Abstract
Child maltreatment is a robust risk factor for internalizing and externalizing psychopathology in children and adolescents. We examined the role of disruptions in emotion regulation processes as a developmental mechanism linking child maltreatment to the onset of multiple forms of psychopathology in adolescents. Specifically, we examined whether child maltreatment was associated with emotional reactivity and maladaptive cognitive and behavioral responses to distress, including rumination and impulsive behaviors, in two separate samples. We additionally investigated whether each of these components of emotion regulation were associated with internalizing and externalizing psychopathology and mediated the association between child maltreatment and psychopathology. Study 1 included a sample of 167 adolescents recruited based on exposure to physical, sexual, or emotional abuse. Study 2 included a sample of 439 adolescents in a community-based cohort study followed prospectively for 5 years. In both samples, child maltreatment was associated with higher levels of internalizing psychopathology, elevated emotional reactivity, and greater habitual engagement in rumination and impulsive responses to distress. In Study 2, emotional reactivity and maladaptive responses to distress mediated the association between child maltreatment and both internalizing and externalizing psychopathology. These findings provide converging evidence for the role of emotion regulation deficits as a transdiagnostic developmental pathway linking child maltreatment with multiple forms of psychopathology.
Keywords: Emotion regulation, Emotional reactivity, Rumination, Responses to distress, Child maltreatment, Adolescence, Internalizing, Externalizing
Introduction
Child maltreatment is a transdiagnostic factor associated with multiple forms of psychopathology. Population-based studies indicate that child maltreatment is associated with elevated risk for the onset of virtually all commonly occurring forms of internalizing and externalizing psychopathology in youths, including anxiety, mood, substance use, and disruptive behavior disorders (Brown et al. 1999; Cohen et al. 2001; Green et al. 2010; McLaughlin et al. 2012). Although numerous processes are involved in the etiology of psychopathology among children who have been maltreated, we argue that disruptions in emotion regulation processes represent a key developmental mechanism linking child maltreatment to the onset of psychopathology. The current paper explores the links between child maltreatment and disruptions in emotion regulation as a transdiagnostic pathway underlying risk for both internalizing and externalizing psychopathology.
Emotion regulation is conceptualized as the processes by which individuals influence the specific emotions they have, when they have them, and how they experience and express emotions (Gross 1998). Here, we focus on the distinct processes involved in emotional reactivity to environmental stimuli and the utilization of specific emotion regulation strategies that serve to modulate the intensity and duration of distress (Cole et al. 2004; Connor-Smith et al. 2000). Together, these processes comprise habitual patterns of responding to emotional stimuli that contribute to adaptation or maladaptation over time and, we argue, represent key mechanisms linking child maltreatment to multiple forms of psychopathology.
Initial evidence for our prediction that child maltreatment results in disruptions in emotional reactivity can be gleaned from studies of stressful life events. A wide range of stressors, ranging from peer victimization and community violence exposure to death of a parent or parental divorce, have been associated with higher levels of self-reported emotional reactivity (Heleniak et al. 2015; McLaughlin et al. 2009; McLaughlin and Hatzenbuehler 2009; Paulussen-Hoogeboom et al. 2007). Evidence from behavioral and neuroimaging studies also suggest that child maltreatment is associated with heightened emotional reactivity. Maltreated children demonstrate both enhanced attention to and early identification of threats in the environment (e.g., facial displays of anger) (Pollak and Kistler 2002; Pollak and Tolley-Schell 2003), as well as elevated emotional reactivity as measured by self-report (in adults with maltreatment history; Glaser et al. 2006) and neuroimaging measures of amygdala response to negative emotional stimuli (Gee et al. 2013; McCrory et al. 2011, 2013). Heightened emotional responses to threat cues represent potentially adaptive responses when living in environments characterized by high levels of danger, as these responses facilitate the early identification of threat and mobilize behavioral responses to promote safety.
Child maltreatment might also be associated with patterns of responding to distress that are maladaptive in environments where danger is minimal, leading to poor ability to effectively modulate the intensity and duration of emotional responses. Evidence from multiple lines of research suggests that children exposed to stressful life events are more likely to engage in problematic cognitive or behavioral coping responses (Compas et al. 2001). For example, exposure to community violence, peer victimization, and parental loss have each been associated with high levels of engagement in habitual rumination, a repetitive and passive cognitive response to dysphoric mood that involves focusing on the causes and consequences of negative affect (Heleniak et al. 2015; McLaughlin et al. 2009; McLaughlin and Hatzenbuehler 2009; Michl et al. 2013; Wadsworth et al. 2005). Stressful life events might increase engagement in rumination in adolescents because negative and unexpected life experiences serve as salient reminders of discrepancies between goals and reality, which increases attention to these discrepancies and rumination about how to resolve them (Brewin and Vallance 1997; Ferguson et al. 2010; Papadakis et al. 2006).
A tendency to use maladaptive cognitive responses to distress like rumination might also develop when emotional displays are met with dismissive or punishing reactions from adults. Such reactions teach children to avoid expressing emotions and disclosing their distress by asking for adult assistance in problem-solving, an adaptive emotion regulation strategy commonly employed by children (Eisenberg et al. 1992, 1996). Child maltreatment exemplifies a particularly traumatic and severe punitive experience in which outward expression of emotion or steps to problem-solve might risk escalation of harm. In this circumstance, reliance on passive strategies like rumination may be the only safe option. Research indicating that adolescents and adults abused as children are more likely to engage in rumination lends credence to this idea (Conway et al. 2004; Sarin and Nolen-Hoeksema 2010; Watkins 2009).
Additionally, children reared in stressful environments are often surrounded by caregivers and other adults who model ineffective responses to distress. A primary way that children learn to regulate their emotions is by observing when and how adults react to emotional situations (Denham et al. 1997; Eisenberg et al. 1998; Gottman et al. 1997). For example, children of depressed mothers tend to engage in the same passive and ruminative cognitive style they observe in their caregivers (Garber et al. 1991; Silk et al. 2006), whereas children and adolescents exposed to violence tend to exhibit disruptive behavioral responses to distress (Bingenheimer 2005; Dodge et al. 1990; Eisenberg and Fabes 1994; McCloskey and Lichter 2003; Oshri et al. 2015). In the case of child maltreatment, violent behavior may represent a severe form of behavioral response style modeled by adult perpetrators that focuses on alleviation of intense emotions without considering long-term consequences. Maltreated children may be particularly vulnerable for adopting this impulsive style of responding as they transition into adolescence.
Accumulating evidence indicates a tendency to engage in rash actions when experiencing intense emotions becomes more common in adolescence (Nelson et al. 2002; Steinberg 2004). These actions, ranging from difficulty following through on goal-directed behavior like homework and chore completion to impulsive use of substances and engagement in risky sex (Anestis et al. 2007; Davidson 2003; Depue 1996; Eisenberg et al. 2000; Hajcak et al. 2007; Hessler and Katz 2010; King et al. 2011; Melnick and Hinshaw 2000; Tarter et al. 2003), may increase in frequency as they are negatively reinforced by a reduction in strong negative emotions associated with effective distraction (Heatherton and Baumeister 1991), and positively reinforced by the gratification of acting on urges. If maltreated if they are already more emotionally reactive, their ability to appropriately direct behavior while experiencing intense negative emotional arousal may be particularly impaired. Together, these lines of evidence suggest that child maltreatment may influence cognitive and behavioral responses to distress through numerous pathways, ultimately leading to elevated use of maladaptive strategies such as rumination and impulsive behaviors.
These patterns of heightened emotional reactivity and habitual use of ineffective responses to distress are potential mechanisms underlying the elevated vulnerability for the onset and maintenance of psychopathology observed among maltreated children. Emotional reactivity has been consistently associated with symptoms of anxiety and depression (Anthony et al. 2002; Fox et al. 2010; Phillips et al. 2002; Silk et al. 2003), as well as externalizing problems in youth (Singh and Waldman 2010). Adolescents who respond to distress by engaging in rumination are more likely to endorse depression and anxiety symptoms (Broderick and Korteland 2004; Grabe et al. 2007; Kuyken et al. 2006; Michl et al. 2013; Nolen-Hoeksema et al. 2007; Rood et al. 2009), as well as substance abuse, eating pathology, and conduct problems (McLaughlin et al. 2014a; Nolen-Hoeksema et al. 2007). A wide range of poor mental health outcomes including self-harm, anxiety, substance use, and conduct problems have been observed among adolescents who routinely engage in impulsive behavioral responses to distress (Adrian et al. 2011; Bender et al. 2012; McLaughlin et al. 2011; Walton and Flouri 2010). If child maltreatment does, indeed, lead to changes in emotional reactivity and habitual responses to distress, these emotion regulation patterns are a plausible mechanism linking child maltreatment with the onset of psychopathology. Yet prior studies that have examined this have been limited by a cross-sectional design or by assessment of only a limited number of emotion regulation processes (Conway et al. 2004; Kim and Cicchetti 2009; Maughan and Cicchetti 2002; McLaughlin et al. 2014b; Robinson et al. 2008).
The current study addresses this gap in the literature by comprehensively examining multiple components of emotion regulation utilizing both cross-sectional and longitudinal data from two studies of adolescent development. First, we examine whether exposure to child maltreatment is associated with patterns of emotional reactivity and responses to distress, both concurrently (Study 1) and prospectively (Study 2). Second, we examine in both studies whether each of these components of emotion regulation are associated with adolescent psychopathology. We expected that child maltreatment would be associated with higher emotional reactivity and greater use of maladaptive strategies for responding to distress, including rumination and impulsive behavioral responding. We additionally predicted that higher levels of emotional reactivity and use of maladaptive responses to distress would be associated with greater internalizing and externalizing symptoms, both concurrently and prospectively, and would mediate the association between child maltreatment and later psychopathology (Study 2). To evaluate these hypotheses, we utilized data from a high-risk sample of adolescents recruited for exposure to child maltreatment (Study 1) and a population-based community sample of adolescents followed prospectively over a 5-year period (Study 2).
Study 1
Methods
Participants
A community-based sample of 169 adolescents aged 13–17 was recruited for participation in a laboratory-based study at schools, after-school programs, medical clinics, and the general community in Boston and Cambridge, MA, USA. Recruitment efforts were targeted at obtaining a sample with high diversity with respect to race/ethnicity and socioeconomic status (SES) and variability in exposure to childhood maltreatment, including physical, sexual, or emotional abuse. To do so, we recruited heavily from low-SES neighborhoods and from clinics that served a predominantly low-SES catchment area with one-fourth of the sample (25.9 %, n = 42) reporting an income below the poverty line. The sample consisted of 56.0 % females (n = 94), had a mean age of 14.9 years (SD = 1.36), and 39.1 % (n = 66) reported exposure to maltreatment. Racial/ethnic composition of the sample was as follows: 40.8 % White (n = 69), 18.3 % Black (n = 31), 17.8 % Hispanic (n = 30), 7.7 % Asian (n = 13), and 14.8 % Biracial or Other (n = 25). Over one-third of the sample (37.9 %, n = 64) was from single-parent households. We excluded participants from analysis due to severe cognitive impairment (n = 1), and a diagnosis of a pervasive developmental disorder (n = 1). The final sample included 167 participants.
Measures
Child Maltreatment
Child maltreatment was assessed using the Childhood Trauma Questionnaire (CTQ) (Bernstein et al. 1997, 2003) and the Childhood Experiences of Care and Abuse (CECA) interview (Bifulco et al. 1994, 1997). The CTQ is a 28-item scale that assesses the frequency of exposure to maltreatment during childhood and adolescence. Three types of abuse are assessed: physical, sexual, and emotional abuse. The CTQ is among the most commonly used measures of child maltreatment and has excellent internal consistency, test–retest reliability, and convergent and discriminant validity with both interview measures and clinician reports of maltreatment (Bernstein et al. 1994, 1997). The CECA assesses multiple aspects of caregiving experiences, including physical and sexual abuse. Inter-rater reliability for maltreatment reports is excellent, and multiple validation studies suggest high agreement between siblings on reports of maltreatment (Bifulco et al. 1994, 1997).
To estimate the overall proportion of participants exposed to maltreatment, we used the CTQ and the CECA to create a dichotomous indicator of abuse exposure. Participants who reported physical or sexual abuse during the CECA interview or who had a score on any of the three CTQ abuse sub-scales above a previously-identified threshold (Walker et al. 1999) were classified as having been exposed to maltreatment. We additionally used the CTQ abuse subscales to assess maltreatment severity separately for each of the three types of maltreatment (physical, sexual, and emotional abuse). The CTQ subscales demonstrated good reliability in this study (α = .73–.92).
