Abstract
Mosaicism for FMR1 premutation (PM: 55–199 CGG)/full mutation (FM: >200 CGG) alleles or the presence of unmethylated FM (UFM) have been associated with a less severe fragile X syndrome (FXS) phenotype and fragile X associated tremor/ataxia syndrome (FXTAS)—a late onset neurodegenerative disorder. We describe a 38 year old male carrying a 100% methylated FM detected with Southern blot (SB), which is consistent with complete silencing of FMR1 and a diagnosis of fragile X syndrome. However, his formal cognitive scores were not at the most severe end of the FXS phenotype and he displayed tremor and ataxic gait. With the association of UFM with FXTAS, we speculated that his ataxia might be related to an undetected proportion of UFM alleles. Such UFM alleles were confirmed by more sensitive PCR based methylation testing showing FM methylation between 60% and 70% in blood, buccal, and saliva samples and real-time PCR analysis showing incomplete silencing of FMR1. While he did not meet diagnostic criteria for FXTAS based on MRI findings, the underlying cause of his ataxia may be related to UFM alleles not detected by SB, and follow-up clinical and molecular assessment are justified if his symptoms worsen.
Keywords: fragile X syndrome, FMR1, FXTAS, ataxia, tremor, methylation, mosaicism, AmplideX, Southern blot, RNA toxicity
1. Introduction
CGG expansions of more than 200 CGG repeats within the 5′untranslated end of FMR1 are termed full mutations (FM) and are associated with epigenetic silencing of the FMR1 gene [1]. Absence of FMR1 transcription usually results from abnormal methylation of the FMR1 promoter [2] and is associated with loss of FMR1 protein (FMRP). Absence of FMRP, which is a protein essential for normal neurodevelopment, is the primary cause of the fragile X syndrome (FXS) [3]. FXS is the most common monogenic cause of autism and intellectual disability [4] with a prevalence of 1 in 4000 males and 1 in 8000 females in the general population [5].
The more common CGG triplet expansions of 55 to 199 CGG repeats are termed premutations (PM) and are found in approximately 1 in 450 males and 1 in 150 females in the general population [6]. In contrast to FM, PM alleles have a completely unmethylated FMR1 promoter similar to normal size alleles with less than 44 repeats [7], but are associated with elevated FMR1 mRNA levels and paradoxically impaired translation and decreased FMRP levels [8]. Increased FMR1 transcription usually leads to gain-of-function toxicity resulting in aggregation of proteins by the excessive mRNA, formation of ubiquitin-positive inclusion bodies in the brain and other tissues, mitochondrial dysfunction, and excessive cell death [9,10,11]. This molecular cascade has been postulated to be a major contributing factor in the development of PM-specific disorders including fragile X tremor and ataxia syndrome (FXTAS)—a neurodegenerative disorder affecting up to 45% PM males and 17% PM females over the age of 50 [12]. Other molecular contributors to PM specific phenotypes have been suggested to be decreased FMRP levels [8], over-expression of long non-coding RNA of ASFMR1/FMR4 [11], FMR5, and FMR6 [13], and repeat associated non-ATG translation [14].
Although FXS and FXTAS are regarded as distinct disorders, several lines of evidence now suggest that they can be comorbid [15]. Specifically, diagnosis of probable FXTAS has been reported in three FM male cases with completely unmethylated FM alleles in blood [16,17,18]. While significant increases in FMR1 mRNA were reported in blood from all three cases, CGG size testing in other peripheral tissues identified PM/FM mosaicism for one of these [18]. More recently, we have described tissue mosaicism for FM methylation and a microdeletion proximal to the CGG repeat in a 33 year old male with clinical and MRI findings consistent with FXTAS, which is the youngest case reported to date of probable FXTAS [19].
