Abstract
Background
It is unclear whether an “obesity paradox” exists in the respiratory system, especially in acute respiratory distress syndrome (ARDS) and acute lung injury (ALI). Previous studies have postulated a causal relation between obesity and ARDS/ALI but have lacked power to form a definitive conclusion.
Objective
To investigate the relationships between obesity, ARDS/ALIrisk, and mortality.
Methods
A systematic search current to April 2016 was performed in Pubmed, EMBASE, Medline, Cochrane databases to find relevant studies. All studies that estimate the effect of obesity in the morbidity and mortality of ARDS/ALI were included.
Results
A total of 24 studies including 9,187,248 subjects were analyzed. The combined results from 16 studies that examined the effect of obesity in morbidity of ARDS/ALI showed an89% increase in odds ratio(pooled odds ratios (OR) 1.89, 95% confidence intervals (CI) 1.45 to 2.47). In subgroup analysis, compared to normal weight, obesity was associated with an increased risk of ARDS/ALI (OR1.57, 95% CI 1.30–1.90 for obese (BMI30-39.9kg/m2); OR1.75, 95% CI 1.42–2.15 for obese(BMI≥30kg/m2); OR1.67, 95% CI 1.04–2.68 for morbid obese(BMI≥40kg/m2)). The combined results from 9 studies that examined the effect of obesity in mortality of ARDS/ALI had a pooled odds ratio(pooled OR 0.63, 95% CI 0.41 to 0.98). Inversely, obesity was significantly associated with reduced risk of ARDS/ALI mortality(OR0.88, 95% CI 0.78–1.00 for overweight(BMI≤18.5m2); OR0.74, 95% CI 0.64–0.84 for obese (BMI30-39.9kg/m2);OR0.84, 95% CI 0.75–0.94 for 60days mortality; OR0.38, 95% CI 0.22–0.66 for 90days mortality).
Conclusions
Our data identify obesity as an important risk factor for the development of ARDS/ALI; however, ARDS/ALI outcomes are improved in this population when compared to individuals with a normal body mass index. This meta-analysis results supported ‘‘obesity paradox” in ARDS/ALI.
Introduction
Acute respiratory distress syndrome(ARDS) /Acute lung injury (ALI) is a severe formof acute edematous lung injury which is characterized by arapid development of acute respiratory failure. It develops in response toother serious medical conditions including sepsis, pneumonia, aspiration and trauma[1, 2],and is associated with high morbidity and mortality. Obesity has risen to epidemic proportions in the US and other developed countries[3]. Over one third of the American population is obese, and over 5% is extremely obese[4].Obesity is a risk factor for many diseases including diabetes, dyslipidemia, heart disease, hypertension, insulin resistance, stroke, sleep apnea and cancer[5].However, an inverse relationship between obesity and mortality has been described in patients with cardiovascular disease and diabetes [6–7].This phenomenon is known as the “obesity paradox”.
Some studies of obesity and ARDS/ALI have focused on morbidity with inconsistent results[8–11]. Some studies found obesity to be associated with decreased mortality[12,13], while other studies showed no to improved mortality in the obese patients[8,14].Whether the “obesity paradox” exists in ARDS/ALI is still unclear. With the rising incidence of obesity and the increased mortality, morbidity and health expenditures associated with ARDS/ALI, we present here a systematic review and meta-analys is to investigate the relationships between obesity, ARDS/ALI risk, and mortality.
Methods
Data Sources and Search Strategy
We searched several databases (Pubmed, EMBASE, Medline and the Cochrane databases) for relevant studies published through April 2016. ‘‘obesity”, ‘‘body mass index” or “BMI”, combined with ‘‘acute respiratory distress syndrome”, “ARDS”, “acute lung injury” or “ALI” were keywords used for searching. There was no language restriction. Moreover, review and reference lists of relevant articles were screened for additional articles. The searches were conducted independently by two authors (Guo Zhi and Wang Xin).
Inclusion and Exclusion Criteria
Studies were included if they met the following criteria: (1) reference to human beings;(2)the primary objective was to investigate the effect of BMIon the morbidity and mortality of ARDS/ALI; (3) obesity was categorized by BMI, and BMI was calculated by dividing the patient’s body weight in kilograms by the square of their height in meters.(4)reference to odds ratio (OR), relative risk (RR) or equivalent values representing risks of morbidity and mortality in ARDS/ALI. Studies were excluded if one of the following existed: (1) case reports, editorials, reviews and abstracts; (2) insufficient data to extract or calculate the pooled results. When pertinent data were not included in a published article, the corresponding author was contacted. If a response was not provided, the article was excluded. All the studies were screened independently by two authors (Guo Zhi and Wang Ying). Disagreements were resolved by a third opinion (Liu Shuying).
Data Extraction and Synthesis
The information of studies included first author, year of publication, study design, sample size, BMI classification,ARDS/ALI diagnostic standard and outcomes. If studies did not report OR, RRand 95% confidence intervals(95%CI), raw data were screened to determine whether ORs could be calculated. When the studies reported both the crude and adjusted OR/RRs, the adjusted OR/RRs were extracted. Data extraction was carried out by two authors (Guo Zhi and Xing Guohong).