Emotional Reactivity
Adolescents completed the Emotion Reactivity Scale (ERS) (Nock et al. 2008), a 21-item scale that measures individuals’ general experience of emotion reactivity. The ERS instructs participants to indicate, “how you experience emotions on a regular basis,” with emotions referring to “angry, sad, excited, or some other emotion.” The ERS asks participants to rate items assessing emotional sensitivity (eight items; e.g., “I tend to get emotional very easily”), arousal/intensity (ten items; e.g., “When I experience emotions, I feel them very strongly/intensely”), and persistence (three items; e.g., “When I am angry/upset, it takes me much longer than most people to calm down”) as well as providing an overall emotion reactivity score (i.e., ERS total score). Participants rate each item on a five-point Likert scale ranging from “not at all like me” (0) to “completely like me” (4) with a total possible score ranging from 0 to 84. The ERS has demonstrated excellent reliability and validity among adolescents (Nock et al. 2008), and demonstrated excellent reliability in this study (α = .92).
Habitual Cognitive Responses to Distress
Adolescents completed an abbreviated form of the Children’s Response Styles Questionnaire (CRSQ) (Abela et al. 2002), a 25-item scale that assesses the extent to which children respond to sad feelings with rumination, distraction, or problem-solving. The measure is modeled after the Response Styles Questionnaire (Nolen-Hoeksema and Morrow 1991) that was developed for adults. For each item, youth are asked to rate how often they respond in that way when they feel sad on a four-point Likert scale ranging from “almost never” (1) to “almost always” (4). To assess maladaptive habitual cognitive responses to distress, we used the rumination subscale of our abbreviated measure which included 6 items that were summed. Sample items include: “Think about a recent situation wishing it had gone better” and “Think why can’t I handle things better?” The reliability and validity of the CRSQ have been demonstrated in samples of early adolescents (Abela et al. 2002). The CRSQ rumination scale demonstrated good reliability in this study (α = .81).
Habitual Behavioral Responses to Distress
Primary caregivers completed the Parent-Report version of the Behavior Rating Inventory of Executive Function (BRIEF) (Gioia et al. 2000), an 86-item scale that measures observations of their child’s executive function difficulties in daily life. For each item, caregivers are asked to respond how often they observe a given behavior on a three-point Likert scale ranging from “never” (0) to “often” (2), with higher scores indicative of greater difficulty within a certain area of executive function. Specifically, we utilized the 28-item Behavioral Regulation Index (BRI) comprised of three subscales that measured inhibition (e.g., “blurts things out”), emotional control (e.g., “has outbursts for no reason”), and task shifting abilities (e.g., “tries the same approach to a problem over and over even when it does not work”). The reliability and validity of the BRIEF has been well-established across a wide variety of age ranges, geographic regions, demographic characteristics, and both internalizing and externalizing psychopathology (for reviews see Isquith et al. 2013, 2014; Roth et al. 2015) and the BRIEF BRI subscale demonstrated good reliability in this study (α = .87).
Psychopathology
Internalizing and externalizing psychopathology were assessed using the Youth Self Report (YSR) and Parent Report forms of the Child Behavior Checklist (CBCL) (Achenbach and Rescorla 2001; Achenbach 1991). The CBCL scales are among the most widely used measures of youth emotional and behavioral problems and use extensive normative data to generate age-standardized estimates of the severity of internalizing and externalizing psychopathology. The broad-band internalizing scale is comprised of withdrawn/depressed (e.g., “I would rather be alone than with others”), somatic complains (e.g., “I feel overtired without good reason”) and anxious/depressed (e.g., “I am nervous or tense”) sub-scales. The broad-band externalizing scale is comprised of rule-breaking behavior (e.g., “I don’t feel guilty after doing something I shouldn’t”) and aggressive behavior (e.g., “I destroy things belonging to other”) subscales. The internalizing and externalizing scales have demonstrated validity in discriminating between youths with and without psychiatric disorders (Achenbach 1991; Chen et al. 1994; Seligman et al. 2004). In this sample the youth-report internalizing scale demonstrated good reliability (α = .88) as did the youth-report externalizing scale (α = .84). The parent-report internalizing scale demonstrated excellent reliability in this sample (α = .90) as did the parent-report externalizing scale (α = .90).
Procedure
Adolescents and their parent visited the laboratory to complete questionnaire measures as part of a larger study protocol examining psychological and physiological measures of emotional reactivity among children with and without exposure to child maltreatment (e.g., McLaughlin et al. 2014b). All measures were administered at one point in time in a single laboratory visit. Informed consent was obtained from the parent/guardian who attended the session, and assent was provided by adolescents. All procedures were approved by the Institutional Review Board at Harvard University and Boston Children’s Hospital. Youth and parents were reimbursed for their participation.
Statistical Analysis
We used linear regression to evaluate the role of emotion regulation as a transdiagnostic risk factor linking child maltreatment to internalizing and externalizing psychopathology. Specifically, we examined the associations of any maltreatment exposure, as well as physical, sexual, and emotional abuse separately, with internalizing and externalizing psychopathology. Next, we examined the associations of these maltreatment variables with each dimension of emotion regulation separately, including emotional reactivity (i.e., emotional sensitivity, arousal/intensity, and persistence), habitual cognitive responses to distress (i.e., rumination), and habitual behavioral responses to distress (i.e., behavioral regulation). We then examined the association between each dimension of emotion regulation and internalizing symptoms and externalizing psychopathology. Finally, we determined whether associations between emotion regulation and internalizing and externalizing psychopathology remained significant after controlling for exposure to child maltreatment (using the CTQ total score). In all models predictors were mean-centered to ensure that effects were always within the range of the data and to reduce multicollinearity (Hayes et al. 2012). We controlled for gender and age in all regression analyses. Because child maltreatment, emotion regulation and psychopathology were assessed at the same time point, we did not conduct a formal mediation analysis (Maxwell and Cole 2007).
Results
Descriptive Statistics
Table 1 provides the means and standard deviations of all measures. Please see “Appendix” Table 5 for the zero-order correlations among all measures of child maltreatment, emotion regulation, and internalizing and externalizing psychopathology.
Table 1.
Means and standard deviations of childhood maltreatment, emotion regulation, and psychopathology variables Study 1
| Measure | Mean | (SD) | Range |
|---|---|---|---|
| 1. CTQ total | 19.63 | 7.01 | 15–52 |
| 2. CTQ-PA | 5.89 | 2.17 | 5–20 |
| 3. CTQ-SA | 5.85 | 2.91 | 5–24 |
| 4. CTQ-EA | 7.89 | 3.72 | 5–25 |
| 5. BRIEF BRI | 59.78 | 12.33 | 45–95 |
| 6. ERS sensitivity | 13.51 | 8.47 | 0–39 |
| 7. ERS arousal | 10.57 | 6.82 | 0–28 |
| 8. ERS persistence | 6.36 | 4.15 | 0–16 |
| 9. ERS total score | 30.44 | 17.85 | 0–79 |
| 10. CRSQ rumination | 5.95 | 4.20 | 0–17 |
| 11. YSR internalizing | 52.93 | 10.23 | 27–79 |
| 12. YSR externalizing | 52.12 | 9.60 | 29–73 |
| 13. CBCL internalizing | 50.96 | 10.57 | 33–81 |
| 14. CBCL externalizing | 48.29 | 10.33 | 34–82 |
CTQ Childhood Trauma Questionnaire, BRIEF BRI behavior rating inventory of executive function behavioral regulation index, ERS sensitivity Emotion Reactivity Scale sensitivity subscale, ERS arousal Emotion Reactivity Scale arousal/intensity subscale, ERS persistence Emotion Reactivity Scale persistence subscale, ERS total score Emotion Reactivity Scale total score, CRSQ rumination Children’s Response Styles Questionnaire rumination subscale, YSR internalizing youth self report form of the Child Behavior Checklist internalizing subscale, YSR externalizing youth self report form of the Child Behavior Checklist externalizing subscale, CBCL internalizing parent report form of the Child Behavior Checklist internalizing subscale, CBCL externalizing parent report form of the Child Behavior Checklist externalizing subscale
Child Maltreatment and Internalizing and Externalizing Psychopathology
All forms of child maltreatment were associated with higher levels of youth-reported internalizing (physical abuse: β = .19, p = .02; sexual abuse: β = .18, p = .03; emotional abuse: β = .42, p <.001) and externalizing (physical abuse: β = .21, p = .009; sexual abuse: β = .20, p = .01; emotional abuse: β = .42, p < .001) symptoms. Only emotional abuse was associated with parent-reported externalizing symptoms (β = .31, p = < .001) and internalizing symptoms at a trend level (β = .14, p = .08). Neither physical nor sexual abuse was associated with parent-reported psychopathology (ps > .10).
Child Maltreatment and Emotion Regulation
Emotional Reactivity
We first examined whether child maltreatment was associated with emotional reactivity using the ERS (Table 2). All forms of child maltreatment were associated with overall higher emotional reactivity (i.e., ERS total score; physical: β = .18, p = .02; sexual: β = .19, p = .01; emotional: β = .36, p = < .001). Emotional abuse was associated with greater symptom levels across each of the ERS subscales including emotional sensitivity (β = .33, p = < .001), arousal/intensity (β = .36, p = < .001), and persistence (β = .30, p = < .001). Physical abuse was associated with greater symptom levels across the arousal/intensity (β = .19, p = .02) and persistence (β = .19, p = .02) subscales, but was only significantly associated with the sensitivity sub-scale at a trend level (β = .14, p = .06). Sexual abuse was associated with greater symptom levels across the sensitivity (β = .17, p = .03) and arousal/intensity (β = .21, p = .008) subscales, but not the persistence subscale (β = .13, p = .10).
Table 2.
Emotion regulation, child maltreatment, and psychopathology Study 1
| Child Trauma Questionnaire
|
Youth self-report
|
Parent report CBCL
|
|||||
|---|---|---|---|---|---|---|---|
| Physical abuse β | Sexual abuse β | Emotional abuse β | Internalizing β | Externalizing β | Internalizing β | Externalizing β | |
| Emotional reactivity | |||||||
| Sensitivity | .14 | .17* | .33** | .63** | .52** | .34** | .29** |
| Arousal/intensity | .19* | .21* | .36** | .54** | .49** | .21* | .28** |
| Persistence | .18* | .13 | .30** | .49** | .48** | .23** | .26** |
| Total | .18* | .19* | .36** | .63** | .55** | .30** | .31** |
| Responses to distress | |||||||
| Rumination | .16* | .23** | .28** | .50** | .36** | .25** | .17* |
| Behavioral regulation | .17* | .06 | .24** | .19* | .22** | .48** | .63** |
Linear regressions controlling for gender and age
Emotional reactivity was measured with the Emotion Reactivity Scale (ERS). Response to distress was measured with the Children’s Response Styles questionnaire (CRSQ). Behavioral regulation was measured with the behavioral regulation index (BRI) of the behavior rating inventory of executive function (BRIEF). Internalizing and externalizing symptoms were measured using the youth self report and parent report forms of the child behavior checklist (CBCL). Physical, sexual, and emotional abuse was measured with the Childhood Trauma Questionnaire (CTQ)
p < .05;
p < .01
Habitual Cognitive Responses to Distress
Additionally, we examined whether child maltreatment was associated with cognitive responses to distress using the rumination scale of the CRSQ (Table 2). All forms of child maltreatment were associated with greater levels of rumination (physical abuse: β = .16, p = .04; sexual abuse: β = .23, p = .003; emotional abuse: β = .28, p = <.001).
Habitual Behavioral Responses to Distress
Finally, we examined whether exposure to maltreatment was associated with dysregulated behavioral responses to distress using the BRI of the BRIEF (Table 2). Physical abuse (β = .17, p = .03) and emotional abuse (β = .24, p = .002), but not sexual abuse (β = −.06, p = .44) were associated with greater levels of behavioral regulation difficulties.
Emotion Regulation and Psychopathology
Emotional Reactivity
Emotional reactivity (i.e., ERS total score) and each ERS subscale (emotional sensitivity, arousal/intensity, and persistence) were all positively associated with youth- and parent-reported internalizing and externalizing symptoms (Table 2).
Habitual Cognitive Responses to Distress
The rumination scale of the CRSQ was positively associated with youth- and parent-reported internalizing and externalizing psychopathology (Table 2).
Habitual Behavioral Responses to Distress
The BRI of the BRIEF was positively associated with youth- and parent-reported internalizing and externalizing psychopathology (Table 2).