In this study, we describe a 38 year old FXS male with a fully methylated FMR1 promoter in blood, detected using Southern blot analysis of the NruI restriction site within the FMR1 CpG island. This approach is the gold standard FXS diagnostic test where full methylation is understood to indicate complete silencing of FMR1 [20]. However, this result was at odds with methylation analysis of other regions within the FMR1 promoter and FMR1 expression that was reduced, but not silenced. While this individual did not meet the diagnostic criteria for FXTAS, he did show early onset ataxia in his 30s.
2. Experimental Section
2.1. Ethics Approval
The follow-up clinical and molecular assessments consequent to assessment of his tremor and ataxia symptoms in the neurology clinic were conducted as part of the FREE FX study, approved by The Royal Children’s Hospital Research and Ethics Committee.
2.2. Sample Processing
CGG triplet repeat sizing and methylation testing were performed on 15 mL of peripheral blood collected in EDTA tubes, saliva samples collected using the Oragene® DNA Self-Collection Kit (DNA Genotek, Ottawa, ONT, Canada), and buccal samples collected using the Master Amp Buccal Swab Brush kit (Epicentre Technologies, Madison, WI, USA). DNA was isolated from these sample types using the NucleoSpin® Tissue genomic DNA extraction kit (Machery-Nagel, Duren, Germany). Five mL of blood was used for peripheral blood mononuclear cell (PBMC) isolation using Ficoll gradient separation [10]. RNA was extracted from the isolated PBMCs using RNeasy kit (Qiagen Global, Waldbronn, Germany) as per the manufacturer’s instructions.
2.3. Molecular Analyses
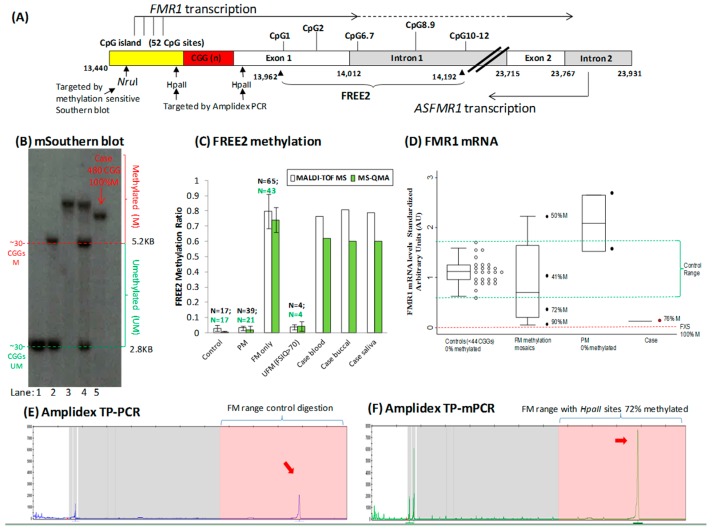
Initial CGG repeat sizing in all samples was performed using polymerase chain reaction (PCR) as previously described [21]. Methylation-sensitive Southern blot was used to confirm presence of a FM allele and to perform methylation analysis of the NruI restriction site located within the CpG island 5′ of the CGG expansion, which is the “gold standard” recommended in FXS diagnostics [20]. Methylation controls included in the Southern blot test were DNA samples from a male and female with normal CGG size alleles and male and female FM carriers as described in a previous publication [2]. Five μg of DNA were digested with the methylation-sensitive enzyme combination of NruI/HindIII. The DNA probe Pfxa3a was radio-labelled with P32 (Random primer DNA labelling kit, TAKARABIO, Otsu, Japan) and used to detect FMR1 allele-specific restriction fragments by autoradiography as previously described [22]. The AmplideX™ FMR1 PCR Kit (Asuragen, Austin, TX, USA) was used to confirm CGG triplet repeat sizing and to perform methylation analysis of two HpaII sites: 5′ and 3′ of the CGG expansion using blood DNA.