Statistical Analysis
This meta-analysis of included studies was carried out with RevMan5.2and Stata 10.0. We abstracted odds ratios (OR), risk ratios(RR), and 95% confidence intervals (CI) from all studies. We then calculated logarithm of the OR (logOR) and its standard error (SE[logOR]) for all studies. The data were analyzed to generate a pooled effect size and 95% CI. A p value ≤ 0.05 was considered statistically significant. The heterogeneity of included studies was examined by the I2statistic. The summary estimates were obtained by the random effects model (P≤0.1, I2≥50% with heterogeneity) or the fixed effects model (P>0.1, I2<50% with no heterogeneity)[15].Subgroup analysis was used to assess heterogeneity between studies. We evaluated the possibility of publication bias with Egger’stest (Stata 10.0)[16].
Results
Literature Search and Study Characteristics
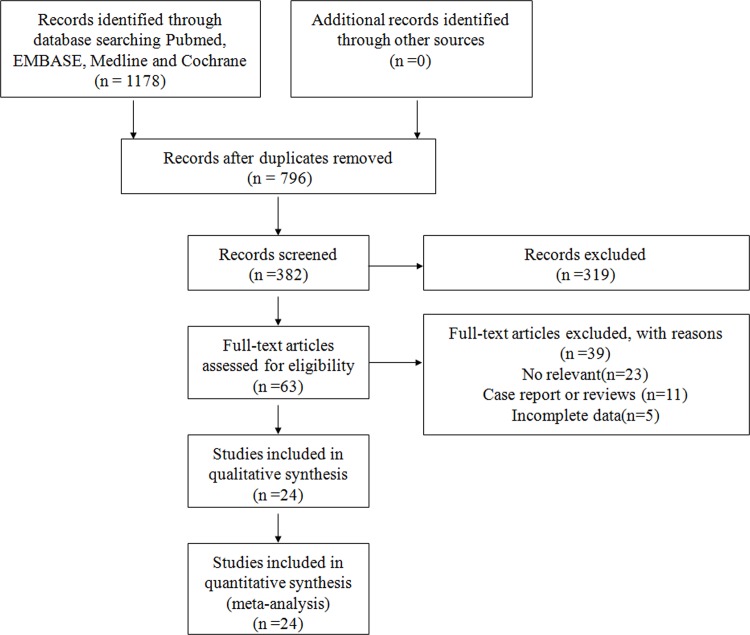
The method used to select studies is shown in Fig 1. 1178 articles were initially identified. After exclusion of duplicates(n = 796) and irrelevant studies (n = 319), 63 potentially eligible studies were selected.39 articles were excluded since they were case report or reviews (n = 10), did not evaluate obesity on ARDS/ALI (n = 20), or haven't provided sufficient data to further calculate(n = 9). Consequently, we identified 24 studies [8–14,17–33] that met our inclusion criteria. The characteristics of included articles are shown in Table 1 and Table 2.
Fig 1. Study flow for the meta-analysis.
Table 1. Characteristics of included studiesthat examined the effect of obesityonmorbidity of ARDS/ALI.
| Author | Year | Studydesign | Sample size | BMI classification(kg/m2) | ARDS/ALI diagnostic standard | Outcomes |
|---|---|---|---|---|---|---|
| Anna M. Bramley | 2012 | retrospective Study | 154 | normal (BMI<30), obese (BMI 30–39.9), morbid obese (BMI ≥40) | NA | Morbidity: OR 1.928, 95% CI 0.718–5.181 |
| Binod Dhakal | 2013 | retrospective study | 320 | normal (BMI<25), obese (BMI ≥25) | NA | Morbidity: OR 0.3, 95% CI 0.027–3.349 |
| Huang Lei | 2013 | retrospective study | 184 | NA | American European Consensus Conference definition* | Morbidity: OR 5.023, 95% CI 2.486–10.150 |
| I Bonmarin | 2015 | retrospective study | 3074 | normal (BMI<30), obese (BMI ≥30) | NA | Morbidity: OR 1.8, 95% CI 1.1–3.0 |
| Jessica A. Palakshappa | 2016 | prospective study | 164 | underweight (BMI<18.5), normal (BMI 18.5–25), overweight (BMI 25–30), obese (BMI ≥30) | ARDS: both PaO2/FiO2 ratio<200 and bilateral infiltrates on chest radiographs within a 24-hour period | Morbidity: OR 2.388, 95% CI 1.075–5.305 |
| John C. Weinlein | 2015 | retrospective study | 507 | normal (BMI<25), overweight (BMI 25–29.9)obese (BMI 30–39.9), morbid obese (BMI ≥40) | ARDS: PaO2/FiO2 ratio<200 for >12 hours, bilateral infiltrates on chest radiographs, and no evidence of a cardiogenic cause. | Morbidity: OR 35.38, 95% CI 1.79–699.7; |
| Jonathan Elmer | 2013 | retrospective study | 697 | normal (BMI≤30), obese (BMI >30) | ALI: diffuse, bilateral infiltrates on chestradiograph; at least two consecutive arterialblood gassamples with a PaO2:FiO2ratio < 300 mmHg; no evidence of left atrial hypertension. | Morbidity: OR 1.67, 95% CI 1.25–2.24 |
| Juan C. Duchesne | 2009 | retrospective study | 12759 | normal (BMI≤29), obese (BMI 30–39.9), morbid obese (BMI ≥40) | American European Consensus Conference definition | Morbidity: OR 1.59, 95% CI 0.90–2.82 |
| Lesly A. Dossett | 2008 | prospective study | 1291 | National Heart, Lung, and Blood Institute guidelines# | ARDS: the presence of bilateral patchy infiltrates seen on a chest radiograph; a PaO2/fraction of inspired oxygen ratio of < 200; and the absence of cardiogenic pulmonary edema | Morbidity: OR 0.36, 95% CI 0.13–0.99 |
