Abstract
The Notch signaling pathway is a crucial regulator of numerous fundamental cellular processes. Increasing evidence suggests that Notch signaling is involved in inflammation and oxidative stress, and thus in the progress of cerebrovascular diseases. In addition, Notch signaling in cerebrovascular diseases is associated with apoptosis, angiogenesis and the function of blood-brain barrier. Despite the contradictory results obtained to date as to whether Notch signaling is harmful or beneficial, the regulation of Notch signaling may provide a novel strategy for the treatment of cerebrovascular diseases.
Keywords: cerebrovascular diseases, Notch signaling, inflammation, oxidative stress, apoptosis
1. Introduction
Cerebrovascular diseases occur following acute cerebrovascular events whereby the arteries of the brain are blocked or a brain blood vessel ruptures. Poor blood flow to the brain subsequently results in cell death. There are three primary types of cerebrovascular diseases: Ischemic stroke, hemorrhagic stroke and transient ischemic attack (TIA). The high incidence of cerebrovascular diseases worldwide is largely due to failed management and prevention of modifiable risk factors, particularly in ischemic stroke, which accounts for >85% of total cerebrovascular diseases. Cerebrovascular diseases more commonly affect people who are overweight, aged ≥55, have a unhealthy lifestyle (limited exercise, heavy drinking, use of illicit drugs, smoking or poor work/life balance), and who have a family history of stroke, hypertension, moyamoya, vasculitis, arterial dissection or venous occlusive disease (1–6). Cerebrovascular disease is the leading cause of mortality and chronic disability in China, and the third leading cause of mortality and the leading cause of chronic disability in the USA (7,8).
Notch signaling is a major intercellular communication pathway, which is highly conserved in the majority of multicellular organisms. Notch signaling is a crucial regulator of numerous fundamental cellular processes, including proliferation, stem cell maintenance and differentiation, during embryonic development in vertebrate and invertebrate organisms (9–11). In addition, Notch signaling is involved in cell differentiation, proliferation, inflammation (12), oxidative stress and apoptosis in a variety of cell types in adults (10,13). The primary mechanisms underlying the Notch signaling pathway in cerebrovascular disease have been well-established by extensive investigation (10,14,15), and include enhancing inflammation (16–18), increasing oxidative stress (19), promoting apoptosis (20) and mediating adult subventricular zone neural progenitor cell proliferation and differentiation following stroke (21). It has been demonstrated that activation of the Notch signaling pathway exacerbates ischemic brain damage, whereas inhibiting the Notch signaling pathway decreases the infarct size and improves the functional outcome in a mouse model of stroke (18,22).
The present review discusses the role of the Notch signaling pathway in the pathogenesis of cerebrovascular diseases. It primarily focuses on the association between Notch signaling and neuroinflammation, oxidative stress and apoptosis in cerebrovascular diseases. An overview is provided for the proposed pathogenic mechanism underlying Notch signaling in stroke via regulation of angiogenesis and the function of the blood–brain barrier (BBB). Finally, the efficacy of regulating Notch signaling as a novel therapeutic intervention for cerebrovascular diseases is considered.
2. Notch signaling pathway
The Notch gene, discovered in the wings of Drosophila melanogaster by Thomas Hunt Morgan in 1917 (23), is crucial for the regulation of various physiological processes (24,25). The Notch signaling pathway, comprised of Notch receptors (Notch1, Notch2, Notch3 and Notch4), Notch ligand and the transcription factor, CBF1/Suppressor of Hairless/L AG -1 (C S L) protein, is critical for numerous fundamental cellular processes, including proliferation, differentiation and survival, during embryonic and adult development (26–30). These effects are mediated by the transmembrane ligand-induced release of the Notch intracellular domain (NICD) and the interaction of this fragment with the CSL family of transcription factors within the nucleus (25,27,31). The Notch receptors are expressed on cell membrane surfaces, and thus can be cleaved by a disintegrin and metalloproteinase (ADAM) 17 or −10 and a presenilin-dependent γ-secretase complex. The cleaved NICD translocates to the nucleus, where it interacts with the ubiquitous transcription factor CSL and recruits co-activator mastermind-like proteins and therefore activates downstream target genes (32–34). In addition, CSL may inhibit the expression of target genes by forming transcription complexes in the absence of NICD.
Extensive evidence has revealed that the Notch signaling pathway is closely associated with the function and structure of the nervous system. In the central nervous system (CNS), the Notch signaling pathway regulates the normal development of neural progenitor cells, neurons, oligodendrocytes and astrocytes (35,36). Numerous diseases of the nervous system are associated with Notch mutations, including sporadic Alzheimer's disease (37,38), Down syndrome (39,40), Pick's disease (38) and cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) (41–44). The molecular and cellular mechanisms underlying the degeneration of brain cells affected by cerebrovascular disease are complex, involving bioenergetic failure, acidosis, excitotoxicity, oxidative stress and inflammation, and resulting in necrotic or apoptotic cell death (45,46). Various signaling pathways are involved, including Notch. For example, in cerebral ischemia, the activation of Notch regulates nerve damage repair, inflammation and angiogenesis in the vascular ischemic area via regulating proliferation and development of neuronal precursor cells, mediating the release of inflammatory factors and promoting angiogenesis (47–50). Studies in vitro and in vivo have demonstrated that blood vessel angiogenesis, endothelial cell proliferation, and artery and vein differentiation are regulated by the Notch signaling pathway (51–53). Enhancing Notch signaling activity promotes arteriogenesis via vascular smooth muscle cell (VSMC) proliferation in the ischemic brain following stroke (51,54,55).
3. Notch signaling and neuroinflammation in cerebrovascular diseases
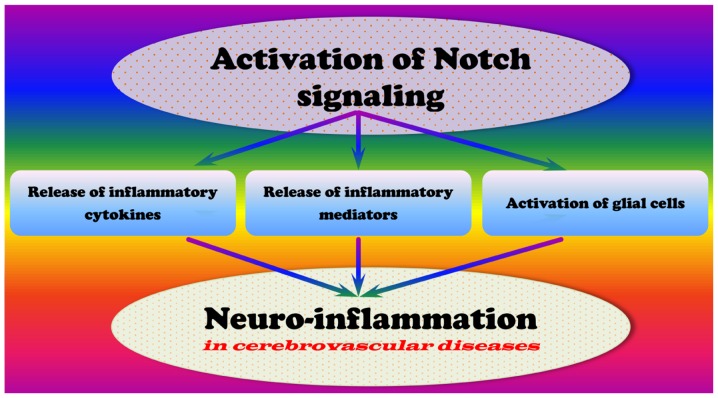
Inflammation is a complex cascade that protects the body from infection and injury. Similarly, neuroinflammation is a response to neurological damage and may be divided into acute and chronic process. A variety of inflammatory cytokines take part in the neuroinflammation. Evidence indicates that acute neuroinflammation is benefcial to damage repair in the nervous system, whereas chronic neuroinflammation aggravates the pathological events occurring in the brain (56–59). In addition, neuroinflammation has been demonstrated to be crucial for the pathogenesis of cerebrovascular diseases (56). Various studies have revealed that the activation of Notch signaling promotes the neuroinflammatory response associated with cerebrovascular diseases (Fig. 1) (18,22,60).
Figure 1.
Potential underlying mechanisms by which the activation of Notch signaling may contribute to the pathogenesis of neuroinflammation in cerebrovascular diseases.
Notch signaling and cytokines
Previous studies have demonstrated that cerebral ischemia initiates an inflammatory response in the brain associated with the release of a variety of inflammatory cytokines, including tumor necrosis factor-α (TNF-α), interleukin (IL)-1β, and IL-6 (55,61,62). Macrophages treated with Toll-like receptor (TLR) 3 or −4 agonists increase their production of interferon (IFN)-β, TNF-α, IL-12 and IL-23. Activation of glial cells and their release of neurotoxic factors enhance inflammation in cerebrovascular disease. In addition, activated glial cells increase the expression of inflammatory cytokines in cerebral ischemia, including TNF-α, IL -1β, IL-6, transforming growth factor β (TGF-β) and IL-8.
Notch signaling is evolutionarily conserved and critical for the development and homeostasis of various tissues. Activation of Notch signaling promotes macrophage polarization to the IFN-γ-producing M1 (inflammatory) subtype (63). Inhibition of Notch signaling by γ-secretase inhibitors (GSI) reduces nuclear factor-κB (NF-κB) activity and suppresses inflammatory responses. Previous studies have demonstrated that GSI significantly decreases peptidoglycan and poly (I:C)-induced secretion of M1 (TNF-α, IL-6, IFN-γ and IL-1α) and the anti-inflammatory subtype M2 (IL-10) cytokines (63,64). Notch signaling is activated in response to TLR ligands, thus amplifying the inflammatory response by enhancing NF-κB signaling. Activation of Notch signaling has been revealed to be involved in the sustained activation of NF-κB and the resulting enhancement of inflammatory responses (65). It is becoming apparent that Notch signaling is central to chronic inflammatory events involved in the pathogenesis of cerebrovascular diseases, and Notch may therefore provide a novel target for therapeutic strategies (15,16,18–20,22,63,65). An ischemic stroke rat model induced by a 90-min occlusion of the right middle cerebral artery demonstrated that inhibiting Notch activation with N-[N-(3,5-Difluorophenacetyl)-L-alanyl]-S-phenylglycine t-butyl ester (DAPT) limited NICD release, and production of IL-6 and IL-1β in the ischemic penumbral cortex (18). Notch mutations may result in a predisposition to stroke and cerebrovascular atherosclerosis, and Notch mutations may also be involved in inflammation process, as genes encoded by Notch mutations include the IL-1 receptor and paraoxonase-1 (66).
Notch signaling and inflammatory mediators
Inflammatory mediators from plasma or cells, exert their effects via binding to specific receptors on target cells. Mediators may have one or numerous target cell types, and may even have varying effects in distinct cell and tissue types. It has been demonstrated that Notch signaling may reprogram mitochondrial metabolism for proinflammatory macrophage activation, inducing the release of inflammatory mediators (67). Nitric oxide (NO), which is produced by cells that express NO synthase (NOS), is a prevalent inflammatory mediator that may inhibit the activity of Notch1 signaling (68,69). A previous study indicates that inducible NOS (iNOS) is directly involved in the generation of NO and the inhibition of Notch1 signaling, and that NO inhibits the binding of Notch1-IC and CSL protein transcriptional complexes to a specific target sequence (69). The dysfunction of Notch signaling pathway increases the vulnerability of neurons and interacts with NF-κB to enhance the inflammatory response following cerebral ischemia (70,71). Numerous signaling pathways involved in neurodegenerative disorders are activated in response to reactive oxygen species (ROS), which induce apoptosis and increase NICD release and the expression of hairy and enhancer of split-1 (HES-1) in cerebral ischemia (71–73). The potential role of Notch signaling in stroke via inflammatory mediators is summarized in Table I.
Table I.
Potential role of Notch signaling in stroke via inflammatory mediators.
| Mediator | Source | Potential role in stroke | References |
|---|---|---|---|
| Histamine and serotonin | Mast cells, platelets | Enhancing vascular leakage, regulating cell proliferation and differentiation | 74–76 |
| Bradykinin | Plasma substrate | Enhancing vascular leakage and pain | 77 |
| C3a | Plasma protein via liver | Enhancing vascular leakage and the formation of opsonic fragment (C3b) | 78 |
| C5a | Macrophages | Enhancing vascular leakage, chemotaxis and leukocyte adhesion and activation | 79 |
| Prostaglandins | Mast cells from membrane phospholipids | Potentiating other mediators, vasodilation, pain and fever | 80,81 |
| Leukotriene B4 | Leukocytes | Leukocyte adhesion and activation | 82 |
| Oxygen metabolites | Leukocytes | Endothelial damage and tissue damage | 22,83–85 |
| IL-1 and TNF-α | Macrophages, other | Acute phase reactions, enhancing vascular leakage and endothelial and tissue damage | 18,65,68, 86–89 |
| Chemokines | Leukocytes, others | Leukocyte activation, enhancing vascular leakage and endothelial and tissue damage | 90–92 |
| Nitric oxide | Macrophages, endothelium | Vasodilation and cytotoxicity | 71 |
C, complement component; IL-1, interleukin-1; TNF-α, tumor necrosis factor α.
Notch signaling and glial cells (microglia and astrocytes)
Microglia are mononuclear phagocytes with various functions in the CNS, with the stage and function of microglia indicated by morphological characteristics. The phagocytic function of microglia is critical for the removal of hematoma and other debris; however, they additionally produce inflammatory mediators (93). Microglia are typically classified into three forms: Ameboid, ramified and activated. Microglia, as the resident immune cells of the CNS, continually sample the environment. Under normal conditions, they exist in a ramified form and phagocytose debris (94). Previous studies indicate that Notch signaling may regulate the different forms of microglia under different conditions (71,95–97). Notch signaling damages neurons by activating microglial cells and stimulating the infiltration of proinflammatory leukocytes (98). Following stroke, microglia are activated, become amoeboid and release inflammatory cytokines (M1 subtype). However, microglia may be differentially activated, subsequently limiting inflammation and destroy tissue debris through phagocytosis (M2 subtype) (63,99). Microglia secrete various inflammatory molecules, including IL-1, IL-6, IFN-γ and TNF-α (22). Furthermore, Notch signaling may be involved in regulating microglia activation following hypoxia, partially via the TLR4/Myeloid differentiation primary response gene 88/TNF receptor associated factor 6/NF-κB signaling pathway (71,100). A model of focal ischemic stroke using mice transgenic for antisense Notch or wild-type mice treated with GSI demonstrated that inhibiting Notch activation reduced brain cell damage and improved functional outcome. This suggests that Notch activation exacerbates brain damage and functional outcome in ischemic stroke (98). Therefore, Notch signaling may be a potential target for inhibition of microglia activation implicated in brain damage (101).
Notch signaling and neuroinflammation in cerebrovascular diseases
Various studies have indicated that Notch activation induces NF-κB-mediated expression of proinflammatory genes in hypoxic astrocytes (102). Notch signaling regulates the activation state of microglia, thus contributing to the control of inflammatory reactions in the CNS (18,96). Notch-1 signaling is activated in hypoxic astrocytes, verified by increased NICD and HES-1, regulating astrocytic proliferation and activation via the suppression of the vascular endothelial growth factor (VEGF) or NF-κB signaling pathways. Dysregulation of Notch may exert effects following stroke via the activation of microglia and astrocytes (63,72,87,103). NF-κB is crucial in promoting ischemic brain damage following stroke. Activation of NF-κB induces the expression of proinflammatory cytokines, the adhesion and migration of leukocytes, thus increasing the inflammatory response (102). The Notch1 signaling pathway regulates the NF-κB signaling pathway via Jagged1 and inhibitor of κB α (IκBα). The dysfunction of the Notch signaling pathway occurs with NF-κB following cerebral ischemia via activating microglia to produce inflammatory mediators (71,101,104). In addition, Notch activation enhances postischemic inflammation by directly modulating the microglial innate response (22,104). In rats with cerebral ischemia and in activated BV-2 microglia, Notch signaling induces the migration and morphological transformation of activated microglia (16). An ischemic rat model using middle-cerebral-artery occlusion demonstrated that Notch-Jagged signaling is involved in dysfunction of astrocyte-associated capillary network (103).
4. Notch signaling and oxidative stress in cerebrovascular diseases
Oxidative stress is broadly defined as a disturbance in the balance between ROS production and antioxidant defenses (105–107). In this state, abnormal levels of ROS, including free radicals (hydroxyl, nitric acid and superoxide) and non-radicals (hydrogen peroxide and lipid peroxide) result in oxidative damage to cells or tissue (105,108–111). The oxidation state is the sum of all redox processes producing ROS, reactive nitrogen species and other reactive intermediates (106,108,112–114). ROS are crucial for physiological processes, including apoptosis, regulation of neurotransmitters and chemotaxis (114–116). ROS may destroy cell function and promote injury to cellular lipids, nucleic acids and proteins, thus inducing apoptosis. Oxidative stress is associated with the pathological process of atherosclerosis, diabetes, neurodegenerative disorders including Alzheimer's disease and Parkinson's disease (117,118), hypertension (119,120), cardiovascular diseases (121) and cerebrovascular diseases (122,123). These diseases may promote the production of ROS (105,107).
Oxidative stress and cerebrovascular diseases
Oxidative stress is involved in the pathogenesis of ischemic and hemorrhagic stroke (124–130) and appears to be a typical feature in diverse models of cerebrovascular disease. Additionally, oxidative stress may be involved in the pathogenesis of acute ischemic stroke (131–136). Oxidative stress regulates cerebral blood flow and controls permeability of the BBB (115,137). A high quantities of superoxide, NO and peroxides are generated during cerebral ischemia/reperfusion, and cellular macromolecules are destroyed by oxygen radicals, resulting in apoptosis (138–142). Oxygen radicals activate matrix metalloproteinases, resulting in the degradation of collagen and laminin proteins in the basilar membrane, and destroying the integrity of the vessel wall (143). In addition, ROS may induce cell death through oxidative modification and fragmentation of DNA mediated by nucleate endonuclease (144–146). Furthermore, oxidative stress promotes transmigration of neutrophilic granulocytes from peripheral blood to the CNS and the release of enzymes that degrade the blood vessel basement membrane, resulting in increased permeability of blood vessels (147–149). Oxidative stress may result in the dysregulation of endothelial cell function, caused by hyperglycemia, dyslipidemia and hyperinsulinemia, leading to impaired vasoregulation, inflammation and altered BBB function (150–152). The described pathological processes result in cerebral parenchymal hemorrhage, vasogenic brain edema and neutrophil infiltration, thus, aggravating cerebral ischemic injury (142,153,154).