The Sequenom MALDI-TOF MS EpiTYPER system (Sequenom, USA) and Methylation Specific Quantitative Melt Analysis (MS-QMA) were used to analyse mean methylation of the fragile X related epigenetic element 2 (FREE2, located 3′ of the CGG repeat) in blood, buccal, and saliva samples as previously described [23]. Specifically, duplicate bisulfite conversions were performed for each DNA sample, with each conversion analysed twice using the EpiTYPER system and MS-QMA. The average of the four methylation output measurements per sample was used as a summary measure of mean FREE2 methylation presented in Figure 1.
Figure 1.
Molecular results. (A) Organization of the FMR1 5′ region including the CGG expansion (sequence numbering from GenBank L29074 L38501) in relation to FMR1 and ASFMR1 transcription start sites (the broken lines indicate spliced out regions), fragile X related epigenetic element 2 (FREE2), the FMR1 CpG island and methylation sensitive restriction site NruI analysed using routine fragile X Southern blot testing, two HpaII sites targeted by AmplideX methylation PCR. The FREE2 region is located downstream of the CGG expansion, at the exon 1/intron1 boundary and includes 12 CpG sites. (B) Methylation sensitive Southern blot analysis of the NruI restriction site within FMR1 CpG island in blood. The DNA sample in question from the fragile X syndrome (FXS) male suspected of fragile X associated tremor/ataxia syndrome (FXTAS) is in lane 5. Comparator DNA sized using standard CGG PCR1 from: (1) a typical male and a female (CGG < 44) are in lanes 1 and 2; (2) full mutation (FM) male with a 100% methylated 613 CGG allele is in lane 3; (3) FM female with a 100% methylated 580 CGG allele is in lane 4. (C) Mean methylation output ratio of CpG sites located within the FREE2 region. Assessed using MALDI-TOF MS and MS-QMA2. Note: the error bars for reference ranges represent one standard deviation from the mean FREE2 methylation in blood of male controls (CGG < 44); Premutation (PM) males (56–170 CGGs); FM males with typical FXS (213–2000 CGGs), and four atypical “high functioning” unmethlyated full mutation (UFM) males by Southern blot (CGG 200–637 CGG). The reference samples were co-run with DNA from the FXS male case suspected of FXTAS from blood, buccal, and saliva samples in question. (D) FMR1 mRNA assessed using real-time PCR relative standard curve method. AmplideX PCR targeting methylation of two HpaII sites. (E) Hexachloto-Fluorescein (HEX) and (F) Fluorescein-Amidite (FAM) channels from capillary electrophoresis of the DNA from the blood of the male case in question. Note: red arrows indicate presence of positive FM alleles with methylated HpaII sites and the control digestion (HpaII methylation independent).
FMR1 mRNA analysis was performed using the relative standard curve real-time PCR method, where the mean of FMR1-5′ and FMR1-3′ assay outputs was normalized to average expression of three internal control genes (GUS, EIF4A2, and SDHA), as previously described [11]. For each sample, RNA was reverse transcribed in two separate cDNA reactions and then each was analysed in two separate real time-PCR reactions. The mean of the four arbitrary unit outputs was used as a summary measure for FMR1 mRNA expression for each sample.
2.4. Ruling Out Other Causes of Ataxia
PCR and fragment analyses were used to examine repeat regions associated Friedreich’s ataxia (FA) and spinocerebellar ataxias (SCA) as part of the molecular diagnostics follow-up, using standard diagnostic protocols as previously described [24,25].
3. Results and Discussion
3.1. Clinical Features and Medical History
A 38 year old intellectually disabled male with a previous diagnosis of fragile X syndrome presented to a neurology clinic with a history of intermittent tremor and increasing unsteadiness over the previous several months. His medical history included type 2 diabetes mellitus and hyperthyroidism due to Grave’s disease. His medications included metformin, gliclazide, insulin, telmisartan, and rabeprazole. His living arrangements were semi-supervised in a flat downstairs from his parents. He has no family history of other movement disorders, including essential tremor; he has only consumed small amounts of alcohol in social settings and there was no history of substance abuse.
