Abstract
Pneumatosis cystoides intestinalis (PCI) is an uncommon disease that generally lacks symptoms and is rarely associated with intussusception. A 29-year-old man visited our hospital for right upper abdominal pain. Computed tomography (CT) scan revealed multiple air-filled cysts along the intestinal wall and a pseudokidney sign in the transverse colon. A gastrographin enema examination showed a so-called crab finger appearance and multiple elevated translucency in the transverse colon. From these findings, the diagnosis of intussusception associated with PCI was made. The enema and manipulative reduction improved the intussusception. Comparing the enema findings before and after the reduction, we thought that mobile cecum could play an important role in the intussusception. Colonoscopy was performed after the reduction and showed multiple elevated lesions in the ascending colon, which were similar to cluster of grapes. The CT scan of the next day revealed no recurrence of the intussusception, and the patient has not had symptoms of recurrence ever since.
Key Words: Pneumatosis cystoides intestinalis, Intussusception, Mobile cecum
Introduction
Pneumatosis cystoides intestinalis (PCI) is a rare condition characterized by the presence of air within the submucosa and/or subserosa of the intestinal wall [1]. Abdominal radiography, contrast enema, ultrasonography and computed tomography (CT) scan can demonstrate the presence of intramural intestinal gas [2, 3].
Possible complications with PCI include pneumoperitoneum, volvulus, intestinal obstruction, perforation and intussusception, but those are not frequent [2, 3].
On the other hand, intussusception in adult patients is usually caused by malignant tumor and operative treatment is often chosen for the therapy of that [4, 5].
In this report, we present an interesting case of intussusception associated with PCI in a young male patient, who was successfully treated by enema and manipulative reduction.
Case Report
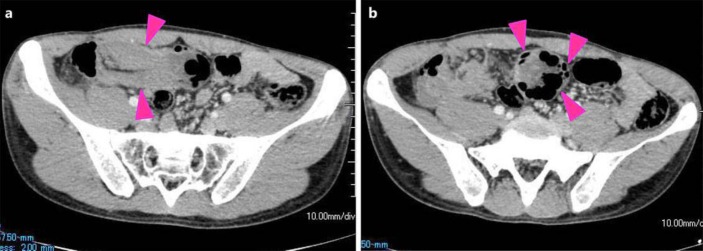
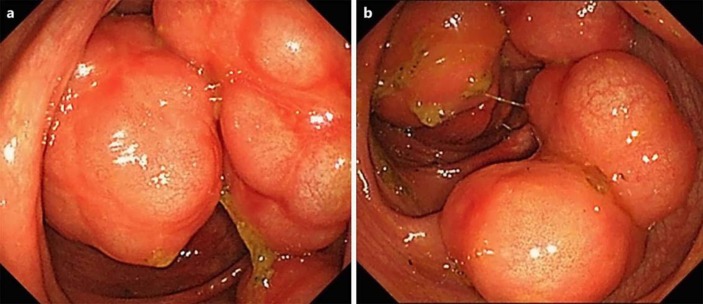
A 29-year-old man who complained of abdominal pain for several days visited our hospital in June 2014. A physical examination revealed tenderness in the right upper abdomen. The serum levels of all variables tested were within the normal range including the white blood cell count (5,600/µl) and C-reactive protein level (0.1 mg/dl). He had a past history of Stevens-Johnson syndrome and bronchiectasis. In addition, his chest X-ray showed enlarged lungs like chronic obstructive pulmonary disease (COPD) patients. Abdominal CT scan on the same day revealed multiple air-filled cysts along the intestinal wall and a pseudokidney sign in the transverse colon (fig 1). However, neither ischemic change in the colonic wall nor ascites could be seen in the CT scan. Then, we performed an enema with gastrographin. The enema examination demonstrated so-called crab finger sign and multiple elevated translucency in the transverse colon (fig 2). We diagnosed intussusception associated with PCI. The carefully performed enema and manipulative reduction improved the intussusception. After the reduction, his abdominal symptom such as right abdominal pain soon disappeared. The subsequently performed colonoscopy revealed a lot of elevated lesions with smooth surface, shaped like a cluster of grapes in the ascending colon (fig 3). CT scans of the next day did not show the recurrence of intussusception (fig 4). Though he refused to undergo hyperbaric oxygen therapy for PCI, he has not had symptoms of the recurrence ever since.
Fig. 1.
CT scan revealing a pseudokidney sign (left; arrowheads) and multiple air-filled cysts along the intestinal wall (right; arrowheads).
Fig. 2.
A crab finger sign and multiple elevated translucency (arrowheads) could be seen in the transverse colon (left). Gastrographin flew into the ascending colon after the reduction (right).
Fig. 3.
