Abstract
Background
Irritable bowel syndrome (IBS) is a common abdominal pain disorder without an organic explanation. Abuse histories (physical, sexual, emotional) are prevalent in IBS. While abuse relates to mood disorders (depression and anxiety) also common in IBS, the influence of abuse on GI symptoms and health-related quality of life (HRQOL) and its independence from psychological symptom comorbidity, has not been studied.
Methods
Consecutive GI outpatients completed the ROME III Research Diagnostic Questionnaire and questionnaires on trauma (Life-Stress Questionnaire), mood (Beck Depression/Anxiety Inventories), somatic symptoms (PHQ-12) and HRQOL (SF-36). Current GI symptom Severity and Bother were assessed using 10-cm VAS scales.
Key Results
272 ROME-defined IBS (47.6±0.9 yrs, 81% female) and 246 non-FGID (51.6±1.0 yrs, 65% female) subjects participated. IBS patients reported greater rates of physical, sexual, and emotional abuse (p < 0.006 each), and higher depression, anxiety, and somatic symptoms (p < 0.001). Greater bowel symptom bother (7.4±0.2 vs 6.7±0.2, p=0.040), severity (7.7±0.2 vs 6.5±0.2, p<0.001), recent symptomatic days (9.8±0.4 vs. 8.5±0.3, p=0.02), and poorer HRQOL (40.9±2.3 vs 55.5±1.7, p<0.001) were noted in IBS with abuse. Abuse effects were additive, with greater IBS symptom severity and poorer HRQOL noted in cases with multiple forms of abuse. Mediation analyses suggested that abuse effects on GI symptoms and HRQOL were partially mediated by mood.
Conclusions & Inferences
Abuse experiences common among IBS sufferers are associated with reports of greater GI symptoms and poorer HRQOL, particularly in those with multiple forms of abuse; this relationship may be partially mediated by concomitant mood disturbances.
Keywords: irritable bowel syndrome, abuse, depression, health-related quality of life
Graphical abstract
We studied the relationship of GI and mood symptoms among IBS patients with- and without abuse histories. IBS patients with abuse experiences had more severe abdominal pain and illness-related disability, an effect partially mediated by comorbid mood. Multiple abuse experiences exerted negative effects on IBS symptoms and health-related quality of life in an additive fashion.
Introduction
Traumatic life experiences, and more particularly abuse (physical, sexual, and/or emotional) unfortunately occur frequently, and are well recognized as factors associated with the development of functional GI disorders (FGIDs), including irritable bowel syndrome (IBS). A recent review revealed that rates of physical, emotional and sexual abuse all are substantially higher among IBS patients compared to the general population (1-3). Further, it has been suggested that abuse experiences among patients with GI conditions lead to greater pain, poorer daily function, and more reports of extraintestinal symptoms (e.g., palpitations, headache, fatigue) (4, 5). While abuse experiences do not appear to be more common to one IBS subtype (i.e. diarrheal-predominant compared to constipation-predominant IBS) (6), the effect of abuse on the non-pain symptoms prototypical to IBS, such as diarrhea, constipation, and bloating, remain less well-understood.
Patients with FGIDs have high rates of lifetime psychiatric illnesses; and, the abuse experiences common to these patients impose an even greater risk for the development of psychiatric disorders, such as major depressive disorder (MDD), generalized anxiety, post-traumatic stress disorder (PTSD) (7-10). Similarly, abuse and trauma histories predict more severe and disabling mood symptoms (11-13). Substantial evidence further suggests that IBS patients with coexisting psychological difficulties suffer severe forms of disease and are less responsive to current standards of treatment (14).
Although individual relationships between abuse, psychological functioning, and IBS have been described, the interplay between these factors in the expression of IBS symptoms remains uncertain. It has been shown that early adverse life events have some association with IBS diagnoses, and indeed that this relationship is independent of psychological measures (6); however, the interactive effects of these factors on IBS symptoms, and on health-related quality of life (HRQOL) have yet to be explored. Further, some proportion of patients with IBS patients have suffered multiple forms of abuse; the potential additive effect of this complex trauma on their symptom experiences and well-being is also under-examined.
This study thus was performed to better delineate the relationship of abuse and mood in the expression IBS symptoms and HRQOL. We primarily sought to answer the following two questions: 1) Is the effect of abuse on IBS symptoms and HRQOL independent of comorbid mood or somatic symptoms? And, 2) Do experiences of multiple forms of abuse experiences exert additive effects on IBS symptoms and HRQOL?
Materials and Methods
This study was approved by the Washington University Institutional Review Board, and all subjects signed a written informed consent prior to study procedures.
Subjects and Clinical Characteristics
272 IBS and 246 non-FGID patients were enrolled for this study at Washington University in St. Louis from April 2009 – March 2013 from our outpatient gastroenterology office. Patients considered for inclusion in the IBS cohort were required to meet a clinical diagnosis of IBS and also meet Rome criteria for the disorder. Conversely, the non-FGID patients carried non-FGID diagnoses, and did not meet Rome criteria for IBS. The most common diagnoses among the non-FGID cohort included: GERD/non-cardiac chest pain (n=56, 22.7%), colorectal cancer screening/polyp history (n=29, 11.8%), dysphagia (n=17, 6.9%), esophageal motility disorder/achalasia (n=15, 6.1%), ulcerative colitis (n=13, 5.3%), chronic constipation (n=11, 4.5%), and gastroparesis (n=10, 4.1%). Patients were excluded if unable to provide consent, refused to completed questionnaires, or were unable to speak and read English. Psychiatric diagnoses were permitted in participants as we sought to examine the influence of abuse experiences in the context of these mood factors, commonly comorbid in FGID patients. We administered multi-dimensional questionnaires to patients who presented at our outpatient GI clinics:
Gastrointestinal symptom assessment
These questionnaires included ROME III diagnostic questionnaires (15) to confirm the diagnosis of IBS. Gastrointestinal symptoms within 2 weeks prior to enrollment were assessed in terms of severity, bother, and frequency. Visual analogue scales (VAS; 10 cm) were used to assess severity and bother of symptoms via questions, “How much have you been bothered overall by your gastrointestinal symptoms over the preceding two weeks,” (0 = “not bothered at all,” 10 = “extremely bothered”) and, “When you have your gastrointestinal symptoms, how severe are they?” (0 = “not severe at all,” 10 = “extremely severe”). Frequency of symptoms in the preceding 2 weeks was noted; specific IBS symptom severity was graded on the Gastrointestinal Symptom Rating Scale for IBS (GSRS-IBS) (16). As we have demonstrated previously, VAS symptom severity scores correlate significantly with other disease-specific instruments such as the (GSRS-IBS) (Pearson r=0.52, p < 0.0001) (17-19).