Notch signaling and oxidative stress in cerebrovascular diseases
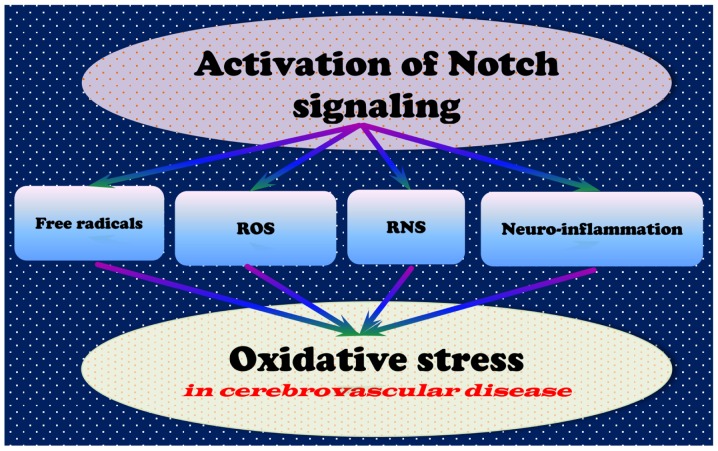
Studies have revealed that oxidative stress may activate multiple signaling pathways associated with cell death; the Notch signaling pathway is closely associated with oxidative stress following cerebral ischemia, suggesting that dysregulation of Notch signaling contributes to the occurrence of oxidative stress (Fig. 2) (155–158). Notch activation results in cell proliferation and metastasis, accompanied by a decrease in B-cell lymphoma-2 (Bcl-2) associated protein X (Bax), Bcl-2 antagonist/killer, cytochrome c and caspase-3 and p53 expression and an increase in Bcl-2 expression (159). It has been reported that inhibiting Notch signaling abrogated cerebral ischemia/reperfusion injury via inhibiting oxidative stress (68,160,161). Inhibiting the Notch signaling pathway attenuates endothelial oxidative stress injury (158), suggesting that Notch inhibition protects against cerebrovascular diseases via decreasing oxidative stress-induced endothelial injury (158). A mutation in Notch3 has been associated with mitochondrial disease, in which oxidative stress caused by chronic hypoxia results in cerebral arteriopathy (162).
Figure 2.
Potential underlying mechanisms by which activation of Notch signaling may contribute to the pathogenesis of oxidative stress in cerebrovascular diseases. ROS, reactive oxygen species; RNS, reactive nitrogen species.
Ischemia/reperfusion injury increases the oxidative stress levels in tissue. The role of the Notch signaling pathway in the oxidative stress-associated pathogenesis of cerebrovascular diseases has been researched extensively (163). Further investigations to elucidate the underlying molecular mechanisms of the Notch signaling pathway in cerebrovascular disease may uncover potential drug targets for the treatment of Notch-associated diseases. However, decreasing the activity of Notch1 increases the production of superoxide anion, iNOS, NO, nitrotyrosine and phosphatase and tensin homolog deleted on chromosome 10 in mice subjected to ischemia/reperfusion injury, whereas the phosphorylation levels of NOS and protein kinase B (Akt) are decreased (68,163,164). As the inhibition or activation of Notch signaling may be beneficial for the treatment of cerebrovascular diseases, Notch signaling may exert distinct functions under different conditions. Therefore, further studies are required to elucidate the mechanisms underlying the role of Notch signaling in cerebrovascular diseases.
5. Notch signaling and apoptosis in cerebrovascular diseases
Programmed cell death by apoptosis is crucial for the development of multicellular organisms, and defects in apop-tosis are associated with a wide variety of diseases (165). Inappropriate apoptosis results in tissue atrophy, whereas a failure of apoptosis, as occurs in cancer, leads to uncontrolled cell proliferation. Certain factors, including Fas receptors and caspases, induce apoptosis, whereas others, including certain Bcl-2 family members, suppress it (166). Apoptosis is induced by either the extrinsic or intrinsic pathways (167,168). Extrinsic stimuli include the binding of ligands to cell surface death receptors, hormones, TNF-α, growth factors, NO and cytokines (169–171). Intrinsic signals result from cellular stress, including heat, radiation, nutrient deprivation and viral infection. The expression of pro- and anti-apoptotic proteins, the strength of the stimulus and the cell cycle stage all alter the response of the cell to the extrinsic or intrinsic trigger (172,173).
Apoptosis and cerebrovascular diseases
In vivo and in vitro studies suggest that apoptosis is critical for the pathogenesis of cerebrovascular diseases (174–179). Increased expression of apoptotic proteins, including phosphorylated (p)-Arabidopsis serine/threonine kinase 1 (ASK1), p-c-Jun N-terminal kinase (JNK), p-p38, cleaved caspase-3 and cytochrome c in the ischemic penumbra has been observed following stroke (177). Studies have reported that the inhibition of apoptosis may prevent the development of cerebral ischemia/reperfusion injury (166,180–185). Thioredoxin-1 (Trx1) small interfering RNA increases ASK1 activation in response to apoptotic stress, Trx1 may therefore be anti-apoptotic and suppress cerebral ischemia/reperfusion injury (186–188), potentially via inhibition of the ASK1-JNK/p38 signaling pathway.
Notch signaling and apoptosis
Notch is involved in various physiological processes, via NICD translocation into the nucleus and binding to target genes (189–191), including apoptosis (172). During apoptosis of tumor cells, microRNA (miR)-100 was demonstrated to mediate Notch signaling (192). A previous study demonstrated that a Notch cis-regulatory element is responsive to loss and gain of Drosophila p53 (Dp53) function and that overexpression of Dp53 upregulates Notch mRNA and protein expression levels (165). Dp53-induced Notch activation and proliferation was revealed to occur even when apoptosis was inhibited, and Dp53 may have a dual role in regulating cell death and proliferation gene networks, to control the balance between apoptosis and proliferation (165). In addition, Notch may be important in the apoptosis- and drug-resistance of chronic lymphocytic leukemia cells. Notch signaling has a cardioprotective effect by regulating apoptosis via inhibiting Bcl-2 and the activation of caspase-3 and -9. Furthermore, the Notch signaling pathway mediates high-glucose-induced podocyte apoptosis via the Bcl-2 and p53 pathways (193–195). It has been reported that miR-34c overexpression increases the expression of anti-apoptotic Bcl-2, and decreases the expression of pro-apoptotic Bax and cleaved caspase-3 via targeting of Notch1 and Jaggged1 (193).
Notch signaling and apoptosis in cerebrovascular diseases
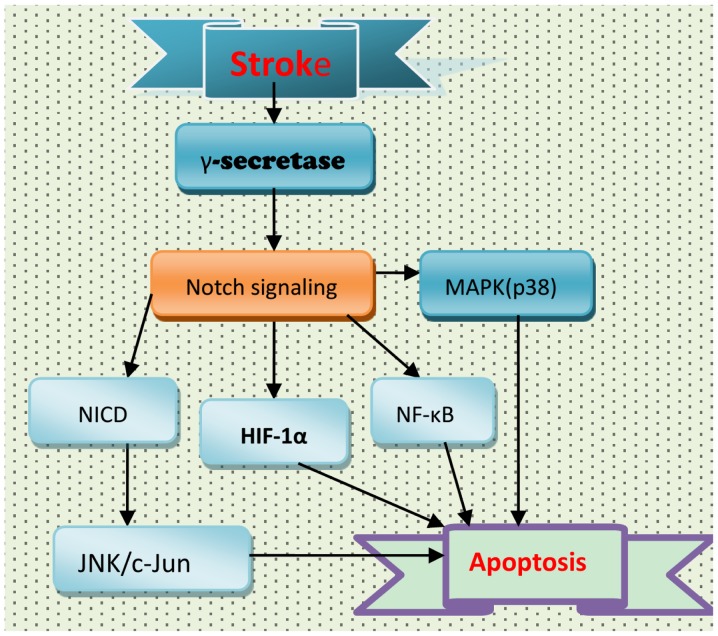
The Notch signaling pathway leads to apoptosis of nerve cells and glia. Cell death in the brain following stroke is the result of an alteration in the balance between pro- and anti-apoptotic factors (196). Neurons undergo apoptosis and necrosis. The Notch signaling pathway is activated by various brain insults, including cerebrovascular diseases (20,47,197), and is associated with the apoptosis involved in the pathogenesis of stroke (Fig. 3). Following stroke, activation of the Notch signaling pathway may result in apoptosis of neurons via NF-κB and hypoxia inducible factor-1α (HIF-1α) (20,197,198). In addition, Notch signaling may affect mitogen-activated protein kinase (MAPK)-associated signaling pathways. However, the role of Notch signaling in MAPK activation following stroke remains to be fully elucidated. In wild-type and NICD1-overexpressing HEK and SH-SY5Y cell lines, ischemic conditions increased the expression levels of NICD1, JNK, p38-MAPK and cleaved caspase-3; this increase in NICD1 and JNK was attenuated by GSI (198). NICD overexpression increased JNK expression levels, resulting in enhanced cell death. Therefore, the Notch signaling pathway may contribute to ischemic stroke via the JNK signaling pathway (198), and the use of GSIs may be a potential strategy for the treatment of ischemic stroke.
Figure 3.
Potential association between apoptosis and Notch signaling following stroke. MAPK, mitogen-activated protein kinase; NICD, Notch intracellular domain; HIF-1α, hypoxia inducible factor-1α; JNK, c-Jun N-terminal kinase; NF-κB, nuclear factor-κB.
Neuronal cell apoptosis associated with Notch signaling occurs in ischemic penumbra and ischemia/reperfusion injury following ischemic cerebrovascular disease (85,199–201). Notch signaling may contribute to apoptosis via the NF-κB, Bcl-like protein 11 and caspase pathways (202). Calsenilin, the expression of which is increased in the brain following experimental ischemic stroke, was revealed to enhance the γ-secretase-mediated cleavage of Notch and to contribute to apoptosis (203). Peptidyl-prolyl cis-trans isomerase NIMA-interacting 1 (Pin1) contributes to the pathogenesis of ischemic stroke by promoting Notch signaling in vitro and in a mouse stroke model, suggesting that Notch signaling activation is involved in the pathogenesis of stroke, and that inhibition of Pin1 may be a novel strategy for the treatment of ischemic stroke (204). However, Notch1 may inhibit neuronal apoptosis in cerebral ischemia/reperfusion injury via increasing the phosphorylation of Akt and promoting inactivation of Bcl-2-associated death promoter. Notch1 may be neuroprotective in the immature brain against ischemic injury, and future studies and clinical trials are required to investigate the suitability of Notch1 inhibitors as a treatment for perinatal ischemia. Inhibiting Notch2 was demonstrated to alter the levels of apoptosis-regulating proteins and slow the process of apoptosis in cerebral ischemia/reperfusion-induced mice (199). Loss-of-function mutations in Notch3 have been identified as the underlying cause of CADASIL (205,206), in addition to complex regulation of multiple pathways, including the Wnt/β-catenin signaling pathway, TGF-β and Notch-induced apoptosis (207).
In summary, the role of Notch signaling in stroke remains controversial. The majority of studies suggest that Notch signaling activation is damaging following stroke, promoting inflammation and apoptosis (20,83,98,202,206,208). However, certain studies have indicated that enhancing Notch signaling may improve stroke pathology (209–211). The effect of Notch on apoptosis is summarized in Table II. Therefore, further studies are required to fully elucidate the role of Notch signaling in stroke.
Table II.
Associations between apoptosis biomarkers and Notch signaling.
| Apoptosis biomarker | Notch | Effect on apoptosis | References |
|---|---|---|---|
| p53 | Notch (↑) | Inhibiting | 195,212,213 |
| Bcl-2 | Notch1, Notch2 (↓) | Anti-apoptosis | 195,202,214 |
| Bax (↑) | Notch 1 (↑) | Apoptosis (↑) | 215 |
| Caspase-9 and -3 (↑) | Notch (↓) | Initiating | 216,217 |
| JNK/p38 | Notch (↑) | Apoptosis (↑) | 198,218 |
| Ca2+ (↑) | Notch 2 (↑) | Apoptosis (↑) | 219,220 |
| ERK | Notch (↑) | Apoptosis (↑) | 221 |
| miR-100 (HS3ST2↑) | Notch (↑) | Initiating | 192,222 |
| NF-κB | NICD (↑) | Apoptosis (↑) | 188 |
| EGFR | Notch-1 | Positive correlation | 223,224 |
| Jagged2, angiopoietin 1, eNOS (↓) | Notch2, Notch4, Notch3 (jagged1) | Caspase 8 (↑) | 225 |
| P21/cyclin D | Notch 2 (↑) | Apoptosis (↑) | 226 |
| PI3K/Akt (↑) | Notch (↓) | Podocyte apoptosis (↓) | 193,194,226,227 |
| ROS | Notch (↑) | Apoptosis (↑) | 228–230 |
| GSIs | Notch (↓) | TRAIL (↑) | 231,232 |
Bcl-2, B-cell lymphoma-2; Bax, Bcl-2 associated X protein; EGFR, epidermal growth factor receptor; eNOS, endothelial nitric oxide synthase; ERK, extracellular signal-regulated kinase; miR, microRNA; GSI, γ-secretase inhibitor; ROS, reactive oxygen species; PI3K, phosphatidylinositol 3-kinase; Akt, protein kinase B; TRAIL, tumor necrosis factor-related apoptosis-inducing ligand.
6. Notch signaling and angiogenesis in cerebrovascular diseases
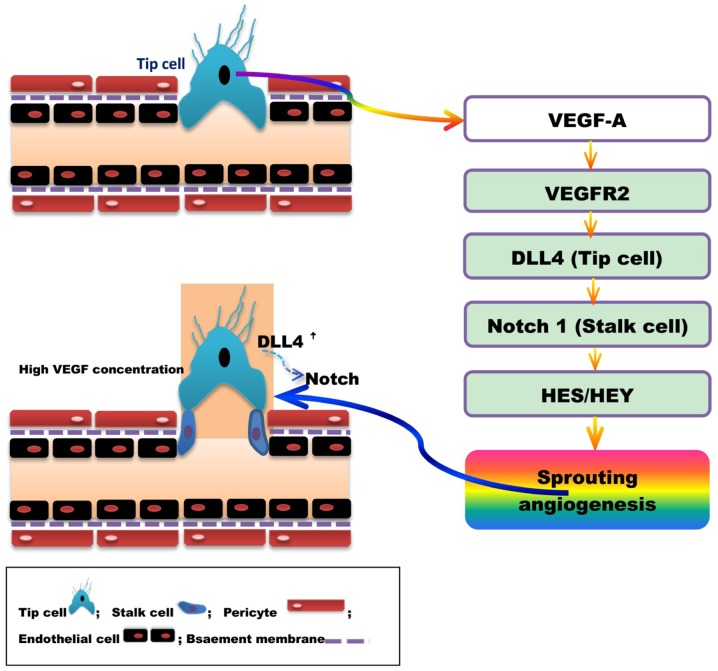
Angiogenesis is a pathophysiological process of vessel branching to form a new capillary network via vascular endothelial cell proliferation and migration, and the sprouting and division of blood vessels (233–236). The vasculature is primarily comprised of vascular endothelial cells, VSMCs and extracellular matrix, the structure and activity of which affect the morphology and function of blood vessels. Angiogenesis is the result of the interaction between endothelial cells, stromal cells and cytokines mediated by a variety of positive and negative angiogenic modulators. Studies have revealed that VEGF/VEGF receptor (VEGFR) (237), Delta-like ligand 4 (DLL4)/Notch are the two primary pathways involved in the promotion and coordination of angiogenesis (Fig. 4) (238,239).
Figure 4.
VEGF and DLL/Notch regulation of angiogenesis. VEGF, vascular endothelial growth factor; VEGFR, vascular endothelial growth factor receptor; DLL4, Delta-like ligand 4; HES, hairy and enhancer of split; HEY, hairy and enhancer of split-related protein.
Lumen formation is required to establish mature blood vessels with complete structure and function. Vascular endothelial cells are divided into acute (tip cell) and lotus cells (trunk cell) depending on their location and characteristics, and are involved in the formation of lumen. High concentrations of VEGF-A induce endothelial cells to differentiate into tip cells. Tip cells extend flopodia through the extracellular matrix, along the VEGF-A gradient, providing direction to the new blood vessel branch. The proliferation of trunk cells behind the tip cell induces vascular sprouting, and the formation of the lumen and extended vascular network. High levels of VEGF induce the synthesis of DLL4 by tip cells, and thus increase Notchl expression in the adjacent trunk cells. The activation of the DLL4/Notchl signaling pathway promotes lumen formation (240,241). DLL4 expression in mouse tip cells was reduced and angiogenesis attenuated following treatment with VEGF antagonists or gene silencing (242,243). Studies have indicated that DLL4/Notch regulate tip and trunk cell number and differentiation, to control blood vessels sprouting and branching. Vascular sprouting and branching proceeds following Notch inhibition, however, these new blood vessels are dysfunctional (243,244).