All analyses examining the associations between emotion regulation and youth- and parent-reported internalizing and externalizing psychopathology remained significant controlling for child maltreatment with the exception of the association between rumination and parent-reported externalizing symptoms (β = .11, p = .18).
To reduce type I error associated with multiple comparisons, we applied a false discovery rate (FDR) correction (Benjamini and Hochberg 1995) to all analyses involving multiple dimensions of emotion regulation. All associations remained significant after applying this correction.
Study 1: Discussion
Study 1 results indicate that physical, sexual, and emotional abuse are associated with greater levels of youth-reported internalizing and externalizing psychopathology symptoms, higher levels of emotional reactivity, and greater habitual use of maladaptive responses to distress, including rumination and impulsive behavior. In turn, rumination, behavioral dysregulation and emotional reactivity are each associated with higher levels of youth- and parent-reported internalizing and externalizing symptoms, even after controlling for child maltreatment. This pattern of results provides support for our two hypotheses: (1) that child maltreatment is associated with both heightened emotional reactivity and maladaptive responses to distress, and (2) that higher levels of emotion dysregulation are a transdiagnostic factor associated with a wide range of psychopathology symptoms. We next turned to evaluating these associations in a longitudinal cohort study.
Study 2
Methods
Participants and Procedures
The developmental pathways project (DPP) is a community-based prospective cohort study designed to examine the antecedents, phenomenology, and outcomes of depression and conduct problems in early adolescence. DPP participants were recruited from four Seattle-area public schools. These schools are located in four distinct geographic and demographic areas within the city and together have a racial/ethnic distribution that is nearly identical to the total enrolled student population of the school district. Universal mental health screening was carried out initially with approximately 1100 sixth-grade students at these schools, and subsequently across four consecutive years (2001–2004); details of the screening procedure have been described elsewhere (Vander Stoep et al. 2005).
Students who were screened, had at least one parent who could speak English, and were still residing in the district been eligible for recruitment into the longitudinal study. A stratified random sample of students was selected for longitudinal follow-up, with students scoring high on depressive and/or conduct problem scores oversampled to increase the likelihood of observing the onset of depressive and conduct disorders over the course of the longitudinal study. The details of the oversampling procedure are described elsewhere (McCarty et al. 2012). Of those selected, 521 (64.6 %) students and their parents/guardians consented to participate.
Baseline interviews were conducted within 3 months of screening (fall 6th grade), and in-person follow-up interviews were conducted spring 6th, fall 7th, spring 7th, fall 8th, 9th, and 12th grades. Responses to distress and emotional reactivity were assessed at the 8th, 9th and 12th grade time points, and psychopathology was assessed via self-report at the spring 6th, spring 7th, 9th, and 12th grade time points. Participants who contributed to time points from spring of 7th grade to 12th grade follow up were included in this study. The final analytic sample included 439 participants (mean age at spring of 7th grade assessment 13.51, SD = .43, 52.4 % boys, 7.9 % exposed to maltreatment). The racial composition of the study was 25.3 % Black (n = 111), 4.1 % Native American (n = 18), 18.2 % Asian (n = 80) and 52.4 % White (n = 230) with 10.3 % reporting Hispanic ethnicity (n = 45). All procedures were approved by the University of Washington Institutional Review Board. The participants included in this study did not differ significantly from those without follow-up data on any demographic variable.
Measures
Child Maltreatment
At 12th grade follow-up, two questions regarding childhood maltreatment were included in the assessment battery. Adolescents were asked whether during their childhood they experienced serious physical abuse (e.g., “Did anyone you lived with ever hurt you physically so that you were still injured or badly bruised the next day, or you needed medical attention?”) or sexual abuse (e.g., “In your life so far, has any person older than you who wasn’t a girlfriend or boyfriend ever touched you or played with you sexually, or forced you to touch them?”). The maltreatment variable was created and scored dichotomously, with 1 representing exposure to either type of abuse and 0 representing no childhood maltreatment.
Emotional Reactivity
Participants completed the abbreviated self-report version of the dysregulation inventory (DRI; Mezzich et al. 2001), an 18-item broad measure of emotion dysregulation (Ford 2011; Wilcox et al. 2012). The DRI assesses emotion dysregulation at multiple levels, including emotional reactivity and engagement in maladaptive behavioral responses to distress. The self-report scale was normed on adolescents and demonstrates good reliability and validity (Mezzich et al. 2001). The Emotional/Affective Dysregulation subscale measures susceptibility to emotional arousal, irritability, and negative affectivity (i.e., emotional reactivity). Sample items include “I am touchy and get easily annoyed” and “Sometimes I get emotional over nothing.” The affective dysregulation subscale demonstrated adequate reliability across all time points (α = .72–.78).
Habitual Cognitive Responses to Distress
The Ruminative Responses Scale of the Short Response Styles Questionnaire (RRS; Treynor et al. 2003) is a ten-item scale that assesses the extent to which individuals respond to sad feelings with maladaptive cognitive responses to distress (brooding, e.g., “think about a recent situation, wishing it had gone better”) or adaptive responses to distress (reflection, e.g., “analyze recent events to try to understand why you feel depressed”). The brooding scale was used to assess habitual cognitive responses to distress. For each item youths are asked to rate how often they respond in that way on a four-point Likert scale. The reliability and validity of the RSQ have been demonstrated in samples of adolescents (Abela et al. 2002). The brooding scale demonstrated good reliability across all three time points in this study (α = .81–.82).
Habitual Behavioral Responses to Distress
The Behavioral Dysregulation subscale of the DRI was used to assess habitual behavioral responses to distress (Mezzich et al. 2001). The Behavioral Dysregulation subscale measures behavioral impulsivity and sensation-seeking (e.g., “I jump into situations before I think it through”). The behavior dysregulation subscale demonstrated adequate reliability across all time points (α = .72–.78).
Psychopathology
Symptoms of internalizing and externalizing psychopathology were assessed using the YSR form and the Parent Report form of the CBCL (Achenbach 1991). As noted above, the YSR and CBCL scales are among the most widely used measures of youth emotional and behavioral problems and use extensive normative data to generate age-standardized estimates of severity of internalizing and externalizing psychopathology. The internalizing and externalizing scales have demonstrated validity in discriminating between youths with and without psychiatric disorders (Achenbach 1991; Chen et al. 1994; Seligman et al. 2004). Both the youth- and parent-report internalizing scales demonstrated good reliability across all time points (α = .81–.87 and α = .87–.90 respectively). The youth-report externalizing scale demonstrated adequate to good reliability across all timepoints (α = .78–.86) and the parent-report externalizing scale demonstrated good to excellent reliability across all time points (α = .89–.91).
Statistical Analysis
First, we examined whether child maltreatment was associated with changes in internalizing and externalizing symptoms from the spring of grade 7 to grade 12 using separate multi-level models for each type of symptoms. A series of two-level models (observations nested within persons) were estimated. This approach allowed us to simultaneously estimate the variance in psychopathology both within and between individuals over time. We first estimated unconditional growth models separately for internalizing and externalizing psychopathology with Time coded as 0 at baseline and the number of months since the baseline interview at subsequent time points. We centered time, modeled both the intercept (i.e., the average level of each symptom) and the slope (i.e., the rate of change over time), and then examined the change in model fit when each were modeled as random effects. In all cases, inclusion of random effects of intercept and time improved model fit. We next added a quadratic term for Time to the fixed effects models to determine the functional form of the growth trajectory for each symptom marker and examined the difference in model fit between the linear and quadratic model. The linear model was a better fit for both internalizing and externalizing symptoms.
Next, we examined Level 2 (i.e., time-invariant) predictors of internalizing and externalizing psychopathology. Specifically, we examined the association of child maltreatment with both intercepts and the linear rate of change over time for internalizing and externalizing psychopathology.
To examine the association of child maltreatment with emotion regulation, we used the same modeling approach described above. Using multi-level modeling, we estimated growth models for each of the emotion regulation variables (emotional reactivity, and maladaptive cognitive and behavioral responses to distress). A model with a linear effect of time provided the best fit to the data, with the exception of emotional reactivity, for which the quadratic model was a better fit. In this case, quadratic growth across children was modeled as a fixed effect (i.e., did not vary across children). Including a random effect to the quadratic term did not significantly improve model fit. We examined child maltreatment as a predictor of emotion regulation intercepts and changes over time from the fall of 8th grade to the fall of 12th grade.
We next examined whether baseline levels and changes in emotion regulation predicted subsequent levels and growth in psychopathology using linear regression. We used this approach, as there were only two time points at which emotion regulation was measured prior to the final measure of psychopathology.
Finally, we investigated whether patterns of emotion regulation across adolescence associated with child maltreatment were responsible for the elevated rates of internalizing and externalizing symptoms using tests of statistical mediation that evaluate direct and indirect effects in multilevel models (Bauer et al. 2006). This approach, in which the mediated effect is calculated as the product of child maltreatment effects on mediators and the effects of the mediators on psychopathology symptoms, has been demonstrated to yield more information in multi-level models than other standard mediation approaches (Krull and MacKinnon 2001; Tate and Pituch 2007).
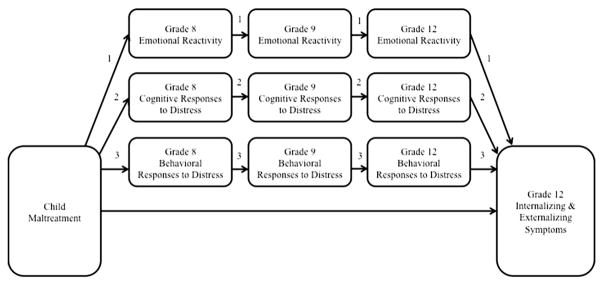
All analyses were conducted using SPSS software Version 19 and controlled for age and sex (Fig. 1).
Fig. 1.
Indirect and direct mediation pathways in Study 2. This figure illustrates the direct and indirect mediation pathways from child maltreatment to psychopathology symptoms via emotional reactivity (pathway 1), cognitive responses to distress (pathway 2), and behavioral responses to distress (pathway 3) across 5 years. Mediation paths 1, 2, and 3 were tested separately
Results
Descriptive Statistics
Table 3 provides the means and standard deviations of all measures. Please see “Appendix” Table 6 for the zero-order correlations among all measures of maltreatment exposure, emotion regulation, and symptoms of internalizing and externalizing psychopathology.
Table 3.
Means, standard deviations, and range of childhood maltreatment, emotion regulation and psychopathology variables Study 2
| Measure | Mean | (SD) | Range |
|---|---|---|---|
| 1. Maltreatment | 7.90a | .29 | 0–1 |
| 2. RRS brooding grade 8 | 10.35 | 3.05 | 5–20 |
| 3. RRS brooding grade 9 | 10.31 | 3.04 | 5–20 |
| 4. RRS brooding grade 12 | 10.60 | 3.40 | 5–20 |
| 5. DRI affective dysregulation grade 8 | 5.70 | 3.74 | 0–20 |
| 6. DRI affective dysregulation grade 9 | 6.10 | 3.86 | 0–20 |
| 7. DRI affective dysregulation grade 12 | 5.90 | 3.19 | 0–20 |
| 8. DRI behavioral dysregulation grade 8 | 4.14 | 2.67 | 0–15 |
| 9. DRI behavioral dysregulation grade 9 | 4.11 | 2.73 | 0–15 |
| 10. DRI behavioral dysregulation grade 12 | 4.23 | 2.31 | 0–15 |
| 11. YSR internalizing grade 7 | 48.65 | 9.77 | 27–84 |
| 12. YSR internalizing grade 9 | 49.95 | 9.95 | 27–84 |
| 13. YSR internalizing grade 12 | 52.09 | 10.13 | 27–91 |
| 14. YSR externalizing grade 7 | 49.39 | 10.02 | 29–78 |
| 15. YSR externalizing grade 9 | 52.31 | 10.12 | 29–83 |
| 16. YSR externalizing grade 12 | 54.52 | 9.71 | 29–83 |
| 17. CBCL internalizing grade 7 | 49.26 | 10.07 | 33–94 |
| 18. CBCL internalizing grade 9 | 50.13 | 10.46 | 33–85 |
| 19. CBCL internalizing grade 12 | 51.46 | 10.79 | 33–94 |
| 20. CBCL externalizing grade 7 | 49.24 | 9.70 | 34–74 |
| 21. CBCL externalizing grade 9 | 49.94 | 10.34 | 34–82 |
| 22. CBCL externalizing grade 12 | 50.67 | 10.62 | 34–82 |
Maltreatment childhood maltreatment exposure, RRS brooding brooding subscale of the Ruminative Responses Scale, DRI affective dysregulation Affective Dysregulation subscale of the dysregulation inventory (DRI), DRI behavioral dysregulation Behavioral Dysregulation subscale of the DRI, YSR internalizing T-scored Internalizing subscale of the youth self report, YSR externalizing T-scored Externalizing subscale of the youth self report
This number represents a percentage rather than mean score
Child Maltreatment and Psychopathology
Youth-reported internalizing and externalizing symptoms were modeled with a linear effect of time and random effects of both intercept and slopes. There was a significant effect of time on both youth-reported internalizing (β = .06, p <.001) and externalizing symptoms (β = .09, p <.001). Significant variation in intercepts was observed for both symptom types (p <.001), however significant variation in slopes was not observed for youth-reported internalizing or externalizing symptoms. Child maltreatment was associated with internalizing symptoms intercept (β = 34.98, p = .008), and changes in symptoms over time (β = .10, p = .006). In contrast, child maltreatment did not significantly predict the intercept (β = 20.18, p = .14), or slope (β = .04, p = .25) of externalizing symptoms.