Psychological symptom measures
Standardized and widely used questionnaires were used to assess degree of self-reported anxiety (Beck Anxiety Inventory, BAI (20)) and depression (Beck Depression Inventory, BDI) (21). Both questionnaires consist of 21 multiple choice questions assessing the degree of symptoms in the past week. Cutoffs of BDI≥20 and BAI≥16 were used as clinical correlates of at least “moderate to severe” mood disturbance based on the literature (22, 23).
Early Life Stressor Questionnaire
The ELSQ assessed the type of abuse, age at onset and duration of abuse experiences (24). Patients were asked questions about types and dates/ages of emotional, physical, and sexual abuse occurrences. “Early abuse” was regarded as experiences that occurred before the age of 17.
Somatic symptom severity
The PHQ-15 (25) is a validated questionnaire focusing on 15 commonly expressed somatic symptoms lacking medical explanation. Patients are asked to rate the bother for each specific symptom with multiple choices being, “Not bothered at all,” “Bothered a little,” or “Bothered a lot.” High scores on the PHQ-15 strongly correlate with DSMIV diagnosis of somatization disorder, although for diagnostic purposes patients need to be seen by a physician to exclude organic explanation for symptoms. Albeit in non-GI populations, a PHQ-15 cutoff of 15 has been proposed to represent “high somatic symptom severity” (25). The standardized PHQ-12 (26) questionnaire excludes the three GI symptoms (“stomach pain,” “constipation, loose bowels, or diarrhea,” and “nausea, gas, or indigestion”) from the PHQ-15. The PHQ-12 allows for assessment of the interplay of somatic symptom severity and GI symptoms in an FGID patient population (19).
Health Related Quality of Life (HRQOL)
Health related quality of life was measured by the (short form) SF-36 (27). This instrument assesses the perception of one's own health and well-being and also provides a measure of how the illness is affecting patients’ physical, emotional and social functioning. Higher scores are reflective of better health. It can be further used to sub-analyze a physical component, measuring illness-limited physical activities, and a mental health component, measuring illness impact on psychological well-being.
Statistical analysis
Grouped values are reported as mean ± standard error of mean, unless otherwise indicated. Between-group comparisons were performed using Student's t-tests, and chi-square tests were performed for binomial data as appropriate. In each case, p < 0.05 was required for statistical significance. Multiple linear regression models were developed using the ‘stepwise method’ wherein predictor variables were entered into the regression equation one at a time, prioritized by which independent variable contributed the most to the prediction equation in terms of increasing the multiple correlation, R (28, 29). This process was continued until no additional a priori predictor variables add further statistical meaning to the regression equation. These models were used to establish the independent contributions of abuse, psychological comorbidities (depression, anxiety, somatic symptoms), and demographics (gender, age) on bowel symptom burden (symptom severity, pain, IBS subtype) and HRQOL scores in IBS patients. Further, we explored whether IBS symptom severity and HRQOL is mediated in part by the presence of mood symptoms in the IBS with abuse population, using the continuous mood measures. The percentage of predictable variation for each variable in the model was calculated as the percentage of the total variation in the dependent variable explained by the model (R2) accounted for by a particular independent variable in the model, or [(variable partial R2/model R2)*100].
Symptom burden (severity) scores were available in the vast majority of patients in each group and the percentages available were similar between groups (93.1% non-FGID, 94.9% IBS). SF-36 scores were not recorded in 15 patients (3 IBS and 12 non-FGID). Psychological (depression, anxiety, and somatic symptom severity) measures were available for all patients, and percentages completed across groups were similar (100% for both groups on BDI and BAI; 88.2% IBS, 85.8% non-FGID on PHQ-12).
Sobel mediation analyses explored whether any effect of abuse on IBS symptom severity and HRQOL in IBS patients might be partially mediated by psychological symptoms. These mediation analyses were carried out with the psychological symptoms (anxiety, depression, and somatic symptom measures) both individually and collectively considered as a latent variable (“Psych symptoms”). Sobel statistics were then calculated as described by Baron and Kenny (30). Preconditionally, all of the variables to be included in mediation analyses were required to be significantly correlated using two-tailed Pearson correlations. Given the high co-linearity between GI symptom severity, symptom bother and symptomatic days for IBS subjects, only symptom severity was implemented as the primary measure of recent GI symptoms, as performed previously (19). All of the reported statistical analyses were carried out using SPSS Statistics v.22 (IBM, Armonk, NY, USA) and exploratory factor analysis was performed in SPSS AMOS v 23.0, Wexford, PA).
Results
Baseline demographics and clinical characteristics
The average age of our study population was 49.4 ± 0.9 years, with a female predominance, particularly among in the IBS group. Severity of symptoms was significantly higher in the IBS compared to the non-FGID group (p < 0.001); bother and frequency were significantly higher in the IBS group compared to the non-IBS group (both at p < 0.001). IBS symptoms (pain, bloating, constipation, diarrhea) assessed on the GSRS scale were also significantly higher in IBS (Table 1).
Table 1.