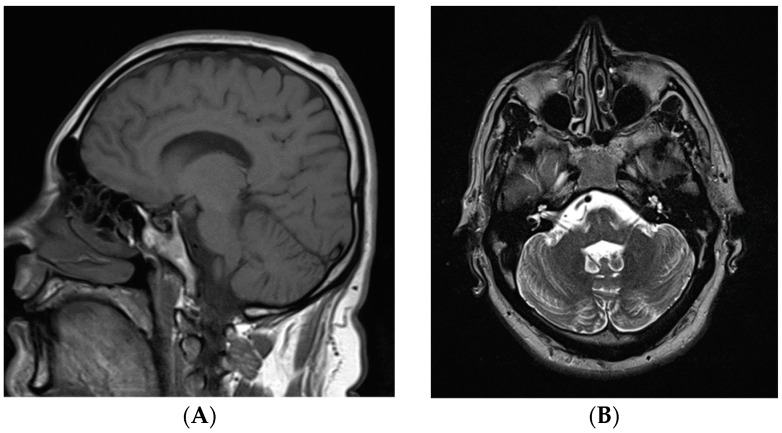
His physical examination demonstrated a high frequency of up-down action tremor without any resting tremor, truncal tremor, titubation, or extrapyramidal signs. Although he had no cerebellar signs in his limbs or nystagmus, he demonstrated a slightly wide-based gait and was unable to complete tandem gait suggesting a mild degree of cerebellar dysfunction. No other involuntary movements or pyramidal signs or apraxia were present. His brain magnetic resonance imaging revealed mild cerebellar atrophy (Figure 2).
Figure 2.
Magnetic resonance imaging of the brain. (A) T1 weighted sagittal view; and (B) T2 weighted axial view. Both images demonstrate the normal appearance of the cerebellum.
Formal assessments of cognitive and behavioural impairments previously associated with the FXS phenotype were performed at 38 years of age, six months after the initial visit. While he was cognitively impaired with full scale IQ (FSIQ) of 50 [26], the score was above the mean FSIQ of 41.2, previously reported in a sample of 51 males with fully methylated FM alleles [27]. However, his overall Autism Diagnostic Observational Schedule-2 (ADOS-2) calibrated severity score (CSS) of 9 [28,29] indicated that he has significant autism spectrum symptomology. His Aberrant Behaviour Checklist Community (ABC-C) scores on Stereotypy and Inappropriate Speech were consistent with individuals with FXS [29] and with the repetitive speech and behaviours observed during the ADOS-2 assessment. However, his ABC-C score on three subscales, (Irritability, Lethargy, and Hyperactivity) were much lower than the mean scores obtained by adult males with FXS [30]. His scores on the Adult Behaviour Checklist (ABCL) were in the normal range for the Externalizing Scale, borderline range for the Internalizing Scale with Somatic Complaints score in the clinically significant range [31].
Blood biochemistry investigations, including thyroid function tests, vitamin B12, folate, autoimmune, and paraneoplastic antibody panel, were all within normal limits. Despite a history of suboptimally controlled diabetes, there was no evidence of sensory or motor neuropathy on the nerve conduction studies, ruling out other possible causes of tremor and ataxia. While PCR based testing for other causes of ataxia did not support Friedrich’s ataxia or spinocerebellar ataxias type 1, 2, 3, 6, and 7, it is possible that the FXS patient has another neurological disorder that would explain the early onset ataxia.
