coefficients linking demographic variables and community violence with subjective sleep parameters.
| Sleep/wake problems | Sleepiness | |||||
|---|---|---|---|---|---|---|
| B (SE) | β | R2 | B (SE) | β | R2 | |
| Step 1 | 12.5% | 15.0% | ||||
| Sex | .75 (.88) | .06 | −.06 (.50) | −.01 | ||
| Ethnicity | 1.48 (.92) | .10 | .74 (.52) | .09 | ||
| Age | .02 (.04) | .03 | −.05+ (.03) | −.12+ | ||
| Income-to-needs ratio | −.32 (.34) | −.06 | −.26 (.19) | −.09 | ||
| Chronic illness | −.36 (1.60) | −.01 | −.38 (.91) | −.03 | ||
| zBMI | .28 (.44) | .04 | −.58* (.25) | −.14* | ||
| Anxiety | .30*** (.06) | .34*** | .15*** (.03) | .29*** | ||
| Step 2 | 15.1% | 16.5% | ||||
| Community violence | 1.38*** (.53) | .17*** | .60* (.30) | .13* | ||
Sex coded: 0 = girls, 1 = boys; ethnicity coded: 0 = European American, 1 = African American; chronic illness coded: 0 = no, 1 = yes.
P < .10,
P < .05,
P < .001.
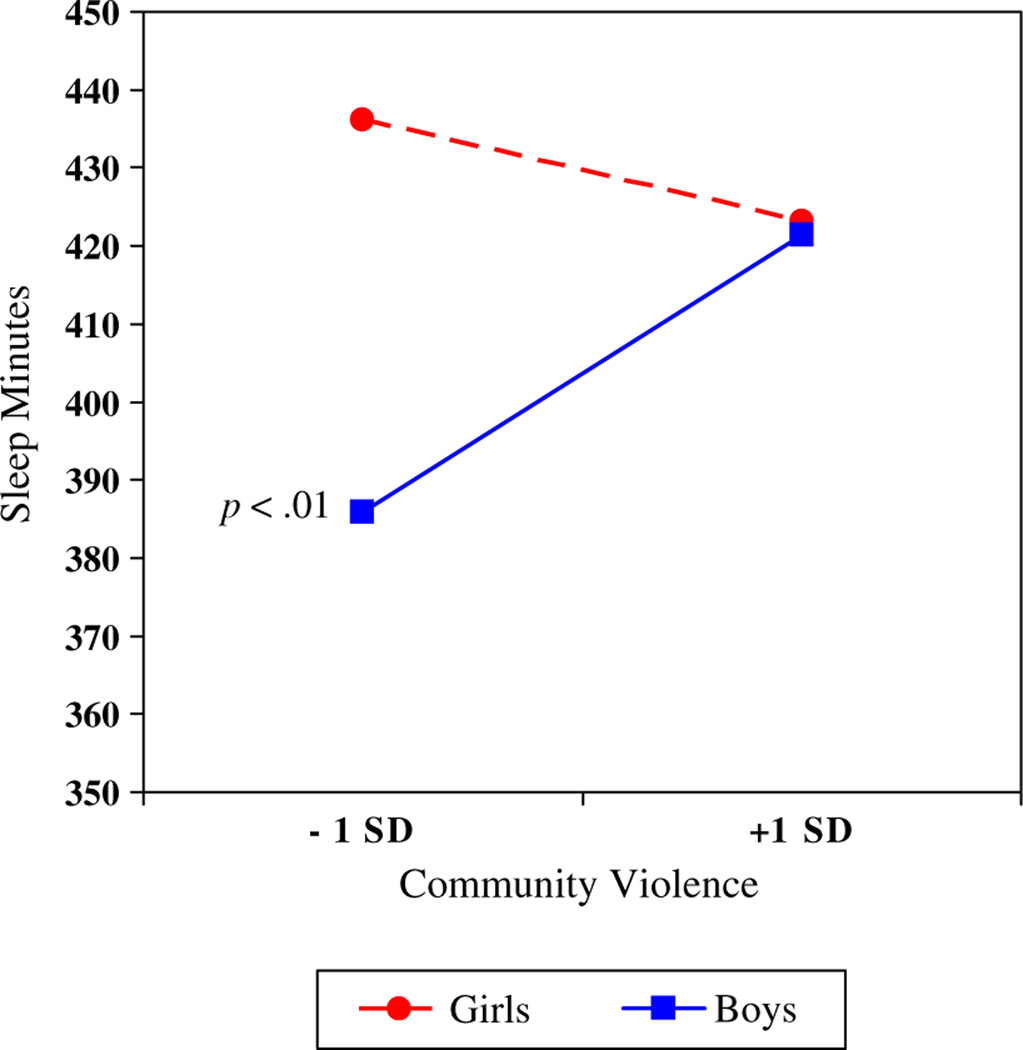
As shown in Figure 1, simple slopes analyses revealed a positive association between community violence and objective sleep duration for boys (B = 21.22, SE = 7.17, P < .01), but no association emerged for girls (B = −7.80, SE = 5.93, P = .19). At low levels of community violence, girls, compared with boys, had longer sleep duration, but girls and boys had similar levels of sleep duration at high levels of community violence.