| Lioudmila V. Karnatovskaia | 2014 | prospective study | 5584 | National Heart, Lung, and Blood Institute guidelines | American European Consensus Conference definition | Morbidity: OR 1.69, 95% CI 0.98–2.8 |
| Mark A Newell | 2007 | retrospective study | 1543 | normal (BMI 18.5–24.9), overweight (BMI 25–29.9), obese (BMI 30–39.9), morbid obese (BMI ≥40) | NA | Morbidity: OR 3.675, 95% CI 1.237–10.916 |
| Michelle Ng Gong | 2010 | prospective study | 1795 | National Heart, Lung, and Blood Institute guidelines | American European Consensus Conference definition | Morbidity: OR 1.78, 95% CI 1.12–2.92; |
| Monisha A. Kumar | 2012 | retrospective study | 69 | normal (BMI<30), obese (BMI ≥30) | ARDS: PaO2/FiO2 ratio <200, bilateral lung infiltrates by radiography and a central venous pressure <18 mmHg. ALI: a PaO2/FiO2 ratio <300. | Morbidity: OR 2.01, 95% CI 0.489–8.27 |
| Natalia Hagau | 2010 | prospective study | 32 | normal (BMI≤30), obese (BMI >30) | American European Consensus Conference definition | Morbidity: OR 13.33, 95% CI 1.434–123.98; |
| Shihua Yao | 2013 | prospective study | 364 | normal (BMI≤28), obese (BMI >28) | American European Consensus Conference definition | Morbidity: OR 3.25, 95% CI 0.392–26.916 |
| Shirin Towfigh | 2009 | prospective study | 2046 | normal (BMI<30), obese (BMI≥30) | American European Consensus Conference definition | Morbidity: OR 1.57, 95% CI 1.01–2.45 |
BMI, body mass index; ALI, acute lung injury; ARDS, acute respiratory distress syndrome.
*American European Consensus Conference definition:the presence of bilateral patchy infiltrates seen on a chest radiograph; hypoxemia (PaO2 /FiO2< 300-ALI, PaO2 /FiO2< 200-ARDS); the absence of cardiogenic pulmonary edema.
#BMI classification by National Heart, Lung, and Blood Institute guidelines: underweight (BMI≤18.5), normal (BMI 18.5–25), overweight (BMI 25–29.9), obese (BMI 30–39.9), morbid obese (BMI ≥40)
Table 2. Characteristics of included studiesthat examined the effect of obesityonmortality of ARDS/ALI.
| Author | Year | Studydesign | Sample size | BMI classification(kg/m2) | ARDS/ALI diagnostic standard | Outcomes |
|---|---|---|---|---|---|---|
| Amy E. Morris | 2007 | prospective study | 825 | National Heart, Lung, and Blood Institute guidelines# | American European Consensus Conference definition* | Mortality: OR 0.513, 95% CI 0.268–0.984; |
| Audrey De Jong | 2013 | retrospective Study | 66 | normal (BMI<30), obese (BMI≥35) | American European Consensus Conference definition | Mortality: OR 0.266, 95% CI 0.087–0.816 |
| Ayman O. Soubani | 2015 | retrospective Study | 2914 | National Heart, Lung, and Blood Institute guidelines | NA | Mortality: OR 1.018, 95% CI 0.671–1.545 |
| Graciela J Soto | 2012 | retrospective study | 751 | National Heart, Lung, and Blood Institute guidelines | American European Consensus Conference definition | Mortality: OR 0.81, 95% CI 0.71–0.93 |
| James M. O’Brien Jr | 2004 | retrospective study | 902 | normal (BMI 18.5–24.9), overweight (BMI 25–29.9), obese (BMI 30–39.9), morbid obese (BMI ≥40) | NA | Mortality: OR 1.111, 95% CI 0.693–1.782 |
| James M. O’Brien Jr | 2006 | retrospective study | 1488 | normal (BMI 18.5–24.9), overweight (BMI 25–29.9), obese (BMI 30–39.9), morbid obese (BMI ≥40) | NA | Mortality: OR 0.78, 95% CI 0.44–1.38 |
| Michelle Ng Gong | 2010 | prospective study | 1795 | National Heart, Lung, and Blood Institute guidelines | American European Consensus Conference definition | Mortality: OR 0.89, 95% CI 0.71–1.12 |
| Renee D. Stapleton | 2010 | retrospective study | 1409 | National Heart, Lung, and Blood Institute guidelines | American European Consensus Conference definition | Mortality: OR 0.425, 95% CI 0.227–0.794 |
| Stavros G. Memtsoudis | 2011 | retrospective study | 9149030 | NA | NA | Mortality: OR 0.31, 95% CI 0.28–0.36 |
BMI, body mass index; ALI, acute lung injury; ARDS, acute respiratory distress syndrome.