3.2. Genetic Testing
The original diagnostic investigation for FXS at 14 years of age, based on morphological features and cytogenetic testing of cells expressing the Xq27.3 fragile site, was negative. At 38 years of age, he was again referred for FXS testing after his nephew was diagnosed with this syndrome. The follow-up testing using Southern blot revealed a FM expansion but did not use methylation-sensitive enzyme/s. Methylation sensitive Southern blot analysis performed that same year identified a FM allele of 480 CGG repeats that had a 100% methylated NruI site within the FMR1 CpG island (Figure 1B). This, at first, appeared to rule out the presence of PM or unmethylated FM alleles. However, methylation of the FREE2 region in blood, saliva, and buccal cells using MALDI-TOF MS and MS-QMA revealed partial methylation of the FMR1 promoter (60%–70%). Presence of partially methylated FM alleles was further confirmed by (i) AmplideX TP-mPCR through analysis of HpaII site methylation on either side of the CGG repeat (72% methylation) (Figure 1F) and (ii) Analysis of FMR1 mRNA levels in PBMCs revealing presence of transcription at 11% of the control group median levels. This suggested that FMR1 mRNA was not completely silenced in some FM alleles that could explain (i) RNA toxicity at least in a minority of cells and (ii) observed symptoms of ataxia. This is consistent with another 33 year old male case where tissue mosaicism for FM methylation, similarly, did not show FMR1 mRNA levels above the normal range, however, he had clinical and MRI findings consistent with FXTAS [19].
4. Conclusions
This FXS patient demonstrated early onset ataxia without MRI changes beyond mild cerebellar atrophy. While his Southern blot results showed a FM with complete methylation of the FMR1 promoter, from which it could be inferred that the gene was completely silenced in all of his cells, this was inconsistent with the following results: (i) reduced but not silenced FMR1 transcription; (ii) blood biochemistry results ruling out other causes of ataxia; (iii) his cognitive impairment being not as severe as previously reported in most fully methylated FM males. All of this suggested that in this FXS male, FM alleles in a proportion of cells had unmethylated FM alleles and thus were able to express potentially toxic FMR1 mRNA. This was supported by FREE2 methylation testing in blood, buccal, and saliva, AmplideX methylation testing, and FMR1 mRNA analysis in blood. Two potential explanations for the discordance in the methylation results obtained between Southern blot and the other techniques are: (i) the analytical sensitivity of Southern blot methylation analysis is 20% [23], meaning alleles that are 80% methylated will appear as if they are 100% methylated; (ii) the NruI restriction site methylation is different to methylation of the HpaII restriction sites targeted by AmplideX and the FREE2 region targeted by MALDI-TOF MS and MS-QMA. Together this evidence supports the conclusion that FMR1 mRNA is expressed from expanded FM alleles that may be toxic, even in individuals who appear to have a fully methylated FM by the “gold standard” methylation-sensitive Southern blot test. Furthermore, co-morbidity of FXS and ataxia may be more common than previously realised as ataxia has been noted in some older FXS FM patients identified using methylation-sensitive Southern blot in previously described cohorts [32]. We, therefore, propose that if an FXS patient develops ataxia, additional testing be performed including DNA methylation analysis of multiple sites within the FMR1 promoter (especially the FREE2 region) and in multiple tissues, along with testing for FMR1 expression analysis if RNA is available. This additional diagnostic information may better explain the clinical phenotype and provide some assurance to the patients and their family that this is another manifestation of the FMR1 PM or unmethylated FM alleles, rather than a new, unexplained aetiology. Whether the underlying cause of this patient’s ataxia is the same as for FXTAS is unknown, but follow-up study is justified to consider if his symptoms worsen.
Acknowledgments
This work was supported by the Victorian Government’s Operational Infrastructure Support Program, Murdoch Childrens Research Institute, Royal Children’s Hospital Foundation, NHMRC development grant (No 1017263 to DEG), Pierce Armstrong Trust (to DEG), and NHMRC project grants (No 104299 and 1103389 to DEG). We thank the study participant and his family for their contribution and Dr. Benjamin Ong from the Sequenom Platform Facility (MCRI).
