Abstract
The compounds, which are obtained from natural plants or microbes may offer potential as one of the strategies for the management of cholangiocarcinoma. Oblongifolin C (OC), a natural small molecule compound extracted and purified from Garcinia yunnanensis Hu, can activate the mitochondrial apoptotic pathway in human cervical cancer cells. However, the direct effects of OC on cholangiocarcinoma cells are not well defined. The effect of OC on cell apoptosis and its underlying mechanisms were investigated in cultured QBC939 cells by the methyl thiazol tetrazolium assay, mitochondrial membrane potential, ATP content and western blot analysis. The present study reported that the in vitro treatment of human cholangiocarcinoma QBC939 cells with different concentrations (5, 10, 20 and 40 μM) of OC decreased cell viability and induced apoptosis in a dose-dependent manner. The results of the present study also showed that OC-induced QBC939 cell apoptosis was mediated through the inhibition of autophagy and mitochondrial dysfunction (MtD). Additionally, inhibiting autophagy increased OC-induced apoptosis and MtD, whereas exposure to the autophagy inducer, rapmycin, attenuated these changes. Together, the results of the present study are the first, to the best of our knowledge, to identify OC as a chemotherapeutic agent against human cholangiocarcinoma QBC939 cells in vitro via the regulation of autophagy and MtD.
Keywords: oblongifolin C, cholangiocarcinoma, autophagy, mitochondrial dysfunction, apoptosis
Introduction
Increasing evidence indicates that the incidence of cholangiocarcinoma has risen in previous decades (1,2). Due to difficulties in early diagnosis and relative resistance of the tumors to chemotherapy, the prognosis of patients with cholangiocarcinoma remains poor (3,4). Although palliative surgical resection has been considered to be the mainstay treatment for cholangiocarcinoma, the high mortality rate and low 5-year survival rate warrants the investigation of novel approaches to overcome the issue (5).
Macroautophagy, hereafter referred to as autophagy, is an evolutionarily conserved catabolic mechanism to suppress carcinogenesis by eliminating oncogenic molecules and damaged organelles (6). Autophagy fuels cancer cell metabolism (6), and is involved in the abnormal proliferation and invasion of cells, and in resistance to chemotherapy and radiation therapy. The inhibition of autophagy can result in mitochondrial dysfunction (MtD), which leads to cell death (7,8), and may be a promising strategy for the treatment of cancer.
Natural products and their synthetic derivatives have been a continuous source of novel compounds for the treatment of cancer (9,10). Oblongifolin C (OC), a natural small molecule compound extracted and purified from Garcinia yunnanensis Hu, can activate a mitochondrial apoptotic pathway in human cervical cancer cells (11). In addition, Lao et al (12) demonstrated that OC is a novel autophagic flux inhibitor by inhibiting autophagosome-lysosome fusion and autophagic degradation.
Therefore, the primary aim of the present study was to determine whether the hypothesis that OC directly induces apoptosis via inhibiting autophagy and MtD in the human cholangiocarcinoma QBC939 cell line, is correct.
Materials and methods
Materials
The established QBC939 cell line was obtained from the Cell Bank of Wuhan University (Wuhan, China). OC, 3-methyladenine (3-MA) and rapamycin (RP) were purchased from Sigma-Aldrich (St. Louis, MO, USA). β-actin, microtubule-associated protein light chain 3 (LC3) and p62 antibodies were purchased from Cell Signaling Technology, Inc. (Beverly, MA, USA). All other chemicals were of analytical grade.
Cell culture
The cells were maintained in Dulbecco's modified Eagle's medium (DMEM) supplemented with 10% fetal calf serum (FCS; Sigma-Aldrich) at 37°C in an atmosphere containing 5% CO2. When the cells reached 80–90% confluence, the cells were added to the DMEM (10% FCS in media) with different concentrations (5, 10, 20 and 40 μM) of OC for another 48 h.
Methylthiazole tetrazolium (MTT) assay
An MTT reduction assay was used as a qualitative index of cell viability. The effect of OC on cell viability was assessed as the percentage cell viability, compared with that of untreated control cells, which were arbitrarily assigned a viability of 100%.
Assessment of cell apoptosis
The cytosolic DNA-histone complexes generated during apoptotic DNA fragmentation in the treated QBC939 cells were evaluated using a cell death detection enzyme-linked immunosorbent assay kit (Cell Death Detection ELISA PLUS; Roche Applied Science, Indianapolis, IN, USA), according to the manufacturer's protocol.