*American European Consensus Conference definition: the presence of bilateral patchy infiltrates seen on a chest radiograph; hypoxemia (PaO2 /FiO2< 300-ALI, PaO2 /FiO2< 200-ARDS); the absence of cardiogenic pulmonary edema.
#BMI classification by National Heart, Lung, and Blood Institute guidelines: underweight (BMI≤18.5), normal (BMI 18.5–25), overweight (BMI 25–29.9), obese (BMI 30–39.9), morbid obese (BMI ≥40)
Meta-Analysis Results
Obesity and morbidity of ARDS/ALI
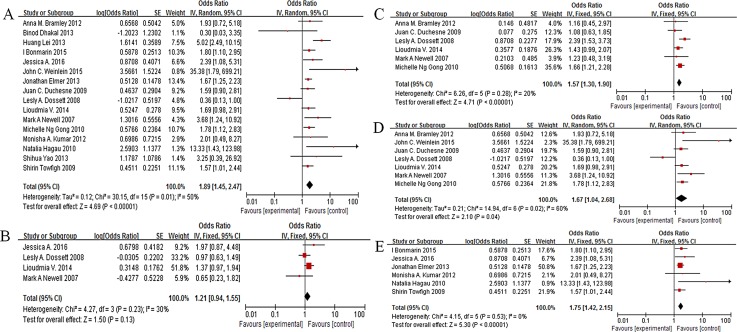
As shown in Fig 2A, Obesity was associated with a significantly increased risk of ARDS/ALI(pooled OR = 1.89, 95% CI: 1.45–2.47, I2 = 50%, P<0.00001, n = 30583,Fig 2A).3 included studies (n = 8670) reported that patients were classified into the following BMI groups according to the National Heart, Lung, and Blood Institute guidelines[34]: underweight (BMI≤18.5m2), normal (BMI 18.5-25m2), overweight (BMI 25–29.9m2), obese (BMI 30–39.9m2), morbid obese (BMI ≥40m2). In the subgroup analysis by this classification, compared to the normal weight, overweight (BMI 25-30kg/m2)was not associated with risk of ARDS/ALI(OR = 1.21, 95% CI: 0.94–1.55, P = 0.13, I2 = 30%, n = 6540,Fig 2B).Six studies evaluated obese (BMI 30–39.9kg/m2) inrisk of ARDS/ALI, and OR was 1.57(OR1.57, 95% CI 1.30–1.90, P<0.00001, I2 = 20%, n = 5426, Fig 2C). For morbid obese (BMI ≥40kg/m2), there was a 67% increase in risk of ARDS/ALI (OR1.67, 95% CI 1.04–2.68, P = 0.04, I2 = 60%, n = 4124, Fig 2D).On the other hand, 6 studies defined obesity as a BMI≥30kg/m2. Obesity(BMI≥30kg/m2) was associated with a significantly increased risk of ARDS/ALI (OR1.75, 95% CI 1.42–2.15, P<0.00001, I2 = 0%, n = 6025, Fig 2E).
Fig 2. Association of obesity and morbidity in ARDS/ALI patients.
A: pooled result; B: overweight(BMI25-29.9kg/m2) vs normal; C: obese(BMI30-39.9kg/m2) vs normal; D: morbid obese(BMI≥40kg/m2) vs normal; E:obese(BMI≥30kg/m2) vs normal.
Obesity and mortality of ARDS/ALI
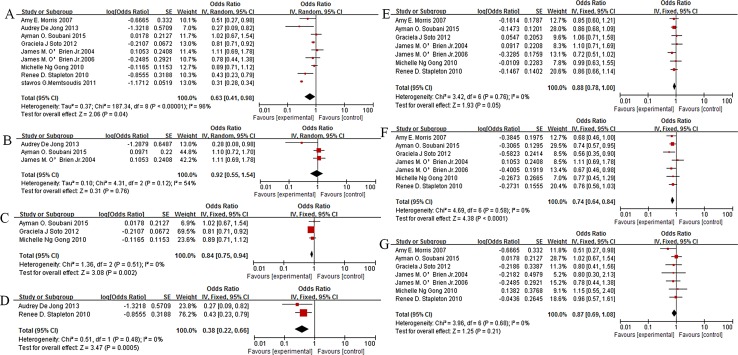
Fig 3 showed the association between obesity and mortality of ARDS/ALI. Obesity was associated with lower risk of mortality in ARDS/ALI (pooled OR 0.63, 95% CI 0.41 to 0.98,P = 0.04,I2 = 96%,n = 9159180, Fig 3A).To clarify the heterogeneity, subgroup analysis was stratified according to BMI classification[34]and mortality in different periods. Three studies were plotted and showed no obvious relationship between obesity and 28days mortality in ARDS/ALI (OR0.92, 95% CI 0.55–1.54, P = 0.76, I2 = 54%, n = 1723, Fig 3B).Obesity was associated with lower risk of 60 days and 90 days mortality in ARDS/ALI(60days: OR0.84, 95% CI 0.75–0.94, P = 0.002, I2 = 0%,n = 1946, Fig 3C;90days:OR0.38, 95% CI 0.22–0.66, P = 0.0005, I2 = 0%,n = 682, Fig 3D). In reference to the normal weight, overweight and obese were associated with decreased mortality risk (overweight:OR0.88, 95% CI 0.78–1.00,P = 0.05, I2 = 0%, n = 6155, Fig 3E; obese: OR0.74, 95% CI 0.64–0.84,P<0.0001, I2 = 0%,n = 5488, Fig 3F).However, there was no evidence of a relationship between morbid obese and ARDS/ALI mortality (OR0.87, 95% CI 0.69–1.08,P = 0.21, I2 = 0%,n = 4145, Fig 3G).