Parent-reported internalizing and externalizing symptoms were modeled with a linear effect of time and random effects of both intercept and slopes. There was a significant effect of time on both parent-reported internalizing (β = .04, p <.001) and externalizing (β = .03, p = .001) symptoms. Significant variation in intercepts was observed for both symptom types (p < .001); however, significant variation in slopes was not observed for either internalizing or externalizing symptoms. Child maltreatment was associated with the parent-reported internalizing symptoms intercept (β = 38.35, p = .010), but not changes in symptoms over time (β = .01, p = .678). Child maltreatment did not significantly predict the intercept (β = 13.39, p = .367), or slope (β = .01, p = .891) of parent-reported externalizing symptoms.
Child Maltreatment and Emotion Regulation
Emotional Reactivity
For emotional reactivity, we included both linear and quadratic effects of time, with random effects for the intercept and linear slope. This model revealed marginal effects of time (β = .03, p = .073) and time squared (β < −.01, p = .069) on emotional reactivity and significant variation across adolescents in both the intercept and linear slope (p < .001). Child maltreatment was marginally associated with linear changes in emotional reactivity over time (β = .03, p = .053) but not with the quadratic growth factor (β = −.01, p = .13), or the intercept (β = 6.57, p = .155).
Habitual Cognitive Responses to Distress
The linear model including random effects of intercept and time provided the best fit to the data for the brooding subscale. Significant variation across adolescents was observed in the intercept (p < .001) of brooding. We found no significant effect of time (β = .01, p = .17) or significant change over time (p = .21) in brooding. As such, we examined maltreatment only as a predictor of variation in the intercept of brooding. Child maltreatment was associated with higher levels of brooding (β = 11.13, p = .004).
Habitual Behavioral Responses to Distress
The linear model with random effects for the intercept and slope of behavioral dysregulation fit the data best. The model indicated significant variation in intercepts and slope (p < .001), but no effect of time on behavioral dysregulation (β < .01, p = .43). Because behavioral dysregulation did not vary over time, we examined the association of maltreatment only with the intercept. Child maltreatment was marginally associated with the behavioral dysregulation intercept (β = 6.47, p = .052).
Emotion Regulation and Psychopathology
We then examined whether difficulties in each domain of emotion regulation predicted psychopathology. Because emotion regulation variables were first assessed in grade 8, only two assessments of psychopathology were conducted after that time (in grade 9 and 12). As such, we utilized linear regression instead of multi-level modeling to examine the associations of emotion regulation with psychopathology.
First, we examined whether baseline levels of emotion regulation (grade 8) predicted youth-reported internalizing and externalizing symptoms in grade 9. Grade 9 internalizing psychopathology was significantly predicted by grade 8 emotional reactivity (β = .43, p <.001), brooding (β = .32, p < .001) and dysregulated behavioral responses to distress (β = .35, p < .001). Similarly emotional reactivity (β = .41, p < .001), brooding (β = .26, p < .001) and dysregulated behavioral responses to distress (β = .49, p <.001) were significantly associated with grade 9 youth-reported externalizing symptoms.
Next, we examined whether grade 8 emotion regulation predicted youth-reported internalizing and externalizing psychopathology in grade 12 controlling for grade 9 symptom levels (i.e., change in psychopathology symptoms). Both emotional reactivity and habitual behavioral responses to distress at baseline were significantly associated with Grade 12 internalizing symptoms controlling for grade 9 symptoms (β = .10–11, p = .024–.038), however brooding was not related to changes in internalizing symptoms over time (β = .06, p = .249). None of the emotion regulation characteristics at baseline predicted Grade 12 externalizing symptoms controlling for Grade 9 symptoms (β = −.06 to .01, p = .16–86).
Examining the relation of emotion regulation at Grade 8 and parent-reported internalizing and externalizing psychopathology at Grade 9 produced a similar pattern of results. Grade 9 parent-reported internalizing psychopathology was predicted by Grade 8 emotional reactivity (β = .25, p < .001), brooding (β = .12, p = .015) and dysregulated behavioral responses to distress (β = .17, p = .001). Similarly, Grade 8 emotional reactivity (β = .24, p < .001), and dysregulated behavioral responses to distress (β = .26, p < .001), but not brooding (β = .08, p = .104), were significantly associated with Grade 9 externalizing symptoms.
In contrast, emotion regulation in Grade 8 did not significantly predict changes in parent-reported internalizing (β = .01–.04, p = .427–.929), or externalizing psychopathology (β = −.04 to .02, p = .259–.681), from grade 9 to grade 12.
Emotion Regulation as a Mechanism Linking Child Maltreatment with Psychopathology
Table 4 presents the mediating role of children’s emotion regulation on the relation between child maltreatment and psychopathology symptoms. Overall we found significant mediated effects for two of three emotion regulation dimensions, emotional reactivity and behavioral responses to distress, on both internalizing and externalizing symptoms. Specifically, the indirect effect of child maltreatment on parent-reported internalizing and parent-reported externalizing symptoms through emotional reactivity were significant (p <.001), though not for youth-reported internalizing and externalizing symptoms. We also found significant indirect effects of dysregulated behavioral responses to distress on both youth-reported internalizing (p = .013) and externalizing symptoms (p = .009), but not parent-reported symptoms of psychopathology. In contrast, we did not find evidence of mediation for brooding on symptoms of either youth-reported or parent-reported psychopathology.
Table 4.
Mediated effects by emotion regulation on internalizing and externalizing psychopathology symptoms Study 2
| Internalizing
|
Externalizing
|
|||
|---|---|---|---|---|
| Mediated effect | SE | Mediated effect | SE | |
| Youth report | ||||
| Emotional reactivity | .21 | .53 | .23 | .56 |
| Habitual cognitive responses to distress | −.32 | 1.02 | −.04 | .93 |
| Habitual behavioral responses to distress | 1.82* | .73 | 1.58** | .61 |
| Parent report | ||||
| Emotional reactivity | 1.75** | .37 | 1.52** | .36 |
| Habitual cognitive responses to distress | 1.05 | .88 | .79 | .67 |
| Habitual behavioral responses to distress | −.90 | .41 | 2.43 | 2.35 |
Mediated effect is unstandardized
p < .05;
p < .01
Given the high number of analyses, we applied a FDR correction (Benjamini and Hochberg 1995) to all analyses involving multiple dimensions of emotion regulation. All significant associations survived this correction, however the following shifted to trend-level significance: the associations of child maltreatment and the intercept of dyssregulated behavioral responses to distress (p = .078), emotional reactivity and youth-reported internalizing symptoms (p = .057), behavioral dysregulation and youth-reported internalizing symptoms (p = .057), and the indirect effects of dysregulated behavioral responses to distress on the association of child maltreatment and parent-reported internalizing symptoms (p = .071).
Study 2: Discussion
In a longitudinal community sample of adolescents, exposure to child maltreatment predicted greater average levels of internalizing symptoms as well as increases in internalizing symptoms over 5 years. Contrary to our hypotheses, child maltreatment exposure was not associated with externalizing symptoms or changes in symptoms over time. Exposure to child maltreatment was associated with higher levels of emotional reactivity and greater growth in emotional reactivity across adolescence. In contrast, levels of habitual cognitive (i.e., brooding) and behavioral (i.e., impulsive behavior) responses to distress remained stable over the follow-up period for most adolescents; child maltreatment was associated with higher levels of mal-adaptive cognitive and behavioral responses to distress.
Emotional reactivity and both measures of maladaptive habitual responses to distress in eighth grade were associated with higher levels of internalizing and externalizing symptoms at the 1-year follow up. Initial levels of emotional reactivity and habitual maladaptive behavioral responses to distress predicted increases over time in internalizing but not externalizing symptoms. In contrast, initial levels of brooding were not associated with changes in psychopathology across high school. Heightened emotional reactivity mediated the association of both parent-reported internalizing and externalizing symptoms, and habitual maladaptive behavioral responses to distress mediated the association of child maltreatment with both youth-reported internalizing and externalizing symptoms.
General Discussion
Accumulating evidence suggests that both child maltreatment and disruptions in emotion regulation are associated with a wide range of internalizing and externalizing problems (Fox et al. 2010; Green et al. 2010; McLaughlin et al. 2011, 2012; Michl et al. 2013; Nolen-Hoeksema et al. 2007; Silk et al. 2003). However, few studies have examined the role of emotion dysregulation as a transdiagnostic mechanism linking child maltreatment exposure to heightened risk for multiple forms of psychopathology. We provide converging evidence from a cross-sectional sample with a high concentration of youths exposed to severe maltreatment and a longitudinal community-based study indicating that child maltreatment is associated with multiple forms of emotion dysregulation, and that these disruptions in emotion regulation, in turn, are associated with both internalizing and externalizing psychopathology among adolescents. In both studies, child maltreatment was associated with elevated emotional reactivity and greater habitual use of maladaptive responses to distress, including rumination and impulsive behaviors. Longitudinal analyses revealed a nuanced pattern of associations such that maltreatment was associated not only with a higher overall level of emotional reactivity and greater engagement in maladaptive responses to distress, the latter of which was stable across the adolescent period, but also with greater growth in emotional reactivity across the follow-up period. Maltreatment, emotional reactivity, and behavioral responses to distress each predicted growth in internalizing but not externalizing symptoms. In addition, emotional reactivity and behavioral responses to distress significantly mediated the relation between child maltreatment and symptoms of both internalizing and externalizing psychopathology. These findings highlight the critical role of child maltreatment in shaping multiple component processes involved in emotion regulation, including emotional reactivity and maladaptive habitual responses to distress, which in turn function as vulnerability factors for internalizing and externalizing psychopathology in adolescence.
Consistent with our hypotheses and prior studies on child trauma (Lansford et al. 2002; McLaughlin et al. 2012), we found strong associations between physical, sexual, and emotional abuse and both internalizing and externalizing symptoms in the sample of youths for whom maltreatment exposure was more prevalent. In the longitudinal study, we were able to additionally examine how child maltreatment predicted symptoms of psychopathology over time. Maltreatment exposure was associated with not only level of internalizing symptoms but increases in youth-reported internalizing symptoms over time during a period of heightened vulnerability for depression and anxiety symptoms (Beesdo et al. 2009; Burke et al. 1990; Costello et al. 2003; Hankin et al. 1998; Kandel and Davies 1982; Kessler et al. 2005). In contrast, maltreatment exposure did not predict externalizing symptom levels or changes over time in the longitudinal study. This finding was surprising, as numerous prior studies have identified child maltreatment as a risk factor for the development of not only internalizing but also externalizing psychopathology (Green et al. 2010; McLaughlin et al. 2012; Molnar et al. 2001). This unexpected finding might be explained by the use of only two dichotomous items of abuse, which provide only a cursory assessment of maltreatment and did not allow us to examine different types of maltreatment or abuse frequency and severity. This may have diminished our ability to detect an association between maltreatment and externalizing symptoms in this sample given recent research indicating that adolescents exposed to multiple forms of trauma had a greater likelihood of engaging in externalizing and delinquent behavior than adolescents who had witnessed violence or were exposed to only one form of trauma (Ford et al. 2010). It is also possible that we were unable to detect an association between child maltreatment and externalizing problems because trajectories of externalizing behavior across childhood and adolescence vary based on the timing of maltreatment exposure (Keiley et al. 2001). These differing trajectories may obscure growth patterns detectable by multi-level modeling. Indeed, supplementary analyses using linear regressions revealed an overall significant association between child maltreatment and externalizing problems in the longitudinal sample.