Angiogenesis is a complex process regulated by numerous factors. The most well-known of these regulators is VEGF, which increases vascular permeability, promotes degradation of the extracellular matrix and migration and proliferation of vascular endothelial cells to induce angiogenesis. The expression of VEGF is controlled by multiple factors, including fibroblast growth factor, angiopoietins/Tie receptors, platelet-derived growth factor, TGF-β, hepatocyte growth factor, HIF-1α, forkhead box (Fox) c1/Foxc2, TNF-α, epidermal growth factor and matrix metalloproteinases (Table III).
Table III.
Factors regulating VEGF expression.
| Regulator | Mechanisms | References |
|---|---|---|
| Ang-1,2,3 | Controls growth, maturation and stability of blood vessels; Ang-2, destabilizes. | 245 |
| FGFa/b | Promotes EC proliferation and migration; induces vascular branching. | 237 |
| PDGF | Recruits perithelial cells, vascular aging. | 246 |
| TGF-β | Bidirectional regulation: Low concentrations of TGF-β promote blood vessel formation, high concentrations of TGF-β inhibit EC growth, and promote smooth muscle cell differentiation and basement membrane formation. | 247,248 |
| HGF | Promotes EC proliferation, improves VEGF secretion in ECs and induces angiogenesis | 249 |
| HIF-1α | Interacts with NICD to increase the response to hypoxia and upregulates DLL4 | 250 |
| Foxc1/Foxc2 | Activates DLL4 expression | 251 |
| Angiopoietins/Tie | Increases expression of Ang-2/1 | 252,253 |
VEGF, vascular endothelial growth factor; Ang, angiopoietin; FGF, fibroblast growth factor; PDGF, platelet-derived growth factor; TGF-β, transforming growth factor β; HGF, hepatocyte growth factor; HIF-1α, hypoxia-inducible factor 1α; Fox, forkhead box; EC, endothelial cell; NICD, Notch intracellular domain; DLL4, Delta-like ligand 4.
VEGF, a growth factor expressed in vascular endothelial and other cells, acts directly on vascular endothelial cells to promote mitosis, induce proliferation and migration, maintain the integrity vessels and increase vascular permeability, and is thus critical for angiogenesis. VEGF-A is the most well-characterized of the VEGF family, and its receptor VEGFR2 is the primary receptor involved in angiogenesis (237). The mammalian Notch signaling pathway, comprised of four homologous Notch receptors (Notchl, Notch2, Notch3 and Notch4) and five cognate ligands (DLL1, DLL3, DLL4, Jaggedl and Jagged2) (254–256), is important for angiogenesis. High concentrations of VEGF induce DLL4 expression, thus, increasing Notchl expression on neighboring cells. The activation of DLL4-Notchl signaling pathways promotes angiogenesis (47,257,258). Studies have revealed that DLL4/Notch signaling mediates negative feedback; the expression of DLL4 may suppress the proliferation and migration of endothelial cells through the inhibition of VEGFR2 by HES-related protein 1 (259,260). VEGF, as a positive regulator of angiogenesis, initiates and promotes angiogenesis, whereas Notch signaling may negatively regulate the process to prevent endothelial cell hyperplasia and, in conjunction with VEGF, promote the formation of a well-differentiated vascular network (261–266).
Injection or nasal feeding of rats with human recombinant VEGF following focal cerebral ischemia in the middle cerebral artery promoted neovascularization of the ischemic area and the recovery of neurological function (267,268). In addition, delayed treatment with VEGF alleviates brain injury, enhances endothelial cell proliferation and augments total vascular volume following neonatal stroke (269). Furthermore, the overexpression of VEGF in close proximity to intracere-bral hemorrhage lesions in mice undergoing transplantation of F3 human neural stem cells (NSCs) facilitated differentiation and survival of the grafted human NSCs, and resulted in renewed angiogenesis in the host brain and functional recovery of mice (270). Studies have revealed that strategies to enhance angiogenesis following focal cerebral ischemia may improve recovery from stroke (271–274). The VEGF/Notch signaling pathway is the primary signaling pathway regulating angiogenesis following cerebral ischemia (47,275,276). VEGF and Notch are upregulated in brain tissue following cerebral ischemia, which may significantly promote angiogenesis in the ischemic region (277–280). Therefore, regulating the Notch signaling pathway may provide a potential strategy for the treatment of cerebrovascular diseases (281).
7. Notch signaling and BBB in cerebrovascular diseases
The BBB is a highly selective permeable barrier separating circulating blood from the brain extracellular fluid, to regulate the CNS microenvironment. The BBB is formed of a complex network of endothelial cells, astroglia, pericytes, perivascular macrophages and a basal membrane. Under physiological conditions, BBB integrity is primarily maintained by endothelial cells, through tight junctions, and the basal lamina; however, the structural and functional integrity of the BBB is markedly altered during CNS disorders, including neoplasia, ischemia, trauma, inflammation and bacterial and viral infections.
Cerebrovascular BBB dysfunction is closely associated with stroke, including intracranial hemorrhage and brain ischemia disorders. Endothelial cells are critical for numerous neurovascular functions, including angiogenesis, BBB formation and maintenance, vascular stability and removal of cellular toxins. Cerebrovascular endothelial cells interact with pericytes to maintain a stable cerebral circulation in the CNS. A number of studies have revealed that endothelial cell dysfunction in the CNS results in breakdown of the BBB and brain hypoperfusion, leading to neurodegeneration. It has been reported that disruption of Smad4 signaling, the central intracellular mediator of TGF-β signaling (14), in endothelial cells leads to the pathogenesis of intracranial hemorrhage and BBB breakdown (14,282), indicating that Smad4 maintains cerebrovascular integrity and that TGF-β/Smad signaling is involved in the pathogenesis of cerebrovascular dysfunction. Notch signaling is also critical in controlling BBB integrity via regulating the normal function of endothelial cells and pericytes. However, the underlying mechanisms regulating cerebral endothelial cell functions remain to be elucidated.
The Notch signaling pathway is involved in blood vessel integrity and BBB stability and function in the mammalian vasculature (75,283–285). In vitro studies have correlated BBB endothelial dysfunction with decreased Notch4 expression (286). Upon activation, the constitutively expressed endothelial cell membrane protein Notch4 appears to become primarily involved in the stability and growth of mature endothelium (287). Permanent ischemia leads to the redistribution of claudin decomposition fragments, zona occludens 1 and occludin protein from the membrane to the cytoplasm in BBB. Additionally, the GSI, DAPT protects against permanent ischemia-induced BBB damage, potentially via the modulation of Notch/NICD/calpastatin homeostasis pathway in vascular endothelial cells.
8. Conclusion and perspective
Increasing evidence indicates that Notch signaling is critical in the pathogenesis of stroke, exerting effects via the following underlying mechanisms: Neuroinfammation, oxidative stress, apoptosis, angiogenesis and BBB function. Thus, regulating Notch signaling may be an effective strategy for the prevention and treatment of cerebrovascular diseases.
Studies have demonstrated that the activation of Notch signaling is harmful and contributes to the pathogenesis of cerebrovascular diseases including stroke (20,98,202,204,288–290). Acute inhibition of Notch signaling has been revealed to rescue cerebral hypoperfusion, reduce apoptosis in penumbra, decrease brain infarct size, elicit certain morphologic features, including neurogenesis and angiogenesis, associated with brain repair and functional recovery, and enhance vascular densities in penumbra in the neonatal rat brain following stroke (288).
However, activation of the Notch signaling pathway may have a neuroprotective role via enhancing endogenous neuroregeneration and brain arteriogenesis following stroke (51,291). In a murine transient global cerebral ischemia/reperfusion model, the neuroprotective effects of preconditioning were mediated via the Notch signaling pathway, and the expression of Notch1, NICD and HES-1 was upregulated (209). Notch signaling is widely accepted to be a fundamental pathway controlling cell fate acquisition through the regulation of adult neurogenesis. Studies have demonstrated that Notch signaling is crucial for the maintenance, proliferation and differentiation of NSCs in the developing brain (292,293). Notch signaling induces the neuronal expansion and differentiation following stroke (21). Increasing the expression level of Notch signaling components may facilitate intrastriatal transplantation therapy for ischemic stroke by promoting endogenous regeneration in the hippocampus (294). Promoting Notch signaling activity may facilitate increased arteriogenesis in a middle cerebral artery occlusion stroke rat model (54). In addition, Notch-induced rat and human bone marrow stromal cell grafts inhibited ischemic cell loss and abrogated behavioral deficits in chronic middle cerebral artery occlusion stroke rats (295).
Therefore, the results on the effect of Notch signaling on the pathogenesis of cerebrovascular diseases are contradictory. Notch signaling may be damaging, as it promotes inflammation, oxidative stress and apoptosis. However, the activation of the Notch signaling pathway may exert neuroprotective effects via enhancing endogenous neuroregeneration and brain arteriogenesis following stroke. What is the exact role of Notch signaling? Clarifying this question has potentially important implications for the treatment of cerebrovascular disease, and will provide novel strategies for future studies.
Acknowledgments
The present study was supported by grants from the Natural Science Foundation of Hubei Province (grant no. 2015CFB260), the Hubei Province Health and Family Planning Scientific Research Project (grant no. WJ2015MB219) the Shiyan Natural Science Foundation (grant no. 15K70) and the Renmin Hospital Natural Science Foundation (grant no. 2015CZY), to Dr Zhiyou Cai.
References
- 1.Lama S, Dolati P, Sutherland GR. Controversy in the management of lenticulostriate artery dissecting aneurysm: A case report and review of the literature. World Neurosurg. 2014;81:441.e1–e7. doi: 10.1016/j.wneu.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 2.Dezmalj-Grbelja L, Bosnjak J, Lovrencić-Huzjan A, Ivica M, Demarin V. Moyamoya disease in a patient with brain tumor: Case report. Acta Clin Croat. 2010;49:459–463. [PubMed] [Google Scholar]
- 3.Sharfstein SR, Ahmed S, Islam MQ, Najjar MI, Ratushny V. Case of moyamoya disease in a patient with advanced acquired immunodeficiency syndrome. J Stroke Cerebrovasc Dis. 2007;16:268–272. doi: 10.1016/j.jstrokecerebrovasdis.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Squizzato A, Gerdes VE, Brandjes DP, Büller HR, Stam J. Thyroid diseases and cerebrovascular disease. Stroke. 2005;36:2302–2310. doi: 10.1161/01.STR.0000181772.78492.07. [DOI] [PubMed] [Google Scholar]
- 5.Vetrano DL, Landi F, De Buyser SL, Carfi A, Zuccalà G, Petrovic M, Volpato S, Cherubini A, Corsonello A, Bernabei R, Onder G. Predictors of length of hospital stay among older adults admitted to acute care wards: A multicentre observational study. Eur J Intern Med. 2014;25:56–62. doi: 10.1016/j.ejim.2013.08.709. [DOI] [PubMed] [Google Scholar]
- 6.Cicconetti P, Riolo N, Priami C, Tafaro L, Ettore E. Risk factors for cognitive impairment. Recenti Prog Med. 2004;95:535–545. In Italian. [PubMed] [Google Scholar]
- 7.Elkind MS. Epidemiology and risk factors. Continuum (Minneap Minn) 2011;17:1213–1232. doi: 10.1212/01.CON.0000410031.34477.8d. [DOI] [PubMed] [Google Scholar]
- 8.Jia Q, Liu LP, Wang YJ. Stroke in China. Clin Exp Pharmacol Physiol. 2010;37:259–264. doi: 10.1111/j.1440-1681.2009.05290.x. [DOI] [PubMed] [Google Scholar]
- 9.Bhoopathi P, Chetty C, Dontula R, Gujrati M, Dinh DH, Rao JS, Lakka SS. SPARC stimulates neuronal differentiation of medulloblastoma cells via the Notch1/STAT3 pathway. Cancer Res. 2011;71:4908–4919. doi: 10.1158/0008-5472.CAN-10-3395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yuan TM, Yu HM. Notch signaling: Key role in intrauterine infection/inflammation, embryonic development, and white matter damage? J Neurosci Res. 2010;88:461–468. doi: 10.1002/jnr.22229. [DOI] [PubMed] [Google Scholar]
- 11.Veenendaal LM, Kranenburg O, Smakman N, Klomp A, Borel Rinkes IH, van Diest PJ. Differential Notch and TGFbeta signaling in primary colorectal tumors and their corresponding metastases. Cell Oncol. 2008;30:1–11. doi: 10.1155/2008/839076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Givogri MI, de Planell M, Galbiati F, Superchi D, Gritti A, Vescovi A, de Vellis J, Bongarzone ER. Notch signaling in astrocytes and neuroblasts of the adult subventricular zone in health and after cortical injury. Dev Neurosci. 2006;28:81–91. doi: 10.1159/000090755. [DOI] [PubMed] [Google Scholar]
- 13.Quillard T, Charreau B. Impact of notch signaling on inflammatory responses in cardiovascular disorders. Int J Mol Sci. 2013;14:6863–6888. doi: 10.3390/ijms14046863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li F, Lan Y, Wang Y, Wang J, Yang G, Meng F, Han H, Meng A, Yang X. Endothelial Smad4 maintains cerebrovascular integrity by activating N-cadherin through cooperation with Notch. Dev Cell. 2011;20:291–302. doi: 10.1016/j.devcel.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 15.Dichgans M. Genetics of ischaemic stroke. Lancet Neurol. 2007;6:149–161. doi: 10.1016/S1474-4422(07)70028-5. [DOI] [PubMed] [Google Scholar]
- 16.Yuan Y, Rangarajan P, Kan EM, Wu Y, Wu C, Ling EA. Scutellarin regulates the Notch pathway and affects the migration and morphological transformation of activated microglia in experimentally induced cerebral ischemia in rats and in activated BV-2 microglia. J Neuroinflammation. 2015;12:11. doi: 10.1186/s12974-014-0226-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheng YL, Choi Y, Sobey CG, Arumugam TV, Jo DG. Emerging roles of the γ-secretase-notch axis in inflammation. Pharmacol Ther. 2015;147:80–90. doi: 10.1016/j.pharmthera.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 18.Wang Z, Huang W, Zuo Z. Perioperative aspirin improves neurological outcome after focal brain ischemia possibly via inhibition of Notch 1 in rat. J Neuroinflammation. 2014;11:56. doi: 10.1186/1742-2094-11-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li S, Zyang X, Wang Y, Ji H, Du Y, Liu H. DAPT protects brain against cerebral ischemia by down-regulating the expression of Notch 1 and nuclear factor κB in rats. Neurol Sci. 2012;33:1257–1264. doi: 10.1007/s10072-012-0948-6. [DOI] [PubMed] [Google Scholar]