Fig 3. Association of obesity and mortality in ARDS/ALI patients.
A:pooled result; B: 28days; C: 60days; D: 90days;E: overweight vs normal; F: obese vs normal; G: morbid obese vs normal.
Publication Bias
We detected no publication bias among the included studies that assessed obesity in morbidity and mortality of ARDS/ALI based on Egger’s test (P = 0.331,S1 Fig;P = 0.530,S2 Fig).
Discussion
This current meta-analysis, including 9,187,248 subjects from 24 observational studies, explored the association between obesity and risks of ARDS/ALI. The results of our meta-analysis indicated that ARDS/ALI morbidity was higher for patients with obesity compared to normal weight. In addition, obesity was significantly associated with a reduction in ARDS/ALI mortality, especially in long-term mortality.
In subgroup analyses by BMI classification, except for overweight, we found that obese and morbid obese could increase the risk of ARDS/ALI. Moreover, it was confirmed by our result in another obesity group (BMI≥30kg/m2).There were several potential explanations for why obesity may have higher risk of ARDS/ALI. First, obesity is a chronic inflammatory disease. Patients who are obese have increased circulating neutrophil levels[35,36] and elevations in blood cytokines such as TNF-α, IL-1β, IL-8 and IL-6[37,38].Some studies in mice have shown that increased inflammatory cytokines induce depletion of anti-oxidant stores, up-regulation of adhesion molecules on lung endothelium and enhanced susceptibility of endothelium to injury [39,40]. Moreover, innate immune cell activation and endothelial injury in the pulmonary microvasculature is a major contributor to the increased permeability pulmonary edema of ARDS/ALI in obese patients[41–43].Another significant feature of obesity is the dysregulation of adipokine release and response. Shah et al[44] found that Obesity-induced adipokine imbalance impaired pulmonary vascular homeostasis, altered the expression of endothelial junctional adherens and adhesion proteins, and primed the lung for acute injury. Moreover, these hormonal changes, inflammation-related actions and immune-related activities have been shown to be important in the development of ARDS/ALI [45–47]. Finally, obese patients experience a number of changes in pulmonary mechanics compared to lean individuals. Some of the changes in obese patients include a decrease in total lung capacity (TLC), functional residual capacity (FRC), and vital capacity (VC) as well as consequently atelectasis, increased airways resistance and closure, and ventilation/perfusion mismatch[48,49].These findings strongly support a link between obesity and risk of developing ARDS/ALI.
Our meta-analysis suggested a survival advantage for obese patients with ARDS/ALI and supported the emerging concept of the ‘‘obesity paradox.”
The mechanism of the ‘‘obesity paradox” in patients with ARDS/ALI was unclear. We propose some explanations for the inverse relationship between obesity and the risk of ARDS/ALI mortality. First, a recent study analyzed plasma biomarker levels in 1409 patients with ARDS and found that obese patients have lower levels of proinflammatory cytokines (IL-6, IL-8) and surfactant protein D (a marker of alveolar epithelial injury) compared to normal weight patients[30].Moreover, recent animal studies[50,51] suggested that obesity-associated attenuation of ALI was in part attributable to an obesity-associated abnormal neutrophil chemoattractant response. These studies indicated that obesity may be “primed” for the development of ARDS/ALI, but innate immunity and the inflammatory response may be altered and attenuated during ARDS/ALI. Second, obese patients may receive optimal medical treatment or aggressive treatment for an increase risk of cardiovascular disease and diabetes [52].Finally, obese patients may provide a metabolic reserve to counteract the increased catabolic stress of ARDS/ALI because of additional energy stores in the form of adipose tissue. Additional energy stores and optimal medical treatments in the obese patients may explain the improved long-term mortality of ARDS/ALI in our results. Interestingly, consistent with a U-shaped relationship between BMI and mortality[53–55],we found obesity(BMI30-39.9kg/m2) had the lowest ARDS/ALI mortality and no obvious relationship between morbid obese(BMI≥40kg/m2)and ARDS/ALI mortality.
Our study has some potential limitations. First, since this is an observational meta-analysis, it inherits the limitation of the original studies. The effect of confounding, such as age, gender, and underlying diseases, was not examined. For example, pre-existing diabetes was associated with a decreased risk of ALI/ARDS [56]. In this meta-analysis, 8 studies included diabetes patients and 8 studies did not report it clearly. For insufficient data, we did not assess the effect of diabetes on the development of ARDS/ALI in patients with obesity. Second, obesity was defined by different methods in different studies, such as BMI >28kg/m2 and BMI >25kg/m2, which were excluded in subgroup analysis. Third, high heterogeneity was found in subgroup, especially for obese patients in 28days mortality and morbid obese patients in risk of ARDS/ALI. Given this limitation, the results should be carefully interpreted, and confirmed by future studies.