Demographics and GI, psychological, and quality of life measures
| IBS (n=272) | Non-FGID (n=246) | p-value | |
|---|---|---|---|
| Demographics | |||
| Age (yrs) | 47.6 ±0.9 | 51.6 ± 1.0 | 0.003 |
| Female sex (%) | 221 (81) | 161 (65) | <0.001 |
| GI Symptoms | |||
| Bowel symptom bother (VAS) | 6.9 ± 0.2 | 4.1 ± 0.2 | <0.001 |
| Bowel symptom severity (VAS) | 6.9 ± 0.2 | 4.0 ± 0.2 | <0.001 |
| Bowel symptom frequency (days/last 2 wk) | 9.0 ± 0.3 | 5.2 ± 0.4 | <0.001 |
| GSRS-IBS | |||
| Pain subscale | 7.8 ± 0.2 | 4.5 ±0.2 | <0.001 |
| Bloating subscale | 10.3 ±0.3 | 6.4 ± 0.3 | <0.001 |
| Constipation subscale | 5.7 ±0.2 | 3.6 ±0.2 | <0.001 |
| Diarrhea subscale | 12.6 ±0.4 | 8.2 ±0.4 | <0.001 |
| Psychological measures (continuous) | |||
| Beck depression inventory [BDI] | 12.3 ± 0.6 | 7.8 ± 0.5 | <0.001 |
| Beck anxiety inventory [BAI] | 13.2 ±0.6 | 8.1 ±0.6 | <0.001 |
| Patient-Health Questionnaire-15 [PHQ-15] | 13.0 ± 0.3 | 9.4 ± 0.5 | <0.001 |
| Patient-Health Questionnaire-12 [PHQ-12]* | 8.5 ± 0.3 | 6.7 ± 0.4 | <0.001 |
| Psychological measures (dichotomous) | |||
| Depression [BDI ≥20] (%) | 59 (22) | 26 (11) | 0.001 |
| Anxiety [BAI ≥16] (%) | 85 (31) | 34 (14) | <0.001 |
| Somatic Symptoms [PHQ-15 ≥15] (%) | 82 (30) | 30 (12) | <0.001 |
| Quality of life measures | |||
| SF-36 Total | 50.4 ± 1.4 | 63.8 ± 1.6 | <0.001 |
| SF-36 Physical | 44.5 ± 1.4 | 58.9 ± 1.7 | <0.001 |
| SF-36 Mental | 51.8 ± 1.5 | 63.5 ± 1.6 | <0.001 |
PHQ-12(26) questionnaire excludes three GI symptoms (“stomach pain,” “constipation, loose bowels, or diarrhea,” and “nausea, gas, or indigestion”) from the PHQ-15.
Degree of anxiety and depression measured by the BAI and BDI were higher in IBS vs non-FGID at p < 0.001. Somatic symptom severity as measured by the PHQ-15 and PHQ-12 was similarly higher in the IBS vs non-FGID group, both at p < 0.001. Higher PHQ-12 scores in the IBS group indicate that higher scores on the PHQ-15 were not completely driven by gastrointestinal symptoms (Table 1). The proportion of patients meeting criteria for moderate anxiety defined by BAI≥16 (31) and moderate depression defined by BDI≥20 (31) were significantly higher in the IBS population.
Health-related quality of life was significantly worse in IBS compared to the non-FGID population. This was the case with scores on both the mental component of the SF-36, and also the physical component scores. (Table 1).
Prevalence of abuse in IBS population versus non-FGID population
Prevalence of abuse was significantly higher in IBS vs non-FGID (35.0% vs 20.0%) at p < 0.001. Specific forms of abuse: physical (18.0% vs 6.5%), emotional (31.6 % vs 16.7%), and sexual (15.4% vs 7.3%) were also significantly higher in IBS vs non-FGID (Figure 1). Abuse experiences were more commonly reported among women compared to men, both in the overall study population (33.2% vs. 12.5%, p < 0.001) and in the IBS subgroup (38.9 vs. 17.6%, p = 0.004).
Figure 1.
Percentage of abuse in sample with and without IBS
Psychological symptom measures in IBS patients with and without history of abuse
Degree of depression and anxiety were significantly higher in IBS with abuse vs IBS with no abuse, p ≤ 0.001. Somatic symptom severity with PHQ-12 was also higher in IBS with abuse compared to IBS with no abuse, p = 0.003 (Table 2).
Table 2.
Demographics and GI, psychological, and quality of life in IBS patients by abuse history
| IBS no abuse (n=177) | IBS with abuse (n=95) | p-value | |
|---|---|---|---|
| Demographics | |||
| Age (yrs) | 48.9 ± 1.1 | 45.1 ± 1.4 | 0.045 |
| Female sex (%) | 135 (76.3) | 86 (90.5) | 0.010 |
| GI Symptoms | |||
| Bowel symptom bother (VAS) | 6.7 ± 0.2 | 7.4 ± 0.2 | 0.040 |
| Bowel symptom severity (VAS) | 6.5 ± 0.2 | 7.7 ± 0.2 | <0.001 |
| Bowel symptom frequency (days/last 2 wk) | 8.5 ± 0.3 | 9.8 ± 0.4 | 0.014 |
| GSRS-IBS | |||
| Pain subscale | 7.4 ± 0.3 | 8.6 ± 0.3 | 0.004 |
| Bloating subscale | 9.6 ± 0.4 | 11.6 ± 0.5 | 0.001 |
| Constipation subscale | 5.3 ± 0.3 | 6.5 ± 0.4 | 0.010 |
| Diarrhea subscale | 12.2 ± 0.5 | 13.3 ± 0.7 | 0.170 |
| Psychological measures (continuous) | |||
| Beck depression inventory [BDI] | 9.6 ± 0.6 | 17.4 ± 1.1 | <0.001 |
| Beck anxiety inventory [BAI] | 10.6 ± 0.6 | 18.0 ± 1.2 | <0.001 |
| Patient-Health Questionnaire-15 [PHQ-15] | 12.1 ± 0.4 | 14.5 ± 0.5 | 0.001 |
| Patient-Health Questionnaire-12 [PHQ-12]* | 7.8 ± 0.4 | 9.6 ± 0.5 | 0.003 |
| Psychological measures (dichotomous) | |||
| Depression [BDI ≥20] (%) | 22 (12.4) | 37 (38.9) | <0.001 |
| Anxiety [BAI ≥16] (%) | 38 (21.5) | 47 (49.5) | <0.001 |
| Somatic Symptoms [PHQ-15 ≥15] (%) | 42 (23.7) | 40 (42.1) | 0.008 |
| Quality of life measures | |||
| SF-36 Total | 55.4 ± 1.7 | 40.9 ± 2.3 | <0.001 |
| SF-36 Physical | 48.8 ± 1.7 | 36.4 ± 2.2 | <0.001 |
| SF-36 Mental | 57.2 ± 1.7 | 41.8 ± 2.4 | <0.001 |
PHQ-12(26) questionnaire excludes three GI symptoms (“stomach pain,” “constipation, loose bowels, or diarrhea,” and “nausea, gas, or indigestion”) from the PHQ-15.
Burden of gastrointestinal symptoms in IBS patients with and without history of abuse
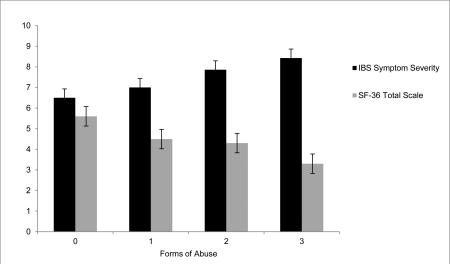
Gastrointestinal symptom severity, frequency and bother were significantly higher in the IBS group with abuse compared to no abuse (p ≤ 0.04 for each). Degree of pain, bloating, and constipation were all significantly (p ≤ 0.01) higher in IBS with abuse compared to IBS with no abuse, however, no difference was found in severity of diarrhea (Table 2, Figure 3). Overall, no difference was found based on age of abuse experiences, with the exception of reported bloating in those with a history of sexual abuse.
