Abstract
Background
National joint replacement registries outside North America have been effective in reducing revision risk. However, there is little information on the role of smaller regional registries similar to those found in Canada or the United States. We sought to understand trends in total hip (THA) and knee (TKA) arthroplasty revision patterns after implementation of a regional registry.
Methods
We reviewed our regional joint replacement registry containing all 30 252 cases of primary and revision THA and TKA performed between Jan. 1, 2005, and Dec. 31, 2013. Each revision case was stratified into early (< 2 yr), mid (2–10 yr) or late (> 10 yr), and we determined the primary reason for revision.
Results
The early revision rate for TKA dropped from 3.0% in 2005 to 1.3% in 2011 (R2 = 0.84, p = 0.003). Similarly, the early revision rate for THA dropped from 4.2% to 2.1% (R2 = 0.78, p = 0.008). Despite primary TKA and THA volumes increasing by 35.5% and 39.5%, respectively, there was no concomitant rise in revision volumes. The leading reasons for TKA revision were infection, instability, aseptic loosening and stiffness. The leading reasons for THA revision were infection, instability, aseptic loosening and periprosthetic fracture. There were no discernible trends over time in reasons for early, mid-term or late revision for either TKA or THA.
Conclusion
After implementation of a regional joint replacement registry we observed a significant reduction in early revision rates. Further work investigating the mechanism by which registry reporting reduces early revision risk is warranted.
Abstract
Contexte
Ailleurs qu’en Amérique du Nord, les registres nationaux des remplacements articulaires ont été efficaces pour réduire le risque de révision. Cependant, il y a peu d’information sur le rôle des plus petits registres régionaux comme ceux qu’on trouve au Canada et aux États-Unis. Nous avons donc cherché à comprendre les tendances en matière de révision des arthroplasties totales de la hanche (ATH) et du genou (ATG) après la création d’un registre régional.
Méthodes
Nous avons passé en revue notre registre régional des remplacements articulaires, qui contient les 30 252 ATH et ATG primaires et de révision effectuées entre le 1er janvier 2005 et le 31 décembre 2013. Chaque cas de révision a été classé précoce (< 2 ans), moyen (de 2 à 10 ans) ou tardif (> 10 ans), et nous avons déterminé la raison principale de la révision.
Résultats
Le taux de révision précoce pour l’ATG a diminué de 3,0 % en 2005 à 1,3 % en 2011 (R2 = 0,84, p = 0,003). De même, le taux de révision précoce pour l’ATH a diminué de 4,2 % à 2,1 % (R2 = 0,78, p = 0,008). Malgré une augmentation des nombres d’ATG et d’ATH primaires de 35,5 % et de 39,5 %, respectivement, il n’y a pas eu de hausse concomitante du nombre de révisions. Les principaux motifs de révision de l’ATG étaient l’infection, l’instabilité, le descellement aseptique et la raideur. Les principaux motifs de révision de l’ATH étaient l’infection, l’instabilité, le descellement aseptique et les fractures périprothétiques. Aucune tendance n’a été décelée au fil du temps dans les motifs de révision précoce, moyenne et tardive pour l’une ou l’autre des interventions.
Conclusion
Nous avons observé une baisse significative des taux de révision précoce après la mise en oeuvre d’un registre régional des remplacements articulaires. Il serait pertinent d’étudier plus en profondeur le mécanisme par lequel le signalement dans un registre réduit le risque de révision précoce.