- 20.Cheng YL, Park JS, Manzanero S, Choi Y, Baik SH, Okun E, Gelderblom M, Fann DY, Magnus T, Launikonis BS, et al. Evidence that collaboration between HIF-1α and Notch-1 promotes neuronal cell death in ischemic stroke. Neurobiol Dis. 2014;62:286–295. doi: 10.1016/j.nbd.2013.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang L, Chopp M, Zhang RL, Zhang L, Letourneau Y, Feng YF, Jiang A, Morris DC, Zhang ZG. The Notch pathway mediates expansion of a progenitor pool and neuronal differentiation in adult neural progenitor cells after stroke. Neuroscience. 2009;158:1356–1363. doi: 10.1016/j.neuroscience.2008.10.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wei Z, Chigurupati S, Arumugam TV, Jo DG, Li H, Chan SL. Notch activation enhances the microglia-mediated inflammatory response associated with focal cerebral ischemia. Stroke. 2011;42:2589–2594. doi: 10.1161/STROKEAHA.111.614834. [DOI] [PubMed] [Google Scholar]
- 23.Morgan TH. The theory of the gene. Am Naturalist. 1917;51:513–544. doi: 10.1086/279629. [DOI] [Google Scholar]
- 24.Becker S, Oelschlaeger TA, Wullaert A, Vlantis K, Pasparakis M, Wehkamp J, Stange EF, Gersemann M. Bacteria regulate intestinal epithelial cell differentiation factors both in vitro and in vivo. PLoS One. 2013;8:e55620. doi: 10.1371/journal.pone.0055620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maier D, Kurth P, Schulz A, Russell A, Yuan Z, Gruber K, Kovall RA, Preiss A. Structural and functional analysis of the repressor complex in the Notch signaling pathway of Drosophila melanogaster. Mol Biol Cell. 2011;22:3242–3252. doi: 10.1091/mbc.E11-05-0420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Braune EB, Lendahl U. Notch-a goldilocks signaling pathway in disease and cancer therapy. Discov Med. 2016;21:189–196. [PubMed] [Google Scholar]
- 27.Del Bianco C, Vedenko A, Choi SH, Berger MF, Shokri L, Bulyk ML, Blacklow SC. Notch and MAML-1 complexation do not detectably alter the DNA binding specificity of the transcription factor CSL. PLoS One. 2010;5:e15034. doi: 10.1371/journal.pone.0015034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Faux CH, Turnley AM, Epa R, Cappai R, Bartlett PF. Interactions between fbroblast growth factors and Notch regulate neuronal differentiation. J Neurosci. 2001;21:5587–5596. doi: 10.1523/JNEUROSCI.21-15-05587.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shimizu K, Chiba S, Kumano K, Hosoya N, Takahashi T, Kanda Y, Hamada Y, Yazaki Y, Hirai H. Mouse jagged1 physically interacts with notch2 and other notch receptors. Assessment by quantitative methods. J Biol Chem. 1999;274:32961–32969. doi: 10.1074/jbc.274.46.32961. [DOI] [PubMed] [Google Scholar]
- 30.Zhang S, Chung WC, Wu G, Egan SE, Xu K. Tumor-suppressive activity of Lunatic Fringe in prostate through differential modulation of Notch receptor activation. Neoplasia. 2014;16:158–167. doi: 10.1593/neo.131870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bresnick EH, Chu J, Christensen HM, Lin B, Norton J. Linking Notch signaling, chromatin remodeling, and T-cell leukemogenesis. J Cell Biochem Suppl. 2000;35(Suppl):S46–S53. doi: 10.1002/1097-4644(2000)79:35+<46::AID-JCB1125>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 32.Nam Y, Weng AP, Aster JC, Blacklow SC. Structural requirements for assembly of the CSL. Intracellular Notch1. Mastermind-like 1 transcriptional activation complex. J Biol Chem. 2003;278:21232–21239. doi: 10.1074/jbc.M301567200. [DOI] [PubMed] [Google Scholar]
- 33.Portin P. General outlines of the molecular genetics of the Notch signalling pathway in Drosophila melanogaster. A review Hereditas. 2002;136:89–96. doi: 10.1034/j.1601-5223.2002.1360201.x. [DOI] [PubMed] [Google Scholar]
- 34.Li Y, Baker NE. Proneural enhancement by Notch overcomes Suppressor-of-Hairless repressor function in the developing Drosophila eye. Curr Biol. 2001;11:330–338. doi: 10.1016/S0960-9822(01)00093-8. [DOI] [PubMed] [Google Scholar]
- 35.Wang J, Ye Z, Zheng S, Chen L, Wan Y, Deng Y, Yang R. Lingo-1 shRNA and Notch signaling inhibitor DAPT promote differentiation of neural stem/progenitor cells into. neurons Brain Res. 2016;1634:34–44. doi: 10.1016/j.brainres.2015.11.029. [DOI] [PubMed] [Google Scholar]
- 36.Cardano M, Diaferia GR, Cattaneo M, Dessí SS, Long Q, Conti L, Deblasio P, Cattaneo E, Biunno I. mSEL-1L (Suppressor/enhancer Lin12-like) protein levels influence murine neural stem cell self-renewal and lineage commitment. J Biol Chem. 2011;286:18708–18719. doi: 10.1074/jbc.M110.210740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berezovska O, Xia MQ, Hyman BT. Notch is expressed in adult brain, is coexpressed with presenilin-1, and is altered in Alzheimer disease. J Neuropathol Exp Neurol. 1998;57:738–745. doi: 10.1097/00005072-199808000-00003. [DOI] [PubMed] [Google Scholar]
- 38.Nagarsheth MH, Viehman A, Lippa SM, Lippa CF. Notch-1 immunoexpression is increased in Alzheimer's and Pick's disease. J Neurol Sci. 2006;244:111–116. doi: 10.1016/j.jns.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 39.Cairney CJ, Sanguinetti G, Ranghini E, Chantry AD, Nostro MC, Bhattacharyya A, Svendsen CN, Keith WN, Bellantuono I. A systems biology approach to Down syndrome: Identification of Notch/Wnt dysregulation in a model of stem cells aging. Biochim Biophys Acta. 2009;1792:353–363. doi: 10.1016/j.bbadis.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 40.Fernandez-Martinez J, Vela EM, Tora-Ponsioen M, Ocaña OH, Nieto MA, Galceran J. Attenuation of Notch signalling by the Down-syndrome-associated kinase DYRK1A. J Cell Sci. 2009;122:1574–1583. doi: 10.1242/jcs.044354. [DOI] [PubMed] [Google Scholar]
- 41.García-Estévez DA, Barros-Angueira F, Navarro C. CADASIL: Brief report on a family with a new p.G296C mutation in exon 6 of the Notch-3 gene. Rev Neurol. 2010;51:729–732. In Spanish. [PubMed] [Google Scholar]
- 42.Tang SC, Jeng JS, Lee MJ, Yip PK. Notch signaling and CADASIL. Acta Neurol Taiwan. 2009;18:81–90. [PubMed] [Google Scholar]
- 43.Louvi A, Arboleda-Velasquez JF, Artavanis-Tsakonas S. CADASIL: A critical look at a Notch disease. Dev Neurosci. 2006;28:5–12. doi: 10.1159/000090748. [DOI] [PubMed] [Google Scholar]
- 44.Tan ZX, Li FF, Qu YY, Liu J, Liu GR, Zhou J, Zhu YL, Liu SL. Identification of a known mutation in Notch 3 in familiar CADASIL in China. PLoS One. 2012;7:e36590. doi: 10.1371/journal.pone.0036590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Posada-Duque RA, Barreto GE, Cardona-Gomez GP. Protection after stroke: Cellular effectors of neurovascular unit integrity. Front Cell Neurosci. 2014;8:231. doi: 10.3389/fncel.2014.00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cotena S, Piazza O, Tufano R. The use of erythtropoietin in cerebral diseases. Panminerva Med. 2008;50:185–192. [PubMed] [Google Scholar]
- 47.Lou YL, Guo F, Liu F, Gao FL, Zhang PQ, Niu X, Guo SC, Yin JH, Wang Y, Deng ZF. miR-210 activates notch signaling pathway in angiogenesis induced by cerebral ischemia. Mol Cell Biochem. 2012;370:45–51. doi: 10.1007/s11010-012-1396-6. [DOI] [PubMed] [Google Scholar]
- 48.Corada M, Morini MF, Dejana E. Signaling pathways in the specifcation of arteries and veins. Arterioscler Thromb Vasc Biol. 2014;34:2372–2377. doi: 10.1161/ATVBAHA.114.303218. [DOI] [PubMed] [Google Scholar]
- 49.Grieskamp T, Rudat C, Lüdtke TH, Norden J, Kispert A. Notch signaling regulates smooth muscle differentiation of epicardium-derived cells. Circ Res. 2011;108:813–823. doi: 10.1161/CIRCRESAHA.110.228809. [DOI] [PubMed] [Google Scholar]
- 50.del Monte G, Casanova JC, Guadix JA, MacGrogan D, Burch JB, Pérez-Pomares JM, de la Pompa JL. Differential Notch signaling in the epicardium is required for cardiac inflow development and coronary vessel morphogenesis. Circ Res. 2011;108:824–836. doi: 10.1161/CIRCRESAHA.110.229062. [DOI] [PubMed] [Google Scholar]
- 51.Proweller A, Wright AC, Horng D, Cheng L, Lu MM, Lepore JJ, Pear WS, Parmacek MS. Notch signaling in vascular smooth muscle cells is required to pattern the cerebral vasculature. Proc Natl Acad Sci USA. 2007;104:16275–16280. doi: 10.1073/pnas.0707950104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Koga J, Nakano T, Dahlman JE, Figueiredo JL, Zhang H, Decano J, Khan OF, Niida T, Iwata H, Aster JC, et al. Macrophage Notch Ligand Delta-Like 4 Promotes Vein Graft Lesion Development: Implications for the Treatment of Vein Graft Failure. Arterioscler Thromb Vasc Biol. 2015;35:2343–2353. doi: 10.1161/ATVBAHA.115.305516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Quillien A, Moore JC, Shin M, Siekmann AF, Smith T, Pan L, Moens CB, Parsons MJ, Lawson ND. Distinct Notch signaling outputs pattern the developing arterial system. Development. 2014;141:1544–1552. doi: 10.1242/dev.099986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zacharek A, Chen J, Cui X, Yang Y, Chopp M. Simvastatin increases notch signaling activity and promotes arteriogenesis after stroke. Stroke. 2009;40:254–260. doi: 10.1161/STROKEAHA.108.524116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen J, Cui X, Zacharek A, Ding GL, Shehadah A, Jiang Q, Lu M, Chopp M. Niaspan treatment increases tumor necrosis factor-alpha-converting enzyme and promotes arteriogenesis after stroke. J Cereb Blood Flow Metab. 2009;29:911–920. doi: 10.1038/jcbfm.2009.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Di Napoli M, Shah IM. Neuroinflammation and cerebrovascular disease in old age: A translational medicine perspective. J Aging Res. 2011;2011:857484. doi: 10.4061/2011/857484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Felsky D, De Jager PL, Schneider JA, Arfanakis K, Fleischman DA, Arvanitakis Z, Honer WG, Pouget JG, Mizrahi R, Pollock BG, et al. Cerebrovascular and microglial states are not altered by functional neuroinflammatory gene variant. J Cereb Blood Flow Metab. 2016;36:819–830. doi: 10.1177/0271678X15626719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cacabelos R, Torrellas C, Fernández-Novoa L, Aliev G. Neuroimmune Crosstalk in CNS Disorders: The Histamine Connection. Curr Pharm Des. 2016;22:819–848. doi: 10.2174/1381612822666151209150954. [DOI] [PubMed] [Google Scholar]
- 59.Silva J, Polesskaya O, Knight W, Zheng JT, Granger M, Lopez T, Ontiveros F, Feng C, Yan C, Kasischke KA, Dewhurst S. Transient hypercapnia reveals an underlying cerebrovascular pathology in a murine model for HIV-1 associated neuroinflammation: Role of NO-cGMP signaling and normalization by inhibition of cyclic nucleotide phosphodiesterase-5. J Neuroinflammation. 2012;9:253. doi: 10.1186/1742-2094-9-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Meschia JF, Worrall BB. New advances in identifying genetic anomalies in stroke-prone probands. Curr Atheroscler Rep. 2003;5:317–323. doi: 10.1007/s11883-003-0055-5. [DOI] [PubMed] [Google Scholar]
- 61.Heo R, Park JS, Jang HJ, Kim SH, Shin JM, Suh YD, Jeong JH, Jo DG, Park JH. Hyaluronan nanoparticles bearing γ-secretase inhibitor: In vivo therapeutic effects on rheumatoid arthritis. J Control Release. 2014;192:295–300. doi: 10.1016/j.jconrel.2014.07.057. [DOI] [PubMed] [Google Scholar]
- 62.Lucitti JL, Mackey JK, Morrison JC, Haigh JJ, Adams RH, Faber JE. Formation of the collateral circulation is regulated by vascular endothelial growth factor-A and a disintegrin and metal-loprotease family members 10 and 17. Circ Res. 2012;111:1539–1550. doi: 10.1161/CIRCRESAHA.112.279109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brifault C, Gras M, Liot D, May V, Vaudry D, Wurtz O. Delayed pituitary adenylate cyclase-activating polypeptide delivery after brain stroke improves functional recovery by inducing m2 microglia/macrophage polarization. Stroke. 2015;46:520–528. doi: 10.1161/STROKEAHA.114.006864. [DOI] [PubMed] [Google Scholar]
- 64.Holden JA, Attard TJ, Laughton KM, Mansell A, O'Brien-Simpson NM, Reynolds EC. Porphyromonas gingivalis lipopolysaccharide weakly activates M1 and M2 polarized mouse macrophages but induces inflammatory cytokines. Infect Immun. 2014;82:4190–4203. doi: 10.1128/IAI.02325-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang Y, He K, Wang F, Li X, Liu D. Notch-1 signaling regulates astrocytic proliferation and activation after hypoxia exposure. Neurosci Lett. 2015;603:12–18. doi: 10.1016/j.neulet.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 66.Meschia JF, Worrall BB. New advances in identifying genetic anomalies in stroke-prone probands. Curr Neurol Neurosci Rep. 2004;4:420–426. doi: 10.1007/s11910-004-0090-9. [DOI] [PubMed] [Google Scholar]
- 67.Xu J, Chi F, Guo T, Punj V, Lee WN, French SW, Tsukamoto H. NOTCH reprograms mitochondrial metabolism for proinflammatory macrophage activation. J Clin Invest. 2015;125:1579–1590. doi: 10.1172/JCI76468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pei H, Song X, Peng C, Tan Y, Li Y, Li X, Ma S, Wang Q, Huang R, Yang D, et al. TNF-α inhibitor protects against myocardial ischemia/reperfusion injury via Notch1-mediated suppression of oxidative/nitrative stress. Free Radic Biol Med. 2015;82:114–121. doi: 10.1016/j.freeradbiomed.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 69.Qin WD, Zhang F, Qin XJ, Wang J, Meng X, Wang H, Guo HP, Wu QZ, Wu DW, Zhang MX. Notch1 inhibition reduces low shear stress-induced plaque formation. Int J Biochem Cell Biol. 2016;72:63–72. doi: 10.1016/j.biocel.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 70.Palaga T, Buranaruk C, Rengpipat S, Fauq AH, Golde TE, Kaufmann SH, Osborne BA. Notch signaling is activated by TLR stimulation and regulates macrophage functions. Eur J Immunol. 2008;38:174–183. doi: 10.1002/eji.200636999. [DOI] [PubMed] [Google Scholar]
- 71.Cao Q, Kaur C, Wu CY, Lu J, Ling EA. Nuclear factor-kappa β regulates Notch signaling in production of proinflammatory cytokines and nitric oxide in murine BV-2 microglial cells. Neuroscience. 2011;192:140–154. doi: 10.1016/j.neuroscience.2011.06.060. [DOI] [PubMed] [Google Scholar]
- 72.Fang M, Yuan Y, Rangarajan P, Lu J, Wu Y, Wang H, Wu C, Ling EA. Scutellarin regulates microglia-mediated TNC1 astrocytic reaction and astrogliosis in cerebral ischemia in the adult rats. BMC Neurosci. 2015;16:84. doi: 10.1186/s12868-015-0219-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhou D, Huang C, Lin Z, Zhan S, Kong L, Fang C, Li J. Macrophage polarization and function with emphasis on the evolving roles of coordinated regulation of cellular signaling pathways. Cell Signal. 2014;26:192–197. doi: 10.1016/j.cellsig.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 74.Qiu Y, Du B, Xie F, Cai W, Liu Y, Li Y, Feng L, Qiu L. Vaccarin attenuates high glucose-induced human EA•hy926 endothelial cell injury through inhibition of Notch signaling. Mol Med Rep. 2016;13:2143–2150. doi: 10.3892/mmr.2016.4801. [DOI] [PubMed] [Google Scholar]
- 75.Henshall TL, Keller A, He L, Johansson BR, Wallgard E, Raschperger E, Mäe MA, Jin S, Betsholtz C, Lendahl U. Notch3 is necessary for blood vessel integrity in the central nervous system. Arterioscler Thromb Vasc Biol. 2015;35:409–420. doi: 10.1161/ATVBAHA.114.304849. [DOI] [PubMed] [Google Scholar]
- 76.Yu LM, Chen DX, Zhou QX, Fang N, Liu ZL. Effects of histamine on immunophenotype and notch signaling in human HL-60 leukemia cells. Exp Biol Med (Maywood) 2006;231:1633–1637. doi: 10.1177/153537020623101008. [DOI] [PubMed] [Google Scholar]
- 77.Boulos N, Helle F, Dussaule JC, Placier S, Milliez P, Djudjaj S, Guerrot D, Joutel A, Ronco P, Boffa JJ, Chatziantoniou C. Notch3 is essential for regulation of the renal vascular tone. Hypertension. 2011;57:1176–1182. doi: 10.1161/HYPERTENSIONAHA.111.170746. [DOI] [PubMed] [Google Scholar]