Figure 3.
Group statistics comparing means of the sample with IBS and abuse to IBS and no abuse.
*Denotes comparisons that are significant at p ≤ 0.05; **at p ≤ 0.001.
HRQOL in IBS patients with abuse versus no abuse
Health related quality of life was also significantly poorer in IBS with abuse compared to IBS group with no abuse (p < 0.001). As with the general IBS group, this difference in HRQOL was observed in both the mental and physical components of the SF-36 in IBS patients with abuse compared to those without abuse (Table 2).
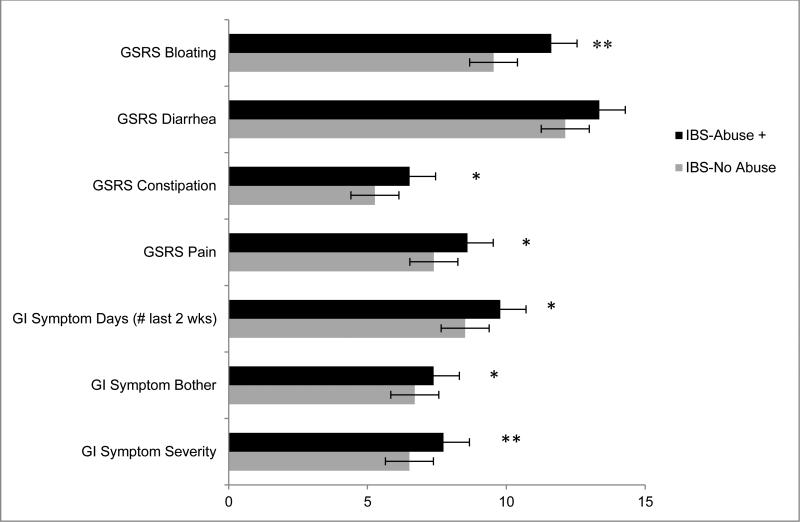
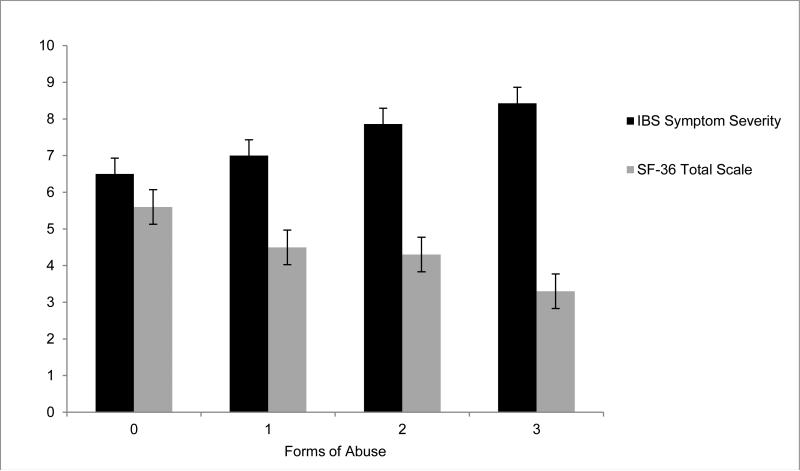
Effects of multiple forms of abuse on IBS symptom severity and HRQOL
Sub-analyses were performed to examine an effect of multiple forms of abuse, as 49% of those self-identifying as experiencing abuse indicated they had endured multiple abuse types (i.e. more than 1 form of physical, emotional, sexual). We first sought to isolate an effect on those who had suffered a single abuse type, which showed significant increase in IBS severity (F= 2.73, p < 0.05) and worse health-related quality of life (F= 3.24, p < 0.05). However, individual between abuse type t-tests were not significant in any case (all were p ≥ 0.06). Examining number of abuse forms, patients who experienced two or three forms of abuse had significantly poorer HRQOL compared to patients who experienced one or none, (p < 0.001). Similarly, patients who experienced higher rates of abuse had significantly more severe IBS symptoms compared to patients who experienced one or no forms of abuse, p < 0.001 (Figure 2).
Figure 2.
IBS severity compared with scaled health-related quality of life score across increasing number of forms of abuse.
Using multivariate models and controlling for demographic variables (i.e., age, gender), we found that within IBS patients, the experience of any form of abuse significantly influenced both severity of IBS symptoms and health related quality of life (overall model p < 0.001 for each, Supplemental Tables 1A and 2A). Further, when adding depression, anxiety, and somatic symptom severity to the experience of any form of abuse in these models, psychosomatic symptoms predicted severe IBS symptoms and HRQOL, with abuse no longer retaining statistical significance (overall model p < 0.001 each, Supplemental Tables 1B and 2B). Multivariate models also revealed that any abuse history significantly predicted more severe IBS pain, bloating, and constipation at p = 0.007, 0.003, and 0.024, respectively. Finally, to further investigate the significance that psychosomatic symptom severity has when modeling the effect of abuse on IBS symptomology and health-related outcomes, we performed mediation analysis using Sobel testing to assess relation between depression, anxiety, and somatic symptoms on IBS symptom severity and HRQOL in the setting of abuse. We found anxious (Z= 4.59) and depressive (Z= 4.67) symptoms partially mediated the effect of abuse on IBS symptom severity with p < 0.0001); somatic symptoms partially mediated abuse effects on IBS severity with p < 0.02 (Z= 2.52). Similarly, anxiety (Z= −5.64, p < 0.0001), depression (Z=−6.19, p < 0.0001), and somatic symptom severity (Z= −3.01, p < 0.005) also partially mediated the effect of abuse on HRQOL (Supplemental Figures 1A and 1B). Given the likely overlap of these psychological symptoms in the same individuals, we represented anxiety, depression, and somatic symptom severity (manifest variables) in a latent variable (‘Psych symptoms’), and repeated the mediation analyses exploring ‘Psych symptoms’ as an intermediate in the effect of abuse on IBS symptom severity and HRQOL. ‘Psych symptoms’ did indeed mediate abuse effects on both IBS symptoms and HRQOL, with anxiety and depression having greater influences (relative to somatic symptoms) on these dependent variables (Supplemental Tables 3A and 3B).