Mitochondrial membrane potential (MMP)
The MMP of the QBC939 cells was monitored using JC-1, an MMP-sensitive fluorescent dye, as described previously (13). Briefly, the dissociated 90% confluent QBC939 cells were washed twice with Hank's balanced salt solution (Sigma-Aldrich) and incubated in the dark with JC-1 (7.5 mmol/l; Sigma-Aldrich) for 30 min at 37°C. The cells were then washed with JC-1 washing buffer, and fluorescence was detected by fluorescence-assisted cell sorting of the QBC939 cells. The relative MMP was calculated using the ratio of J-aggregate/monomer (590/520 nm).
Measurement of adenosine triphosphate (ATP) content
The ATP levels in 90% confluent QBC939 cells were determined using a luciferase-based bioluminescence assay kit (Sigma-Aldrich) in a FLUOstar Optima reader (BMG Labtech GmbH, Ortenberg, Germany), according to the manufacturer's protocol. The total ATP levels were determined as the respective luminescence normalized by the protein concentration.
Western blot analysis
The total cellular proteins from the cells of the respective groups were extracted by lysis of the cells with buffer containing 150 mM NaCl, 0.1% Triton X-100, 0.5% deoxycholate, 0.1% sodium dodecyl sulfate (SDS), 50 mM Tris-HCl (pH 7.0) and 1 mM ethylenediaminetetraacetic acid. Protein concentrations were determined using the bicinchoninic acid method (Beyotime Institute of Biotechnology, Haimen, China) Equal amounts of protein (50 μg) were subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis on 10 % gels and transferred to a polyvinylidene difluoride membrane. The membrane was blocked for 1 h with blocking buffer containing 5% non-fat dry milk and 0.05% Tween-20 in Tris-buffered saline, followed by overnight incubation at 4°C with the primary antibodies as follows: rabbit polyclonal anti-LC3 (1:1,000; cat. no. ab48394), mouse monoclonal anti-p62 (1:2,000; ab56416) and mouse monoclonal anti-β-actin (1:1,000; ab8226) obtained from Abcam (Cambridge, UK). Following further incubation with the corresponding secondary antibody (1:2,500; cat. no. A27041; Thermo Fisher Scientific, Inc., Waltham, MA, USA) for 2 h at room temperature, immune complexes were detected using enhanced chemiluminescence western blotting reagents (Sinopharm Chemical Reagent Co., Ltd., Shanghai, China). The relative intensity of each respective band was normalized to β-actin.
Statistical analysis
Quantitative data are presented as the mean ± standard deviation. Statistical significance was determined with one-way analysis of variance and Dunnett's post-test using GraphPad Prism software (version 6.0; GraphPad Software, Inc., La Jolla, CA, USA). P<0.05 was considered to indicate a statistically significant difference.
Results
OC decreases cell viability and induces apoptosis in human cholangiocarcinoma QBC939 cells
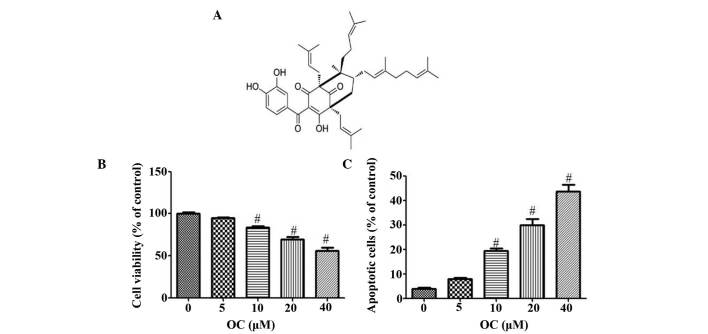
The chemical structure of OC is shown in Fig. 1A. The results of the MTT assay showed that, compared with the normal group, the addition of OC for 48 h inhibited human cholangiocarcinoma cell viability in a dose-dependent manner at concentrations between 10 and 40 μM (P<0.05; Fig. 1B). As shown in Fig. 1C, when compared with the control cholangiocarcinoma cells, without OC, treatment of the QBC939 cells with OC for 48 h resulted in a 16–23% (P<0.05) increase in cell apoptosis at 10 μM, a 21–39% (P<0.01) increase in cell death at 20 μM and a 38–52% (P<0.01) increase in cell death at 40 μM.