Across both studies, we found that child maltreatment was associated with higher levels of self-reported emotional reactivity. Greater emotional reactivity among maltreated adolescents likely reflects an adaptation to early experiences of danger, resulting in lasting alterations in the salience of emotional information and heightened responding to potential threats. This finding is consistent with prior studies which have observed associations between child maltreatment and emotional reactivity using physiological measures of the autonomic nervous system and hypothalamic–pituitary–adrenal (HPA) axis among youth (Cicchetti and Rogosch 2001; De Bellis et al. 1999; Hart et al. 1996; Kaufman et al. 1997; McLaughlin et al. 2014b; Tyrka et al. 2009) and adults (Heim and Nemeroff 2001; Stein et al. 1997), as well as neuroimaging studies indicating that child maltreatment is associated with heightened amygdala response to both negative and positive emotional cues (McCrory et al. 2011, 2013). Heightened emotional arousal provides a signal that can enable the child to identify and respond to the source of their distress and may facilitate adaptive safety-seeking behaviors. If such a pattern promotes safety in situations involving threat, it is likely to be strongly reinforced over time. Our findings from the longitudinal study support this hypothesis. Child maltreatment was not only associated with higher levels of emotional reactivity but also increases in reactivity across adolescence. Adolescence is a period characterized by developmental increases in negative affect and emotional lability (Larson et al. 2002), a tighter coupling between environmental stressors and the emergence of negative affect (Larson and Ham 1992), and heightened physiological reactivity to social evaluation and academic stressors (Gunnar et al. 2009; Silk et al. 2012; Stroud et al. 2009). Our finding that child maltreatment predicts greater increases in emotional reactivity during adolescence suggests an enduring effect of childhood trauma exposure on the development of patterns of emotional responding to the environment. Together, findings from both studies support the idea that early experiences of threat in the environment are associated with increases in emotional reactivity during the adolescent period.
Child maltreatment exposure was also associated with maladaptive patterns of responding to distress in both studies. Our finding that maltreated adolescents engaged in higher levels of rumination is consistent with prior evidence suggesting that child abuse influences reliance on passive cognitive response styles rather than a more active problem-solving response style focused on remedying the cause of distress (Conway et al. 2004; Sarin and Nolen-Hoeksema 2010; Watkins 2009). Maltreated children may engage in low levels of active problem-solving because they are more likely to attribute negative life events to global, stable causes over which they have no control (Gibb 2002). Indeed, maltreatment experiences are typically uncontrollable, which may engender this type of cognitive style. Our results further suggest that maltreated youths are also more likely to engage in rash behaviors, rather than deliberate problem-solving strategies, to alleviate emotional distress. This pattern may emerge because violence perpetration by adults models problematic behavioral responses to negative emotional arousal for youth (Bingenheimer 2005; Dodge et al. 1990; McCloskey and Lichter 2003). The only form of child maltreatment that was not related to dysregulated behavioral responses to distress was sexual abuse, consistent with prior research suggesting that sexual abuse has different associations with adolescent problem behaviors than exposure to physical abuse (Riggs et al. 1990). In the longitudinal study, responses to distress—both brooding and behavioral dysregulation—were stable across the adolescent period. This finding is consistent with prior work documenting that engagement in maladaptive cognitive response styles, including rumination, is a dimension of emotion regulation that is a stable trait by 6th grade (Hankin 2008). Although we are unaware of previous research examining patterns of reliance on impulsive behavioral responses to distress across development, our findings suggest that this type of impulsive behavioral responding to distress is similarly stable by adolescence. Taken together our results indicate that maltreatment exposure is associated with elevations in emotional reactivity, greater increases in reactivity across the adolescent period, and overreliance on maladaptive emotion regulation strategies, the latter of which emerged as a stable trait during the adolescent period in our longitudinal study.
Our finding that emotional reactivity, but not use of maladaptive strategies, increased over time suggests that these are indeed distinct dimensions of emotion regulation that follow different developmental trajectories. However it is likely that emotional reactivity and maladaptive regulation transact over time and influence each other. Evidence suggests that individuals are more likely to engage in rash behaviors under heightened emotional states (e.g., Cyders and Smith 2008). Given our findings that adolescents exposed to maltreatment are more likely to experience greater emotional reactivity, it is possible that they will engage in a higher frequency of rash behaviors. Conversely, practice of adaptive emotion regulation strategies has been shown to diminish emotional reactivity (Watkins et al. 2008). It will be important for future research to disentangle not only how specific kinds of maltreatment exposure influence the development of emotional reactivity and maladaptive and adaptive regulation strategies but also employ state behavioral tasks to examine how these processes influence each other immediately and over time.
High levels of emotional reactivity and engagement in maladaptive habitual responses to distress were associated with adolescent psychopathology in both studies, although associations with externalizing problems were observed only in the cross-sectional study of adolescents with higher levels of exposure to maltreatment. In the longitudinal study, baseline levels of emotional reactivity and mal-adaptive responses to distress were associated with symptoms of psychopathology concurrently and at a 1-year follow up period. Continued growth in youth-reported internalizing symptoms, but not externalizing symptoms, across the additional 3-year follow up was predicted by initial levels of emotional reactivity and habitual behavioral responses to distress. This finding suggests that disruptions in emotion regulation are robust risk factors for symptoms of anxiety and mood pathology during a developmental period of elevated risk for these conditions (Beesdo et al. 2009; Burke et al. 1990; Costello et al. 2003; Hankin et al. 1998; Kandel and Davies 1982; Kessler et al. 2005), building on a growing body of work documenting the role of emotion regulation deficits as a transdiagnostic factor linked with multiple forms of internalizing problems (Aldao et al. 2010; McLaughlin et al. 2011). Contrary to expectations, however, brooding did not predict later increases in internalizing symptoms. The early stabilization of this facet of emotion regulation may explain its diminished influence on growth in psychopathology symptoms across adolescence, although extensive prior research has documented that rumination is associated with increases in depressive symptoms over time in both adolescents and adults (McLaughlin et al. 2011; Michl et al. 2013), as well as the onset of major depression (Nolen-Hoeksema 2000). Finally, the relations between internalizing symptoms and both child maltreatment and components of emotion regulation were stronger for youth-reported as compared to parent-reported symptoms. One explanation is simply that two measures are more likely to be correlated when they share a reporter. Alternatively, accumulating evidence suggests that adolescents are more valid reporters of internalizing problems than their parents (Achenbach et al. 1987; Cantwell et al. 1997). Future research is needed to determine how these facets of emotion regulation are associated with internalizing and externalizing psychopathology across development, and whether the associations vary across developmental stages.
Overall, our study suggests that in adolescence, disruptions in two core components of emotion regulation, emotional reactivity and habitual responses to distress, represent plausible mechanisms linking child maltreatment exposure and psychopathology. Indeed, longitudinal mediation analyses document that both emotional reactivity and impulsive responding to distress are mechanisms underlying the link between child maltreatment and both internalizing and externalizing psychopathology. Findings from these two studies provide new evidence for specific treatment targets for adolescents exposed to maltreatment. Our findings suggest that treatments—such as trauma-focused cognitive behavior therapy (TFCBT; Cohen et al. 2006)—that include techniques targeting heightened physiological and emotional reactivity (e.g., relaxation training), strategies to reduce rumination, brooding, (e.g., cognitive restructuring), and tools to reduce impulsive behavioral responses to distress (e.g., parent management training, emotion regulation skill training) are likely to be most effective at reducing maltreatment-related psychopathology. Extensive evidence supports this (Cohen et al. 2004, 2011; Silverman et al. 2008). Prevention and intervention efforts that utilize these strategies to remediate disruptions in a variety of dimensions of emotion regulation may be critical for this population of youths.
This study had many notable strengths, including replication of primary findings across two distinct samples, one including adolescents with exposure to severe maltreatment and a normative community-based sample followed over a 6 year follow-up period. However, study findings should be interpreted in light of several limitations. First, since Study 1 was cross-sectional, we were unable to establish temporal sequence or examine changes in emotion regulation and psychopathology symptoms over time. We also did not test a formal mediation model in Study 1, given the bias associated with such analyses in cross-sectional studies (Maxwell and Cole 2007). These limitations were addressed in Study 2, where we were able to use statistical mediation analyses to evaluate the direct and indirect effects of these associations over time in a multi-wave longitudinal study. Second, in both studies adolescents provided retrospective reports of their exposure to child maltreatment, introducing potential issues associated with biased recall and underreporting (Fergusson et al. 2000; Hardt and Rutter 2004; Harvey and Herman 1994). Furthermore, assessing maltreatment at the 12th grade follow up in Study 2 precludes us from establishing with certainty that the maltreatment exposure occurred before adolescents completed our measurements of emotion regulation and psychopathology at earlier time points, potentially hampering our mediational analyses. Third, in Study 2 adolescents were given a cursory assessment of child maltreatment exposure. This measurement limitation was addressed in Study 1, where experiences of child maltreatment were assessed with well-established measures. Fourth, although both studies measured emotional reactivity and habitual responses to distress, the specific measures were not identical across studies. In particular, the Behavioral Dysregulation subscale of the DRI had considerably poorer reliability than the BRI of the BRIEF. This discrepancy in reliability may be attributed to a tendency among children with behavioral problems to underreport these symptoms (Cantwell et al. 1997). This limitation was addressed in Study 1 as symptoms on the BRI were contributed by caregivers rather than participants. Additionally, the measure used to assess emotional reactivity in Study 1 included items about the persistence of emotions that may also reflect emotion regulation ability. Despite these limitations, our confidence in the results is bolstered by the similar patterns of findings across both samples. This convergence of results justifies greater support for the role of disruptions in emotion regulation as a transdiagnostic mechanism linking child maltreatment to internalizing and externalizing symptoms during adolescence.
Across multiple studies, we observed consistent associations between child maltreatment exposure, heightened emotional reactivity, and maladaptive responses to distress, measured both cross-sectionally and longitudinally. These patterns of emotion dysregulation, in turn, were associated with higher levels of internalizing and externalizing psychopathology, suggesting a transdiagnostic pathway linking child maltreatment to psychopathology through disruptions in emotion regulation. These findings suggest the importance of targeting emotion regulation in interventions aimed at preventing the onset of mental health problems in youths who have been maltreated.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health to Ann Vander Stoep and Eliza-beth McCauley (MH-663711 and MH-079402) and Katie McLaughlin (MH-092526).
Appendix
Table 5.
Correlations of childhood maltreatment, emotion regulation, and psychopathology Study 1
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. CTQ total | – | ||||||
| 2. CTQ PA | .77** | – | |||||
| 3. CTQ SA | .72** | .36** | – | ||||
| 4. CTQ EA | .87** | .59** | .37** | – | |||
| 5. BRIEF BRI | .13 | .15 | −.07 | .23* | – | ||
| 6. ERS sensitivity | .35** | .18* | .23* | .38** | .19* | – | |
| 7. ERS arousal | .39** | .22* | .26** | .41** | .16* | .77** | – |
| 8. ERS persistence | .31** | .21* | .17 | .33* | .19* | .73** | .76** |
| 9. ERS total | .39** | .22* | .25** | .41** | .19* | .94** | .92** |
| 10. CRSQ rumination | .34** | .19* | .26** | .32** | .16* | .51** | .50** |
| 11. YSR internalizing | .39** | .23* | .22* | .44** | .18* | .61** | .54** |
| 12. YSR externalizing | .39** | .24* | .23* | .43** | .22** | .51** | .48** |
| 13. CBCL internalizing | .10 | .05 | .02 | .14 | .50** | .33** | .22** |
| 14. CBCL externalizing | .21* | .11 | .02 | .31** | .64** | .29** | .28** |
|
| |||||||
| 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|
| |||||||
| 1. CTQ total | |||||||
| 2. CTQ PA | |||||||
| 3. CTQ SA | |||||||
| 4. CTQ EA | |||||||
| 5. BRIEF BRI | |||||||
| 6. ERS sensitivity | |||||||
| 7. ERS arousal | |||||||
| 8. ERS persistence | – | ||||||
| 9. ERS total | .87** | – | |||||
| 10. CRSQ rumination | .51** | .55** | – | ||||
| 11. YSR internalizing | .50** | .61** | .49** | – | |||
| 12. YSR externalizing | .48** | .54** | .36** | .54** | – | ||
| 13. CBCL internalizing | .24* | .30** | .26** | .36** | .24* | – | |
| 14. CBCL externalizing | .28** | .31** | .20* | .16* | .45** | .62** | – |
CTQ Childhood Trauma Questionnaire, PA physical abuse, SA sexual abuse, EA emotional abuse, ERS sensitivity Emotion Reactivity Scale sensitivity subscale, ERS arousal Emotion Reactivity Scale arousal/intensity subscale, ERS persistence Emotion Reactivity Scale persistence subscale, ERS total score Emotion Reactivity scale total score, CRSQ rumination Children’s Response Styles Questionnaire rumination subscale, YSR internalizing youth self report form of the Child Behavior Checklist internalizing subscale, YSR externalizing Youth self report form of the Child Behavior Checklist externalizing subscale
p < .05;
p < .001
Table 6.