Discussion
In our study, we observed that abuse experiences among a tertiary center IBS population are much more common than in non-FGID subjects. Severity of depression, anxiety, and somatic symptoms all were higher in IBS patients with abuse histories compared to those without abuse experiences. In turn, IBS symptom severity, including bowel-specific symptoms, and health-related quality of life were found to be significantly worse in IBS patients with abuse histories. Additionally, our results indicate that individuals enduring multiple forms of abuse endorsed more severe IBS symptoms and lower HRQOL compared to those who had fewer or no abuse experiences. Previously, abuse has been demonstrated to be a predictor of increased rates of psychiatric illness, and further it is well established that mood disorders are more common in IBS (32-36); mediation analyses performed to explore the interplay of these factors in the current study indicated that depression, anxiety, and somatic symptoms partially mediate the effect of abuse on IBS symptom severity and HRQOL, with mood (anxiety/depression) symptoms perhaps having greater influences on IBS symptoms and HRQOL among individuals with multiple active psychological symptoms.
Abuse experiences are common in the general population; one in four adults self-report physical abuse experiences as a child, and one in five women report sexual abuse as a child (37). These experiences have lasting effects on the mental and physical health of the individual, with multiple studies previously having established a strong relationship between history of childhood abuse and development of IBS (38, 39). Indeed, prior work reported rates of abuse in IBS populations ranging from 30-50% (2, 40, 41). In line with previously published data, we report the rate of abuse experiences to be around 35% in our tertiary center IBS population. Our study IBS group also had similarly high detectable rates of depression, anxiety and somatic symptoms (over two-thirds of IBS patients were found to have least one of these mood-based factors), a rate of detection much higher than that observed in the non-FGID population (40%) (9, 10, 42). The Adverse Childhood Experience Study by Felitti et.al. (43) showed that patients with childhood abuse experiences are at 4-12 fold higher risk of developing depression, a finding supported by similar results in several other studies (41, 44, 45). In another meta-analysis of over 3000 subjects, patients with early life stressful events were found to have severe forms of psychiatric illness, with less favorable outcomes to treatment. (46) IBS patients with self-reported abuse in our study were observed to have more severe depression, anxiety, and somatic symptoms compared to their IBS counterparts with no abuse history. GI symptom severity, bother, and frequency accordingly were significantly higher in the IBS group with abuse compared to the group without any abuse, consistent with earlier studies (5, 14, 47). This observation did not appear to track with any single type of abuse experience in particular. With regard to specific bowel symptoms, we found that abdominal pain, constipation and bloating, but not diarrhea, were significantly more severe in the IBS with abuse histories. Importantly, patients with multiple forms of abuse were found to have significantly more severe IBS symptoms, exerting its deleterious effects in additive fashion. Furthermore, HRQOL was significantly lower in IBS patients with abuse histories compared to those without. Notably, both physical and mental components of the SF-36 were negatively affected in the IBS with abuse group. This observation implies that low HRQOL in IBS patients are not an effect of these comorbidities on mood alone, but appear more to globally influence physical well-being.
How might abuse experiences be linked mechanistically to greater IBS symptom severity and psychological distress in affected individuals? Neuroimaging studies conducted in the IBS and mood disorder population reveal that childhood trauma or abuse increases the hypothalamic-pituitary-adrenal axis activation and further is related to low volume of the hippocampus and anterior cingulate. These alterations in limbic circuitry among maltreated children (48) are consistently identified, and are strikingly similar to those seen in major depressive disorder (49); it has been suggested that these limbic structure abnormalities, particularly within the dorsal anterior cingulate cortex (dACC) and prefrontal cortex, are sufficiently specific for PTSD to be useful complements to the clinical diagnosis (49, 50). In neuroimaging studies on IBS, those subjects with abuse histories exhibit similar limbic structure changes (50-53) and report more severe symptoms and poorer outcomes in response to chronic pain symptoms (52). We speculate that abuse experiences may trigger derangements in these brain neurocircuits, resulting in enhanced emotional arousal responses to visceral afferent signals and alterations in mood (54); the latter may hold the potential to independently enhance pain symptom experiences (55), as was suggested by our exploratory mediation analyses. In a notable case report by Drossman et al. it was suggested that functional activations in these limbic structures can be modified following therapy, and indeed reflect clinical improvements in patients with a history of abuse and severe IBS (56). Further work is needed to objectively clarify the role of the limbic system in the common triad of abuse, psychological symptoms, and IBS.
This study is subject to the limitations of its cross-sectional design; specifically, we cannot establish causal relationships between abuse and IBS symptom severity or health-related quality of life. Many of the reported experiences of abuse occurred decades ago, leading to some potential for recall and self-report biases. The FGID cohort was, as expected, younger and predominantly female; these factors may have further influenced both recall and reporting of abuse experiences in this group. Also, we relied on self-report instruments rather than formal diagnoses to establish psychiatric/psychological symptom comorbidity. The exploratory analyses in the study modelled the interplay of abuse, psychological symptoms, and IBS as simple linear, unidirectional relationships; bidirectional effects (e.g., IBS symptoms resulting in greater feelings of anxiety) should be considered in future studies. While we examine mood as one potential intermediate in the relationship between abuse and IBS in this study, we further acknowledge that this relationship is complex, and it is probable that additional mechanisms mediate the effects of abuse on FGID symptoms as well. Finally, we note that not all of the control subjects in this study had active GI complaints—a small subset presented for colorectal cancer screening or polyp surveillance. Nevertheless, we feel that these limitations were outweighed by the strengths of the study, which included the study of a clinically-identified patient population, and the use of more advanced statistical methods to explore our hypotheses and generate areas for future research focus.
IBS is a complex symptom-based disorder, heterogeneous in presentation and likely deriving from a multitude of underlying pathophysiologic mechanisms. Paramount to the success of treatment is to differentiate the IBS patient based on pathophysiology, and to invoke target treatments which address factors potentially amplifying symptom experiences. The findings from this study, when placed in the context of the existing literature, emphasize the clinical and mechanistic relevance of abuse experiences in IBS as: 1) important predictors of symptom severity and poor health-related quality of life; 2) central to mood comorbidities common to the disorder, and 3) an indicator of an IBS subgroup wherein CNS derangements (e.g., limbic neurocircuitry) may be particularly salient. Abuse experiences become increasingly important to IBS in those who have suffered multiple forms of abuse, exerting additive effects on IBS symptoms and health-related quality of life outcomes. These observations should inspire additional work to clarify mechanistic relevance and therapeutic implications of abuse experiences in the IBS population.