Figure 1.
Treatment of QBC939 cells with OC inhibits cell viability and induces cell death in a dose-dependent manner. (A) Chemical structure of OC. (B) Dose-dependent effect of OC on the cell viability of QBC939 cells. (C) Apoptotic effect of OC on QBC939 cells. Values are presented as the mean ± standard deviation from six independent experiments. #P<0.05, vs. control. OC, oblongifolin C.
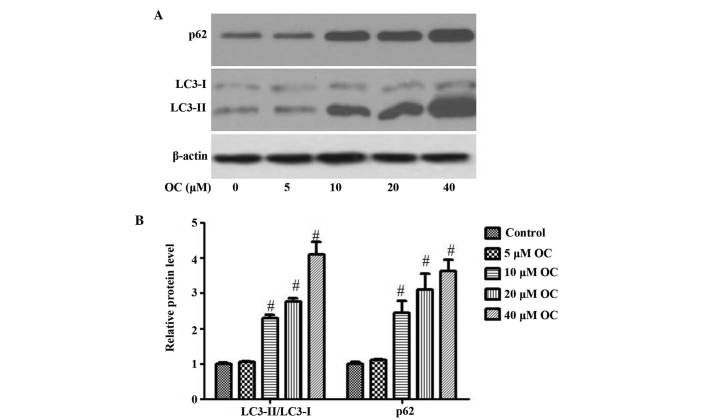
OC inhibits autophagy in QBC939 cells
To monitor autophagic fluctuation, the levels of LC3II/LC3I and p62, a selective substrate of autophagy, were measured in the QBC939 cells. Following incubation with different concentrations (5, 10, 20 and 40 μM) of OC for 48 h, the levels of LC3II/LC3I and p62 were increased, compared with the control cells (Fig. 2A and B). These results suggested that OC treatment inhibited cellular autophagic flux in the QBC939 cells.
Figure 2.
OC inhibits autophagic flux in QBC939 cells in a dose-dependent manner. (A) Western blot analysis was used to determine the protein expression of LC3II/LC3I, p62 and β-actin in QBC939 cells treated without or with different concentration of OC (0, 5, 10, 20 and 40 μM) for 48 h, as indicated. (B) Graphical presentation shows the relative abundances of LC3II/LC3I and p62 following normalization with β-actin. Data are presented as the mean ± standard error of the mean of three independent experiments. #P<0.05, vs. control. OC, oblongifolin C; LC3, microtubule-associated protein light chain 3.
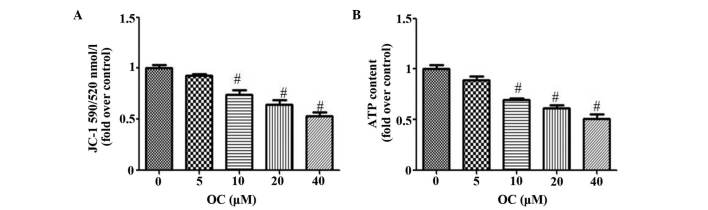
OC inhibits MtD in QBC939 cells
To evaluate the MtD, the present study used two independent parameters: Levels of MMP and ATP. MMP collapse has been shown to be important in the mediation of apoptosis, in which it allows the release of cytochrome c and activation of caspase-9, and subsequently leads to the apoptosis of cells (14). Mitochondria are also the energy powerhouses of cells and efficiently utilize the cell's ATP. Tumor cells consume a substantial quantities of energy supplied as ATP, therefore, any disruption in this supply is likely to cause cell death. As expected, OC reduced the MMP in a dose-dependent manner, as indicated by the reduction of JC-1 fluorescence at 590/520 nm (Fig. 3A). OC also reduced the production of ATP (Fig. 3B).
Figure 3.
OC inhibits mitochondrial dysfunction in QBC939 cells in a dose-dependent manner. Confluent QBC939 cells were exposed to vehicle (culture medium) or different concentrations of OC (0, 5, 10, 20 and 40 μM) for 48 h. (A) Mitochondrial membrane potential and (B) ATP content were determined. Values are presented the mean ± standard deviation (n=6). #P<0.05, vs. control. OC, oblongifolin C; ATP, adenosine triphosphate.