Correlations of maltreatment exposure, emotion regulation, and psychopathology Study 2
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Maltreatment | – | ||||||||||
| 2. RRS brooding grade 8 | .07 | – | |||||||||
| 3. RRS brooding grade 9 | .13** | .50** | – | ||||||||
| 4. RRS brooding grade 12 | .17** | .34** | .38** | – | |||||||
| 5. DRI affective dysregulation grade 8 | .03 | .42** | .29** | .27** | – | ||||||
| 6. DRI affective dysregulation grade 9 | .12* | .33** | .43** | .29** | .56** | – | |||||
| 7. DRI affective dysregulation grade 12 | .13** | .20** | .28** | .43** | .39** | .49** | – | ||||
| 8. DRI behavioral dysregulation grade 8 | .07 | .32** | .15** | .16** | .67** | .43** | .30** | – | |||
| 9. DRI behavioral dysregulation grade 9 | .11* | .22** | .20** | .14** | .43** | .61** | .39** | .57** | – | ||
| 10. DRI behavioral dysregulation grade 12 | .04 | .14** | .06 | .19** | .20** | .30** | .52** | .30** | .47** | – | |
| 11. YSR internalizing grade 7 | .06 | .32** | .24** | .29** | .51** | .40** | .31** | .36** | .28** | .17** | – |
| 12. YSR internalizing grade 9 | .07 | .33** | .40** | .31** | .44** | .55** | .40** | .35** | .40** | .20** | .59** |
| 13. YSR internalizing grade 12 | .19** | .19** | .20** | .45** | .30** | .32** | .60** | .28** | .28** | .37** | .41** |
| 14. YSR externalizing grade 7 | .16** | .24** | .21** | .18** | .43** | .37** | .28** | .49** | .45** | .27** | .54** |
| 15. YSR externalizing grade 9 | .20** | .26** | .27** | .21** | .41** | .49** | .37** | .49** | .62** | .37** | .35** |
| 16. YSR externalizing grade 12 | .17** | .15** | .14** | .29** | .23** | .29** | .49** | .30** | .44** | .56** | .22** |
| 17. CBCL internalizing grade 7 | .07 | .06 | .01 | .14** | .23** | .13* | .23** | .18* | .14** | .22** | .30** |
| 18. CBCL internalizing grade 9 | .10* | .12* | .09 | .15** | .24** | .24** | .25** | .17** | .19** | .15** | .30** |
| 19. CBCL internalizing grade 12 | .08 | .10 | .08 | .19** | .16** | .24** | .33** | .10* | .19** | .20** | .23** |
| 20. CBCL externalizing grade 7 | .16** | .13** | .01 | .07 | .19** | .15** | .19** | .26** | .23** | .24** | .16** |
| 21. CBCL externalizing grade 9 | .15** | .08 | .01 | .07 | .24** | .22** | .25** | .27** | .32** | .25** | .17** |
| 22. CBCL externalizing grade 12 | .12* | .08 | .07 | .13** | .12* | .19** | .28** | .14* | .29** | .29** | .10* |
|
| |||||||||||
| 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | |
|
| |||||||||||
| 1. Maltreatment | |||||||||||
| 2. RRS brooding grade 8 | |||||||||||
| 3. RRS brooding grade 9 | |||||||||||
| 4. RRS brooding grade 12 | |||||||||||
| 5. DRI affective dysregulation grade 8 | |||||||||||
| 6. DRI affective dysregulation grade 9 | |||||||||||
| 7. DRI affective dysregulation grade 12 | |||||||||||
| 8. DRI behavioral dysregulation grade 8 | |||||||||||
| 9. DRI behavioral dysregulation grade 9 | |||||||||||
| 10. DRI behavioral dysregulation grade 12 | |||||||||||
| 11. YSR internalizing grade 7 | |||||||||||
| 12. YSR internalizing grade 9 | – | ||||||||||
| 13. YSR internalizing grade 12 | .54** | – | |||||||||
| 14. YSR externalizing grade 7 | .36** | .30** | – | ||||||||
| 15. YSR externalizing grade 9 | .53** | .29** | .66** | – | |||||||
| 16. YSR externalizing grade 12 | .28** | .48** | .49** | .65** | – | ||||||
| 17. CBCL internalizing grade 7 | .19** | .23** | .17** | .14** | .11 | – | |||||
| 18. CBCL internalizing grade 9 | .31** | .29** | .22** | .23** | .16** | .66** | – | ||||
| 19. CBCL internalizing grade 12 | .22** | .36*8 | .20** | .19** | .19** | .58** | .62** | – | |||
| 20. CBCL externalizing grade 7 | .15** | .17** | .39** | .37** | .32** | .58** | .45** | .44** | – | ||
| 21. CBCL externalizing grade 9 | .16** | .19** | .37** | .44** | .39** | .47** | .59** | .44** | .78** | – | |
| 22. CBCL externalizing grade 12 | .09 | .19** | .32** | .42** | .50** | .33** | .42** | .57** | .63** | .71** | – |
Maltreatment childhood maltreatment exposure; RRS brooding brooding subscale of the Ruminative Responses scale, DRI affective dysregulation Affective Dysregulation subscale of the dysregulation inventory (DRI), DRI behavioral dysregulation Behavioral Dysregulation subscale of the DRI, YSR internalizing T-scored Internalizing subscale of the youth self report, YSR externalizing T-scored Externalizing subscale of the youth self report, CBCL internalizing T-scored internalizing subscale of the child behavior checklist, CBCL externalizing T-scored Externalizing subscale of the child behavior checklist
p < .05;
p < .001
Table 7.
Measures at each time point in Study 2
| Measure | 7th grade | 8th grade | 9th grade | 12th grade |
|---|---|---|---|---|
| Demographics | S P |
|||
| Child maltreatment | S | |||
| Dysregulation inventory (DRI): Affective and Behavioral Dysregulation subscales | S | S | S | |
| Ruminative Responses scale (RRS) | S | S | S | |
| Child behavior checklist (CBCL) | P | P | P | |
| Youth self report (YSR) | S | S | S |
P parent-report, S adolescent self-report
Footnotes
Compliance with Ethical Standards
Conflict of Interest Charlotte Heleniak, Jessica L. Jenness, Ann Vander Stoep, Elizabeth McCauley and Katie A. McLaughlin declare that they have no conflict of interest.
Informed Consent All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (national and institutional). Informed consent was obtained from all individual subjects participating in the study.
Animal Rights No animal studies were carried out by the authors for this article.
References
- Abela JR, Brozina K, Haigh EP. An examination of the response styles theory of depression in third- and seventh-grade children: A short-term longitudinal study. Journal of Abnormal Child Psychology. 2002;30(5):515–527. doi: 10.1023/A:1019873015594. [DOI] [PubMed] [Google Scholar]
- Achenbach TM. Integrative guide for the 1991 CBCL/4–18, YSR, and TRF profiles. Burlington: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin. 1987;101(2):213–232. [PubMed] [Google Scholar]
- Achenbach TM, Rescorla L. ASEBA school-age forms & profiles. Burlington: ASEBA; 2001. http://aseba.com/ordering/ASEBA%20Reliability%20and%20Validity-School%20Age.pdf. [Google Scholar]
- Adrian M, Zeman J, Erdley C, Lisa L, Sim L. Emotional dysregulation and interpersonal difficulties as risk factors for nonsuicidal self-injury in adolescent girls. Journal of Abnormal Child Psychology. 2011;39(3):389–400. doi: 10.1007/s10802-010-9465-3. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30(2):217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Anestis MD, Selby EA, Joiner TE. The role of urgency in maladaptive behaviors. Behaviour Research and Therapy. 2007;45(12):3018–3029. doi: 10.1016/j.brat.2007.08.012. [DOI] [PubMed] [Google Scholar]
- Anthony JL, Lonigan CJ, Hooe ES, Phillips BM. An affect-based, hierarchical model of temperament and its relations with internalizing symptomatology. Journal of Clinical Child and Adolescent Psychology. 2002;31(4):480–490. doi: 10.1207/S15374424JCCP3104_7. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Preacher KJ, Gil KM. Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: New procedures and recommendations. Psychological Methods. 2006;11(2):142–163. doi: 10.1037/1082-989X.11.2.142. [DOI] [PubMed] [Google Scholar]
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America. 2009;32(3):483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender PK, Reinholdt-Dunne ML, Esbjørn BH, Pons F. Emotion dysregulation and anxiety in children and adolescents: Gender differences. Personality and Individual Differences. 2012;53(3):284–288. doi: 10.1016/j.paid.2012.03.027. [DOI] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. Series B (Methodological) 1995 doi: 10.2307/2346101. [DOI] [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(3):340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. The American Journal of Psychiatry. 1994;151(8):1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bifulco A, Brown GW, Harris TO. Childhood Experience of Care and Abuse (CECA): A retrospective interview measure. Journal of Child Psychology and Psychiatry. 1994;35(8):1419–1435. doi: 10.1111/j.1469-7610.1994.tb01284.x. [DOI] [PubMed] [Google Scholar]
- Bifulco A, Brown GW, Lillie A, Jarvis J. Memories of childhood neglect and abuse: Corroboration in a series of sisters. Journal of Child Psychology and Psychiatry. 1997;38(3):365–374. doi: 10.1111/j.1469-7610.1997.tb01520.x. [DOI] [PubMed] [Google Scholar]
- Bingenheimer JB. Firearm violence exposure and serious violent behavior. Science. 2005;308(5726):1323–1326. doi: 10.1126/science.1110096. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Vallance H. Self-discrepancies in young adults and childhood violence. Journal of Interpersonal Violence. 1997;12(4):600–606. doi: 10.1177/088626097012004008. [DOI] [Google Scholar]
- Broderick PC, Korteland C. A prospective study of rumination and depression in early adolescence. Clinical Child Psychology and Psychiatry. 2004;9(3):383–394. doi: 10.1177/1359104504043920. [DOI] [Google Scholar]
- Brown J, Cohen P, Johnson JG, Smailes EM. Childhood abuse and neglect: Specificity of effects on adolescent and young adult depression and suicidality. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(12):1490–1496. doi: 10.1097/00004583-199912000-00009. [DOI] [PubMed] [Google Scholar]
- Burke KC, Burke JD, Regier DA, Rae DS. Age at onset of selected mental disorders in five community populations. Archives of General Psychiatry. 1990;47(6):511–518. doi: 10.1001/archpsyc.1990.01810180011002. [DOI] [PubMed] [Google Scholar]
- Cantwell DP, Lewinsohn PM, Rohde P, Seeley JR. Correspondence between adolescent report and parent report of psychiatric diagnostic data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(5):610–619. doi: 10.1097/00004583-199705000-00011. [DOI] [PubMed] [Google Scholar]
- Chen WJ, Faraone SV, Biederman J, Tsuang MT. Diagnostic accuracy of the Child Behavior Checklist scales for attention-deficit hyperactivity disorder: A receiver-operating characteristic analysis. Journal of Consulting and Clinical Psychology. 1994;62(5):1017. doi: 10.1037/0022-006X.62.5.1017. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. The impact of child maltreatment and psychopathology on neuroendocrine functioning. Development and Psychopathology. 2001;13(4):783–804. [PubMed] [Google Scholar]
- Cohen P, Brown J, Smailes E. Child abuse and neglect and the development of mental disorders in the general population. Development and Psychopathology. 2001;13(4):981–999. [PubMed] [Google Scholar]
- Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(4):393–402. doi: 10.1097/00004583-200404000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Deblinger E. Treating trauma and traumatic grief in children and adolescents. New York: Guilford Press; 2006. [Google Scholar]
- Cohen J, Mannarino A, Iyengar S. Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence: A randomized controlled trial. Archives of Pediatrics and Adolescent Medicine. 2011;165(1):16–21. doi: 10.1001/archpediatrics.2010.247. [DOI] [PubMed] [Google Scholar]
- Cole PM, Martin SE, Dennis TA. Emotion regulation as a scientific construct: Methodological challenges and directions for child development research. Child Development. 2004;75(2):317–333. doi: 10.1111/j.1467-8624.2004.00673.x. [DOI] [PubMed] [Google Scholar]
- Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin. 2001;127(1):87–127. doi: 10.1037//0033-2909.127.1.87. [DOI] [PubMed] [Google Scholar]
- Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology. 2000;68(6):976–992. doi: 10.1037//0022-006X.68.6.976. [DOI] [PubMed] [Google Scholar]