Colonoscopy showed many elevated lesions with smooth surface, shaped like a cluster of grapes in the ascending colon.
Fig. 4.
CT scans of the next day did not show the recurrence of intussusception. There were multiple air-filled cysts along the intestinal wall in the ascending colon (arrowhead).
Discussion
PCI is a rare condition in which multiple pneumatocysts develop in the submucosal or subserosa of the small or large intestine [1]. Most commonly, the patients have no symptoms. Rarely, patients may experience symptoms, such as diarrhea, mucus discharge, rectal bleeding, and constipation [6]. Possible complications associated with PCI include pneumoperitoneum, volvulus, intestinal obstruction, perforation and intussusception [2, 3]. Recently, the number of the reports of PCI has been increasing because of the wider use of CT scans and colonoscopy. However, the cases that were found with intussusception remain still very rare. PCI is classified into idiopathic and secondary disease, the former accounts for 15%, the latter 85%, according to Koss's report [7]. Secondary PCI has been reported to develop in association with pulmonary disease such as chronic bronchitis, emphysema, and bronchial asthma, collagen disease, inflammatory bowel disease (IBD), infection disease, leukemia, malignant tumor, cerebral palsy, trauma and use of immune suppressants and alpha-glucosidase inhibitors [8]. The locations where PCI occurs range from the esophagus to the rectum. Idiopathic PCI usually occurs in the colon, particularly the left colon. Secondary PCI usually occurs in the small intestine and right colon [9]. Because of his past history and the location of the PCI, we guess that this case can be secondary PCI.
Operative treatment is usually chosen for the therapy of intussusception in adult patients because the most common cause of that is malignant tumor [4, 5]. Furthermore, if it is suspected that intussusception causes strangulation ileus, bowel ischemia, perforation, and diffuse peritonitis, emergent surgery should be performed. Otherwise, however, firstly performed conservative treatments, such as contrast enema and colonoscopy, can often provide useful diagnostic information. In fact, in our case, the contrast enema made it possible to diagnose that it was intussusception associated with PCI.
In some operated cases, the cecum was not fixed on the retroperitoneum, the so-called mobile cecum. In those situations, the cecum can move relatively freely in the abdominal cavity. Elechi and Elechi [10] reported that the mobile cecum can be the cause of intussusception. In our case, the findings of the enema examination (fig 2) indicate that the mobile cecum can be responsible for the colic intussusception.
In conclusion, carefully performed conservative treatments, such as contrast enema and manipulative reduction, are effective for patients with intussusception associated with PCI except in the case of possible strangulation ileus, bowel ischemia, perforation, and diffuse peritonitis.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- 1.Pear BL. Pneumatosis intestinalis: a review. Radiology. 1998;207:13–19. doi: 10.1148/radiology.207.1.9530294. [DOI] [PubMed] [Google Scholar]
- 2.Heng Y, Schuffler MD, Haggit RC, et al. Pneumatosis intestinalis: a review. Am J Gastroentrol. 1995;90:1747–1758. [PubMed] [Google Scholar]
- 3.Rogy MA, Mirza DF, Kovats E, et al. Pneumatosis cystoides intestinalis (PCI) Int J Colorect Dis. 1990;5:120–124. doi: 10.1007/BF00298485. [DOI] [PubMed] [Google Scholar]
- 4.Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134–138. doi: 10.1097/00000658-199708000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88–94. doi: 10.1016/S0002-9610(96)00419-9. [DOI] [PubMed] [Google Scholar]
- 6.Gagliardi G, Thompson IW, Hershman MJ, et al. Pneumatosis coli: a proposed pathogenesis based on study of 25 cases and review of the literature. Int J Colorectal Dis. 1996;11:111–118. doi: 10.1007/s003840050031. [DOI] [PubMed] [Google Scholar]
- 7.Koss LG. Abdominal gas cysts (pneumatosis cystoides intestinorum hominis) AMA Arch Pathol. 1952;53:523–549. [PubMed] [Google Scholar]
- 8.Cabrera GE, Scopelitis E, Cuellar ML, et al. Pneumatosis cystoides intestinalis in systemic lupus erythematosus with intestinal vasculitis: treatment with high dose prednisone. Clin Rheumatol. 1994;13:312–316. doi: 10.1007/BF02249034. [DOI] [PubMed] [Google Scholar]
- 9.Hujisawa R, Matumoto K, Nakamura S, et al. Pneumatosis cystoides intestinalis. Stomach and intestine. 2005;40:657–660. [Google Scholar]
- 10.Elechi EN, Elechi GN. Intussusception: is floating cecum a causative factor? Analysis of 10 cases. East Afr Med J. 1990;67:779–784. [PubMed] [Google Scholar]