Author Contributions
Yun Tae Hwang, Carolyn Rogers, Tracy Dudding, and Robert Heard clinically assessed the patient. Marta Arpone and Lesley Bretherton performed the psychological tests mentioned in the paper. David Eugeny Godler, David Francis, Xin Li, Solange Mabel Aliaga, Desirée du Sart and Howard Robert Slater performed the molecular analyses and were involved in providing results interpretation related to the clinical observations. Yun Tae Hwang and David Eugeny Godler prepared the drafts of the paper. All authors have reviewed, provided corrections, and have agreed to be co-authors on the submitted version of the paper.
Conflicts of Interest
David Eugeny Godler holds patents related to the technology described in this article. The other authors declare that they have no competing interests.
References
- 1.Verkerk A.J., Pieretti M., Sutcliffe J.S., Fu Y.H., Kuhl D.P., Pizzuti A., Reiner O., Richards S., Victoria M.F., Zhang F.P., et al. Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell. 1991;65:905–914. doi: 10.1016/0092-8674(91)90397-H. [DOI] [PubMed] [Google Scholar]
- 2.Godler D.E., Tassone F., Loesch D.Z., Taylor A.K., Gehling F., Hagerman R.J., Burgess T., Ganesamoorthy D., Hennerich D., Gordon L., et al. Methylation of novel markers of fragile X alleles is inversely correlated with FMRP expression and FMR1 activation ratio. Hum. Mol. Genet. 2010;19:1618–1632. doi: 10.1093/hmg/ddq037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pieretti M., Zhang F.P., Fu Y.H., Warren S.T., Oostra B.A., Caskey C.T., Nelson D.L. Absence of expression of the FMR-1 gene in fragile X syndrome. Cell. 1991;66:817–822. doi: 10.1016/0092-8674(91)90125-I. [DOI] [PubMed] [Google Scholar]
- 4.Harris S.W., Hessl D., Goodlin-Jones B., Ferranti J., Bacalman S., Barbato I., Tassone F., Hagerman P.J., Herman H., Hagerman R.J. Autism profiles of males with fragile X syndrome. Am. J. Ment. Retard. 2008;113:427–438. doi: 10.1352/2008.113:427-438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Turner G., Webb T., Wake S., Robinson H. Prevalence of fragile X syndrome. Am. J. Med. Genet. 1996;64:196–197. doi: 10.1002/(SICI)1096-8628(19960712)64:1<196::AID-AJMG35>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 6.Seltzer M.M., Baker M.W., Hong J., Maenner M., Greenberg J., Mandel D. Prevalence of CGG expansions of the FMR1 gene in a US population-based sample. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2012;159B:589–597. doi: 10.1002/ajmg.b.32065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Inaba Y., Schwartz C.E., Bui Q.M., Li X., Skinner C., Field M., Wotton T., Hagerman R.J., Francis D., Amor D.J., et al. Early detection of fragile X syndrome: Applications of a novel approach for improved quantitative methylation analysis in venous blood and newborn blood spots. Clin. Chem. 2014;60:963–973. doi: 10.1373/clinchem.2013.217331. [DOI] [PubMed] [Google Scholar]
- 8.Ludwig A.L., Espinal G.M., Pretto D.I., Jamal A.L., Arque G., Tassone F., Berman R.F., Hagerman P.J. CNS expression of murine fragile X protein (FMRP) as a function of CGG-repeat size. Hum. Mol. Genet. 2014;23:3228–3238. doi: 10.1093/hmg/ddu032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arocena D.G., Iwahashi C.K., Won N., Beilina A., Ludwig A.L., Tassone F., Schwartz P.H., Hagerman P.J. Induction of inclusion formation and disruption of lamin A/C structure by premutation CGG-repeat RNA in human cultured neural cells. Hum. Mol. Genet. 2005;14:3661–3671. doi: 10.1093/hmg/ddi394. [DOI] [PubMed] [Google Scholar]