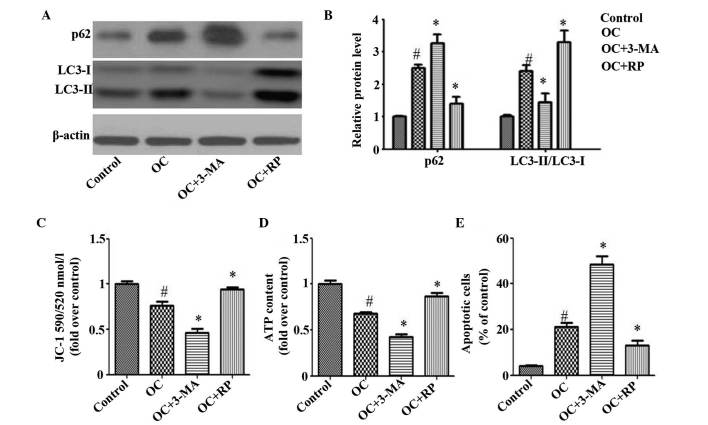
Pharmacological regulation of autophagy affects OC-induced apoptosis and MtD in QBC939 cells
Using pharmacological drugs to demonstrate the involvement of autophagy in the regulation of cell apoptosis has been widely acknowledged. In the present study, 3-MA, which inhibits autophagosomal cargo sequestration, and RP, an autophagy enhancer, were used to evaluate the effect of autophagy on OC-induced apoptosis and MtD in QBC939 cells. As the lowest level of induction was found in the 10 μM OC treatment group, 10 μM OC was used as a stimulation factor in the experiments. As expected, 3-MA inhibited autophagy, as demonstrated by the further accumulation of p62 and decrease in LC3II/LC3I, compared with the cells treated with OC alone (Fig. 4A and B). However, RP had the opposite effect (Fig. 4A and B). As shown in Fig. 4C–E, 3-MA treatment increased the OC-induced apoptosis and MtD of the QBC939 cells, whereas RP significantly improved the OC-induced changes.
Figure 4.
Autophagy affects OC-induced apoptosis and mitochondrial dysfunction in QBC939 cells. Confluent QBC939 cells were exposed to vehicle (culture medium) or 10 μM OC in the presence or absence of 3-MA or RP for 24 h. (A) Western blot analysis showed the protein expression of LC3II/LC3I, p62 and β-actin. (B) Graphical presentation shows the relative abundances of LC3II/LC3I and p62 following normalization with β-actin. (C) Mitochondrial membrane potential, (D) ATP content and (E) cell apoptosis were detected. Values are presented as the mean ± standard deviation (n=6). #P<0.05 vs. control; *P<0.05 vs. OC. OC, oblongifolin C; ATP, adenosine triphosphate; 3-MA, 3-methyladenine; RP, rapamycin.
Discussion
Cholangiocarcinoma remains one of the most difficult types of tumor to treat in clinical practice and novel therapeutic modalities are required, with the induction of cholangiocarcinoma apoptosis considered to be one promising therapeutic strategy.
Several toxic compounds from traditional Chinese medicines (15–17) exhibit antitumor effects and have been used for cancer therapy. OC has been acknowledged to activate a mitochondrial apoptotic pathway in human cervical cancer cells (11). However the effect of OC on cholangiocarcinoma remains to be elucidated. In the present study, it was shown that OC significantly reduced the viability and induced the apoptosis of the QBC939 cells (Fig. 1), which suggested that OC may be examined as an effective chemotherapeutic agent against cholangiocarcinoma.
It has been recognized that controlling the progression of autophagy in cancer cells is an effective strategy to inhibit tumor growth (18,19), and molecular analyses of human cancer have revealed that autophagy regulators are frequently deregulated in the majority of common malignancies (20,21). For this reason, the inhibition of autophagy has been regarded as a promising anticancer strategy to inhibit multiple cellular processes. The in vitro data obtained in the present study demonstrated that the treatment of QBC939 cells with OC, a novel autophagic flux inhibitor, inhibited the progression of autophagy (Fig. 2). Additionally, the pharmacological inhibition of autophagy increased OC-induced apoptosis, wheareas the promotion of autophagy attenuated OC-induced apoptosis, indicating that the inhibition of autophagy was one of the mechanisms by which OC induced the apoptosis of QBC939 cells (Fig. 4).