It is generally accepted that lower extremity joint replacement registries are effective at reducing revision risk following elective primary total knee (TKA) and total hip arthroplasty (THA) by providing outcome information to surgeons, hospitals and administrators. For example, recent reports from both the Swedish hip and knee arthroplasty registries document decreasing revision risk with each passing decade over the past 40 years.1,2 The reasons for the reduction in revision rate are no doubt multifactorial, and likely include such elements as patient and implant selection, surgical technique and postoperative care. The Australian joint replacement registry has implemented a method to facilitate prompt identification of “outlier” prostheses, thus facilitating abandoning implants that have higher than expected early revision risk.3 The most recent Swedish hip arthroplasty registry has demonstrated a reduced early THA revision risk attributable to a decrease in revisions for instability; this may be explained by the increased use of large head sizes,1 which has also been reported in the National Joint Registry (NJR) of England and Wales.4 Based on findings from previous registry reports demonstrating revision risks associated with patellar component use, Swedish surgeons now resurface the patella in less than 3% of their patients.2
While robust joint replacement registries have been in place for decades outside North America, there is little evidence of their effectiveness in a North American context, since there are no registries in either Canada5 or the United States6 that have capture rates above 90% or that routinely report on revision risk. This leaves North American surgeons dependent upon international registry reports, making it unclear whether registry reporting in Canada or the United States would be associated with the same positive effect on revision rates seen in other countries. Accordingly, we decided to examine patterns of THA and TKA revisions after implementation of a regional joint replacement registry in a Canadian health authority. Specifically, we sought to determine trends in THA and TKA revision caseload, early (< 2 yr) revision rate and reasons for revisions since implementation of our registry.
Methods
The Winnipeg Regional Health Authority (WRHA) is Manitoba’s largest health authority, serving a large proportion of Manitoba’s 1.2 million residents with 2 tertiary and 4 community hospitals. The province has a single-payer health care system that provides all necessary hospital, medical and surgical services, and private purchasing of joint replacement surgery is not allowed; this characteristic, along with Winnipeg’s relative geographic isolation, allows for nearly complete capture of all primary and revision TKAs and THAs. Currently, the region performs approximately 3000 primary and revision joint replacements per year among 19 surgeons.
Description of the registry
In partnership with the Manitoba Orthopaedic Society, the WRHA regional joint replacement registry was initiated in 2004 with partial coverage and expanded to full mandatory coverage in 2005. The registry collects patient demographic data; disease-specific and generic health related quality-of-life data both preoperatively and 1 year postoperatively; intraoperative information related to diagnosis, surgical technique and implant details; and 1-year self-reported complications and satisfaction. Funding for the registry is provided by the WRHA surgery program. Preoperative data capture occurs in the preadmission clinic under the guidance of the clinic nurse. Operating room nurses are responsible for ensuring that operative details are captured on the registry form. Postoperative data are collected via mail out, which is conducted by registry staff. Data entry is undertaken by both the hospital medical records department for hospital stay characteristics, and by the registry staff for patient-reported outcome measures. Surgical volumes are tracked through operative slate reconciliation with the regional orthopedic wait list database. Data from these 3 sources (hospital medical records, orthopedic wait list and patient-reported outcome measures) are combined to generate reports on a yearly basis for each surgeon performing TKA or THA and for each hospital site. All reports are reviewed by the WRHA Orthopaedic Standards and Quality Committee, while surgeons with outcomes inferior to regional averages for 2 or more years meet with the committee for review.
Study sample
This study received ethical approval from our university research ethics board. All patients who underwent either primary or revision TKA or THA within the WRHA between Jan. 1, 2005, and Dec. 31, 2013, were included in the study. When determining the 2-year revision rate, only primary joints inserted between Jan. 1, 2005, and Dec. 31, 2011, were included, as they all had a minimum of 2 years of follow-up at the time of analysis (January 2014). For revision cases, the reason for revision and date of the primary joint replacement were extracted from the registry; this was supplemented with data from the medical chart if the reason for revision was missing, or if the joint being revised was inserted before initiation of the registry. The primary reason for revision was coded using the same diagnostic codes as the Canadian Joint Replacement Registry.5
Statistical analysis
Primary and revision volumes were plotted year over year to look for trends. We calculated the 2-year revision rate as the proportion of THAs or TKAs revised within 2 years of the index procedure. Multiple revisions of the same joint were counted only once. We performed linear regression to assess the association between revision rate and year of surgery. For revision cases, the time to revision was stratified as early (< 2 yr), mid (2–10 yr) or late (> 10 yr). We then graphically plotted the top 4 reasons for revision as proportions, stratified by time frame and procedure, to examine trends.