- 10.Willemsen R., Hoogeveen-Westerveld M., Reis S., Holstege J., Severijnen L.A., Nieuwenhuizen I.M., Schrier M., van Unen L., Tassone F., Hoogeveen A.T., et al. The FMR1 CGG repeat mouse displays ubiquitin-positive intranuclear neuronal inclusions; implications for the cerebellar tremor/ataxia syndrome. Hum. Mol. Genet. 2003;12:949–959. doi: 10.1093/hmg/ddg114. [DOI] [PubMed] [Google Scholar]
- 11.Loesch D.Z., Godler D.E., Evans A., Bui Q.M., Gehling F., Kotschet K.E., Trost N., Storey E., Stimpson P., Kinsella G., et al. Evidence for the toxicity of bidirectional transcripts and mitochondrial dysfunction in blood associated with small CGG expansions in the FMR1 gene in patients with parkinsonism. Genet. Med. 2011;13:392–399. doi: 10.1097/GIM.0b013e3182064362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rodriguez-Revenga L., Madrigal I., Pagonabarraga J., Xuncla M., Badenas C., Kulisevsky J., Gomez B., Mila M. Penetrance of FMR1 premutation associated pathologies in fragile X syndrome families. Eur. J. Hum. Genet. 2009;17:1359–1362. doi: 10.1038/ejhg.2009.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pastori C., Peschansky V.J., Barbouth D., Mehta A., Silva J.P., Wahlestedt C. Comprehensive analysis of the transcriptional landscape of the human FMR1 gene reveals two new long noncoding RNAs differentially expressed in fragile X syndrome and fragile X-associated tremor/ataxia syndrome. Hum. Genet. 2014;133:59–67. doi: 10.1007/s00439-013-1356-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Todd P.K., Oh S.Y., Krans A., He F., Sellier C., Frazer M., Renoux A.J., Chen K.C., Scaglione K.M., Basrur V., et al. CGG repeat-associated translation mediates neurodegeneration in fragile X tremor ataxia syndrome. Neuron. 2013;78:440–455. doi: 10.1016/j.neuron.2013.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hagerman P.J., Hagerman R.J. Fragile X-associated tremor/ataxia syndrome. Ann. N. Y. Acad. Sci. 2015;1338:58–70. doi: 10.1111/nyas.12693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Loesch D.Z., Sherwell S., Kinsella G., Tassone F., Taylor A., Amor D., Sung S., Evans A. Fragile X-associated tremor/ataxia phenotype in a male carrier of unmethylated full mutation in the FMR1 gene. Clin. Genet. 2012;82:88–92. doi: 10.1111/j.1399-0004.2011.01675.x. [DOI] [PubMed] [Google Scholar]
- 17.Santa Maria L., Pugin A., Alliende M., Aliaga S., Curotto B., Aravena T., Tang H.T., Mendoza-Morales G., Hagerman R., Tassone F. Fxtas in an unmethylated mosaic male with fragile X syndrome from chile. Clin. Genet. 2013;86:378–382. doi: 10.1111/cge.12278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Basuta K., Schneider A., Gane L., Polussa J., Woodruff B., Pretto D., Hagerman R., Tassone F. High functioning male with fragile X syndrome and fragile X-associated tremor/ataxia syndrome. Am. J. Med. Genet. A. 2015;167:2154–2161. doi: 10.1002/ajmg.a.37125. [DOI] [PubMed] [Google Scholar]
- 19.Hwang T.Y., Aliaga S., Arpone M.V., Francis D., Li X., Chong B., Slater H.R., Rogers C., Bretherton L., Hunter M., et al. Partially methylated alleles, microdeletion and tissue mosaicism in a fragile X male with tremor and ataxia at 30 years of age: A case report. Am. J. Med. Genet. 2016 doi: 10.1002/ajmg.a.37954. in press. [DOI] [PubMed] [Google Scholar]