MtD represents a malfunction in biochemical processes, characterized by MMP collapse, which has been shown to be essential in the mediation of apoptosis (14). Furthermore, mitochondria are the energy powerhouses of cells and efficiently utilize the cell's ATP. Cancer cells consume a substantial quantity of energy supplied as ATP, therefore, any disruption in this supply is likely to cause the apoptosis of cells. An increasing number of studies have shown that the inhibition of autophagy often leads to MtD, which is usually associated with cell death (22,23). In the present study, it was found that OC inhibited autophagy, accompanied by MtD (Fig. 2), and that inhibiting autophagy increased OC-induced MtD, whereas treatment with RP attenuated this process (Fig. 4). These results indicated that MtD resulted from the inhibition of autophagy and may have contributed to the OC-induced apoptosis of QBC939 cells.
In conclusion, the present study provided the first evidence, to the best of our knowledge, that OC-induced apoptosis resulted from inhibition of autophagy and MtD in human cholangiocarcinoma QBC939 cells, and OC may offer potential as an effective agent for the prevention of cholangiocarcinoma.
Acknowledgments
This study was financially supported by the Scientific Research Program from Nanjing Medical University (grant nos. 2011NJMU251 and 2014NJMUZD068).
References
- 1.Shaib YH, Davila JA, McGlynn K, El-Serag HB. Rising incidence of intrahepatic cholangiocarcinoma in the United States: A true increase? J Hepatol. 2004;40:472–477. doi: 10.1016/j.jhep.2003.11.030. [DOI] [PubMed] [Google Scholar]
- 2.Landis SH, Murray T, Bolden S, Wingo PA. Cancer statistics, 1998. CA Cancer J Clin. 1998;48:6–29. doi: 10.3322/canjclin.48.1.6. [DOI] [PubMed] [Google Scholar]
- 3.Mittal B, Deutsch M, Iwatsuki S. Primary cancers of extrahepatic biliary passages. Int J Radiat Oncol Biol Phys. 1985;11:849–854. doi: 10.1016/0360-3016(85)90320-7. [DOI] [PubMed] [Google Scholar]
- 4.Pitt HA, Nakeeb A, Abrams RA, Coleman J, Piantadosi S, Yeo CJ, Lillemore KD, Cameron JL. Perihilar cholangiocarcinoma. Postoperative radiotherapy does not improve survival. Ann Surg. 1995;221:788–797. doi: 10.1097/00000658-199506000-00017. discussion 797–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boerma EJ. Research into the results of resection of hilar bile duct cancer. Surgery. 1990;108:572–580. [PubMed] [Google Scholar]
- 6.White E. Deconvoluting the context-dependent role for autophagy in cancer. Nat Rev Cancer. 2012;12:401–410. doi: 10.1038/nrc3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim MJ, Choi OK, Chae KS, Kim MK, Kim JH, Komatsu M, Tanaka K, Lee H, Chung SS, Kwak SH, et al. Mitochondrial complexes I and II are more susceptible to autophagy deficiency in mouse β-cells. Endocrinol Metab (Seoul) 2015;30:65–70. doi: 10.3803/EnM.2015.30.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dhingra R, Kirshenbaum LA. Regulation of mitochondrial dynamics and cell fate. Circ J. 2014;78:803–810. doi: 10.1253/circj.CJ-14-0240. [DOI] [PubMed] [Google Scholar]
- 9.Kang YJ, Park KK, Chung WY, Hwang JK, Lee SK. Xanthorrhizol, a natural sesquiterpenoid, induces apoptosis and growth arrest in HCT116 human colon cancer cells. J Pharmacol Sci. 2009;111:276–284. doi: 10.1254/jphs.09141FP. [DOI] [PubMed] [Google Scholar]
- 10.Chang JS, Lee SW, Kim MS, Yun BR, Park MH, Lee SG, Park SJ, Lee WS, Rho MC. Manassantin A and B from Saururus chinensis inhibit interleukin-6-induced signal transducer and activator of transcription 3 activation in Hep3B cells. J Pharmacol Sci. 2011;115:84–88. doi: 10.1254/jphs.10239SC. [DOI] [PubMed] [Google Scholar]