Results
We identified 10 920 primary and 1811 revision THAs and 16 202 primary and 1501 revision TKAs in the registry. After exclusion of repeat revisions and cases for which there was no information on either the date of the primary procedure or the reason for revision, 930 revision THAs and 734 revision TKAs were available for inclusion in our reason for revision analysis.
The average ages of primary and revision TKA patients were 67.1 and 66.9 years, respectively; 61.6% of the primary and 56.5% of the revision TKA patients, respectively, were women. The average ages of primary and revision THA patients were 67.5 and 68.7 years, respectively; 55.7% of the primary and 54.6% of the revision THA patients, respectively, were women. The average body mass index (BMI) of primary TKA and THA patients was 32.6 and 29.2, respectively.
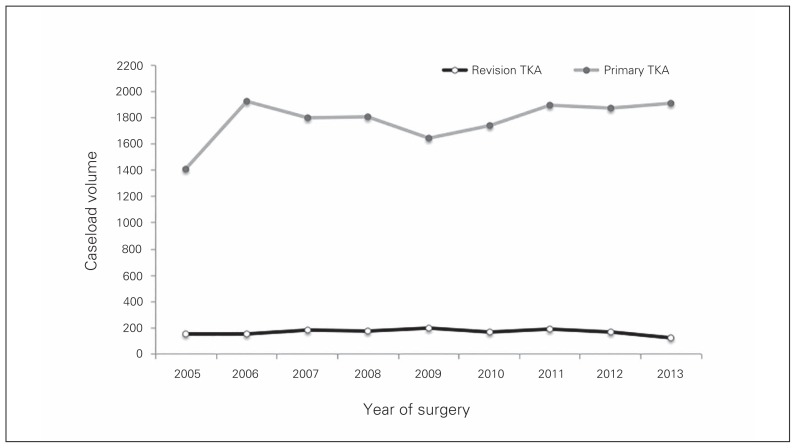
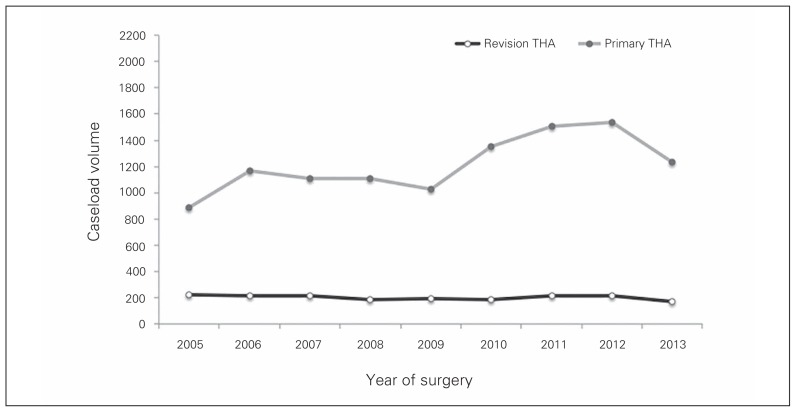
Despite the yearly primary TKA volumes increasing by 35.5% from 1412 procedures in 2005 to 1913 procedures in 2013, the yearly revision TKA volumes stayed fairly constant at an average of 166 procedures per year (Fig. 1) As a proportion of total procedures, revision TKA dropped from 9.7% (151 of 1563) in 2005 to 6.0% (123 of 2036) in 2013. Similarly, yearly primary THA volumes increased by 39.5% from 884 procedures in 2005 to 1234 procedures in 2013, with yearly THA revision volumes staying relatively constant at an average of 201 cases per year (Fig. 2). As a proportion of total procedures, revision THA dropped from 20.2% (224 of 1108) in 2005 to 11.9% (167 of 1401) in 2013.
Fig. 1.
Primary and revision total knee arthroplasty (TKA) volumes throughout the study period.
Fig. 2.
Primary and revision total hip arthroplasty (THA) volumes throughout the study period.