- 78.Fischer AJ, Zelinka C, Gallina D, Scott MA, Todd L. Reactive microglia and macrophage facilitate the formation of Müller glia-derived retinal progenitors. Glia. 2014;62:1608–1628. doi: 10.1002/glia.22703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shipp LE, Hill RZ, Moy GW, Gokirmak T, Hamdoun A. ABCC5 is required for cAMP-mediated hindgut invagination in sea urchin embryos. Development. 2015;142:3537–3548. doi: 10.1242/dev.126144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bartosh TJ, Ylostalo JH, Bazhanov N, Kuhlman J, Prockop DJ. Dynamic compaction of human mesenchymal stem/precursor cells into spheres self-activates caspase-dependent IL1 signaling to enhance secretion of modulators of inflammation and immunity (PGE2, TSG6, and STC1) Stem Cells. 2013;31:2443–2456. doi: 10.1002/stem.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Clement N, Gueguen M, Glorian M, Blaise R, Andréani M, Brou C, Bausero P, Limon I. Notch3 and IL-1beta exert opposing effects on a vascular smooth muscle cell inflammatory pathway in which NF-kappaB drives crosstalk. J Cell Sci. 2007;120:3352–3361. doi: 10.1242/jcs.007872. [DOI] [PubMed] [Google Scholar]
- 82.Ali M, Heyob K, Rogers LK. DHA suppresses primary macrophage inflammatory responses via Notch 1/Jagged 1 signaling. Sci Rep. 2016;6:22276. doi: 10.1038/srep22276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yin J, Li H, Feng C, Zuo Z. Inhibition of brain ischemia-caused notch activation in microglia may contribute to isoflurane postconditioning-induced neuroprotection in male rats. CNS Neurol Disord Drug Targets. 2014;13:718–732. doi: 10.2174/1871527313666140618110837. [DOI] [PubMed] [Google Scholar]
- 84.Liu Q, Fan X, Zhu J, Xu G, Li Y, Liu X. Co-culturing improves the OGD-injured neuron repairing and NSCs differentiation via Notch pathway activation. Neurosci Lett. 2014;559:1–6. doi: 10.1016/j.neulet.2013.11.027. [DOI] [PubMed] [Google Scholar]
- 85.Albéri L, Chi Z, Kadam SD, Mulholland JD, Dawson VL, Gaiano N, Comi AM. Neonatal stroke in mice causes long-term changes in neuronal Notch-2 expression that may contribute to prolonged injury. Stroke. 2010;41(Suppl 10):S64–S71. doi: 10.1161/STROKEAHA.110.595298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lipsey CC, Harbuzariu A, Daley-Brown D, Gonzalez-Perez RR. Oncogenic role of leptin and Notch interleukin-1 leptin crosstalk outcome in cancer. World J Methodol. 2016;6:43–55. doi: 10.5662/wjm.v6.i1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Grill M, Syme TE, Nocon AL, Lu AZ, Hancock D, Rose-John S, Campbell IL. Strawberry notch homolog 2 is a novel inflammatory response factor predominantly but not exclusively expressed by astrocytes in the central nervous system. Glia. 2015;63:1738–1752. doi: 10.1002/glia.22841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wang H, Tian Y, Wang J, Phillips KL, Binch AL, Dunn S, Cross A, Chiverton N, Zheng Z, Shapiro IM, et al. Inflammatory cytokines induce NOTCH signaling in nucleus pulposus cells: Implications in intervertebral disc degeneration. J Biol Chem. 2013;288:16761–16774. doi: 10.1074/jbc.M112.446633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Keuylian Z, de Baaij JH, Gueguen M, Glorian M, Rouxel C, Merlet E, Lipskaia L, Blaise R, Mateo V, Limon I. The Notch pathway attenuates interleukin 1β (IL1β)-mediated induction of adenylyl cyclase 8 (AC8) expression during vascular smooth muscle cell (VSMC) trans-differentiation. J Biol Chem. 2012;287:24978–24989. doi: 10.1074/jbc.M111.292516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mirandola L, Apicella L, Colombo M, Yu Y, Berta DG, Platonova N, Lazzari E, Lancellotti M, Bulfamante G, Cobos E, et al. Anti-Notch treatment prevents multiple myeloma cells localization to the bone marrow via the chemokine system CXCR4/SDF-1. Leukemia. 2013;27:1558–1566. doi: 10.1038/leu.2013.27. [DOI] [PubMed] [Google Scholar]
- 91.Fukuda D, Aikawa E, Swirski FK, Novobrantseva TI, Kotelianski V, Gorgun CZ, Chudnovskiy A, Yamazaki H, Croce K, Weissleder R, et al. Notch ligand delta-like 4 blockade attenuates atherosclerosis and metabolic disorders. Proc Natl Acad Sci USA. 2012;109:E1868–E1877. doi: 10.1073/pnas.1116889109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Al Haj Zen A, Oikawa A, Bazan-Peregrino M, Meloni M, Emanueli C, Madeddu P. Inhibition of delta-like-4-mediated signaling impairs reparative angiogenesis after ischemia. Circ Res. 2010;107:283–293. doi: 10.1161/CIRCRESAHA.110.221663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kumari B, Jain P, Das S, Ghosal S, Hazra B, Trivedi AC, Basu A, Chakrabarti J, Vrati S, Banerjee A. Dynamic changes in global microRNAome and transcriptome reveal complex miRNA-mRNA regulated host response to Japanese Encephalitis Virus in microglial cells. Sci Rep. 2016;6:20263. doi: 10.1038/srep20263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yao L, Cao Q, Wu C, Kaur C, Hao A, Ling EA. Notch signaling in the central nervous system with special reference to its expression in microglia. CNS Neurol Disord Drug Targets. 2013;12:807–814. doi: 10.2174/18715273113126660172. [DOI] [PubMed] [Google Scholar]
- 95.Salta E, Lau P, Sala Frigerio C, Coolen M, Bally-Cuif L, De Strooper B. A self-organizing miR-132/Ctbp2 circuit regulates bimodal notch signals and glial progenitor fate choice during spinal cord maturation. Dev Cell. 2014;30:423–436. doi: 10.1016/j.devcel.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 96.Grandbarbe L, Michelucci A, Heurtaux T, Hemmer K, Morga E, Heuschling P. Notch signaling modulates the activation of microglial cells. Glia. 2007;55:1519–1530. doi: 10.1002/glia.20553. [DOI] [PubMed] [Google Scholar]
- 97.Morgan SC, Taylor DL, Pocock JM. Microglia release activators of neuronal proliferation mediated by activation of mitogen-activated protein kinase, phosphatidylinositol-3-kinase/Akt and delta-Notch signalling cascades. J Neurochem. 2004;90:89–101. doi: 10.1111/j.1471-4159.2004.02461.x. [DOI] [PubMed] [Google Scholar]
- 98.Arumugam TV, Chan SL, Jo DG, Yilmaz G, Tang SC, Cheng A, Gleichmann M, Okun E, Dixit VD, Chigurupati S, et al. Gamma secretase-mediated Notch signaling worsens brain damage and functional outcome in ischemic stroke. Nat Med. 2006;12:621–623. doi: 10.1038/nm1403. [DOI] [PubMed] [Google Scholar]
- 99.Liu HC, Zheng MH, Du YL, Wang L, Kuang F, Qin HY, Zhang BF, Han H. N9 microglial cells polarized by LPS and IL4 show differential responses to secondary environmental stimuli. Cell Immunol. 2012;278:84–90. doi: 10.1016/j.cellimm.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 100.Yao L, Kan EM, Kaur C, Dheen ST, Hao A, Lu J, Ling EA. Notch-1 signaling regulates microglia activation via NF-κB pathway after hypoxic exposure in vivo and in vitro. PLoS One. 2013;8:e78439. doi: 10.1371/journal.pone.0078439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Cao Q, Lu J, Kaur C, Sivakumar V, Li F, Cheah PS, Dheen ST, Ling EA. Expression of Notch-1 receptor and its ligands Jagged-1 and Delta-1 in amoeboid microglia in postnatal rat brain and murine BV-2 cells. Glia. 2008;56:1224–1237. doi: 10.1002/glia.20692. [DOI] [PubMed] [Google Scholar]
- 102.Morga E, Mouad-Amazzal L, Felten P, Heurtaux T, Moro M, Michelucci A, Gabel S, Grandbarbe L, Heuschling P. Jagged1 regulates the activation of astrocytes via modulation of NFkappaB and JAK/STAT/SOCS pathways. Glia. 2009;57:1741–1753. doi: 10.1002/glia.20887. [DOI] [PubMed] [Google Scholar]
- 103.Nardai S, Dobolyi A, Pál G, Skopál J, Pintér N, Lakatos K, Merkely B, Nagy Z. Selegiline promotes NOTCH-JAGGED signaling in astrocytes of the peri-infarct region and improves the functional integrity of the neurovascular unit in a rat model of focal ischemia. Restor Neurol Neurosci. 2015;33:1–14. doi: 10.3233/RNN-140420. [DOI] [PubMed] [Google Scholar]
- 104.Monsalve E, Ruiz-García A, Baladrón V, Ruiz-Hidalgo MJ, Sánchez-Solana B, Rivero S, García-Ramírez JJ, Rubio A, Laborda J, Díaz-Guerra MJ. Notch1 upregulates LPS-induced macrophage activation by increasing NF-kappaB activity. Eur J Immunol. 2009;39:2556–2570. doi: 10.1002/eji.200838722. [DOI] [PubMed] [Google Scholar]
- 105.Jones DP. Extracellular redox state: Refining the definition of oxidative stress in aging. Rejuvenation Res. 2006;9:169–181. doi: 10.1089/rej.2006.9.169. [DOI] [PubMed] [Google Scholar]
- 106.Darley-Usmar V, Halliwell B. Blood radicals: Reactive nitrogen species, reactive oxygen species, transition metal ions, and the vascular system. Pharm Res. 1996;13:649–662. doi: 10.1023/A:1016079012214. [DOI] [PubMed] [Google Scholar]
- 107.Wu JQ, Kosten TR, Zhang XY. Free radicals, antioxidant defense systems, and schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;46:200–206. doi: 10.1016/j.pnpbp.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 108.Catarino MD, Alves-Silva JM, Pereira OR, Cardoso SM. Antioxidant capacities of favones and benefts in oxidative-stress related diseases. Curr Top Med Chem. 2015;15:105–119. doi: 10.2174/1568026615666141209144506. [DOI] [PubMed] [Google Scholar]
- 109.Lee JC, Won MH. Neuroprotection of antioxidant enzymes against transient global cerebral ischemia in gerbils. Anat Cell Biol. 2014;47:149–156. doi: 10.5115/acb.2014.47.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Valko M, Morris H, Cronin MT. Metals, toxicity and oxidative stress. Curr Med Chem. 2005;12:1161–1208. doi: 10.2174/0929867053764635. [DOI] [PubMed] [Google Scholar]
- 111.Wu D, Yotnda P. Production and detection of reactive oxygen species (ROS) in cancers. J Vis Exp. 2011 doi: 10.3791/3357. pii: 3357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Reiter RJ, Tan DX, Manchester LC, Qi W. Biochemical reactivity of melatonin with reactive oxygen and nitrogen species: A review of the evidence. Cell Biochem Biophys. 2001;34:237–256. doi: 10.1385/CBB:34:2:237. [DOI] [PubMed] [Google Scholar]
- 113.Reiter RJ, Acuña-Castroviejo D, Tan DX, Burkhardt S. Free radical-mediated molecular damage. Mechanisms for the protective actions of melatonin in the central nervous system. Ann N Y Acad Sci. 2001;939:200–215. doi: 10.1111/j.1749-6632.2001.tb03627.x. [DOI] [PubMed] [Google Scholar]
- 114.Hemnani T, Parihar MS. Reactive oxygen species and oxidative DNA damage. Indian J Physiol Pharmacol. 1998;42:440–452. [PubMed] [Google Scholar]
- 115.Rodrigo R, Fernández-Gajardo R, Gutiérrez R, Matamala JM, Carrasco R, Miranda-Merchak A, Feuerhake W. Oxidative stress and pathophysiology of ischemic stroke: Novel therapeutic opportunities. CNS Neurol Disord Drug Targets. 2013;12:698–714. doi: 10.2174/1871527311312050015. [DOI] [PubMed] [Google Scholar]
- 116.Oprea E, Berteanu M, Cintezã D, Manolescu BN. The effect of the ALAnerv nutritional supplement on some oxidative stress markers in postacute stroke patients undergoing rehabilitation. Appl Physiol Nutr Metab. 2013;38:613–620. doi: 10.1139/apnm-2012-0436. [DOI] [PubMed] [Google Scholar]
- 117.Liang H, Zhang Y, Shi X, Wei T, Lou J. Role of Notch-1 signaling pathway in PC12 cell apoptosis induced by amyloid beta-peptide (25–35) Neural Regen Res. 2014;9:1297–1302. doi: 10.4103/1673-5374.137577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Braidy N, Jayasena T, Poljak A, Sachdev PS. Sirtuins in cognitive ageing and Alzheimer's disease. Curr Opin Psychiatry. 2012;25:226–230. doi: 10.1097/YCO.0b013e32835112c1. [DOI] [PubMed] [Google Scholar]
- 119.Nakane H, Kamouchi M, Hata J, Ibayashi S, Kusuda K, Omae T, Nagao T, Ago T, Kitazono T, EMINENT Study Investigators Effects of hydrochlorothiazide on oxidative stress and pulse pressure in hypertensive patients with chronic stroke: The EMINENT study. Intern Med. 2015;54:573–577. doi: 10.2169/internalmedicine.54.2631. [DOI] [PubMed] [Google Scholar]
- 120.Nakagawa T, Hasegawa Y, Uekawa K, Ma M, Katayama T, Sueta D, Toyama K, Kataoka K, Koibuchi N, Maeda M, et al. Renal denervation prevents stroke and brain injury via attenuation of oxidative stress in hypertensive rats. J Am Heart Assoc. 2013;2:e000375. doi: 10.1161/JAHA.113.000375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Das UN. Can free radicals induce coronary vasospasm and acute myocardial infarction? Med Hypotheses. 1992;39:90–94. doi: 10.1016/0306-9877(92)90147-5. [DOI] [PubMed] [Google Scholar]
- 122.Manzanero S, Santro T, Arumugam TV. Neuronal oxidative stress in acute ischemic stroke: Sources and contribution to cell injury. Neurochem Int. 2013;62:712–718. doi: 10.1016/j.neuint.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 123.Cojocaru IM, Cojocaru M, Sapira V, Ionescu A. Evaluation of oxidative stress in patients with acute ischemic stroke. Rom J Intern Med. 2013;51:97–106. [PubMed] [Google Scholar]
- 124.Icme F, Erel Ö, Avci A, Satar S, Gülen M, Acehan S. The relation between oxidative stress parameters, ischemic stroke, and hemorrhagic stroke. Turk J Med Sci. 2015;45:947–953. doi: 10.3906/sag-1402-96. [DOI] [PubMed] [Google Scholar]
- 125.Simão AN, Lehmann MF, Alferi DF, Meloni MZ, Flauzino T, Scavuzzi BM, de Oliveira SR, Lozovoy MA, Dichi I, Reiche EM. Metabolic syndrome increases oxidative stress but does not influence disability and short-time outcome in acute ischemic stroke patients. Metab Brain Dis. 2015;30:1409–1416. doi: 10.1007/s11011-015-9720-y. [DOI] [PubMed] [Google Scholar]
- 126.Tsai NW, Chang YT, Huang CR, Lin YJ, Lin WC, Cheng BC, Su CM, Chiang YF, Chen SF, Huang CC, et al. Association between oxidative stress and outcome in different subtypes of acute ischemic stroke. Biomed Res Int. 2014;2014:256879. doi: 10.1155/2014/256879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Pantcheva P, Elias M, Duncan K, Borlongan CV, Tajiri N, Kaneko Y. The role of DJ-1 in the oxidative stress cell death cascade after stroke. Neural Regen Res. 2014;9:1430–1433. doi: 10.4103/1673-5374.139458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Nabavi SF, Dean OM, Turner A, Sureda A, Daglia M, Nabavi SM. Oxidative stress and post-stroke depression: Possible therapeutic role of polyphenols? Curr Med Chem. 2015;22:343–351. doi: 10.2174/0929867321666141106122319. [DOI] [PubMed] [Google Scholar]
- 129.Gonullu H, Aslan M, Karadas S, Kati C, Duran L, Milanlioglu A, Aydin MN, Demir H. Serum prolidase enzyme activity and oxidative stress levels in patients with acute hemorrhagic stroke. Scand J Clin Lab Invest. 2014;74:199–205. doi: 10.3109/00365513.2013.873949. [DOI] [PubMed] [Google Scholar]
- 130.El Kossi MM, Zakhary MM. Oxidative stress in the context of acute cerebrovascular stroke. Stroke. 2000;31:1889–1892. doi: 10.1161/01.STR.31.8.1889. [DOI] [PubMed] [Google Scholar]
- 131.Milanlioglu A, Aslan M, Ozkol H, Çilingir V, Nuri Aydin M, Karadas S. Serum antioxidant enzymes activities and oxidative stress levels in patients with acute ischemic stroke: Influence on neurological status and outcome. Wien Klin Wochenschr. 2016;128:169–174. doi: 10.1007/s00508-015-0742-6. [DOI] [PubMed] [Google Scholar]
- 132.Newton DF, Naiberg MR, Goldstein BI. Oxidative stress and cognition amongst adults without dementia or stroke: Implications for mechanistic and therapeutic research in psychiatric disorders. Psychiatry Res. 2015;227:127–134. doi: 10.1016/j.psychres.2015.03.038. [DOI] [PubMed] [Google Scholar]