- Conway M, Mendelson M, Giannopoulos C, Csank PAR, Holm SL. Childhood and adult sexual abuse, rumination on sadness, and dysphoria. Child Abuse and Neglect. 2004;28(4):393–410. doi: 10.1016/j.chiabu.2003.05.004. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Smith GT. Emotion-based dispositions to rash action: Positive and negative urgency. Psychological Bulletin. 2008;134(6):807–828. doi: 10.1037/a0013341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ. Affective neuroscience and psychophysiology: Toward a synthesis. Psychophysiology. 2003;40(5):655–665. doi: 10.1111/1469-8986.00067. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Baum AS, Birmaher B, Keshavan MS, Eccard CH, Boring AM, et al. Developmental traumatology part I: Biological stress systems. Biological Psychiatry. 1999;45(10):1259–1270. doi: 10.1016/S0006-3223(99)00044-X. [DOI] [PubMed] [Google Scholar]
- Denham SA, Mitchell-Copeland J, Strandberg K, Auerbach S, Blair K. Parental contributions to preschoolers’ emotional competence: Direct and indirect effects. Motivation and Emotion. 1997;21(1):65–86. doi: 10.1023/A:1024426431247. [DOI] [Google Scholar]
- Depue RA. A neurobiological framework for the structure of personality and emotion: Implications for personality disorders. In: Clarkin JF, Lenzenweger MF, editors. Major theories of personality disorder. New York, NY: Guilford Press; 1996. pp. 347–390. [Google Scholar]
- Dodge KA, Bates JE, Pettit GS. Mechanisms in the cycle of violence. Science. 1990;250(4988):1678–1683. doi: 10.1126/science.2270481. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL. Parental socialization of emotion. Psychological Inquiry. 1998;9(4):241–273. doi: 10.1207/s15327965pli0904_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA. Mothers’ reactions to children’s negative emotions: Relations to children’s temperament and anger behavior. Merrill-Palmer Quarterly. 1994;40(1):138–156. [Google Scholar]
- Eisenberg N, Fabes RA, Carlo G, Karbon M. Emotional responsivity to others: Behavioral correlates and socialization antecedents. New Directions for Child and Adolescent Development. 1992;1992(55):57–73. doi: 10.1002/cd.23219925506. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Guthrie IK, Reiser M. Dispositional emotionality and regulation: Their role in predicting quality of social functioning. Journal of Personality and Social Psychology. 2000;78(1):136–157. doi: 10.1037/0022-3514.78.1.136. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Murphy BC. Parents’ reactions to children’s negative emotions: Relations to children’s social competence and comforting behavior. Child Development. 1996;67(5):2227–2247. [PubMed] [Google Scholar]
- Ferguson GM, Hafen CA, Laursen B. Adolescent psychological and academic adjustment as a function of discrepancies between actual and ideal self-perceptions. Journal of Youth and Adolescence. 2010;39(12):1485–1497. doi: 10.1007/s10964-009-9461-5. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Woodward LJ. The stability of child abuse reports: A longitudinal study of the reporting behaviour of young adults. Psychological Medicine. 2000;30(03):529–544. doi: 10.1017/s0033291799002111. [DOI] [PubMed] [Google Scholar]
- Ford JD. Assessing child and adolescent complex traumatic stress reactions. Journal of Child & Adolescent Trauma. 2011;4(3):217–232. doi: 10.1080/19361521.2011.597080. [DOI] [Google Scholar]
- Ford JD, Elhai JD, Connor DF, Frueh BC. Polyvictimization and risk of posttraumatic, depressive, and substance use disorders and involvement in delinquency in a national sample of adolescents. Journal of Adolescent Health. 2010;46(6):545–552. doi: 10.1016/j.jadohealth.2009.11.212. [DOI] [PubMed] [Google Scholar]
- Fox JK, Halpern LF, Ryan JL, Lowe KA. Stressful life events and the tripartite model: Relations to anxiety and depression in adolescent females. Journal of Adolescence. 2010;33(1):43–54. doi: 10.1016/j.adolescence.2009.05.009. [DOI] [PubMed] [Google Scholar]
- Garber J, Braafladt N, Zeman J. The regulation of sad affect: An information-processing perspective. In: Garber J, Dodge KA, editors. The development of emotion regulation and dysregulation. New York, NY: Cambridge University Press; 1991. pp. 208–240. [Google Scholar]
- Gee DG, Gabard-Durnam LJ, Flannery J, Goff B, Humphreys KL, Telzer EH, et al. Early developmental emergence of human amygdala–prefrontal connectivity after maternal deprivation. Proceedings of the National Academy of Sciences. 2013;110(39):15638–15643. doi: 10.1073/pnas.1307893110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibb BE. Childhood maltreatment and negative cognitive styles: A quantitative and qualitative review. Clinical Psychology Review. 2002;22(2):223–246. doi: 10.1016/S0272-7358(01)00088-5. [DOI] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, Kenworthy L. Test review behavior rating inventory of executive function. Child Neuropsychology. 2000;6(3):235–238. doi: 10.1076/chin.6.3.235.3152. [DOI] [PubMed] [Google Scholar]
- Glaser JP, van Os J, Portegijs PJM, Myin-Germeys I. Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. Journal of Psychosomatic Research. 2006;61(2):229–236. doi: 10.1016/j.jpsychores.2006.04.014. [DOI] [PubMed] [Google Scholar]
- Gottman JM, Katz LF, Hooven C. Meta-emotion: How families communicate emotionally. Hillsdale, NJ: Lawrence Erlbaum; 1997. [Google Scholar]
- Grabe S, Hyde JS, Lindberg SM. Body objectification and depression in adolescents: The role of gender, shame, and rumination. Psychology of Women Quarterly. 2007;31(2):164–175. doi: 10.1111/j.1471-6402.2007.00350.x. [DOI] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the national comorbidity survey replication (NCS-R) I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry. 2010;67(2):113. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ. The emerging field of emotion regulation: An integrative review. Review of General Psychology. 1998;2(3):271–299. doi: 10.1037/1089-2680.2.3.271. [DOI] [Google Scholar]
- Gunnar MR, Frenn K, Wewerka SS, Van Ryzin MJ. Moderate versus severe early life stress: Associations with stress reactivity and regulation in 10–12-year-old children. Psychoneuroendocrinology. 2009;34(1):62–75. doi: 10.1016/j.psyneuen.2008.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajcak G, Moser JS, Holroyd CB, Simons RF. It’s worse than you thought: The feedback negativity and violations of reward prediction in gambling tasks. Psychophysiology. 2007;44(6):905–912. doi: 10.1111/j.1469-8986.2007.00567.x. [DOI] [PubMed] [Google Scholar]
- Hankin BL. Cognitive vulnerability–stress model of depression during adolescence: Investigating depressive symptom specificity in a multi-wave prospective study. Journal of Abnormal Child Psychology. 2008;36(7):999–1014. doi: 10.1007/s10802-008-9228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;107(1):128–140. doi: 10.1037/0021-843X.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2004;45(2):260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Hart J, Gunnar M, Cicchetti D. Altered neuroendocrine activity in maltreated children related to symptoms of depression. Development and Psychopathology. 1996;8(01):201–214. doi: 10.1017/S0954579400007045. [DOI] [Google Scholar]
- Harvey MR, Herman JL. Amnesia, partial amnesia, and delayed recall among adult survivors of childhood trauma. Consciousness and Cognition. 1994;3(3–4):295–306. doi: 10.1006/ccog.1994.1017. [DOI] [Google Scholar]
- Hayes AF, Glynn CJ, Huge ME. Cautions regarding the interpretation of regression coefficients and hypothesis tests in linear models with interactions. Communication Methods and Measures. 2012;6(1):1–11. doi: 10.1080/19312458.2012.651415. [DOI] [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110(1):86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: Preclinical and clinical studies. Biological Psychiatry. 2001;49(12):1023–1039. doi: 10.1016/S0006-3223(01)01157-X. [DOI] [PubMed] [Google Scholar]
- Heleniak C, King KM, Monahan K, McLaughlin KA. Disruptions in emotion regulation as a mechanism linking community violence exposure to internalizing problems in adolescents. 2015 doi: 10.1111/jora.12328. submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hessler D, Katz LF. Brief Report: Associations between emotional competence and adolescent risky behavior. Journal of Adolescence. 2010;33(1):241. doi: 10.1016/j.adolescence.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isquith PK, Roth RM, Gioia G. Contribution of rating scales to the assessment of executive functions. Applied Neuropsychology: Child. 2013;2(2):125–132. doi: 10.1080/21622965.2013.748389. [DOI] [PubMed] [Google Scholar]
- Isquith PK, Roth RM, Kenworthy L, Gioia G. Contribution of rating scales to intervention for executive dysfunction. Applied Neuropsychology: Child. 2014;3(3):197–204. doi: 10.1080/21622965.2013.870014. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Davies M. Epidemiology of depressive mood in adolescents: An empirical study. Archives of General Psychiatry. 1982;39(10):1205–1212. doi: 10.1001/archpsyc.1982.04290100065011. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keiley MK, Howe TR, Dodge KA, Bates JE, Pettit GS. The timing of child physical maltreatment: A cross-domain growth analysis of impact on adolescent externalizing and internalizing problems. Development and Psychopathology. 2001;13(4):891–912. [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kim J, Cicchetti D. Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology: Pathways linking maltreatment, emotion regulation, and psychopathology. Journal of Child Psychology and Psychiatry. 2009;51(6):706–716. doi: 10.1111/j.1469-7610.2009.02202.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King KM, Karyadi KA, Luk JW, Patock-Peckham JA. Dispositions to rash action moderate the associations between concurrent drinking, depressive symptoms, and alcohol problems during emerging adulthood. Psychology of Addictive Behaviors. 2011;25(3):446–454. doi: 10.1037/a0023777. [DOI] [PubMed] [Google Scholar]
- Krull JL, MacKinnon DP. Multilevel modeling of individual and group level mediated effects. Multivariate Behavioral Research. 2001;36(2):249–277. doi: 10.1207/S15327906MBR3602_06. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Watkins E, Holden E, Cook W. Rumination in adolescents at risk for depression. Journal of Affective Disorders. 2006;96(1–2):39–47. doi: 10.1016/j.jad.2006.05.017. [DOI] [PubMed] [Google Scholar]
- Lansford JE, Dodge KA, Pettit GS, Bates JE, Crozier J, Kaplow J. A 12-year prospective study of the long-term effects of early child physical maltreatment on psychological, behavioral, and academic problems in adolescence. Archives of Pediatrics and Adolescent Medicine. 2002;156(8):824–830. doi: 10.1001/archpedi.156.8.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson R, Ham M. Stress and “storm and stress” in early adolescence: The relationship of negative events with dysphoric affect. Developmental Psychology. 1992;29(1):130–140. doi: 10.1037/0012-1649.29.1.130. [DOI] [Google Scholar]
- Larson RW, Moneta G, Richards MH, Wilson S. Continuity, stability, and change in daily emotional experience across adolescence. Child Development. 2002;73(4):1151–1165. doi: 10.1111/1467-8624.00464. [DOI] [PubMed] [Google Scholar]
- Maughan A, Cicchetti D. Impact of child maltreatment and interadult violence on children’s emotion regulation abilities and socioemotional adjustment. Child Development. 2002;73(5):1525–1542. doi: 10.1111/1467-8624.00488. [DOI] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods. 2007;12(1):23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- McCarty CA, Wymbs BT, King KM, Mason WA, Vander Stoep A, McCauley E, et al. Developmental consistency in associations between depressive symptoms and alcohol use in early adolescence. Journal of Studies on Alcohol and Drugs. 2012;73(3):444–453. doi: 10.15288/jsad.2012.73.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCloskey LA, Lichter EL. The contribution of marital violence to adolescent aggression across different relationships. Journal of Interpersonal Violence. 2003;18(4):390–412. doi: 10.1177/0886260503251179. [DOI] [Google Scholar]