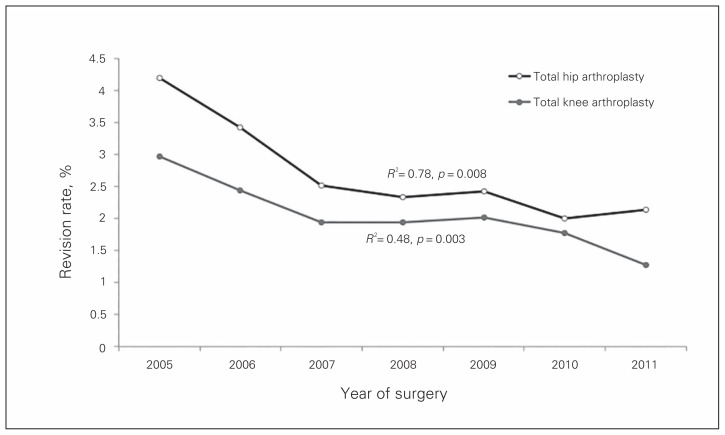
The early (< 2 yr) revision rate for TKA improved nearly every year, dropping from 3.0% (42 of 1412) in 2005 to 1.3% (24 of 1895) in 2011; this downward trend was significant (R2 = 0.84, p = 0.003). Similarly, the early revision rate for THA dropped nearly every year, from a high of 4.2% (37 of 884) in 2005 to 2.1% (32 of 1504) in 2013 (R2 = 0.78, p = 0.008; Fig. 3).
Fig. 3.
Early revision rates for total hip and total knee arthroplasty.
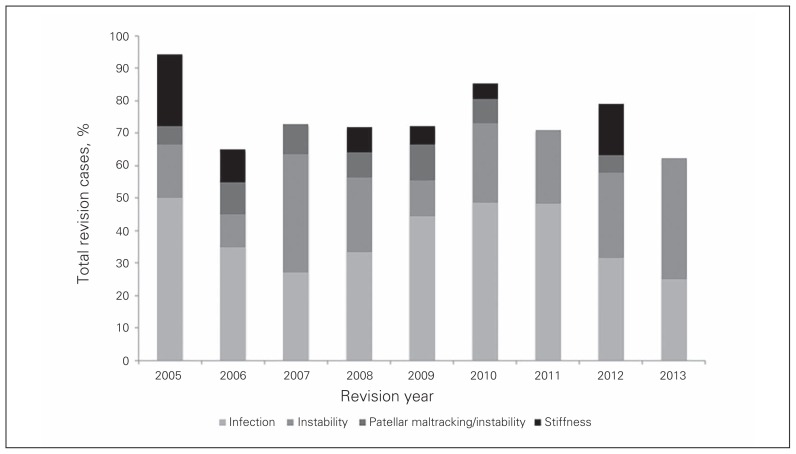
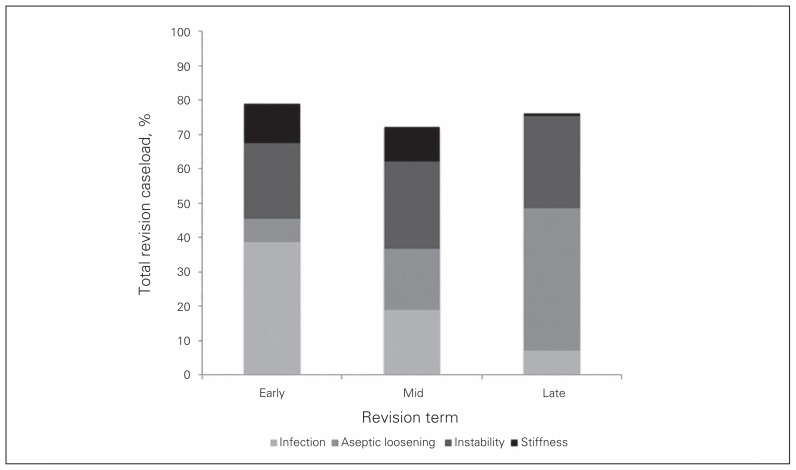
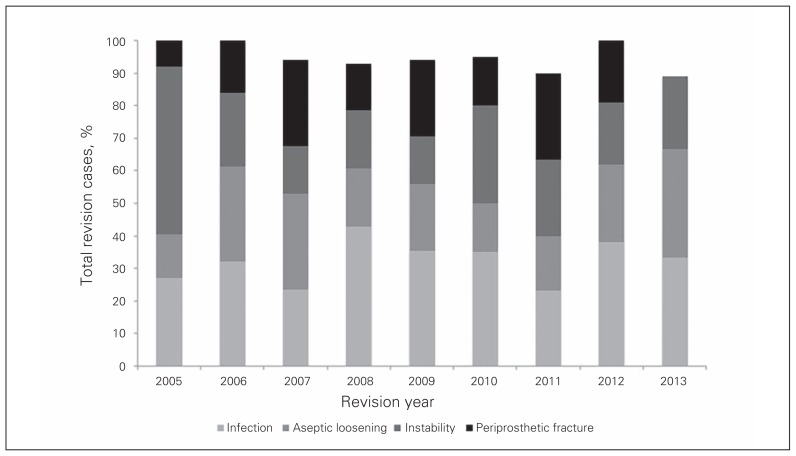
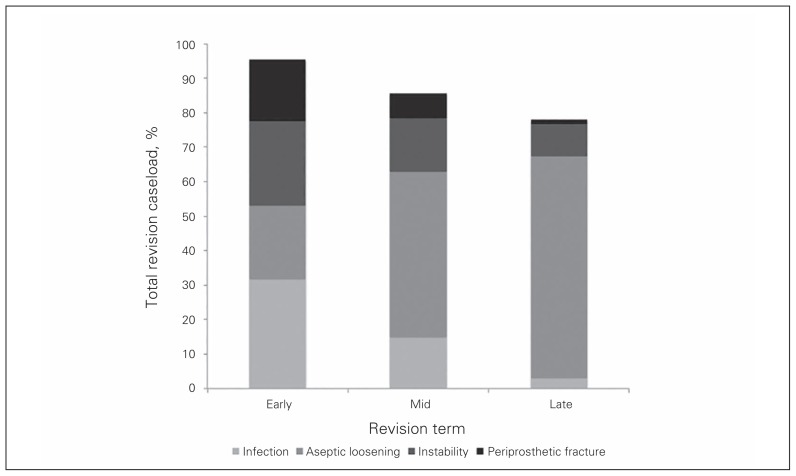
The top 4 reasons for early (< 2 yr) TKA revision were infection (39%), instability (22%), stiffness (12%) and patella mal-tracking or instability (7%). There was no discernible change to this distribution of reasons from 2005 to 2013 (Fig. 4). Figure 5 illustrates how the reasons for TKA revision changed with the revision period (early, mid, late). As the time to revision increased from early to mid to late, infection dropped from 39% to 19% to 7%, instability increased from 22% to 25% to 27%, stiffness dropped from 12% to 10% to 1%, and aseptic loosening increased from 7% to 18% to 41%. The top 4 reasons for early (< 2 yr) THA revision were infection (32%), aseptic loosening (21%), instability (25%) and periprosthetic fracture (18%). There was no discernible change to this distribution of reasons from 2005 to 2013 (Fig. 6). Figure 7 illustrates how the reasons for THA revision changed with the revision period. As the time to revision increased from early to mid to late, infection dropped from 32% to 15% to 3%, aseptic loosening increased from 21% to 55% to 71%, instability decreased from 25% to 15% to 9%, and periprosthetic fracture decreased from 18% to 8% to 1%.
Fig. 4.
Reasons for early revision of total knee arthroplasty during the study period.
Fig. 5.
Reasons for total knee arthroplasty revision changed depending on the revision period (early, mid, late).
Fig. 6.
Reasons for early revision of total hip arthroplasty during the study period.
Fig. 7.
Reasons for total hip arthroplasty revision changed depending on the revision period (early, mid, late).