Fig. 1.
Adolescent sex moderating the association between community violence and sleep minutes.
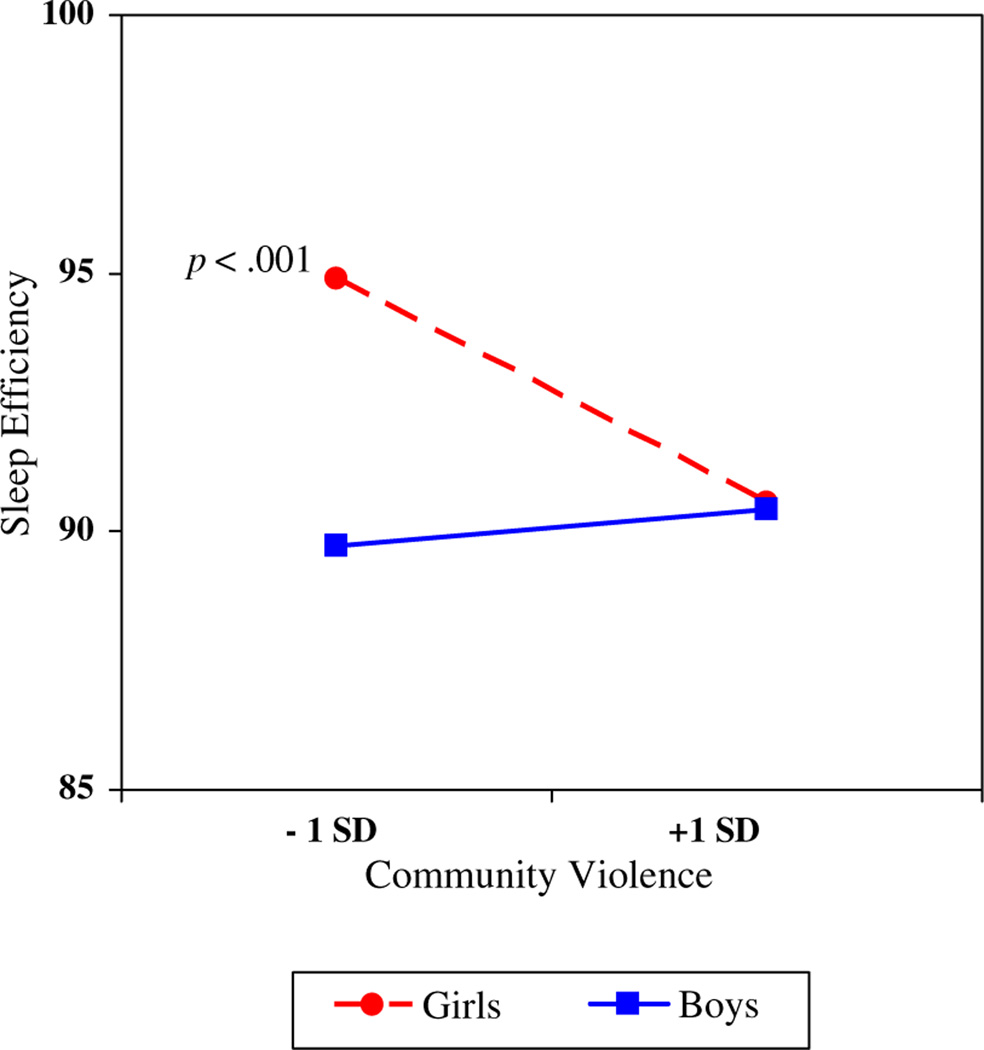
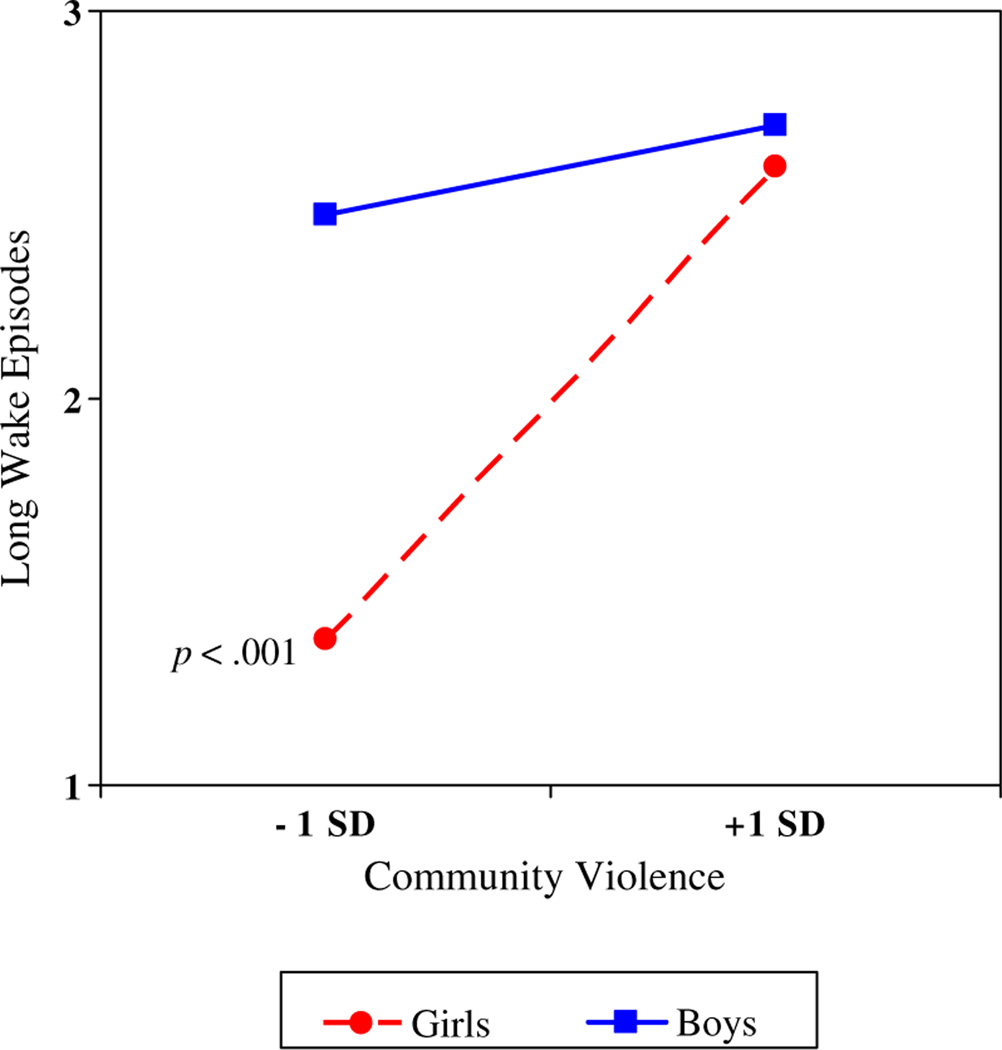
As depicted in Figures 2 and 3, the associations between community violence and poorer objective sleep quality were exacerbated among girls but not boys (sleep efficiency: Bgirls = −2.57, SE= .75, P < .001; Bboys = .41, SE = .90, P =.66; long-wake episodes: Bgirls = .73, SE = .19, P < .001; Bboys=.14, SE=.24, P = .57). Adolescent boys generally had poor sleep quality (lower efficiency, more frequent long-wake episodes) regardless of community violence. However, among girls, associations between community violence and sleep quality emerged. At low levels of community violence, girls had better sleep quality (ie, higher efficiency, fewer long-wake episodes) compared with boys, with differences of approximately .71 to .80 SD. However, at high levels of community violence, adolescent boys and girls had very similar levels of reduced sleep quality.