In conclusion, obesity is associated with an increased risk of ARDS/ALI, but obese patients have a lower mortality risk when compared to patients with a normal BMI. Our results support the emerging concept of the ‘‘obesity paradox” in ARDS/ALI.
Supporting Information
(DOC)
(TIF)
(TIF)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med.2000; 342:1334–49. 10.1056/NEJM200005043421806 [DOI] [PubMed] [Google Scholar]
- 2.Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M,et al. Incidence and outcomes of acute lung injury. N Engl JMed.2005;353:1685–93. [DOI] [PubMed] [Google Scholar]
- 3.Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP. The continuing epidemic of obesity in the United States. JAMA. 2000; 284:1650–1651. [DOI] [PubMed] [Google Scholar]
- 4.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010; 303:235–241. 10.1001/jama.2009.2014 [DOI] [PubMed] [Google Scholar]
- 5.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr. Body-mass index and mortality in a prospective cohort of USadults. N Engl J Med. 1999;341:1097–1105. 10.1056/NEJM199910073411501 [DOI] [PubMed] [Google Scholar]
- 6.De Schutter A, Lavie CJ, Milani RV. The impact of obesity on risk factorsand prevalence and prognosis of coronary heart disease-the obesityparadox. Prog Cardiovasc Dis. 2014;56:401–408. 10.1016/j.pcad.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 7.Carnethon MR, De Chavez PJ, Biggs ML, Lewis CE, Pankow JS, Bertoni AG,et al. Association ofweight status with mortality in adults with incident diabetes. JAMA. 2012,308:581–590. 10.1001/jama.2012.9282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gong MN, Bajwa EK, Thompson BT, Christiani DC. Body mass index is associated with the development of acute respiratory distress syndrome. Thorax. 2010; 65:44–50. 10.1136/thx.2009.117572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dossett LA, Heffernan D, Lightfoot M, Collier B, Diaz JJ, Sawyer RG, et al. Obesity and pulmonary complications in critically injured adults. Chest.2008;134:974–80. 10.1378/chest.08-0079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karnatovskaia LV, Lee AS, Bender SP, Talmor D, Festic E; US Critical Illness and Injury Trials Group: Lung Injury Prevention Study Investigators (USCIITG–LIPS). Obstructive sleep apnea, obesity, and the development ofacute respiratory distress syndrome.J Clin Sleep Med. 2014;10:657–62. 10.5664/jcsm.3794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Newell MA, Bard MR, Goettler CE, Toschlog EA, Schenarts PJ, Sagraves SG,et al. Body mass index and outcomes in critically injured blunt trauma patients: weighing the impact.J Am Coll Surg. 2007;204:1056–61; discussion 1062–4. 10.1016/j.jamcollsurg.2006.12.042 [DOI] [PubMed] [Google Scholar]
- 12.Memtsoudis SG, Bombardieri AM, Ma Y, Walz JM, Chiu YL, Mazumdar M. Mortality of patients with respiratory insufficiency and adult respiratory distress syndrome after surgery: the obesity paradox.J Intensive Care Med.2012;27:306–11. 10.1177/0885066611411410 [DOI] [PubMed] [Google Scholar]
- 13.Soto GJ, Frank AJ, Christiani DC, Gong MN. Body mass index and acute kidney injury in the acute kidney injury in the acute respiratory distress syndrome.Crit Care Med.2012;40:2601–8. 10.1097/CCM.0b013e3182591ed9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Brien JM Jr, Welsh CH, Fish RH, Ancukiewicz M, Kramer AM; National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network.Excess body weight is not independently associated with outcome in mechanically ventilated patients with acute lung injury. Ann Intern Med. 2004;140:338–45. [DOI] [PubMed] [Google Scholar]
- 15.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ.1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bramley AM, Dasgupta S, Skarbinski J, Kamimoto L, Fry AM, Finelli L,et al. Intensive care unit patients with 2009 pandemic influenza A (H1N1pdm09) virus infection- United States, 2009.Influenza Other Respir Viruses. 2012;6:e134–42. 10.1111/j.1750-2659.2012.00385.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Jong A, Molinari N, Sebbane M, Prades A, Futier E, Jung B, et al. Feasibility and effectiveness of position in morbidly obese patients with ARDS: a case-control clinical study.Chest. 2013;143:1554–61. 10.1378/chest.12-2115 [DOI] [PubMed] [Google Scholar]