- 133.Nakajima H, Kubo T, Ihara H, Hikida T, Danjo T, Nakatsuji M, Shahani N, Itakura M, Ono Y, Azuma YT, et al. Nuclear-translocated Glyceraldehyde-3-phosphate dehydrogenase promotes poly(ADP-ribose) polymerase-1 activation during Oxidative/Nitrosative stress in stroke. J Biol Chem. 2015;290:14493–14503. doi: 10.1074/jbc.M114.635607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kotur-Stevuljevic J, Bogavac-Stanojevic N, Jelic-Ivanovic Z, Stefanovic A, Gojkovic T, Joksic J, Sopic M, Gulan B, Janac J, Milosevic S. Oxidative stress and paraoxonase 1 status in acute ischemic stroke patients. Atherosclerosis. 2015;241:192–198. doi: 10.1016/j.atherosclerosis.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 135.Han Z, Shen F, He Y, Degos V, Camus M, Maze M, Young WL, Su H. Activation of α-7 nicotinic acetylcholine receptor reduces ischemic stroke injury through reduction of pro-inflammatory macrophages and oxidative stress. PLoS One. 2014;9:e105711. doi: 10.1371/journal.pone.0105711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lagowska-Lenard M, Bielewicz J, Raszewski G, Stelmasiak Z, Bartosik-Psujek H. Oxidative stress in cerebral stroke. Pol Merkur Lekarski. 2008;25:205–208. In Polish. [PubMed] [Google Scholar]
- 137.Takemori K, Murakami T, Kometani T, Ito H. Possible involvement of oxidative stress as a causative factor in blood-brain barrier dysfunction in stroke-prone spontaneously hypertensive rats. Microvasc Res. 2013;90:169–172. doi: 10.1016/j.mvr.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 138.Hung LM, Huang JP, Liao JM, Yang MH, Li DE, Day YJ, Huang SS. Insulin renders diabetic rats resistant to acute ischemic stroke by arresting nitric oxide reaction with superoxide to form peroxynitrite. J Biomed Sci. 2014;21:92. doi: 10.1186/s12929-014-0092-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Fabian RH, Kent TA. Hyperglycemia accentuates persistent 'functional uncoupling' of cerebral microvascular nitric oxide and superoxide following focal ischemia/reperfusion in rats. Transl Stroke Res. 2012;3:482–490. doi: 10.1007/s12975-012-0210-9. [DOI] [PubMed] [Google Scholar]
- 140.Fabian RH, Perez-Polo JR, Kent TA. Perivascular nitric oxide and superoxide in neonatal cerebral hypoxia-ischemia. Am J Physiol Heart Circ Physiol. 2008;295:H1809–H1814. doi: 10.1152/ajpheart.00301.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Gümüştaş K, Meta Güzeyli FM, Atükeren P, Sanus GZ, Kemerdere R, Tanriverdi T, Kaynar MY. The effects of vitamin E on lipid peroxidation, nitric oxide production and superoxide dismutase expression in hyperglycemic rats with cerebral ischemia-reperfusion injury. Turk Neurosurg. 2007;17:78–82. [PubMed] [Google Scholar]
- 142.Forman LJ, Liu P, Nagele RG, Yin K, Wong PY. Augmentation of nitric oxide, superoxide, and peroxynitrite production during cerebral ischemia and reperfusion in the rat. Neurochem Res. 1998;23:141–148. doi: 10.1023/A:1022468522564. [DOI] [PubMed] [Google Scholar]
- 143.Brosnan MJ, Hamilton CA, Graham D, Lygate CA, Jardine E, Dominiczak AF. Irbesartan lowers superoxide levels and increases nitric oxide bioavailability in blood vessels from spontaneously hypertensive stroke-prone rats. J Hypertens. 2002;20:281–286. doi: 10.1097/00004872-200202000-00018. [DOI] [PubMed] [Google Scholar]
- 144.Baumeister P, Huebner T, Reiter M, Schwenk-Zieger S, Harréus U. Reduction of oxidative DNA fragmentation by ascorbic acid, zinc and N-acetylcysteine in nasal mucosa tissue cultures. Anticancer Res. 2009;29:4571–4574. [PubMed] [Google Scholar]
- 145.Mikhaĭlov VF, Mazurik VK, Burlakova EB. Signal function of the reactive oxygen species in regulatory networks of the cell reaction to damaging effects: Contribution of radiosensitivity and genome instability. Radiats Biol Radioecol. 2003;43:5–18. In Russian. [PubMed] [Google Scholar]
- 146.Fischer-Nielsen A, Corcoran GB, Poulsen HE, Kamendulis LM, Loft S. Menadione-induced DNA fragmentation without 8-oxo-2′-deoxyguanosine formation in isolated rat hepatocytes. Biochem Pharmacol. 1995;49:1469–1474. doi: 10.1016/0006-2952(94)00525-Q. [DOI] [PubMed] [Google Scholar]
- 147.Zhou T, He Q, Tong Y, Zhan R, Xu F, Fan D, Guo X, Han H, Qin S, Chui D. Phospholipid transfer protein (PLTP) deficiency impaired blood-brain barrier integrity by increasing cerebrovascular oxidative stress. Biochem Biophys Res Commun. 2014;445:352–356. doi: 10.1016/j.bbrc.2014.01.194. [DOI] [PubMed] [Google Scholar]
- 148.Tóth AE, Walter FR, Bocsik A, Sántha P, Veszelka S, Nagy L, Puskás LG, Couraud PO, Takata F, Dohgu S, et al. Edaravone protects against methylglyoxal-induced barrier damage in human brain endothelial cells. PLoS One. 2014;9:e100152. doi: 10.1371/journal.pone.0100152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Elmorsy E, Elzalabany LM, Elsheikha HM, Smith PA. Adverse effects of antipsychotics on micro-vascular endothelial cells of the human blood-brain barrier. Brain Res. 2014;1583:255–268. doi: 10.1016/j.brainres.2014.08.011. [DOI] [PubMed] [Google Scholar]
- 150.Sathanoori R, Swärd K, Olde B, Erlinge D. The ATP Receptors P2X7 and P2X4 modulate high glucose and Palmitate-Induced inflammatory responses in endothelial cells. PLoS One. 2015;10:e0125111. doi: 10.1371/journal.pone.0125111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Okada R, Wu Z, Zhu A, Ni J, Zhang J, Yoshimine Y, Peters C, Saftig P, Nakanishi H. Cathepsin D deficiency induces oxidative damage in brain pericytes and impairs the blood-brain barrier. Mol Cell Neurosci. 2015;64:51–60. doi: 10.1016/j.mcn.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 152.Abdul-Muneer PM, Chandra N, Haorah J. Interactions of oxidative stress and neurovascular infammation in the pathogenesis of traumatic brain injury. Mol Neurobiol. 2015;51:966–979. doi: 10.1007/s12035-014-8752-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ste-Marie L, Hazell AS, Bémeur C, Butterworth R, Montgomery J. Immunohistochemical detection of inducible nitric oxide synthase, nitrotyrosine and manganese superoxide dismutase following hyperglycemic focal cerebral ischemia. Brain Res. 2001;918:10–19. doi: 10.1016/S0006-8993(01)02903-1. [DOI] [PubMed] [Google Scholar]
- 154.Kumura E, Yoshimine T, Kubo S, Tanaka S, Hayakawa T, Shiga T, Kosaka H. Effects of superoxide dismutase on nitric oxide production during reperfusion after focal cerebral ischemia is rats. Neurosci Lett. 1995;200:137–140. doi: 10.1016/0304-3940(95)12099-P. [DOI] [PubMed] [Google Scholar]
- 155.Al-Maghrebi M, Renno WM. Genistein alleviates testicular ischemia and reperfusion injury-induced sper-matogenic damage and oxidative stress by suppressing abnormal testicular matrix metalloproteinase system via the Notch 2/Jagged 1/Hes-1 and caspase-8 pathways. J Physiol Pharmacol. 2016;67:129–137. [PubMed] [Google Scholar]
- 156.Xie H, Sun J, Chen Y, Zong M, Li S, Wang Y. EGCG attenuates uric Acid-Induced inflammatory and oxidative stress responses by medicating the NOTCH pathway. Oxid Med Cell Longev. 2015;2015:214836. doi: 10.1155/2015/214836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Xie F, Cai W, Liu Y, Li Y, Du B, Feng L, Qiu L. Vaccarin attenuates the human EA.hy926 endothelial cell oxidative stress injury through inhibition of Notch signaling. Int J Mol Med. 2015;35:135–142. doi: 10.3892/ijmm.2014.1977. [DOI] [PubMed] [Google Scholar]
- 158.Yang Y, Duan W, Liang Z, Yi W, Yan J, Wang N, Li Y, Chen W, Yu S, Jin Z, Yi D. Curcumin attenuates endothelial cell oxidative stress injury through Notch signaling inhibition. Cell Signal. 2013;25:615–629. doi: 10.1016/j.cellsig.2012.11.025. [DOI] [PubMed] [Google Scholar]
- 159.Li M, Chen F, Clifton N, Sullivan DM, Dalton WS, Gabrilovich DI, Nefedova Y. Combined inhibition of Notch signaling and Bcl-2/Bcl-xL results in synergistic antimyeloma effect. Mol Cancer Ther. 2010;9:3200–3209. doi: 10.1158/1535-7163.MCT-10-0372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Chen C, Cui H, Li Z, Wang R, Zhou C. Normobaric oxygen for cerebral ischemic injury. Neural Regen Res. 2013;8:2885–2894. doi: 10.3969/j.issn.1673-5374.2013.31.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Zhu B, Yang P, Mammat N, Ding H, He J, Qian Y, Fei J, Abdukerim K. Aiweixin, a traditional Uyghur medicinal formula, protects against chromium toxicity in Caenorhabditis elegans. BMC Complement Altern Med. 2015;15:285. doi: 10.1186/s12906-015-0783-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Finsterer J. Neuromuscular implications in CADASIL. Cerebrovasc Dis. 2007;24:401–404. doi: 10.1159/000108428. [DOI] [PubMed] [Google Scholar]
- 163.Santoni M, Pantano F, Amantini C, Nabissi M, Conti A, Burattini L, Zoccoli A, Berardi R, Santoni G, Tonini G, et al. Emerging strategies to overcome the resistance to current mTOR inhibitors in renal cell carcinoma. Biochim Biophys Acta. 2014;1845:221–231. doi: 10.1016/j.bbcan.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 164.Pei H, Yu Q, Xue Q, Guo Y, Sun L, Hong Z, Han H, Gao E, Qu Y, Tao L. Notch1 cardioprotection in myocardial ischemia/reperfusion involves reduction of oxidative/nitrative stress. Basic Res Cardiol. 2013;108:373. doi: 10.1007/s00395-013-0373-x. [DOI] [PubMed] [Google Scholar]
- 165.Simón R, Aparicio R, Housden BE, Bray S, Busturia A. Drosophila p53 controls Notch expression and balances apoptosis and proliferation. Apoptosis. 2014;19:1430–1443. doi: 10.1007/s10495-014-1000-5. [DOI] [PubMed] [Google Scholar]
- 166.Zheng WX, Cao XL, Wang F, Wang J, Ying TZ, Xiao W, Zhang Y, Xing H, Dong W, Xu SQ, et al. Baicalin inhibiting cerebral ischemia/hypoxia-induced neuronal apoptosis via MRTF-A-mediated transactivity. Eur J Pharmacol. 2015;767:201–210. doi: 10.1016/j.ejphar.2015.10.027. [DOI] [PubMed] [Google Scholar]
- 167.Baroja-Mazo A, Martín-Sánchez F, Gomez AI, Martínez CM, Amores-Iniesta J, Compan V, Barberà-Cremades M, Yagüe J, Ruiz-Ortiz E, Antón J, et al. The NLRP3 inflammasome is released as a particulate danger signal that amplifes the inflammatory response. Nat Immunol. 2014;15:738–748. doi: 10.1038/ni.2919. [DOI] [PubMed] [Google Scholar]
- 168.Yang RY, Liu FT. Galectins in cell growth and apoptosis. Cell Mol Life Sci. 2003;60:267–276. doi: 10.1007/s000180300022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Bao JX, Su YT, Cheng YP, Zhang HJ, Xie XP, Chang YM. Vascular sphingolipids in physiological and pathological adaptation. Front Biosci (Landmark Ed) 2016;21:1168–1186. doi: 10.2741/4448. [DOI] [PubMed] [Google Scholar]
- 170.Kagiya G, Ogawa R, Tabuchi Y, Feril LB, Jr, Nozaki T, Fukuda S, Yamamoto K, Kondo T. Expression of heme oxygenase-1 due to intracellular reactive oxygen species induced by ultrasound. Ultrason Sonochem. 2006;13:388–396. doi: 10.1016/j.ultsonch.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 171.Santiago B, Galindo M, Palao G, Pablos JL. Intracellular regulation of Fas-induced apoptosis in human fibroblasts by extracellular factors and cycloheximide. J Immunol. 2004;172:560–566. doi: 10.4049/jimmunol.172.1.560. [DOI] [PubMed] [Google Scholar]
- 172.Wang L, Song G, Liu M, Chen B, Chen Y, Shen Y, Zhu J, Zhou X. MicroRNA-375 overexpression influences P19 cell proliferation, apoptosis and differentiation through the Notch signaling pathway. Int J Mol Med. 2016;37:47–55. doi: 10.3892/ijmm.2015.2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Aboutaleb N, Shamsaei N, Khaksari M, Erfani S, Rajabi H, Nikbakht F. Pre-ischemic exercise reduces apoptosis in hippocampal CA3 cells after cerebral ischemia by modulation of the Bax/Bcl-2 proteins ratio and prevention of caspase-3 activation. J Physiol Sci. 2015;65:435–443. doi: 10.1007/s12576-015-0382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Zhang JF, Shi LL, Zhang L, Zhao ZH, Liang F, Xu X, Zhao LY, Yang PB, Zhang JS, Tian YF. MicroRNA-25 negatively regulates cerebral Ischemia/Reperfusion Injury-Induced cell apoptosis through Fas/FasL pathway. J Mol Neurosci. 2016;58:507–516. doi: 10.1007/s12031-016-0712-0. [DOI] [PubMed] [Google Scholar]
- 175.Xue R, Wu G, Wei X, Lv J, Fu R, Lei X, Zhang Z, Li W, He J, Zhao H, et al. Tea polyphenols may attenuate the neurocognitive impairment caused by global cerebral ischemia/reperfusion injury via anti-apoptosis. Nutr Neurosci. 2016;19:63–69. doi: 10.1179/1476830514Y.0000000160. [DOI] [PubMed] [Google Scholar]
- 176.Yang Y, Gao K, Hu Z, Li W, Davies H, Ling S, Rudd JA, Fang M. Autophagy upregulation and apoptosis downregulation in DAHP and triptolide treated cerebral ischemia. Mediators Inflamm. 2015;2015:120198. doi: 10.1155/2015/120198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Wu L, Zhao QS, Li TW, Li HY, Wang QB, Bi XY, Cai XK, Tang N. Yifei Xuanfei Jiangzhuo formula, a Chinese herbal decoction, improves memory impairment through inhibiting apoptosis and enhancing PKA/CREB signal transduction in rats with cerebral ischemia/reperfusion. Mol Med Rep. 2015;12:4273–4283. doi: 10.3892/mmr.2015.3962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Saad MA, Abdelsalam RM, Kenawy SA, Attia AS. Ischemic preconditioning and postconditioning alleviates hippocampal tissue damage through abrogation of apoptosis modulated by oxidative stress and inflammation during transient global cerebral ischemia-reperfusion in rats. Chem Biol Interact. 2015;232:21–29. doi: 10.1016/j.cbi.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 179.Fan M, Jin W, Zhao H, Xiao Y, Jia Y, Yin Y, Jiang X, Xu J, Meng N, Lv P. Lithium chloride administration prevents spatial learning and memory impairment in repeated cerebral ischemia-reperfusion mice by depressing apoptosis and increasing BDNF expression in hippocampus. Behav Brain Res. 2015;291:399–406. doi: 10.1016/j.bbr.2015.05.047. [DOI] [PubMed] [Google Scholar]
- 180.Garrigue P, Giacomino L, Bucci C, Muzio V, Filannino MA, Sabatier F, Dignat-George F, Pisano P, Guillet B. Single photon emission computed tomography imaging of cerebral blood flow, blood-brain barrier disruption, and apoptosis time course after focal cerebral ischemia in rats. Int J Stroke. 2016;11:117–126. doi: 10.1177/1747493015607516. [DOI] [PubMed] [Google Scholar]
- 181.Cao G, Zhou H, Jiang N, Han Y, Hu Y, Zhang Y, Qi J, Kou J, Yu B. YiQiFuMai powder injection ameliorates cerebral ischemia by inhibiting endoplasmic reticulum Stress-Mediated neuronal apoptosis. Oxid Med Cell Longev. 2016;2016:5493279. doi: 10.1155/2016/5493279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Yan XG, Cheng BH, Wang X, Ding LC, Liu HQ, Chen J, Bai B. Lateral intracerebroventricular injection of Apelin-13 inhibits apoptosis after cerebral ischemia/reperfusion injury. Neural Regen Res. 2015;10:766–771. doi: 10.4103/1673-5374.157243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Saad MA, Abdel Salam RM, Kenawy SA, Attia AS. Pinocembrin attenuates hippocampal inflammation, oxidative perturbations and apoptosis in a rat model of global cerebral ischemia reperfusion. Pharmacol Rep. 2015;67:115–122. doi: 10.1016/j.pharep.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 184.Jiang Y, Li L, Tan X, Liu B, Zhang Y, Li C. miR-210 mediates vagus nerve stimulation-induced antioxidant stress and anti-apoptosis reactions following cerebral ischemia/reperfusion injury in rats. J Neurochem. 2015;134:173–181. doi: 10.1111/jnc.13097. [DOI] [PubMed] [Google Scholar]