Fig. 2.
Adolescent sex moderating the association between community violence and sleep efficiency.
Fig. 3.
Adolescent sex moderating the association between community violence and long-wake episodes.
Additional analyses examining the direct effects of each index of community violence (neighborhood crime, threat of community violence, threat of school violence) on objective and subjective sleep revealed similar findings as those using the overall community violence composite reported earlier. However, sex only moderated the association linking threat of community violence, but not neighborhood crime or threat of school violence, with objective sleep parameters. Lastly, exploratory analyses examining race/ethnicity and socioeconomic status as moderators were conducted, but no effects emerged.
Discussion
The results of the current investigation are the first to demonstrate that concerns about community violence are related to objectively assessed sleep quality and subjective reports of sleepiness and sleep problems in an adolescent sample. Overall, findings suggest that greater concerns about one’s safety interfere with the initiation and maintenance of sleep, and particularly with actigraphy-based sleep quality among girls in our sample, even after controlling for demographic variables and general anxiety. Concerns about one’s safety may bring on a psychological and physiological state of arousal that makes attaining high-quality sleep difficult. From this perspective, concerns about community violence are a potential process variable that may explain the association between exposure to community violence to sleep problems.
Research has clearly linked the social environment, including the communities that adolescents live within, to health27; however, the explanations for the observed associations between the social environment and health are less clear. Although not directly examined, findings from the current study support the possibility that sleep may be an important pathway that may explain how the social environment can “get under the skin.”28 Research in adults, which demonstrated that lower sleep quality partially mediated relations between perceived neighborhood disorder and self-rated health,29 supports this proposition. In addition, studies with adolescent populations suggest that the level of sleep problems in our community sample could have a significant impact on physical and mental well-being,30 including risk for prehypertension,31 diabetes,32 and suicidal behavior.33 Given the associations between community violence concerns and disrupted sleep that emerged, and the importance of sleep for many developmental outcomes in adolescence, assessments of pathways of effects that may underlie these associations are warranted
Sex was a moderator of effects between community violence concerns and objective indicators of sleep quality. Girls appear to be more sensitive to the effects of these concerns on sleep, whereas boys in our sample had worse sleep quality overall irrespective of violence concerns. In interpreting the observed sex differences, it is particularly important to make distinctions between exposure to community violence and concerns about community violence (the construct being assessed in the current study). Although prior research has consistently shown that adolescent boys are exposed to greater community violence,34,35 both quantitative and qualitative research suggests that females express more fear and concerns about being the victim of community violence.36,37 Beyond simply being more likely to report concerns, it is also possible that evaluations and coping strategies differ between boys and girls.38 For example, qualitative studies examining reactions to community violence found with both child39 and adult40 samples that females reported a much greater sense of vulnerability to dangers in the community. They suggest that sex roles dictate that, although an awareness of vulnerability is common for females, it is the exception for males. Because of these differences, compared with boys, girls’ sense of security may be undermined by community violence concerns, leading to more disturbed sleep.
Our findings are also consistent with other studies of the consequences of community violence exposure that have shown that girls are more likely to react with internalizing and post-traumatic symptoms, including sleep disturbance.38,41 In addition, it has been postulated that some adolescents respond to violence by becoming desensitized and show blunted reactions to violence.2 Prior research comparing bullied and non-bullied young adults found that this blunted response after chronic exposure to peer victimization was more likely to occur in males.42 Thus, although females might become hypervigilant from exposure to violence, the opposite might be true for males. This prior research may help explain the observed sex differences in regard to sleep efficiency and long-wake episodes and the somewhat paradoxical finding that sleep minutes actually were higher for boys who reported greater community violence concerns. Certainly, more research is needed to further investigate the reasons for the observed sex differences.