Supplementary Material
Key Points.
■ Abuse experiences are important to IBS symptoms and health-related quality of life (HRQOL). We studied the relationship of GI and mood symptoms among IBS patients with-and without abuse histories.
■ IBS patients with abuse experiences had more severe abdominal pain and illness-related disability, an effect partially mediated by comorbid mood. Multiple abuse experiences exerted negative effects on IBS symptoms and HRQOL in an additive fashion.
■ These observations have both mechanistic and therapeutic implications in this IBS population.
Acknowledgments
Funding: This work was supported by NIH grant K23 DK84113 (GSS) and Washington University School of Medicine Mentors in Medicine (MiM) Program (BC).
Footnotes
Contributorship: NK & GS: study concept and design, data analysis and interpretation, drafting and revision of manuscript, study supervision; BC: data collection, manuscript revision; BG: data analysis and interpretation, drafting and revision of manuscript; KW & SB: study concept and design, data interpretation, drafting and revision of manuscript; CG: data interpretation, drafting and revision of manuscript. Dr. Sayuk is the guarantor of the article.
Presentation in preliminary form at the Digestive Diseases Week Scientific Meeting, Chicago, 2014
Disclosures: None of the authors have any conflicts of interest to report. No writing assistance was obtained.
References
- 1.Salmon P, Skaife K, Rhodes J. Abuse, dissociation, and somatization in irritable bowel syndrome: towards an explanatory model. Journal of behavioral medicine. 2003 Feb;26(1):1–18. doi: 10.1023/a:1021718304633. PubMed PMID: 12690943. [DOI] [PubMed] [Google Scholar]
- 2.Chitkara DK, van Tilburg MA, Blois-Martin N, Whitehead WE. Early life risk factors that contribute to irritable bowel syndrome in adults: a systematic review. The American journal of gastroenterology. 2008 Mar;103(3):765–74. doi: 10.1111/j.1572-0241.2007.01722.x. quiz 75. PubMed PMID: 18177446. Pubmed Central PMCID: 3856200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheung CW, Qiu Q, Choi SW, Moore B, Goucke R, Irwin M. Chronic opioid therapy for chronic non-cancer pain: a review and comparison of treatment guidelines. Pain physician. 2014 Sep-Oct;17(5):401–14. PubMed PMID: 25247898. [PubMed] [Google Scholar]
- 4.Leserman J, Li Z, Drossman DA, Hu YJ. Selected symptoms associated with sexual and physical abuse history among female patients with gastrointestinal disorders: the impact on subsequent health care visits. Psychological medicine. 1998 Mar;28(2):417–25. doi: 10.1017/s0033291797006508. PubMed PMID: 9572098. Epub 1998/05/08. eng. [DOI] [PubMed] [Google Scholar]
- 5.Drossman DA, Li Z, Leserman J, Toomey TC, Hu YJ. Health status by gastrointestinal diagnosis and abuse history. Gastroenterology. 1996 Apr;110(4):999–1007. doi: 10.1053/gast.1996.v110.pm8613034. PubMed PMID: 8613034. [DOI] [PubMed] [Google Scholar]
- 6.Bradford K, Shih W, Videlock EJ, Presson AP, Naliboff BD, Mayer EA, et al. Association between early adverse life events and irritable bowel syndrome. Clin Gastroenterol Hepatol. 2012 Apr;10(4):385–90. e1–3. doi: 10.1016/j.cgh.2011.12.018. PubMed PMID: 22178460. Pubmed Central PMCID: 3311761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tanaka Y, Kanazawa M, Fukudo S, Drossman DA. Biopsychosocial model of irritable bowel syndrome. Journal of neurogastroenterology and motility. 2011 Apr;17(2):131–9. doi: 10.5056/jnm.2011.17.2.131. PubMed PMID: 21602989. Pubmed Central PMCID: 3093004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olden KW, Drossman DA. Psychologic and psychiatric aspects of gastrointestinal disease. The Medical clinics of North America. 2000 Sep;84(5):1313–27. doi: 10.1016/s0025-7125(05)70288-1. PubMed PMID: 11026930. [DOI] [PubMed] [Google Scholar]
- 9.Sayuk GS, Elwing JE, Lustman PJ, Clouse RE. High somatic symptom burdens and functional gastrointestinal disorders. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2007 May;5(5):556–62. doi: 10.1016/j.cgh.2006.11.024. PubMed PMID: 17258513. [DOI] [PubMed] [Google Scholar]
- 10.Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology. 2002 Apr;122(4):1140–56. doi: 10.1053/gast.2002.32392. PubMed PMID: 11910364. [DOI] [PubMed] [Google Scholar]
- 11.Chu DA, Williams LM, Harris AW, Bryant RA, Gatt JM. Early life trauma predicts selfreported levels of depressive and anxiety symptoms in nonclinical community adults: relative contributions of early life stressor types and adult trauma exposure. Journal of psychiatric research. 2013 Jan;47(1):23–32. doi: 10.1016/j.jpsychires.2012.08.006. PubMed PMID: 23020924. Epub 2012/10/02. eng. [DOI] [PubMed] [Google Scholar]
- 12.Heim C, Newport DJ, Mletzko T, Miller AH, Nemeroff CB. The link between childhood trauma and depression: insights from HPA axis studies in humans. Psychoneuroendocrinology. 2008 Jul;33(6):693–710. doi: 10.1016/j.psyneuen.2008.03.008. PubMed PMID: 18602762. [DOI] [PubMed] [Google Scholar]
- 13.Briere J, Kaltman S, Green BL. Accumulated childhood trauma and symptom complexity. Journal of traumatic stress. 2008 Apr;21(2):223–6. doi: 10.1002/jts.20317. PubMed PMID: 18404627. Epub 2008/04/12. eng. [DOI] [PubMed] [Google Scholar]
- 14.Drossman DA. Do psychosocial factors define symptom severity and patient status in irritable bowel syndrome? The American journal of medicine. 1999 Nov 8;107(5A):41S–50S. doi: 10.1016/s0002-9343(99)00081-9. PubMed PMID: 10588172. Epub 1999/12/10. eng. [DOI] [PubMed] [Google Scholar]
- 15.Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006 Apr;130(5):1377–90. doi: 10.1053/j.gastro.2006.03.008. PubMed PMID: 16678553. [DOI] [PubMed] [Google Scholar]