- 185.Chopp M, Li Y. Apoptosis in focal cerebral ischemia. Acta Neurochir Suppl. 1996;66:21–26. doi: 10.1007/978-3-7091-9465-2_4. [DOI] [PubMed] [Google Scholar]
- 186.Wu X, Li L, Zhang L, Wu J, Zhou Y, Zhou Y, Zhao Y, Zhao J. Inhibition of thioredoxin-1 with siRNA exacerbates apoptosis by activating the ASK1-JNK/p38 pathway in brain of a stroke model rats. Brain Res. 2015;1599:20–31. doi: 10.1016/j.brainres.2014.12.033. [DOI] [PubMed] [Google Scholar]
- 187.Baregamian N, Song J, Bailey CE, Papaconstantinou J, Evers BM, Chung DH. Tumor necrosis factor-alpha and apoptosis signal-regulating kinase 1 control reactive oxygen species release, mitochondrial autophagy, and c-Jun N-terminal kinase/p38 phosphorylation during necrotizing enterocolitis. Oxid Med Cell Longev. 2009;2:297–306. doi: 10.4161/oxim.2.5.9541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Bedogni B, Warneke JA, Nickoloff BJ, Giaccia AJ, Powell MB. Notch1 is an effector of Akt and hypoxia in melanoma development. J Clin Invest. 2008;118:3660–3670. doi: 10.1172/JCI36157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Petit A, Bihel F, Alvès da Costa C, Pourquié O, Checler F, Kraus JL. New protease inhibitors prevent gamma-secretase-mediated production of Abeta40/42 without affecting Notch cleavage. Nat Cell Biol. 2001;3:507–511. doi: 10.1038/35074581. [DOI] [PubMed] [Google Scholar]
- 190.Okochi M, Steiner H, Fukumori A, Tanii H, Tomita T, Tanaka T, Iwatsubo T, Kudo T, Takeda M, Haass C. Presenilins mediate a dual intramembranous gamma-secretase cleavage of Notch-1. EMBO J. 2002;21:5408–5416. doi: 10.1093/emboj/cdf541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ikeuchi T, Sisodia SS. The Notch ligands, Delta1 and Jagged2, are substrates for presenilin-dependent 'gamma-secretase' cleavage. J Biol Chem. 2003;278:7751–7754. doi: 10.1074/jbc.C200711200. [DOI] [PubMed] [Google Scholar]
- 192.Yang G, Gong Y, Wang Q, Wang Y, Zhang X. The role of miR-100-mediated Notch pathway in apoptosis of gastric tumor cells. Cell Signal. 2015;27:1087–1101. doi: 10.1016/j.cellsig.2015.02.013. [DOI] [PubMed] [Google Scholar]
- 193.Liu XD, Zhang LY, Zhu TC, Zhang RF, Wang SL, Bao Y. Overexpression of miR-34c inhibits high glucose-induced apoptosis in podocytes by targeting Notch signaling pathways. Int J Clin Exp Pathol. 2015;8:4525–4534. [PMC free article] [PubMed] [Google Scholar]
- 194.Wang XM, Yao M, Liu SX, Hao J, Liu QJ, Gao F. Interplay between the Notch and PI3K/Akt pathways in high glucose-induced podocyte apoptosis. Am J Physiol Renal Physiol. 2014;306:F205–F213. doi: 10.1152/ajprenal.90005.2013. [DOI] [PubMed] [Google Scholar]
- 195.Gao F, Yao M, Shi Y, Hao J, Ren Y, Liu Q, Wang X, Duan H. Notch pathway is involved in high glucose-induced apoptosis in podocytes via Bcl-2 and p53 pathways. J Cell Biochem. 2013;114:1029–1038. doi: 10.1002/jcb.24442. [DOI] [PubMed] [Google Scholar]
- 196.Yang Y, Li X, Zhang L, Liu L, Jing G, Cai H. Ginsenoside Rg1 suppressed infammation and neuron apoptosis by activating PPAR γ/HO-1 in hippocampus in rat model of cerebral ischemia-reperfusion injury. Int J Clin Exp Pathol. 2015;8:2484–2494. [PMC free article] [PubMed] [Google Scholar]
- 197.Zhao Y, Deng B, Li Y, Zhou L, Yang L, Gou X, Wang Q, Chen G, Xu H, Xu L. Electroacupuncture pretreatment attenuates cerebral ischemic injury via Notch Pathway-Mediated Up-Regulation of hypoxia inducible Factor-1α in Rats. Cell Mol Neurobiol. 2015;35:1093–1103. doi: 10.1007/s10571-015-0203-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Cheng YL, Choi Y, Seow WL, Manzanero S, Sobey CG, Jo DG, Arumugam TV. Evidence that neuronal Notch-1 promotes JNK/c-Jun activation and cell death following ischemic stress. Brain Res. 2014;1586:193–202. doi: 10.1016/j.brainres.2014.08.054. [DOI] [PubMed] [Google Scholar]
- 199.Meng S, Su Z, Liu Z, Wang N, Wang Z. Rac1 contributes to cerebral ischemia reperfusion-induced injury in mice by regulation of Notch2. Neuroscience. 2015;306:100–114. doi: 10.1016/j.neuroscience.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 200.Ma M, Wang X, Ding X, Teng J, Shao F, Zhang J. Numb/Notch signaling plays an important role in cerebral ischemia-induced apoptosis. Neurochem Res. 2013;38:254–261. doi: 10.1007/s11064-012-0914-y. [DOI] [PubMed] [Google Scholar]
- 201.Sun J, Ling Z, Wang F, Chen W, Li H, Jin J, Zhang H, Pang M, Yu J, Liu J. Clostridium butyricum pretreatment attenuates cerebral ischemia/reperfusion injury in mice via anti-oxidation and anti-apoptosis. Neurosci Lett. 2016;613:30–35. doi: 10.1016/j.neulet.2015.12.047. [DOI] [PubMed] [Google Scholar]
- 202.Arumugam TV, Cheng YL, Choi Y, Choi YH, Yang S, Yun YK, Park JS, Yang DK, Thundyil J, Gelderblom M, et al. Evidence that gamma-secretase-mediated Notch signaling induces neuronal cell death via the nuclear factor-kappaB-Bcl-2-interacting mediator of cell death pathway in ischemic stroke. Mol Pharmacol. 2011;80:23–31. doi: 10.1124/mol.111.071076. [DOI] [PubMed] [Google Scholar]
- 203.Park JS, Manzanero S, Chang JW, Choi Y, Baik SH, Cheng YL, Li YI, Gwon AR, Woo HN, Jang J, et al. Calsenilin contributes to neuronal cell death in ischemic stroke. Brain Pathol. 2013;23:402–412. doi: 10.1111/bpa.12013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Baik SH, Fane M, Park JH, Cheng YL, Yang-Wei Fann D, Yun UJ, Choi Y, Park JS, Chai BH, Back SH, et al. Pin1 promotes neuronal death in stroke by stabilizing Notch intracellular domain. Ann Neurol. 2015;77:504–516. doi: 10.1002/ana.24347. [DOI] [PubMed] [Google Scholar]
- 205.Viswanathan A, Gray F, Bousser MG, Baudrimont M, Chabriat H. Cortical neuronal apoptosis in CADASIL. Stroke. 2006;37:2690–2695. doi: 10.1161/01.STR.0000245091.28429.6a. [DOI] [PubMed] [Google Scholar]
- 206.Kalimo H, Ruchoux MM, Viitanen M, Kalaria RN. CADASIL: A common form of hereditary arteriopathy causing brain infarcts and dementia. Brain Pathol. 2002;12:371–384. doi: 10.1111/j.1750-3639.2002.tb00451.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Liu XY, Gonzalez-Toledo ME, Fagan A, Duan WM, Liu Y, Zhang S, Li B, Piao CS, Nelson L, Zhao LR. Stem cell factor and granulocyte colony-stimulating factor exhibit therapeutic effects in a mouse model of CADASIL. Neurobiol Dis. 2015;73:189–203. doi: 10.1016/j.nbd.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 208.Wang S, Yuan Y, Xia W, Li F, Huang Y, Zhou Y, Guo Y. Neuronal apoptosis and synaptic density in the dentate gyrus of ischemic rats' response to chronic mild stress and the effects of Notch signaling. PLoS One. 2012;7:e42828. doi: 10.1371/journal.pone.0042828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Zhang HP, Sun YY, Chen XM, Yuan LB, Su BX, Ma R, Zhao RN, Dong HL, Xiong L. The neuroprotective effects of isofurane preconditioning in a murine transient global cerebral ischemia-reperfusion model: The role of the Notch signaling pathway. Neuromolecular Med. 2014;16:191–204. doi: 10.1007/s12017-013-8273-7. [DOI] [PubMed] [Google Scholar]
- 210.Yang Q, Yan W, Li X, Hou L, Dong H, Wang Q, Wang S, Zhang X, Xiong L. Activation of canonical notch signaling pathway is involved in the ischemic tolerance induced by sevo-flurane preconditioning in mice. Anesthesiology. 2012;117:996–1005. doi: 10.1097/ALN.0b013e31826cb469. [DOI] [PubMed] [Google Scholar]
- 211.Yao J, Qian C. Over-activated Notch-1 protects gastric carcinoma BGC-823 cells from TNFalpha-induced apoptosis. Dig Liver Dis. 2009;41:867–874. doi: 10.1016/j.dld.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 212.Yang X, Klein R, Tian X, Cheng HT, Kopan R, Shen J. Notch activation induces apoptosis in neural progenitor cells through a p53-dependent pathway. Dev Biol. 2004;269:81–94. doi: 10.1016/j.ydbio.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 213.de Antonellis P, Medaglia C, Cusanelli E, Andolfo I, Liguori L, De Vita G, Carotenuto M, Bello A, Formiggini F, Galeone A, et al. MiR-34a targeting of Notch ligand delta-like 1 impairs CD15+/CD133+ tumor-propagating cells and supports neural differentiation in medulloblastoma. PLoS One. 2011;6:e24584. doi: 10.1371/journal.pone.0024584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Sionov RV, Kfr-Erenfeld S, Spokoini R, Yefenof E. A role for bcl-2 in notch1-dependent transcription in thymic lymphoma cells. Adv Hematol. 2012;2012:435241. doi: 10.1155/2012/435241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Ye QF, Zhang YC, Peng XQ, Long Z, Ming YZ, He LY. Silencing Notch-1 induces apoptosis and increases the chemo-sensitivity of prostate cancer cells to docetaxel through Bcl-2 and Bax. Oncol Lett. 2012;3:879–884. doi: 10.3892/ol.2012.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Cao H, Hu Y, Wang P, Zhou J, Deng Z, Wen J. Down-regulation of Notch receptor signaling pathway induces caspase-dependent and caspase-independent apoptosis in lung squamous cell carcinoma cells. APMIS. 2012;120:441–450. doi: 10.1111/j.1600-0463.2011.02825.x. [DOI] [PubMed] [Google Scholar]
- 217.Brockhaus M, Grünberg J, Röhrig S, Loetscher H, Wittenburg N, Baumeister R, Jacobsen H, Haass C. Caspase-mediated cleavage is not required for the activity of presenilins in amyloidogenesis and NOTCH signaling. Neuroreport. 1998;9:1481–1486. doi: 10.1097/00001756-199805110-00043. [DOI] [PubMed] [Google Scholar]
- 218.Wu K, Hu L, Hou J. Selective suppression of Notch1 inhibits proliferation of renal cell carcinoma cells through JNK/p38 pathway. Oncol Rep. 2016;35:2795–2800. doi: 10.3892/or.2016.4687. [DOI] [PubMed] [Google Scholar]
- 219.Smith KA, Voiriot G, Tang H, Fraidenburg DR, Song S, Yamamura H, Yamamura A, Guo Q, Wan J, Pohl NM, et al. Notch activation of Ca(2+) signaling in the development of hypoxic pulmonary vasoconstriction and pulmonary hypertension. Am J Respir Cell Mol Biol. 2015;53:355–367. doi: 10.1165/rcmb.2014-0235OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Rothschild SC, Lahvic J, Francescatto L, McLeod JJ, Burgess SM, Tombes RM. CaMK-II activation is essential for zebrafsh inner ear development and acts through Delta-Notch signaling. Dev Biol. 2013;381:179–188. doi: 10.1016/j.ydbio.2013.05.028. [DOI] [PubMed] [Google Scholar]
- 221.Kim SK, Park HJ, Hong HS, Baik EJ, Jung MW, Mook-Jung I. ERK1/2 is an endogenous negative regulator of the gamma-secretase activity. FASEB J. 2006;20:157–159. doi: 10.1096/fj.05-4055fje. [DOI] [PubMed] [Google Scholar]
- 222.Servín-González LS, Granados-López AJ, López JA. Families of microRNAs expressed in clusters regulate cell signaling in cervical cancer. Int J Mol Sci. 2015;16:12773–12790. doi: 10.3390/ijms160612773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Aguirre A, Rubio ME, Gallo V. Notch and EGFR pathway interaction regulates neural stem cell number and self-renewal. Nature. 2010;467:323–327. doi: 10.1038/nature09347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Nagaraj R, Banerjee U. Regulation of Notch and Wingless signalling by phyllopod, a transcriptional target of the EGFR pathway. EMBO J. 2009;28:337–346. doi: 10.1038/emboj.2008.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Elmadhun NY, Sabe AA, Lassaletta AD, Chu LM, Kondra K, Sturek M, Sellke FW. Metabolic syndrome impairs notch signaling and promotes apoptosis in chronically ischemic myocardium. J Thorac Cardiovasc Surg. 2014;148:1048–1055. doi: 10.1016/j.jtcvs.2014.05.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Guo D, Ye J, Dai J, Li L, Chen F, Ma D, Ji C. Notch-1 regulates Akt signaling pathway and the expression of cell cycle regulatory proteins cyclin D1, CDK2 and p21 in T-ALL cell lines. Leuk Res. 2009;33:678–685. doi: 10.1016/j.leukres.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 227.Sweetwyne MT, Gruenwald A, Niranjan T, Nishinakamura R, Strobl LJ, Susztak K. Notch1 and Notch2 in podocytes play differential roles during diabetic nephropathy development. Diabetes. 2015;64:4099–4111. doi: 10.2337/db15-0260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Bheeshmachar G, Purushotaman D, Sade H, Gunasekharan V, Rangarajan A, Sarin A. Evidence for a role for notch signaling in the cytokine-dependent survival of activated T cells. J Immunol. 2006;177:5041–5050. doi: 10.4049/jimmunol.177.8.5041. [DOI] [PubMed] [Google Scholar]
- 229.Sholler GS, Currier EA, Dutta A, Slavik MA, Illenye SA, Mendonca MC, Dragon J, Roberts SS, Bond JP. PCI-24781 (abexinostat), a novel histone deacetylase inhibitor, induces reactive oxygen species-dependent apoptosis and is synergistic with bortezomib in neuroblastoma. J Cancer Ther Res. 2013;2:21. doi: 10.7243/2049-7962-2-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Yu HC, Bai L, Yue SQ, Wang DS, Wang L, Han H, Dou KF. Notch signal protects non-parenchymal cells from ischemia/reperfusion injury in vitro by repressing ROS. Ann Hepatol. 2013;12:815–821. [PubMed] [Google Scholar]
- 231.Naik S, MacFarlane M, Sarin A. Notch4 signaling confers susceptibility to TRAIL-induced apoptosis in breast cancer cells. J Cell Biochem. 2015;116:1371–1380. doi: 10.1002/jcb.25094. [DOI] [PubMed] [Google Scholar]
- 232.Wang C, Qi R, Li N, Wang Z, An H, Zhang Q, Yu Y, Cao X. Notch1 signaling sensitizes tumor necrosis factor-related apoptosis-inducing ligand-induced apoptosis in human hepatocellular carcinoma cells by inhibiting Akt/Hdm2-mediated p53 degradation and up-regulating p53-dependent DR5 expression. J Biol Chem. 2009;284:16183–16190. doi: 10.1074/jbc.M109.002105. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 233.Chung AS, Lee J, Ferrara N. Targeting the tumour vascu-lature: Insights from physiological angiogenesis. Nat Rev Cancer. 2010;10:505–514. doi: 10.1038/nrc2868. [DOI] [PubMed] [Google Scholar]
- 234.Carmeliet P, Moons L, Dewerchin M, Mackman N, Luther T, Breier G, Ploplis V, Müller M, Nagy A, Plow E, et al. Insights in vessel development and vascular disorders using targeted inactivation and transfer of vascular endothelial growth factor, the tissue factor receptor and the plasminogen system. Ann N Y Acad Sci. 1997;811:191–206. doi: 10.1111/j.1749-6632.1997.tb52002.x. [DOI] [PubMed] [Google Scholar]
- 235.Lymboussaki A, Olofsson B, Eriksson U, Alitalo K. Vascular endothelial growth factor (VEGF) and VEGF-C show overlapping binding sites in embryonic endothelia and distinct sites in differentiated adult endothelia. Circ Res. 1999;85:992–999. doi: 10.1161/01.RES.85.11.992. [DOI] [PubMed] [Google Scholar]
- 236.McColl BK, Stacker SA, Achen MG. Molecular regulation of the VEGF family-inducers of angiogenesis and lymphangiogenesis. APMIS. 2004;112:463–480. doi: 10.1111/j.1600-0463.2004.apm11207-0807.x. [DOI] [PubMed] [Google Scholar]
- 237.Przybylski M. A review of the current research on the role of bFGF and VEGF in angiogenesis. J Wound Care. 2009;18:516–519. doi: 10.12968/jowc.2009.18.12.45609. [DOI] [PubMed] [Google Scholar]
- 238.Li JL, Harris AL. Crosstalk of VEGF and Notch pathways in tumour angiogenesis: Therapeutic implications. Front Biosci (Landmark Ed) 2009;14:3094–3110. doi: 10.2741/3438. [DOI] [PubMed] [Google Scholar]
- 239.Dimova I, Popivanov G, Djonov V. Angiogenesis in cancer-general pathways and their therapeutic implications. J BUON. 2014;19:15–21. [PubMed] [Google Scholar]