Although findings are supportive of the framework that concerns about community violence interfere with sleep, other models are possible. For example, safety concerns may have influenced other daytime behaviors (eg, physical activity) that have a subsequent negative effect on sleep. There is reason to suggest that sedentary day-time behavior (not assessed as part of this study), which has been shown to predict lower objective and subjective sleep quality in adolescents,43might be higher among the youth who reported greater concerns about community violence. A recent study of nearly 2500 youth showed links between perceptions of neighborhood crime and increased screen time for girls and reduced physical activity for boys.44 Parental worries about community violence might also lead them to restrict access and limit the movement of their adolescents within the neighborhood,45 thereby reducing daytime physical activity. In addition, the cross-sectional data leave open the possibility that instead of (or in addition to) the proposed direction of effects (worry predicting sleep), it is also possible that poor sleep may contribute to greater worry. Indeed, prior longitudinal research with adolescents found that sleep disturbance predicted catastrophic worry and that worry meditated relations between disturbed sleep and depressive symptoms over time.46 This raises the possibility that poor sleep and worries about safety may exacerbate each other, creating a particularly negative cycle for adolescents living in dangerous communities. Further studies are necessary to better understand the mechanisms by which concerns about violence affect sleep and reciprocal effects in these relations. Such research will best inform prevention efforts aimed at reducing negative outcomes for high-risk youth.
The findings of the current study should be considered in light of study limitations. The sample was drawn from primarily semirural communities in the Southeastern United States where the exposures to community violence may be quantitatively and qualitatively different from those encountered in more urban environments. Indeed, approximately half of our participants reported no concerns about community violence and, thus, the unique attributes of our sample may mean that findings may not generalize to other populations. Our assessment of community violence concerns should be interpreted as the overall level of concern the adolescent has about violence in the community; however, it is possible that particular concerns are more salient than others in terms of their effect on sleep. Finally, because we did not assess community violence exposure, the potential role of concerns about violence as a mediator that explains prior research linking exposure to violence and sleep remains an important and open scientific question. Despite these limitations, findings from the current study demonstrate the link between community violence concerns and objective and subjective reports of disturbed sleep among adolescents, particularly among girls.
Acknowledgments
This research was supported by grant R01-HD046795 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development awarded to Mona El-Sheikh. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We wish to thank the staff of our research laboratory, most notably Bridget Wingo, for data collection and preparation, and the school personnel, children, and parents who participated.
Footnotes
Disclosure
The authors declare no conflicts of interest.
References
- 1.Buckner JC, Beardslee WR, Bassuk EL. Exposure to violence and low-income children's mental health: direct, moderated, and mediated relations. Am J Orthopsychiatry. 2004;74:413–423. doi: 10.1037/0002-9432.74.4.413. [DOI] [PubMed] [Google Scholar]
- 2.Fowler PJ, Tompsett CJ, Braciszewski JM, Jacques-Tiura AJ, Baltes BB. Community violence: a meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Dev Psychopathol. 2009;21:227–259. doi: 10.1017/S0954579409000145. [DOI] [PubMed] [Google Scholar]
- 3.Wilson DK, Kliewer W, Teasley N, Plybon L, Sica DA. Violence exposure, catecholamine excretion, and blood pressure nondipping status in African American male versus female adolescents. Psychosom Med. 2002;64:906–915. doi: 10.1097/01.psy.0000024234.11538.d3. [DOI] [PubMed] [Google Scholar]