- 16.Wiklund IK, Fullerton S, Hawkey CJ, Jones RH, Longstreth GF, Mayer EA, et al. An irritable bowel syndrome-specific symptom questionnaire: development and validation. Scand J Gastroenterol. 2003 Sep;38(9):947–54. doi: 10.1080/00365520310004209. PubMed PMID: 14531531. Epub 2003/10/09. eng. [DOI] [PubMed] [Google Scholar]
- 17.Svedlund J, Sjodin I, Dotevall G. GSRS--a clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Digestive diseases and sciences. 1988 Feb;33(2):129–34. doi: 10.1007/BF01535722. PubMed PMID: 3123181. [DOI] [PubMed] [Google Scholar]
- 18.Bengtsson M, Ohlsson B, Ulander K. Development and psychometric testing of the Visual Analogue Scale for Irritable Bowel Syndrome (VAS-IBS). BMC gastroenterology. 2007;7:16. doi: 10.1186/1471-230X-7-16. PubMed PMID: 17475020. Pubmed Central PMCID: 1868742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vu J, Kushnir V, Cassell B, Gyawali CP, Sayuk GS. The impact of psychiatric and extraintestinal comorbidity on quality of life and bowel symptom burden in functional GI disorders. Neurogastroenterol Motil. 2014 Sep;26(9):1323–32. doi: 10.1111/nmo.12396. PubMed PMID: 25070610. [DOI] [PubMed] [Google Scholar]
- 20.Beck AT, Steer RA. Beck Anxiety Inventory Manual. Psychological Corporation; San Antonio, TX: 1993. [Google Scholar]
- 21.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of general psychiatry. 1961;4(6):561. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 22.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988 Dec;56(6):893–7. doi: 10.1037//0022-006x.56.6.893. PubMed PMID: 3204199. [DOI] [PubMed] [Google Scholar]
- 23.Beck AT, Steer RA. Psychometric Properties of the Beck Depression Inventory:Twenty-five Years of Evaluation. Clin Psych Rev. 1988;8:77–100. [Google Scholar]
- 24.Cohen RA, Hitsman BL, Paul RH, McCaffery J, Stroud L, Sweet L, et al. Early life stress and adult emotional experience: an international perspective. International journal of psychiatry in medicine. 2006;36(1):35–52. doi: 10.2190/5R62-9PQY-0NEL-TLPA. PubMed PMID: 16927577. [DOI] [PubMed] [Google Scholar]
- 25.Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002 Mar-Apr;64(2):258–66. doi: 10.1097/00006842-200203000-00008. PubMed PMID: 11914441. [DOI] [PubMed] [Google Scholar]
- 26.Spiller RC, Humes DJ, Campbell E, Hastings M, Neal KR, Dukes GE, et al. The Patient Health Questionnaire 12 Somatic Symptom scale as a predictor of symptom severity and consulting behaviour in patients with irritable bowel syndrome and symptomatic diverticular disease. Aliment Pharmacol Ther. 2010 Sep;32(6):811–20. doi: 10.1111/j.1365-2036.2010.04402.x. PubMed PMID: 20629976. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE, Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical care. 1992 Jun;30(6):473–83. PubMed PMID: 1593914. [PubMed] [Google Scholar]
- 28.Draper NR, Smith H. Applied Regression Analysis. John Wiley and Sons; New York, N.Y.: 1981. [Google Scholar]
- 29.McCullagh P, Nelder JA. Generalized Linear Models. 2nd ed Chapman and Hall/CRC; 1989. [Google Scholar]
- 30.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986 Dec;51(6):1173–82. doi: 10.1037//0022-3514.51.6.1173. PubMed PMID: 3806354. Epub 1986/12/01. eng. [DOI] [PubMed] [Google Scholar]
- 31.Steer RA, Clark DA, Beck AT, Ranieri WF. Common and specific dimensions of self-reported anxiety and depression: the BDI-II versus the BDI-IA. Behav Res Ther. 1999 Feb;37(2):183–90. doi: 10.1016/s0005-7967(98)00087-4. PubMed PMID: 9990749. [DOI] [PubMed] [Google Scholar]
- 32.Levy RL, Olden KW, Naliboff BD, Bradley LA, Francisconi C, Drossman DA, et al. Psychosocial aspects of the functional gastrointestinal disorders. Gastroenterology. 2006 Apr;130(5):1447–58. doi: 10.1053/j.gastro.2005.11.057. PubMed PMID: 16678558. [DOI] [PubMed] [Google Scholar]
- 33.McCauley J, Kern DE, Kolodner K, Dill L, Schroeder AF, DeChant HK, et al. Clinical characteristics of women with a history of childhood abuse: unhealed wounds. Jama. 1997 May 7;277(17):1362–8. PubMed PMID: 9134941. [PubMed] [Google Scholar]
- 34.Talley NJ, Fett SL, Zinsmeister AR, Melton LJ., 3rd. Gastrointestinal tract symptoms and selfreported abuse: a population-based study. Gastroenterology. 1994 Oct;107(4):1040–9. doi: 10.1016/0016-5085(94)90228-3. PubMed PMID: 7926457. [DOI] [PubMed] [Google Scholar]
- 35.Walker EA, Gelfand A, Katon WJ, Koss MP, Von Korff M, Bernstein D, et al. Adult health status of women with histories of childhood abuse and neglect. Am J Med. 1999 Oct;107(4):332–9. doi: 10.1016/s0002-9343(99)00235-1. PubMed PMID: 10527034. Epub 1999/10/20. eng. [DOI] [PubMed] [Google Scholar]
- 36.Koloski NA, Talley NJ, Boyce PM. Predictors of health care seeking for irritable bowel syndrome and nonulcer dyspepsia: a critical review of the literature on symptom and psychosocial factors. Am J Gastroenterol. 2001 May;96(5):1340–9. doi: 10.1111/j.1572-0241.2001.03789.x. PubMed PMID: 11374666. [DOI] [PubMed] [Google Scholar]
- 37.World Health Organization . Global status report on violence prevention. World Health Organization; Geneva: 2014. [Google Scholar]
- 38.Beesley H, Rhodes J, Salmon P. Anger and childhood sexual abuse are independently associated with irritable bowel syndrome. British journal of health psychology. 2010 May;15(Pt 2):389–99. doi: 10.1348/135910709X466496. PubMed PMID: 19691916. Epub 2009/08/21. eng. [DOI] [PubMed] [Google Scholar]