- 19.Soubani AO, Chen W, Jang H.The outcome of acute respiratory distress syndrome in relation to body mass index and diabetes mellitus. Heart Lung. 2015;44:441–7. 10.1016/j.hrtlng.2015.06.007 [DOI] [PubMed] [Google Scholar]
- 20.Dhakal B, Eastwood D, Sukumaran S, Hassler G, Tisol W, Gasparri M,et al. Morbidities of lung cancer surgery in obese patients.J Thorac Cardiovasc Surg. 2013;146:379–84. 10.1016/j.jtcvs.2013.02.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lei H, Minghao W, Xiaonan Y,Ping X, Ziqi L, Qing X.Acute lung injury in patients with severe acute pancreatitis. Turk J Gastroenterol.2013;24:502–7. [DOI] [PubMed] [Google Scholar]
- 22.Bonmarin I, Belchior E, Bergounioux J, Brun-Buisson C, Mégarbane B, Chappert JL, et al. Intensive care unit surveillance of influenza infection in France: the 2009/10 pandemic and the three subsequent seasons.Euro Surveill. 2015;20(46). 10.2807/1560-7917.ES.2015.20.46.30066 [DOI] [PubMed] [Google Scholar]
- 23.O'Brien JM Jr, Phillips GS, Ali NA, Lucarelli M, Marsh CB, Lemeshow S. Body mass index is independently associated with hospital mortality in mechanically ventilated adults with acute lung injury.Crit Care Med. 2006;34:738–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palakshappa JA, Anderson BJ, Reilly JP, Shashaty MG, Ueno R, Wu Q,et al. Low plasma levels of adiponectin do not explain acute respiratory distress syndrome risk: a prospective cohort study of patients with severe sepsis. Crit Care. 2016;20:71 10.1186/s13054-016-1244-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weinlein JC, Deaderick S, Murphy RF. Morbid obesity increases the risk for systemic complications in patients with femoral shaft fractures.J Orthop Trauma. 2015;29:e91–5. 10.1097/BOT.0000000000000167 [DOI] [PubMed] [Google Scholar]
- 26.Elmer J, Hou P, Wilcox SR, Chang Y, Schreiber H, Okechukwu I, et al. Acute respiratory distress syndrome after spontaneous intracerebral hemorrhage*. Crit Care Med. 2013;41:1992–2001. 10.1097/CCM.0b013e31828a3f4d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duchesne JC, Schmieg RE Jr, Simmons JD, Islam T, McGinness CL, McSwain NE Jr. Impact of obesity in damage control laparotomy patients.J Trauma. 2009;67:108–12; discussion 112–4. 10.1097/TA.0b013e3181a92ce0 [DOI] [PubMed] [Google Scholar]
- 28.Kumar MA, Chanderraj R, Gant R, Butler C, Frangos S, Maloney-Wilensky E,et al. Obesity is associated with reduced brain tissue oxygen tension after severe brain injury.Neurocrit Care. 2012;16:286–93. 10.1007/s12028-011-9576-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hagau N, Slavcovici A, Gonganau DN, Oltean S, Dirzu DS, Brezoszki ES,et al. Clinical aspects and cytokine response in severe H1N1 influenza A virus infection. Crit Care. 2010;14:R203 10.1186/cc9324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stapleton RD, Dixon AE, Parsons PE, Ware LB, Suratt BT; NHLBI Acute Respiratory Distress Syndrome Network.The association between BMI and plasma cytokine levels in patients with acute lung injury. Chest. 2010;138:568–77. 10.1378/chest.10-0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yao S, Mao T, Fang W, Xu M, Chen W. Incidence and risk factors for acute lung injury after open thoracotomy for the thoracic diseases.J Thorac Dis. 2013;5:455–60. 10.3978/j.issn.2072-1439.2013.08.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Towfigh S, Peralta MV, Martin MJ, Salim A, Kelso R, Sohn H, et al. Acute respiratory distress syndrome in nontrauma surgical patients: a 6-year study. J Trauma.2009;67:1239–43. 10.1097/TA.0b013e31818b1733 [DOI] [PubMed] [Google Scholar]
- 33.Morris AE, Stapleton RD, Rubenfeld GD, Hudson LD, Caldwell E, Steinberg KP.The association between body mass index and clinical outcomes in acute lung injury.Chest. 2007;131:342–8. 10.1378/chest.06-1709 [DOI] [PubMed] [Google Scholar]
- 34.National Institutes of Health, National Heart, Lung, and Blood Institute: The practical guide: identification, evaluation, and treatment of overweight and obesity in adults. Available: http://www.nhlbi.nih.gov/files/docs/guidelines/prctgd_c.pdf.