Discussion
Since implementation of the registry, there has been a drop in the early (< 2 yr) revision rate for both TKA and THA. This finding is consistent with results reported by others on the effects of implementation of a registry. For example, Sweden’s 2-year revision rate for primary TKA dropped from approximately 5% for the decade 1976–1986 to approximately 2% for the decade 1986–1995.2 Examining more recent data, the Swedes have seen a drop in early THA revision risk from approximately 2.5% for the decade 1993–2002 to 2.0% for the decade 2003–2012.1 Our early revision rates of 1.3% for TKA and 2.1% for THA are similar to those found in the Australian registry of approximately 2.0% for TKA and 2.1% for THA.7
Despite a significant increase in primary TKA and THA volumes over the time period examined (35.5% and 39.5%, respectively), there was no concurrent increase in the volume of revision procedures. This occurred because the falling early revision rate prevented an increase in early revision burden that would have been expected from the increased primary joint replacement volumes. This finding differs significantly from the rest of Canada; during this period revision TKA volumes increased nationally by 50.0%, and revision THA volumes increased nationally by 38.5%.8,9 Our revision hip replacement burden of 11.9% is slightly higher than the Canadian average of 11.1% (excluding partial hip replacements), but our knee revision burden of 6.0% compares favourably to the Canadian national average of 6.8%.5 The revision burden in the United States may be higher. Using data from 1990 to 2002, Kurtz and colleagues10 found that 8.2% of knee replacements and 17.5% of hip replacements were revision procedures.
We found that the leading reasons for early TKA revision were infection, instability, stiffness and patella maltracking or instability. Owing to differences in coding and reporting time frame, it is difficult to compare these findings to those of studies examining other registries. However, these reasons are similar to those found in both the Australian Registry7 and the NJR4 (Table 1). The top 4 reasons for early THA revision in our registry were infection, aseptic loosening, instability and periprosthetic fracture; again, these are similar to those found in both the Australian Registry7 and the NJR4 (Table 2). The reasons for revision reported in the Swedish1,2 and Canadian5 Joint Replacement Registries could not be stratified into those associated with early, mid, or late time frames because the time frames were not reported.
Table 1.
Top 4 reasons for revision TKA by term and registry
| Term\registry | AJRR 2013 | NJR 2014* | Present study |
|---|---|---|---|
| Early (< 2 yr) | Infection | Infection | Infection |
| Loosening/lysis | Aseptic loosening | Instability | |
| Patellofemoral pain | Pain | Stiffness | |
| Pain | Lysis | Patella maltracking | |
| Mid (2–10 yr) | Loosening/lysis | Aseptic loosening | Instability |
| Infection | Pain | Infection | |
| Patellofemoral pain | Lysis | Aseptic loosening | |
| Pain | Infection | Stiffness | |
| Late (> 10 yr) | Loosening/lysis | — | Aseptic loosening |
| Infection | — | Instability | |
| Patellofemoral pain | — | Infection | |
| Pain | — | Stiffness |
AJRR = Australian Joint Replacement Registry; NJR = National Joint Registry; TKA = total knee arthroplasty.
Estimated from report owing to difference in reporting methods.
Table 2.
Top 4 reasons for revision THA by term and registry
| Term\registry | AJRR 2013 | NJR 2014* | Present study |
|---|---|---|---|
| Early (< 2 yr) | Dislocation | Dislocation | Infection |
| Loosening/lysis | Periprosthetic fracture | Aseptic loosening | |
| Infection | Infection | Instability | |
| Fracture | Aseptic loosening | Periprosthetic fracture | |
| Mid (2–10 yr) | Loosening/lysis | Pain | Aseptic loosening |
| Dislocation | Aseptic loosening | Instability | |
| Infection | Lysis | Infection | |
| Fracture | Dislocation | Periprosthetic fracture | |
| Late (> 10 yr) | Loosening/lysis | Aseptic loosening | |
| Dislocation | Instability | ||
| Fracture | Infection | ||
| Infection | Fracture |
AJRR = Australian Joint Replacement Registry; NJR = National Joint Registry; THA = total hip arthroplasty.