- 240.Phng LK, Gerhardt H. Angiogenesis: A team effort coordinated by notch. Dev Cell. 2009;16:196–208. doi: 10.1016/j.devcel.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 241.Benedito R, Roca C, Sörensen I, Adams S, Gossler A, Fruttiger M, Adams RH. The notch ligands Dll4 and Jagged1 have opposing effects on angiogenesis. Cell. 2009;137:1124–1135. doi: 10.1016/j.cell.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 242.Boas SE, Merks RM. Tip cell overtaking occurs as a side effect of sprouting in computational models of angiogenesis. BMC Syst Biol. 2015;9:86. doi: 10.1186/s12918-015-0230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Garcia-Pascual CM, Zimmermann RC, Ferrero H, Shawber CJ, Kitajewski J, Simón C, Pellicer A, Gomez R. Delta-like ligand 4 regulates vascular endothelial growth factor receptor 2-driven luteal angiogenesis through induction of a tip/stalk phenotype in proliferating endothelial cells. Fertil Steril. 2013;100:1768–1776.e1. doi: 10.1016/j.fertnstert.2013.08.034. [DOI] [PubMed] [Google Scholar]
- 244.Brzozowa M, Wojnicz R, Kowalczyk-Ziomek G, Helewski K. The Notch ligand Delta-like 4 (DLL4) as a target in angiogenesis-based cancer therapy? Contemp Oncol (Pozn) 2013;17:234–237. doi: 10.5114/wo.2013.35588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Fukuhara S, Sako K, Noda K, Zhang J, Minami M, Mochizuki N. Angiopoietin-1/Tie2 receptor signaling in vascular quiescence and angiogenesis. Histol Histopathol. 2010;25:387–396. doi: 10.14670/HH-25.387. [DOI] [PubMed] [Google Scholar]
- 246.Cao Y, Cao R, Hedlund EM. R Regulation of tumor angiogenesis and metastasis by FGF and PDGF signaling pathways. J Mol Med (Berl) 2008;86:785–789. doi: 10.1007/s00109-008-0337-z. [DOI] [PubMed] [Google Scholar]
- 247.van Meeteren LA, Goumans MJ, ten Dijke P. TGF-β receptor signaling pathways in angiogenesis; emerging targets for anti-angiogenesis therapy. Curr Pharm Biotechnol. 2011;12:2108–2120. doi: 10.2174/138920111798808338. [DOI] [PubMed] [Google Scholar]
- 248.Orlova VV, Liu Z, Goumans MJ, ten Dijke P. Controlling angiogenesis by two unique TGF-β type I receptor signaling pathways. Histol Histopathol. 2011;26:1219–1230. doi: 10.14670/HH-26.1219. [DOI] [PubMed] [Google Scholar]
- 249.Taniyama Y, Morishita R, Aoki M, Nakagami H, Yamamoto K, Yamazaki K, Matsumoto K, Nakamura T, Kaneda Y, Ogihara T. Therapeutic angiogenesis induced by human hepatocyte growth factor gene in rat and rabbit hindlimb ischemia models: Preclinical study for treatment of peripheral arterial disease. Gene Ther. 2001;8:181–189. doi: 10.1038/sj.gt.3301379. [DOI] [PubMed] [Google Scholar]
- 250.Wu L, Fu Z, Zhou S, Gong J, Liu CA, Qiao Z, Li S. HIF-12α and HIF-22α: Siblings in promoting angiogenesis of residual hepatocellular carcinoma after high-intensity focused ultrasound ablation. PLoS One. 2014;9:e88913. doi: 10.1371/journal.pone.0088913. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 251.Hayashi H, Kume T. Foxc transcription factors directly regulate Dll4 and Hey2 expression by interacting with the VEGF-Notch signaling pathways in endothelial cells. PLoS One. 2008;3:e2401. doi: 10.1371/journal.pone.0002401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Mitsuhashi N, Shimizu H, Ohtsuka M, Wakabayashi Y, Ito H, Kimura F, Yoshidome H, Kato A, Nukui Y, Miyazaki M. Angiopoietins and Tie-2 expression in angiogenesis and proliferation of human hepatocellular carcinoma. Hepatology. 2003;37:1105–1113. doi: 10.1053/jhep.2003.50204. [DOI] [PubMed] [Google Scholar]
- 253.Wulff C, Wilson H, Largue P, Duncan WC, Armstrong DG, Fraser HM. Angiogenesis in the human corpus luteum: Localization and changes in angiopoietins, tie-2 and vascular endothelial growth factor messenger ribonucleic acid. J Clin Endocrinol Metab. 2000;85:4302–4309. doi: 10.1210/jcem.85.11.6942. [DOI] [PubMed] [Google Scholar]
- 254.Weinmaster G. Notch signaling: Direct or what? Curr Opin Genet Dev. 1998;8:436–442. doi: 10.1016/S0959-437X(98)80115-9. [DOI] [PubMed] [Google Scholar]
- 255.Reizis B, Leder P. Direct induction of T lymphocyte-specific gene expression by the mammalian Notch signaling pathway. Genes Dev. 2002;16:295–300. doi: 10.1101/gad.960702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Nakano N, Nishiyama C, Yagita H, Hara M, Motomura Y, Kubo M, Okumura K, Ogawa H. Notch signaling enhances FcεRI-mediated cytokine production by mast cells through direct and indirect mechanisms. J Immunol. 2015;194:4535–4544. doi: 10.4049/jimmunol.1301850. [DOI] [PubMed] [Google Scholar]
- 257.Wüstehube J, Bartol A, Liebler SS, Brütsch R, Zhu Y, Felbor U, Sure U, Augustin HG, Fischer A. Cerebral cavernous malformation protein CCM1 inhibits sprouting angiogenesis by activating DELTA-NOTCH signaling. Proc Natl Acad Sci USA. 2010;107:12640–12645. doi: 10.1073/pnas.1000132107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.You C, Sandalcioglu IE, Dammann P, Felbor U, Sure U, Zhu Y. Loss of CCM3 impairs DLL4-Notch signalling: Implication in endothelial angiogenesis and in inherited cerebral cavernous malformations. J Cell Mol Med. 2013;17:407–418. doi: 10.1111/jcmm.12022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Patel NS, Li JL, Generali D, Poulsom R, Cranston DW, Harris AL. Up-regulation of delta-like 4 ligand in human tumor vasculature and the role of basal expression in endothelial cell function. Cancer Res. 2005;65:8690–8697. doi: 10.1158/0008-5472.CAN-05-1208. [DOI] [PubMed] [Google Scholar]
- 260.Rath S, Liebl J, Furst R, Vollmar AM, Zahler S. Regulation of endothelial signaling and migration by v-ATPase. Angiogenesis. 2014;17:587–601. doi: 10.1007/s10456-013-9408-z. [DOI] [PubMed] [Google Scholar]
- 261.Hernandez SL, Banerjee D, Garcia A, Kangsamaksin T, Cheng WY, Anastassiou D, Funahashi Y, Kadenhe-Chiweshe A, Shawber CJ, Kitajewski JK, et al. Notch and VEGF pathways play distinct but complementary roles in tumor angiogenesis. Vasc Cell. 2013;5:17. doi: 10.1186/2045-824X-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Jin Y, Kaluza D, Jakobsson L. VEGF, Notch and TGFβ/BM Ps in regulation of sprouting angiogenesis and vascular patterning. Biochem Soc Trans. 2014;42:1576–1583. doi: 10.1042/BST20140231. [DOI] [PubMed] [Google Scholar]
- 263.Chintala H, Krupska I, Yan L, Lau L, Grant M, Chaqour B. The matricellular protein CCN1 controls retinal angiogenesis by targeting VEGF, Src homology 2 domain phosphatase-1 and Notch signaling. Development. 2015;142:2364–2374. doi: 10.1242/dev.121913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Kiec-Wilk B, Grzybowska-Galuszka J, Polus A, Pryjma J, Knapp A, Kristiansen K. The MAPK-dependent regulation of the Jagged/Notch gene expression by VEGF, bFGF or PPAR gamma mediated angiogenesis in HUVEC. J Physiol Pharmacol. 2010;61:217–225. [PubMed] [Google Scholar]
- 265.Cao L, Arany PR, Wang YS, Mooney DJ. Promoting angio-genesis via manipulation of VEGF responsiveness with notch signaling. Biomaterials. 2009;30:4085–4093. doi: 10.1016/j.biomaterials.2009.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Thurston G, Kitajewski J. VEGF and Delta-Notch: Interacting signalling pathways in tumour angiogenesis. Br J Cancer. 2008;99:1204–1209. doi: 10.1038/sj.bjc.6604484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Zechariah A, ElAli A, Doeppner TR, Jin F, Hasan MR, Helfrich I, Mies G, Hermann DM. Vascular endothelial growth factor promotes pericyte coverage of brain capillaries, improves cerebral blood flow during subsequent focal cerebral ischemia, and preserves the metabolic penumbra. Stroke. 2013;44:1690–1697. doi: 10.1161/STROKEAHA.111.000240. [DOI] [PubMed] [Google Scholar]
- 268.Yang JP, Liu HJ, Liu XF. VEGF promotes angiogenesis and functional recovery in stroke rats. J Invest Surg. 2010;23:149–155. doi: 10.3109/08941930903469482. [DOI] [PubMed] [Google Scholar]
- 269.Dzietko M, Derugin N, Wendland MF, Vexler ZS, Ferriero DM. Delayed VEGF treatment enhances angiogenesis and recovery after neonatal focal rodent stroke. Transl Stroke Res. 2013;4:189–200. doi: 10.1007/s12975-012-0221-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Lee HJ, Kim KS, Park IH, Kim SU. Human neural stem cells over-expressing VEGF provide neuroprotection, angiogenesis and functional recovery in mouse stroke model. PLoS One. 2007;2:e156. doi: 10.1371/journal.pone.0000156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Esposito E, Hayakawa K, Maki T, Arai K, Lo EH. Effects of postconditioning on neurogenesis and angiogenesis during the recovery phase after focal cerebral ischemia. Stroke. 2015;46:2691–2694. doi: 10.1161/STROKEAHA.115.009070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Oh TW, Park KH, Jung HW, Park YK. Neuroprotective effect of the hairy root extract of Angelica gigas NAKAI on transient focal cerebral ischemia in rats through the regulation of angiogenesis. BMC Complement Altern Med. 2015;15:101. doi: 10.1186/s12906-015-0589-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Duan S, Shao G, Yu L, Ren C. Angiogenesis contributes to the neuroprotection induced by hyperbaric oxygen preconditioning against focal cerebral ischemia in rats. Int J Neurosci. 2015;125:625–634. doi: 10.3109/00207454.2014.956101. [DOI] [PubMed] [Google Scholar]
- 274.Hayward NM, Yanev P, Haapasalo A, Miettinen R, Hiltunen M, Grohn O, Jolkkonen J. Chronic hyperperfusion and angiogenesis follow subacute hypoperfusion in the thalamus of rats with focal cerebral ischemia. J Cereb Blood Flow Metab. 2011;31:1119–1132. doi: 10.1038/jcbfm.2010.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Guo F, Lv S, Lou Y, Tu W, Liao W, Wang Y, Deng Z. Bone marrow stromal cells enhance the angiogenesis in ischaemic cortex after stroke: Involvement of notch signalling. Cell Biol Int. 2012;36:997–1004. doi: 10.1042/CBI20110596. [DOI] [PubMed] [Google Scholar]
- 276.Dao M, Tate CC, McGrogan M, Case CC. Comparing the angiogenic potency of naïve marrow stromal cells and Notch-transfected marrow stromal cells. J Transl Med. 2013;11:81. doi: 10.1186/1479-5876-11-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Lähteenvuo JE, Lähteenvuo MT, Kivelä A, Rosenlew C, Falkevall A, Klar J, Heikura T, Rissanen TT, Vähakängas E, Korpisalo P, et al. Vascular endothelial growth factor-B induces myocardium-specific angiogenesis and arteriogenesis via vascular endothelial growth factor receptor-1- and neuropilin receptor-1-dependent mechanisms. Circulation. 2009;119:845–856. doi: 10.1161/CIRCULATIONAHA.108.816454. [DOI] [PubMed] [Google Scholar]
- 278.Semenza GL. Vasculogenesis, angiogenesis, and arteriogenesis: Mechanisms of blood vessel formation and remodeling. J Cell Biochem. 2007;102:840–847. doi: 10.1002/jcb.21523. [DOI] [PubMed] [Google Scholar]
- 279.Carmeliet P. Mechanisms of angiogenesis and arteriogenesis. Nat Med. 2000;6:389–395. doi: 10.1038/74651. [DOI] [PubMed] [Google Scholar]
- 280.Buschmann I, Schaper W. Arteriogenesis Versus Angiogenesis: Two Mechanisms of Vessel Growth. News Physiol Sci. 1999;14:121–125. doi: 10.1152/physiologyonline.1999.14.3.121. [DOI] [PubMed] [Google Scholar]
- 281.Rangarajan A, Talora C, Okuyama R, Nicolas M, Mammucari C, Oh H, Aster JC, Krishna S, Metzger D, Chambon P, et al. Notch signaling is a direct determinant of keratinocyte growth arrest and entry into differentiation. EMBO J. 2001;20:3427–3436. doi: 10.1093/emboj/20.13.3427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Gunaratne A, Chan E, El-Chabib TH, Carter D, Di Guglielmo GM. aPKC alters the TGFβ response in NSCLC cells through both Smad-dependent and Smad-independent pathways. J Cell Sci. 2015;128:487–498. doi: 10.1242/jcs.155440. [DOI] [PubMed] [Google Scholar]
- 283.Wang Y, Pan L, Moens CB, Appel B. Notch3 establishes brain vascular integrity by regulating pericyte number. Development. 2014;141:307–317. doi: 10.1242/dev.096107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Blasi F, Wei Y, Balkaya M, Tikka S, Mandeville JB, Waeber C, Ayata C, Moskowitz MA. Recognition memory impairments after subcortical white matter stroke in mice. Stroke. 2014;45:1468–1473. doi: 10.1161/STROKEAHA.114.005324. [DOI] [PubMed] [Google Scholar]
- 285.Yao H, Duan M, Hu G, Buch S. Platelet-derived growth factor B chain is a novel target gene of cocaine-mediated Notch1 signaling: Implications for HIV-associated neurological disorders. J Neurosci. 2011;31:12449–12454. doi: 10.1523/JNEUROSCI.2330-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Manda VK, Mittapalli RK, Geldenhuys WJ, Lockman PR. Chronic exposure to nicotine and saquinavir decreases endothelial Notch-4 expression and disrupts blood-brain barrier integrity. J Neurochem. 2010;115:515–525. doi: 10.1111/j.1471-4159.2010.06948.x. [DOI] [PubMed] [Google Scholar]
- 287.Nakatsu MN, Sainson RC, Aoto JN, Taylor KL, Aitkenhead M, Pérez-del-Pulgar S, Carpenter PM, Hughes CC. Angiogenic sprouting and capillary lumen formation modeled by human umbilical vein endothelial cells (HUVEC) in fibrin gels: The role of fibroblasts and Angiopoietin-1. Microvasc Res. 2003;66:102–112. doi: 10.1016/S0026-2862(03)00045-1. [DOI] [PubMed] [Google Scholar]
- 288.Li Z, Wang J, Zhao C, Ren K, Xia Z, Yu H, Jiang K. Acute Blockage of Notch signaling by DAPT induces neuroprotection and Neurogenesis in the Neonatal rat brain after stroke. Transl Stroke Res. 2016;7:132–140. doi: 10.1007/s12975-015-0441-7. [DOI] [PubMed] [Google Scholar]
- 289.Marumo T, Takagi Y, Muraki K, Hashimoto N, Miyamoto S, Tanigaki K. Notch signaling regulates nucleocytoplasmic Olig2 translocation in reactive astrocytes differentiation after ischemic stroke. Neurosci Res. 2013;75:204–209. doi: 10.1016/j.neures.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 290.Shimada IS, Borders A, Aronshtam A, Spees JL. Proliferating reactive astrocytes are regulated by Notch-1 in the peri-infarct area after stroke. Stroke. 2011;42:3231–3237. doi: 10.1161/STROKEAHA.111.623280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Uyttendaele H, Closson V, Wu G, Roux F, Weinmaster G, Kitajewski J. Notch4 and Jagged-1 induce microvessel differentiation of rat brain endothelial cells. Microvasc Res. 2000;60:91–103. doi: 10.1006/mvre.2000.2254. [DOI] [PubMed] [Google Scholar]
- 292.Xiao MJ, Han Z, Shao B, Jin K. Notch signaling and neuro-genesis in normal and stroke brain. Int J Physiol Pathophysiol Pharmacol. 2009;1:192–202. [PMC free article] [PubMed] [Google Scholar]
- 293.Carlén M, Meletis K, Göritz C, Darsalia V, Evergren E, Tanigaki K, Amendola M, Barnabe-Heider F, Yeung MS, Naldini L, et al. Forebrain ependymal cells are Notch-dependent and generate neuroblasts and astrocytes after stroke. Nat Neurosci. 2009;12:259–267. doi: 10.1038/nn.2268. [DOI] [PubMed] [Google Scholar]
- 294.Yang T, Liu LY, Ma YY, Zhang W. Notch signaling-mediated neural lineage selection facilitates intrastriatal transplantation therapy for ischemic stroke by promoting endogenous regeneration in the hippocampus. Cell Transplant. 2014;23:221–238. doi: 10.3727/096368912X661355. [DOI] [PubMed] [Google Scholar]
- 295.Yasuhara T, Matsukawa N, Hara K, Maki M, Ali MM, Yu SJ, Bae E, Yu G, Xu L, McGrogan M, et al. Notch-induced rat and human bone marrow stromal cell grafts reduce ischemic cell loss and ameliorate behavioral deficits in chronic stroke animals. Stem Cells Dev. 2009;18:1501–1514. doi: 10.1089/scd.2009.0011. [DOI] [PubMed] [Google Scholar]