- 39.Heitkemper MM, Cain KC, Burr RL, Jun SE, Jarrett ME. Is childhood abuse or neglect associated with symptom reports and physiological measures in women with irritable bowel syndrome? Biological research for nursing. 2011 Oct;13(4):399–408. doi: 10.1177/1099800410393274. PubMed PMID: 21196423. Pubmed Central PMCID: 3569490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Drossman DA. Irritable bowel syndrome and sexual/physical abuse history. European journal of gastroenterology & hepatology. 1997 Apr;9(4):327–30. doi: 10.1097/00042737-199704000-00002. PubMed PMID: 9160192. Epub 1997/04/01. eng. [DOI] [PubMed] [Google Scholar]
- 41.Teicher MH, Samson JA. Childhood maltreatment and psychopathology: A case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. The American journal of psychiatry. 2013 Oct;170(10):1114–33. doi: 10.1176/appi.ajp.2013.12070957. PubMed PMID: 23982148. Pubmed Central PMCID: 3928064. Epub 2013/08/29. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Blanchard EB, Scharff L. Psychosocial aspects of assessment and treatment of irritable bowel syndrome in adults and recurrent abdominal pain in children. Journal of consulting and clinical psychology. 2002 Jun;70(3):725–38. doi: 10.1037//0022-006x.70.3.725. PubMed PMID: 12090379. [DOI] [PubMed] [Google Scholar]
- 43.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American journal of preventive medicine. 1998 May;14(4):245–58. doi: 10.1016/s0749-3797(98)00017-8. PubMed PMID: 9635069. Epub 1998/06/23. eng. [DOI] [PubMed] [Google Scholar]
- 44.Blanco C, Rubio J, Wall M, Wang S, Jiu CJ, Kendler KS. Risk Factors for Anxiety Disorders: Common and Specific Effects in a National Sample. Depression and anxiety. 2014 Feb 27; doi: 10.1002/da.22247. PubMed PMID: 24577934. Pubmed Central PMCID: 4147018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Teicher MH, Samson JA, Sheu YS, Polcari A, McGreenery CE. Hurtful words: association of exposure to peer verbal abuse with elevated psychiatric symptom scores and corpus callosum abnormalities. The American journal of psychiatry. 2010 Dec;167(12):1464–71. doi: 10.1176/appi.ajp.2010.10010030. PubMed PMID: 20634370. Pubmed Central PMCID: 3246683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nanni V. Childhood Maltreatment Predicts Unfavorable Course of Illness and Treatment Outcome in Depression: A Meta-Analysis (vol 169, pg 141, 2012). Am J Psychiat. 2012 Apr;169(4):439. doi: 10.1176/appi.ajp.2011.11020335. PubMed PMID: ISI:000302115400023. English. [DOI] [PubMed] [Google Scholar]
- 47.van Tilburg MA, Palsson OS, Whitehead WE. Which psychological factors exacerbate irritable bowel syndrome? Development of a comprehensive model. J Psychosom Res. 2013 Jun;74(6):486–92. doi: 10.1016/j.jpsychores.2013.03.004. PubMed PMID: 23731745. Pubmed Central PMCID: 3673027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McCrory EJ, De Brito SA, Kelly PA, Bird G, Sebastian CL, Mechelli A, et al. Amygdala activation in maltreated children during pre-attentive emotional processing. The British journal of psychiatry : the journal of mental science. 2013 Apr;202(4):269–76. doi: 10.1192/bjp.bp.112.116624. PubMed PMID: 23470285. [DOI] [PubMed] [Google Scholar]
- 49.Liu F, Xie B, Wang Y, Guo W, Fouche JP, Long Z, et al. Characterization of Post-traumatic Stress Disorder Using Resting-State fMRI with a Multi-level Parametric Classification Approach. Brain topography. 2014 Jul 31; doi: 10.1007/s10548-014-0386-2. PubMed PMID: 25078561. [DOI] [PubMed] [Google Scholar]
- 50.Etkin A, Wager TD. Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. The American journal of psychiatry. 2007 Oct;164(10):1476–88. doi: 10.1176/appi.ajp.2007.07030504. PubMed PMID: 17898336. Pubmed Central PMCID: 3318959. Epub 2007/09/28. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ringel Y, Drossman DA, Leserman JL, Suyenobu BY, Wilber K, Lin W, et al. Effect of abuse history on pain reports and brain responses to aversive visceral stimulation: an FMRI study. Gastroenterology. 2008 Feb;134(2):396–404. doi: 10.1053/j.gastro.2007.11.011. PubMed PMID: 18242208. Epub 2008/02/05. eng. [DOI] [PubMed] [Google Scholar]
- 52.Noll-Hussong M, Otti A, Laeer L, Wohlschlaeger A, Zimmer C, Lahmann C, et al. Aftermath of sexual abuse history on adult patients suffering from chronic functional pain syndromes: an fMRI pilot study. Journal of psychosomatic research. 2010 May;68(5):483–7. doi: 10.1016/j.jpsychores.2010.01.020. PubMed PMID: 20403508. Epub 2010/04/21. eng. [DOI] [PubMed] [Google Scholar]
- 53.Thomaes K, Dorrepaal E, Draijer N, de Ruiter MB, Elzinga BM, van Balkom AJ, et al. Treatment effects on insular and anterior cingulate cortex activation during classic and emotional Stroop interference in child abuse-related complex post-traumatic stress disorder. Psychological medicine. 2012 Nov;42(11):2337–49. doi: 10.1017/S0033291712000499. PubMed PMID: 22436595. Epub 2012/03/23. eng. [DOI] [PubMed] [Google Scholar]
- 54.Labus JS, Gupta A, Coveleskie K, Tillisch K, Kilpatrick L, Jarcho J, et al. Sex differences in emotion-related cognitive processes in irritable bowel syndrome and healthy control subjects. Pain. 2013 Oct;154(10):2088–99. doi: 10.1016/j.pain.2013.06.024. PubMed PMID: 23791896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zambito Marsala S, Pistacchi M, Tocco P, Gioulis M, Fabris F, Brigo F, et al. Pain perception in major depressive disorder: A neurophysiological case-control study. Journal of the neurological sciences. 2015 Oct 15;357(1-2):19–21. doi: 10.1016/j.jns.2015.06.051. PubMed PMID: 26233807. [DOI] [PubMed] [Google Scholar]
- 56.Drossman DA, Ringel Y, Vogt BA, Leserman J, Lin W, Smith JK, et al. Alterations of brain activity associated with resolution of emotional distress and pain in a case of severe irritable bowel syndrome. Gastroenterology. 2003 Mar;124(3):754–61. doi: 10.1053/gast.2003.50103. PubMed PMID: 12612913. Epub 2003/03/04. eng. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.