- McCrory EJ, De Brito SA, Kelly PA, Bird G, Sebastian CL, Mechelli A, et al. Amygdala activation in maltreated children during pre-attentive emotional processing. The British Journal of Psychiatry. 2013;202(4):269–276. doi: 10.1192/bjp.bp.112.116624. [DOI] [PubMed] [Google Scholar]
- McCrory EJ, De Brito SA, Sebastian CL, Mechelli A, Bird G, Kelly PA, Viding E. Heightened neural reactivity to threat in child victims of family violence. Current Biology. 2011;21(23):R947–R948. doi: 10.1016/j.cub.2011.10.015. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Aldao A, Wisco BE, Hilt LM. Rumination as a transdiagnostic factor underlying transitions between internalizing symptoms and aggressive behavior in early adolescents. Journal of Abnormal Psychology. 2014a;123(1):13–23. doi: 10.1037/a0035358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Archives of General Psychiatry. 2012;69(11):1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML. Mechanisms linking stressful life events and mental health problems in a prospective, community-based sample of adolescents. Journal of Adolescent Health. 2009;44(2):153–160. doi: 10.1016/j.jadohealth.2008.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Hilt LM. Emotion dysregulation as a mechanism linking peer victimization to internalizing symptoms in adolescents. Journal of Consulting and Clinical Psychology. 2009;77(5):894–904. doi: 10.1037/a0015760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Mennin DS, Nolen-Hoeksema S. Emotion dysregulation and adolescent psychopathology: A prospective study. Behaviour Research and Therapy. 2011;49(9):544–554. doi: 10.1016/j.brat.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA, Alves S, Mendes WB. Child maltreatment and autonomic nervous system reactivity: Identifying dysregulated stress reactivity patterns by using the biopsychosocial model of challenge and threat. Psychosomatic Medicine. 2014b;76(7):538–546. doi: 10.1097/PSY.0000000000000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnick SM, Hinshaw SP. Emotion regulation and parenting in AD/HD and comparison boys: Linkages with social behaviors and peer preference. Journal of Abnormal Child Psychology. 2000;28(1):73–86. doi: 10.1023/a:1005174102794. [DOI] [PubMed] [Google Scholar]
- Mezzich AC, Tarter RE, Giancola PR, Kirisci L. The dysregulation inventory: A new scale to assess the risk for substance use disorder. Journal of Child & Adolescent Substance Abuse. 2001;10(4):35–43. doi: 10.1300/J029v10n04_04. [DOI] [Google Scholar]
- Michl LC, McLaughlin KA, Shepherd K, Nolen-Hoeksema S. Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: Longitudinal evidence in early adolescents and adults. Journal of Abnormal Psychology. 2013;122(2):339–352. doi: 10.1037/a0031994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: Results from the National Comorbidity Survey. American Journal of Public Health. 2001;91(5):753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson CA, Bloom FE, Cameron JL, Amaral D, Dahl RE, Pine D. An integrative, multidisciplinary approach to the study of brain–behavior relations in the context of typical and atypical development. Development and Psychopathology. 2002;14(3):499–520. doi: 10.1017/s0954579402003061. [DOI] [PubMed] [Google Scholar]
- Nock MK, Wedig MM, Holmberg EB, Hooley JM. The emotion reactivity scale: Development, evaluation, and relation to self-injurious thoughts and behaviors. Behavior Therapy. 2008;39(2):107–116. doi: 10.1016/j.beth.2007.05.005. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology. 2000;109(3):504–511. doi: 10.1037/0021-843X.109.3.504. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta earthquake. Journal of Personality and Social Psychology. 1991;61(1):115. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Stice E, Wade E, Bohon C. Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in female adolescents. Journal of Abnormal Psychology. 2007;116(1):198–207. doi: 10.1037/0021-843X.116.1.198. [DOI] [PubMed] [Google Scholar]
- Oshri A, Sutton TE, Clay-Warner J, Miller JD. Child maltreatment types and risk behaviors: Associations with attachment style and emotion regulation dimensions. Personality and Individual Differences. 2015;73:127–133. doi: 10.1016/j.paid.2014.09.015. [DOI] [Google Scholar]
- Papadakis AA, Prince RP, Jones NP, Strauman TJ. Self-regulation, rumination, and vulnerability to depression in adolescent girls. Development and Psychopathology. 2006 doi: 10.1017/S0954579406060408. [DOI] [PubMed] [Google Scholar]
- Paulussen-Hoogeboom M, Stams GJ, Hermanns J, Peetsma T. Child negative emotionality and parenting from infancy to preschool: A meta-analytic review. Developmental Psychology. 2007;43(2):438–453. doi: 10.1037/0012-1649.43.2.438. [DOI] [PubMed] [Google Scholar]
- Phillips BM, Lonigan CJ, Driscoll K, Hooe ES. Positive and negative affectivity in children: A multitrait–multimethod investigation. Journal of Clinical Child and Adolescent Psychology. 2002;31(4):465–479. doi: 10.1207/S15374424JCCP3104_6. [DOI] [PubMed] [Google Scholar]
- Pollak SD, Kistler DJ. Early experience is associated with the development of categorical representations for facial expressions of emotion. Proceedings of the National Academy of Sciences. 2002;99(13):9072–9076. doi: 10.1073/pnas.142165999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak SD, Tolley-Schell SA. Selective attention to facial emotion in physically abused children. Journal of Abnormal Psychology. 2003;112(3):323–338. doi: 10.1037/0021-843X.112.3.323. [DOI] [PubMed] [Google Scholar]
- Riggs S, Alario AJ, McHorney C. Health risk behaviors and attempted suicide in adolescents who report prior maltreatment. The Journal of Pediatrics. 1990;116(5):815–821. doi: 10.1016/S0022-3476(05)82679-4. [DOI] [PubMed] [Google Scholar]
- Robinson LR, Morris AS, Heller SS, Scheeringa MS, Boris NW, Smyke AT. Relations between emotion regulation, parenting, and psychopathology in young maltreated children in out of home care. Journal of Child and Family Studies. 2008;18(4):421–434. doi: 10.1007/s10826-008-9246-6. [DOI] [Google Scholar]
- Rood L, Roelofs J, Bögels SM, Nolen-Hoeksema S, Schouten E. The influence of emotion-focused rumination and distraction on depressive symptoms in non-clinical youth: A meta-analytic review. Clinical Psychology Review. 2009;29(7):607–616. doi: 10.1016/j.cpr.2009.07.001. [DOI] [PubMed] [Google Scholar]
- Roth RM, Erdodi LA, McCulloch LJ, Isquith PK. Much ado about norming: The behavior rating inventory of executive function. Child Neuropsychology. 2015;21(2):225–233. doi: 10.1080/09297049.2014.897318. [DOI] [PubMed] [Google Scholar]
- Sarin S, Nolen-Hoeksema S. The dangers of dwelling: An examination of the relationship between rumination and consumptive coping in survivors of childhood sexual abuse. Cognition and Emotion. 2010;24(1):71–85. doi: 10.1080/02699930802563668. [DOI] [Google Scholar]
- Seligman LD, Ollendick TH, Langley AK, Baldacci HB. The utility of measures of child and adolescent anxiety: A meta-analytic review of the Revised Children’s Manifest Anxiety Scale, the state-trait anxiety inventory for children, and the child behavior checklist. Journal of Clinical Child and Adolescent Psychology. 2004;33(3):557–565. doi: 10.1207/s15374424jccp3303_13. [DOI] [PubMed] [Google Scholar]
- Silk JS, Shaw DS, Skuban EM, Oland AA, Kovacs M. Emotion regulation strategies in offspring of childhood-onset depressed mothers. Journal of Child Psychology and Psychiatry. 2006;47(1):69–78. doi: 10.1111/j.1469-7610.2005.01440.x. [DOI] [PubMed] [Google Scholar]
- Silk JS, Steinberg L, Morris AS. Adolescents’ emotion regulation in daily life: Links to depressive symptoms and problem behavior. Child Development. 2003;74(6):1869–1880. doi: 10.1046/j.1467-8624.2003.00643.x. [DOI] [PubMed] [Google Scholar]
- Silk JS, Stroud LR, Siegle GJ, Dahl RE, Lee KH, Nelson EE. Peer acceptance and rejection through the eyes of youth: Pupillary, eyetracking and ecological data from the chatroom interact task. Social Cognitive and Affective Neuroscience. 2012;7(1):93–105. doi: 10.1093/scan/nsr044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, Ortiz CD, Viswesvaran C, Burns BJ, Kolko DJ, Putnam FW, Amaya-Jackson L. Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child & Adolescent Psychology. 2008;37(1):156–183. doi: 10.1080/15374410701818293. [DOI] [PubMed] [Google Scholar]
- Singh AL, Waldman ID. The etiology of associations between negative emotionality and childhood externalizing disorders. Journal of Abnormal Psychology. 2010;119(2):376–388. doi: 10.1037/a0019342. [DOI] [PubMed] [Google Scholar]
- Stein MB, Koverola C, Hanna C, Torchia MG, McClarty B. Hippocampal volume in women victimized by childhood sexual abuse. Psychological Medicine. 1997;27(04):951–959. doi: 10.1017/S0033291797005242. [DOI] [PubMed] [Google Scholar]
- Steinberg L. Risk taking in adolescence: What changes, and why? Annals of the New York Academy of Sciences. 2004;1021(1):51–58. doi: 10.1196/annals.1308.005. [DOI] [PubMed] [Google Scholar]
- Stroud LR, Foster E, Papandonatos GD, Handwerger K, Granger DA, Kivlighan KT, Niaura R. Stress response and the adolescent transition: Performance versus peer rejection stressors. Development and Psychopathology. 2009;21(01):47. doi: 10.1017/S0954579409000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, Vanyukov M, et al. Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. American Journal of Psychiatry. 2003;160(6):1078–1085. doi: 10.1176/appi.ajp.160.6.1078. [DOI] [PubMed] [Google Scholar]
- Tate RL, Pituch KA. Multivariate hierarchical linear modeling in randomized field experiments. The Journal of Experimental Education. 2007;75(4):317–337. doi: 10.3200/JEXE.75.4.317-338. [DOI] [Google Scholar]
- Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research. 2003;27(3):247–259. [Google Scholar]
- Tyrka AR, Price LH, Gelernter J, Schepker C, Anderson GM, Carpenter LL. Interaction of childhood maltreatment with the corticotropin-releasing hormone receptor gene: Effects on HPA axis reactivity. Biological Psychiatry. 2009;66(7):681–685. doi: 10.1016/j.biopsych.2009.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vander Stoep A, Mccauley E, Thompson KA, Herting JR, Kuo ES, Stewart DG, et al. Universal emotional health screening at the middle school transition. Journal of Emotional and Behavioral Disorders. 2005;13(4):213–223. doi: 10.1177/10634266050130040301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadsworth ME, Raviv T, Compas BE, Connor-Smith JK. Parent and adolescent responses to poverty related stress: Tests of mediated and moderated coping models. Journal of Child and Family Studies. 2005;14(2):283–298. doi: 10.1007/s10826-005-5056-2. [DOI] [Google Scholar]
- Walker EA, Unutzer J, Rutter C, et al. Costs of health care use by women HMO members with a history of childhood abuse and neglect. Archives of General Psychiatry. 1999;56(7):609–613. doi: 10.1001/archpsyc.56.7.609. [DOI] [PubMed] [Google Scholar]
- Walton A, Flouri E. Contextual risk, maternal parenting and adolescent externalizing behaviour problems: The role of emotion regulation. Child: Care, Health and Development. 2010;36(2):275–284. doi: 10.1111/j.1365-2214.2009.01065.x. [DOI] [PubMed] [Google Scholar]
- Watkins ER. Depressive rumination: Investigating mechanisms to improve cognitive behavioural treatments. Cognitive Behaviour Therapy. 2009;38(Suppl 1):8–14. doi: 10.1080/16506070902980695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins E, Moberly NJ, Moulds ML. Processing mode causally influences emotional reactivity: Distinct effects of abstract versus concrete construal on emotional response. Emotion. 2008;8(3):364–378. doi: 10.1037/1528-3542.8.3.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox HC, Arria AM, Caldeira KM, Vincent KB, Pinchevsky GM, O’Grady KE. Longitudinal predictors of past-year non-suicidal self-injury and motives among college students. Psychological Medicine. 2012;42(04):717–726. doi: 10.1017/S0033291711001814. [DOI] [PMC free article] [PubMed] [Google Scholar]