Estimated from report owing to difference in reporting methods.
The reasons for revision changed as the interval from the primary procedure increased. Revision for infection dropped for both knees and hips; this was expected as the early infections were likely related to the surgical procedure and the later ones to hematogenous spread. As the time frame increased, revision for aseptic loosening increased for both TKA and THA, which again we expected as a result of implant wear and osteolysis.
Limitations
Our study has a number of limitations. First, we were unable to include all of the revision procedures in our analysis of reasons for revision, as we were missing either the date of the primary procedure or the reason for revision in 33.8% (508 of 1501) of the revision TKAs and 36.7% (664 of 1811) of the revision THAs. The date of the primary procedure was incomplete because either the index procedure occurred before the registry was established, occurred outside of our health region, and/or the original operative report was unavailable. Data on the reason for revision were occasionally unavailable if they were not contained in either the registry (incomplete registry form completion) or in the revision procedure operation details in the medical chart. This limitation would affect primarily the late term revisions, and to a lesser extent the midterm revisions. Importantly, this limitation does not affect the early revision rate, as this was calculated using only primary procedures recorded in the registry.
Second, we did not look at the possible confounding effect of patient, surgical or implant characteristics on revision rates. However, in a separate analysis of the same data set, we found that patient characteristics and disease severity have not changed over the time period examined (data not shown), and we feel that motivating surgeons to improve both surgical technique and implant selection is an intended effect of the registry.
Third, since this is an observational study and not an experimental one, it is not possible for us to definitively conclude that our findings of decreased revision rates were a direct result of initiating the registry; they may in fact reflect pre-existing trends or other care improvement initiatives. However, the knowledge gained from registry reporting is broadly acknowledged to facilitate improvement in care, and a recent Cochrane review found support for the effectiveness of audit and feedback at driving improvement.11
Conclusion
Initiation of a regional joint replacement registry that incorporates individual surgeon performance review and feedback appears to be associated with a reduction in early revision rates. In our region, this allowed for a significant increase in primary TKA and THA procedures without an associated increase in revision volumes. Further work investigating the mechanism by which registry reporting reduces early revision risk is warranted.
Footnotes
Competing interests: L. Louks was employed as a researcher with the Concordia Joint Replacement Group during the conduct of the study. No other competing interests declared.
Contributors: All authors designed the study. J. Singh, A. Politis, L. Louks and E. Bohm acquired and analyzed the data and wrote the article, which all authors reviewed and approved for publication.
References
- 1.Garellick G, Rogmark C, Karrholm J, et al. Swedish Hip Arthroplasty Register Annual Report 2012. Sweden: 2012. [Google Scholar]
- 2.Swedish Knee Arthroplasty Register. Lund, Sweden: 2013. [Google Scholar]
- 3.de Steiger RN, Miller LN, Davidson DC, et al. Joint registry approach for identification of outlier prostheses. Acta Orthop. 2013;84:348–52. doi: 10.3109/17453674.2013.831320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Joint Registry. 11th Annual Report for England, Wales and Northern Ireland. Bristol: 2014. [Google Scholar]
- 5.Canadian Institute for Health Information. Hip and knee replacements in Canada: Canadian Joint Replacement Registry 2014 annual report. [Google Scholar]
- 6.Ayers DC, Franklin PD. Joint replacement registries in the United States: a new paradigm. J Bone Joint Surg Am. 2014;96:1567–9. doi: 10.2106/JBJS.N.00641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Australian Orthopaedic Association. National Joint Replacement Registry. Annual Report 2013. Adelaide: [Google Scholar]
- 8.Canadian Institute for Health Information. Hip and knee replacements in Canada: Canadian Joint Replacement Registry 2015 annual report. [Google Scholar]
- 9.Canadian Institute for Health Information. 2007 CJRR report: total hip and knee replacements in Canada. [Google Scholar]
- 10.Kurtz S, Mowat F, Ong K, et al. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–97. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 11.Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;6:CD000259. doi: 10.1002/14651858.CD000259.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]