- 11.Feng C, Zhou LY, Yu T, Xu G, Tian HL, Xu JJ, Xu HX, Luo KQ. A new anticancer compound, oblongifolin C, inhibits tumor growth and promotes apoptosis in HeLa cells through Bax activation. Int J Cancer. 2012;131:1445–1454. doi: 10.1002/ijc.27365. [DOI] [PubMed] [Google Scholar]
- 12.Lao Y, Wan G, Liu Z, Wang X, Ruan P, Xu W, Xu D, Xie W, Zhang Y, Xu H, Xu N. The natural compound oblongifolin C inhibits autophagic flux and enhances antitumor efficacy of nutrient deprivation. Autophagy. 2014;10:736–749. doi: 10.4161/auto.28034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Acton BM, Jurisicova A, Jurisica I, Casper RF. Alterations in mitochondrial membrane potential during preimplantation stages of mouse and human embryo development. Mol Hum Reprod. 2004;10:23–32. doi: 10.1093/molehr/gah004. [DOI] [PubMed] [Google Scholar]
- 14.Mao WP, Ye JL, Guan ZB, Zhao JM, Zhang C, Zhang NN, Jiang P, Tian T. Cadmium induces apoptosis in human embryonic kidney (HEK) 293 cells by caspase-dependent and -independent pathways acting on mitochondria. Toxicol In Vitro. 2007;21:343–354. doi: 10.1016/j.tiv.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 15.He W, Wang B, Zhuang Y, Shao D, Sun K, Chen J. Berberine inhibits growth and induces G1 arrest and apoptosis in human cholangiocarcinoma QBC939 cells. J Pharmacol Sci. 2012;119:341–348. doi: 10.1254/jphs.12052FP. [DOI] [PubMed] [Google Scholar]
- 16.Fukuda T, Oda K, Wada-Hiraike O, Sone K, Inaba K, Ikeda Y, Miyasaka A, Kashiyama T, Tanikawa M, Arimoto T, et al. The anti-malarial chloroquine suppresses proliferation and overcomes cisplatin resistance of endometrial cancer cells via autophagy inhibition. Gynecol Oncol. 2015;137:538–545. doi: 10.1016/j.ygyno.2015.03.053. [DOI] [PubMed] [Google Scholar]
- 17.Jiang L, Zhao MN, Liu TY, Wu XS, Weng H, Ding Q, Shu YJ, Bao RF, Li ML, Mu JS, et al. Bufalin induces cell cycle arrest and apoptosis in gallbladder carcinoma cells. Tumour Biol. 2014;35:10931–10941. doi: 10.1007/s13277-014-1911-3. [DOI] [PubMed] [Google Scholar]
- 18.Sharma N, Thomas S, Golden EB, Hofman FM, Chen TC, Petasis NA, Schönthal AH, Louie SG. Inhibition of autophagy and induction of breast cancer cell death by mefloquine, an antimalarial agent. Cancer Lett. 2012;326:143–154. doi: 10.1016/j.canlet.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 19.Egger ME, Huang JS, Yin W, McMasters KM, McNally LR. Inhibition of autophagy with chloroquine is effective in melanoma. J Surg Res. 2013;184:274–281. doi: 10.1016/j.jss.2013.04.055. [DOI] [PubMed] [Google Scholar]
- 20.Schonewolf CA, Mehta M, Schiff D, Wu H, Haffty BG, Karantza V, Jabbour SK. Autophagy inhibition by chloroquine sensitizes HT-29 colorectal cancer cells to concurrent chemoradiation. World J Gastrointest Oncol. 2014;6:74–82. doi: 10.4251/wjgo.v6.i3.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu F, Shang Y, Chen SZ. Chloroquine potentiates the anti-cancer effect of lidamycin on non-small cell lung cancer cells in vitro. Acta Pharmacol Sin. 2014;35:645–652. doi: 10.1038/aps.2014.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hall AM, Unwin RJ. The not so 'mighty chondrion': Emergence of renal diseases due to mitochondrial dysfunction. Nephron Physiol. 2007;105:p1–p10. doi: 10.1159/000096860. [DOI] [PubMed] [Google Scholar]
- 23.Hagiwara M, Yamagata K, Capaldi RA, Koyama A. Mitochondrial dysfunction in focal segmental glomerulosclerosis of puromycin aminonucleoside nephrosis. Kidney Int. 2006;69:1146–1152. doi: 10.1038/sj.ki.5000207. [DOI] [PubMed] [Google Scholar]