- 4.Dahl RE. The regulation of sleep and arousal: development and psychopathology. Dev Psychopathol. 1996;8:3–27. [Google Scholar]
- 5.El-Sheikh M, Buckhalt JA, Mize J, Acebo C. Marital conflict and disruption of children's sleep. Child Dev. 2006;77:31–43. doi: 10.1111/j.1467-8624.2006.00854.x. [DOI] [PubMed] [Google Scholar]
- 6.El-Sheikh M, Buckhalt JA, Cummings EM, Keller P. Sleep disruptions and emotional insecurity are pathways of risk for children. J Child Psychol Psychiatry. 2007;48:88–96. doi: 10.1111/j.1469-7610.2006.01604.x. [DOI] [PubMed] [Google Scholar]
- 7.Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C, Redline S. Correlates of adolescent sleep time and variability in sleep time: the role of individual and health related characteristics. Sleep Med. 2011;12(3):239–245. doi: 10.1016/j.sleep.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pabayo R, Molnar BE, Street N, Kawachi I. The relationship between social fragmentation and sleep among adolescents living in Boston, Massachusetts. J Public Health. 2014;36:587–598. doi: 10.1093/pubmed/fdu001. [DOI] [PubMed] [Google Scholar]
- 9.Spilsbury JC. Sleep as a mediator in the pathway from violence-induced traumatic stress to poorer health and functioning: a review of the literature and proposed conceptual model. Behav Sleep Med. 2009;7:223–244. doi: 10.1080/15402000903190207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Umlauf MG, Bolland JM, Lian BE. Sleep disturbance and risk behaviors among inner-city African-American adolescents. J Urban Health. 2011;88:1130–1142. doi: 10.1007/s11524-011-9591-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simonelli G, Patel SR, Rodríguez-Espínola S, et al. The impact of home safety on sleep in a Latin American country. Sleep Health. 2015;1:98–103. doi: 10.1016/j.sleh.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Hill TD, Trinh HN, Wen M, Hale L. Perceived neighborhood safety and sleep quality: a global analysis of six countries. Sleep Med. 2015 doi: 10.1016/j.sleep.2014.12.003. [forthcoming] [DOI] [PubMed] [Google Scholar]
- 13.U.S. Department of Commerce. How the Census Bureau Measures Poverty. 2013 [Available from: http://www.census.gov/hhes/www/poverty/about/overview/measure.html]
- 14.Acebo C, Carskadon MA. Scoring Actigraph Data Using ACTION-W 2. Providence, RI: Bradley Sleep Center, Brown University; 2001. [Google Scholar]
- 15.Rosenberg D, Ding D, Sallis JF, et al. Neighborhood Environment Walkability Scale for Youth (NEWS-Y): reliability and relationship with physical activity. Prev Med. 2009;49:213–218. doi: 10.1016/j.ypmed.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz D, Proctor LJ. Community violence exposure and children's social adjustment in the school peer group: the mediating roles of emotion regulation and social cognition. J Consult Clin Psychol. 2000;68:670–683. [PubMed] [Google Scholar]
- 17.Ardsley, NY: Ambulatory Monitoring Inc.; Available from: http://www.ambulatory-monitoring.com/motionlogger.html. [Google Scholar]
- 18.Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep. 1994;17:201–207. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
- 19.Meltzer LJ, Montgomery-Downs HE, Insana SP, Walsh CM. Use of actigraphy for assessment in pediatric sleep research. Sleep Med Rev. 2012;16:463–475. doi: 10.1016/j.smrv.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–887. [PubMed] [Google Scholar]
- 21.Reynolds CR, Richmond BO. Revised Children's Manifest Anxiety Scale Manual, Second Edition (RCMAS-2) Los Angeles, CA: Western Psychological Services; 2008. [Google Scholar]
- 22.Wilcox R. Introduction to Robust Estimation and Hypothesis Testing. 2nd. San Diego, CA: Academic Press; 2005. [Google Scholar]
- 23.Muthén LK, Muthén BO. Mplus User’s Guide. Sixth. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- 24.Arbuckle J. Amos 21 Users Guide. Chicago, IL: Amos Development Corporation; 2012. [Google Scholar]
- 25.Acock AC. Working with missing values. J Marriage Fam. 2005;67:1012–1028. [26] [Google Scholar]
- 26.Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. J Educ Behav Stat. 2006;31:437–448. [Google Scholar]
- 27.Viner RM, Ozer EM, Denny S, et al. Adolescence and the social determinants of health. The Lancet. 2012;379(9826):1641–1652. doi: 10.1016/S0140-6736(12)60149-4. [DOI] [PubMed] [Google Scholar]