- 20.Biancalana V., Glaeser D., McQuaid S., Steinbach P. Emqn best practice guidelines for the molecular genetic testing and reporting of fragile X syndrome and other fragile X-associated disorders. Eur. J. Hum. Genet. 2015;23:417–425. doi: 10.1038/ejhg.2014.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khaniani M.S., Kalitsis P., Burgess T., Slater H.R. An improved diagnostic PCR assay for identification of cryptic heterozygosity for CGG triplet repeat alleles in the fragile X gene (FMR1) Mol. Cytogenet. 2008 doi: 10.1186/1755-8166-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Godler D.E., Slater H.R., Bui Q.M., Ono M., Gehling F., Francis D., Amor D.J., Hopper J.L., Hagerman R., Loesch D.Z. FMR1 intron 1 methylation predicts FMRP expression in blood of female carriers of expanded FMR1 alleles. J. Mol. Diagn. 2011;13:528–536. doi: 10.1016/j.jmoldx.2011.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aliaga S.M., Slater H.R., Francis D., Du Sart D., Li X., Amor D.J., Alliende A.M., Santa Maria L., Faundes V., Morales P., et al. Identification of males with cryptic fragile X alleles by methylation-specific quantitative melt analysis. Clin. Chem. 2016;62:343–352. doi: 10.1373/clinchem.2015.244681. [DOI] [PubMed] [Google Scholar]
- 24.Biros I.I., Forrest S.M. Duplex PCR for autosomal dominant spinocerebellar ataxia testing: A nonradioactive rapid screening method. Mol. Diagn. 1998;3:223–227. doi: 10.1016/S1084-8592(98)80044-1. [DOI] [PubMed] [Google Scholar]
- 25.Campuzano V., Montermini L., Molto M.D., Pianese L., Cossee M., Cavalcanti F., Monros E., Rodius F., Duclos F., Monticelli A., et al. Friedreich’s ataxia: Autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science. 1996;271:1423–1427. doi: 10.1126/science.271.5254.1423. [DOI] [PubMed] [Google Scholar]
- 26.Wechsler D. Wechsler Adult Intelligence Scale. 4th ed. Psychological Corporation; Orlando, FA, USA: 2008. Administration and Scoring Manual. [Google Scholar]
- 27.Merenstein S.A., Sobesky W.E., Taylor A.K., Riddle J.E., Tran H.X., Hagerman R.J. Molecular-clinical correlations in males with an expanded FMR1 mutation. Am. J. Med. Genet. 1996;64:388–394. doi: 10.1002/(SICI)1096-8628(19960809)64:2<388::AID-AJMG31>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 28.Lord C., Rutter M., DiLavore P.C., Risi S., Gotham K., Bishop S.L. Autism Diagnostic Observation Schedule. 2nd ed. Western Psychological Services; Torrance, CA, USA: 2012. [Google Scholar]
- 29.Hus V., Lord C. The autism diagnostic observation schedule, module 4: Revised algorithm and standardized severity scores. J. Autism. Dev. Disord. 2014;44:1996–2012. doi: 10.1007/s10803-014-2080-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sansone S.M., Widaman K.F., Hall S.S., Reiss A.L., Lightbody A., Kaufmann W.E., Berry-Kravis E., Lachiewicz A., Brown E.C., Hessl D. Psychometric study of the aberrant behavior checklist in fragile X syndrome and implications for targeted treatment. J. Autism. Dev. Disord. 2012;42:1377–1392. doi: 10.1007/s10803-011-1370-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Achenbach T., Rescorla L. Manual for the ASEBA Adult Forms and Profiles. University of Vermont; Burlington, VT, USA: 2003. [Google Scholar]
- 32.Utari A., Adams E., Berry-Kravis E., Chavez A., Scaggs F., Ngotran L., Boyd A., Hessl D., Gane L.W., Tassone F., et al. Aging in fragile X syndrome. J. Neurodev. Disord. 2010;2:70–76. doi: 10.1007/s11689-010-9047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]