- 35.Kim JA, Park HS. White blood cell count and abdominal fat distribution in female obeseadolescents. Metabolism. 2008; 57:1375–1379. 10.1016/j.metabol.2008.05.005 [DOI] [PubMed] [Google Scholar]
- 36.Desai MY, Dalal D, Santos RD, Carvalho JA, Nasir K, Blumenthal RS. Association of body mass index, metabolic syndrome, and leukocyte count. Am J Cardiol. 2006; 97:835–838. 10.1016/j.amjcard.2005.10.021 [DOI] [PubMed] [Google Scholar]
- 37.Ramos EJ, Xu Y, Romanova I, Middleton F, Chen C, Quinn R,et al. Is obesity an inflammatory disease? Surgery. 2003; 134:329–35 10.1067/msy.2003.267 [DOI] [PubMed] [Google Scholar]
- 38.Yudkin JS. Adipose tissue, insulin action and vascular disease: inflammatory signals. Int J Obes Relat Metab Disord. 2003; 27(Suppl 3):S25–S28. 10.1038/sj.ijo.0802496 [DOI] [PubMed] [Google Scholar]
- 39.Simpson SQ, Casey LC. Role of tumor necrosis factor in sepsis and acute lung injury. Crit CareClin. 1989; 5:27–47. [PubMed] [Google Scholar]
- 40.Klein CL, Hoke TS, Fang WF, Altmann CJ, Douglas IS, Faubel S. Interleukin-6 mediates lunginjury following ischemic acute kidney injury or bilateral nephrectomy. Kidney Int. 2008;74:901–909. 10.1038/ki.2008.314 [DOI] [PubMed] [Google Scholar]
- 41.Cottam DR, Schaefer PA, Shaftan GW, Velcu L, Angus LD. Effect of surgically-induced weight loss on leukocyte indicators of chronic inflammation in morbid obesity. Obes Surg. 2002; 12:335–342. [DOI] [PubMed] [Google Scholar]
- 42.Blann AD, Bushell D, Davies A, Faragher EB, Miller JP, McCollum CN. von Willebrand factor, the endothelium and obesity. Int J Obes Relat Metab Disord. 1993; 17:723–725. [PubMed] [Google Scholar]
- 43.Pontiroli AE, Frige F, Paganelli M, Folli F. In morbid obesity, metabolic abnormalities and adhesion molecules correlate with visceral fat, not with subcutaneous fat: effect of weight loss through surgery. Obes Surg.2009; 19:745–750. 10.1007/s11695-008-9626-4 [DOI] [PubMed] [Google Scholar]
- 44.Shah D, Romero F, Duong M, Wang N, Paudyal B, Suratt BT, et al. Obesity-induced adipokine imbalance impairs mouse pulmonary vascular endothelial function and primes the lung for injury. Sci Rep. 2015;5:11362 10.1038/srep11362 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 45.Bellmeyer A, Martino JM, Chandel NS, Scott Budinger GR, Dean DA, Mutlu GM. Leptinresistance protects mice from hyperoxia-induced acute lung injury. Am J Respir Crit Care Med.2007; 175:587–594. 10.1164/rccm.200603-312OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jain M, Budinger GR, Lo A, Urich D, Rivera SE, Ghosh AK,et al. Leptin promotes fibroproliferative acute respiratory distresssyndrome by inhibiting peroxisome proliferator-activated receptor-gamma. Am J Respir Crit CareMed. 2011;183:1490–8. 10.1164/rccm.201009-1409OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Konter JM, Parker JL, Baez E, Li SZ, Ranscht B, Denzel M,et al. Adiponectin attenuates lipopolysaccharide-induced acute lunginjury through suppression of endothelial cell activation. J Immunol. 2012;188:854–863. 10.4049/jimmunol.1100426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gattinoni L, Chiumello D, Carlesso E, Valenza F. Bench-to-bedside review: chest wall elastance in acute lung injury/acute respiratory distress syndrome patients. Crit Care. 2004; 8:350–355. 10.1186/cc2854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hess DR, Bigatello LM. The chest wall in acute lung injury/acute respiratory distress syndrome. Curr Opin Crit Care. 2008; 14:94–102. 10.1097/MCC.0b013e3282f40952 [DOI] [PubMed] [Google Scholar]
- 50.Kordonowy LL, Burg E, Lenox CC, Gauthier LM, Petty JM, Antkowiak M, et al. Obesity is associated with neutrophil dysfunction and attenuation of murine acute lung injury. Am J Respir Cell Mol Biol. 2012;47:120–7. 10.1165/rcmb.2011-0334OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ubags ND, Burg E, Antkowiak M, Wallace AM, Dilli E, Bement J,et al. A comparative study of lung host defense in murine obesity models. Insights into neutrophil function.Am J Respir Cell Mol Biol. 2016;55:188–200. 10.1165/rcmb.2016-0042OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schenkeveld L, Magro M, Oemrawsingh RM, Lenzen M, Lenzen M, de Jaegere P, et al. The influence of optimal medical treatment on the 'obesity paradox', body mass index and long-term mortality in patients treated with percutaneous coronary intervention: a prospective cohort study. BMJ Open. 2012;2:e000535 10.1136/bmjopen-2011-000535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chang HW, Li YH, Hsieh CH, Liu PY, Lin GM.Association of body mass index with all-cause mortality in patients with diabetes: a systemic review and meta-analysis. Cardiovasc Diagn Ther. 2016;6:109–19. 10.21037/cdt.2015.12.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xu W, Shubina M, Goldberg SI, Turchin A.Body mass index and all-cause mortality in patients with hypertension. Obesity (Silver Spring). 2015;23:1712–20. 10.1002/oby.21129 [DOI] [PubMed] [Google Scholar]
- 55.Kapoor JR, Heidenreich PA. Obesity and survival in patients with heart failure and preserved systolic function: a U-shaped relationship.Am Heart J. 2010;159:75–80. 10.1016/j.ahj.2009.10.026 [DOI] [PubMed] [Google Scholar]
- 56.Gu WJ, Wan YD, Tie HT, Kan QC, Sun TW. Risk of acute lung injury/acute respiratory distress syndrome in critically ill adult patients with pre-existing diabetes: a meta-analysis. PLoS One. 2014;9:e90426 10.1371/journal.pone.0090426 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(TIF)
(TIF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.