- 28.McEwen BS. Brain on stress: how the social environment gets under the skin. Proc Natl Acad Sci. 2012;109(Supplement 2):17180–17185. doi: 10.1073/pnas.1121254109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hale L, Hill TD, Burdette AM. Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Prev Med. 2010;51(3–4):275–278. doi: 10.1016/j.ypmed.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 30.Kelly RJ, El-Sheikh M. Reciprocal relations between children’s sleep and their adjustment over time. Dev Psychol. 2014;50(4):1137–1147. doi: 10.1037/a0034501. [DOI] [PubMed] [Google Scholar]
- 31.Javaheri S, Storfer-Isser A, Rosen CL, Redline S. Sleep quality and elevated blood pressure in adolescents. Circulation. 2008;118(10):1034–1040. doi: 10.1161/CIRCULATIONAHA.108.766410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matthews KA, Dahl RE, Owens JF, Lee L, Hall M. Sleep duration and insulin resistance in healthy black and white adolescents. Sleep. 2012;35(10):1353–1358. doi: 10.5665/sleep.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wong MM, Brower KJ. The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. J Psychiatr Res. 2012;46(7):953–959. doi: 10.1016/j.jpsychires.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stein BD, Jaycox LH, Kataoka S, Rhodes HJ, Vestal KD. Prevalence of child and adolescent exposure to community violence. Clin Child Fam Psychol Rev. 2003;6:247–264. doi: 10.1023/b:ccfp.0000006292.61072.d2. [DOI] [PubMed] [Google Scholar]
- 35.Springer C, Padgett DK. Gender differences in young adolescents' exposure to violence and rates of PTSD symptomatology. Am J Orthopsychiatry. 2000;70:370–379. doi: 10.1037/h0087637. [DOI] [PubMed] [Google Scholar]
- 36.Pain RH. Social geographies of women's fear of crime. Trans Inst Br Geogr. 1997;22(2):231–244. [Google Scholar]
- 37.Rasmussen A, Aber M, Bhana A. Adolescent coping and neighborhood violence: perceptions, exposure, and urban youths' efforts to deal with danger. Am J Community Psychol. 2004;33(1–2):61–75. doi: 10.1023/b:ajcp.0000014319.32655.66. [DOI] [PubMed] [Google Scholar]
- 38.Rosario M, Salzinger S, Feldman R, Ng-Mak D. Intervening processes between youths’ exposure to community violence and internalizing symptoms over time: the roles of social support and coping. Am J Community Psychol. 2008;41(1–2):43–62. doi: 10.1007/s10464-007-9147-7. [DOI] [PubMed] [Google Scholar]
- 39.Valentine G. “Oh yes I can”“Oh no you can't”: children and parents' understandings of kids' competence to negotiate public space safely. Antipode. 1997;29(1):65–89. [Google Scholar]
- 40.Hollander JA. Vulnerability and dangerousness: the construction of gender through conversation about violence. Gend Soc. 2001;15(1):83–109. [Google Scholar]
- 41.Foster JD, Kuperminc GP, Price AW. Gender differences in posttraumatic stress and related symptoms among inner-city minority youth exposed to community violence. J Youth Adolesc. 2004;33:59–69. [Google Scholar]
- 42.Hamilton LD, Newman ML, Delville CL, Delville Y. Physiological stress response of young adults exposed to bullying during adolescence. Physiol Behav. 2008;95:617–624. doi: 10.1016/j.physbeh.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 43.Lang C, Brand S, Feldmeth AK, Holsboer-Trachsler E, Pühse U, Gerber M. Increased self-reported and objectively assessed physical activity predict sleep quality among adolescents. Physiol Behav. 2013;120:46–53. doi: 10.1016/j.physbeh.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 44.Forsyth A, Wall M, Choo T, Larson N, Van Riper D, Neumark-Sztainer D. Perceived and police-reported neighborhood crime: linkages to adolescent activity behaviors and weight status. J Adolesc Health. 2015;57:222–228. doi: 10.1016/j.jadohealth.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Echeverria SE, Kang AL, Isasi C, Johnson-Dias J, Pacquiao D. A community survey on neighborhood violence, park use, physical activity among urban youth. J Phys Act Health. 2014;11:186–194. doi: 10.1123/jpah.2012-0023. [DOI] [PubMed] [Google Scholar]
- 46.Danielsson NS, Harvey AG, MacDonald S, Jansson-Fröjmark M, Linton SJ. Sleep disturbance and depressive symptoms in adolescence: the role of catastrophic worry. J Youth Adolesc. 2013;42:1223–1233. doi: 10.1007/s10964-012-9811-6. [DOI] [PubMed] [Google Scholar]