Abstract
Esophageal lipoma is an uncommon benign tumor of the esophagus and accounts for only 0.4% of all benign neoplasms of the gastrointestinal system. The majority of these are located in the cervical part; only very few are located in the lower third of the esophagus. We discuss the case of a 37-year-old female who presented with dysphagia and an esophageal lipoma located in the lower third of the esophagus. The patient underwent right mini-thoracotomy and enucleation of lipoma. Histopathologic examination revealed adipose tissue with a collection of matured adipose tissue. We present the case because of the atypical localization of an esophageal lipoma and development of a diverticulum, which was caused by the lipoma and required an additional surgical procedure.
Key Words: Esophagus, Lipoma, Surgery, Diverticula
Introduction
Esophageal lipomas are uncommon benign tumors, making up only 0.4% of all benign neoplasms of the alimentary tract [1, 2]. Approximately 60% of the benign esophageal neoplasms are leiomyomas, 20% are cysts, 5% are polyps and less than 1% are lipomas. Indeed, Mayo et al. [1] reported comprehensive clinical cases of benign neoplasms of the digestive tract. Lipomas accounted for only 4.1% of all gastrointestinal tract cases, and esophageal lipomas for only 0.4%. Most of the esophageal lipomas are asymptomatic due to their small size. Rarely, esophageal lipomas become large and cause symptoms such as dysphagia, odynophagia, substernal fullness, regurgitation of undigested food and epigastralgia [2, 3, 4]. If they become large and symptoms due to compression of the adjacent structures occur, surgical excision becomes necessary [3, 4, 5]. Additionally, they must be differentiated from malignant tumors of the esophagus and adjacent structures.
Esophageal diverticula are also uncommon benign pathologies, which can be located at any level of the esophagus, but the most common localization is the cervical part of the esophagus where they present as pulsion diverticula. They are classified either as traction or pulsion diverticula, and the primary treatment strategy is diverticulectomy [6]. To the best of our knowledge, esophageal diverticula requiring surgical manipulation after the resection of benign esophageal tumors have not been described before. Herein, we discuss an uncommon benign tumor of the esophagus, which represented with dysphagia and required diverticulectomy after enucleating of the benign mass.
Case Presentation
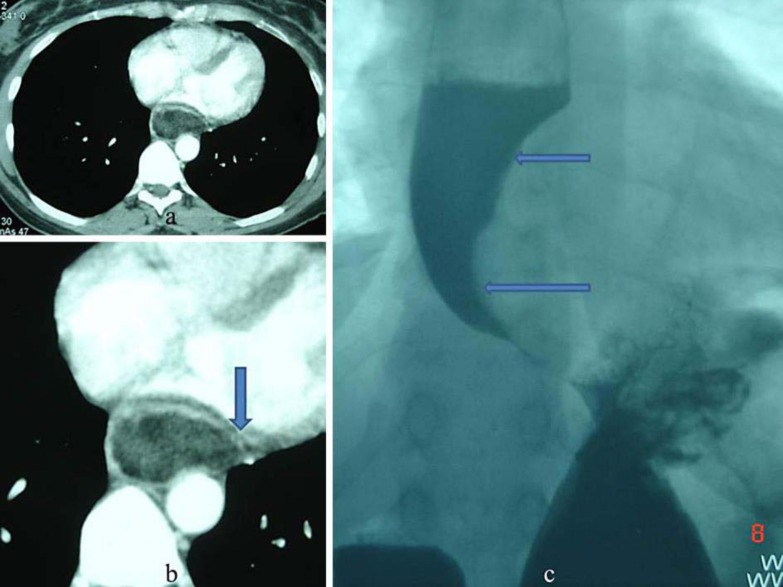
A 37-year-old female was admitted to the thoracic surgery department with dysphagia that had progressively worsened during the previous year. Endoscopy of the upper gastrointestinal system revealed a yellowish-colored, adipose-tissue-like appearance of a polypoid mass with a smooth surface covering between 25 and 34 cm of the esophageal wall (fig 1a). Computed tomography (CT) of the thorax revealed a posterior mediastinal mass (height × width × depth: 10 × 5 × 3 cm; fig 2a), which was compressed between the vertebral column, aorta and heart and pushed the lumen of the esophagus leftward (fig 2b). The mass had low-density tissue absorption, which was characteristic of adipose tissue when compared with surrounding tissues. A barium-swallowed contrast study disclosed an intraluminal space-occupying polypoid lesion protruding through the esophageal wall, which narrowed the lumen of the esophagus (fig 2c). Therefore, esophageal lipoma was considered the most likely diagnosis, and the decision for surgical excision was made.
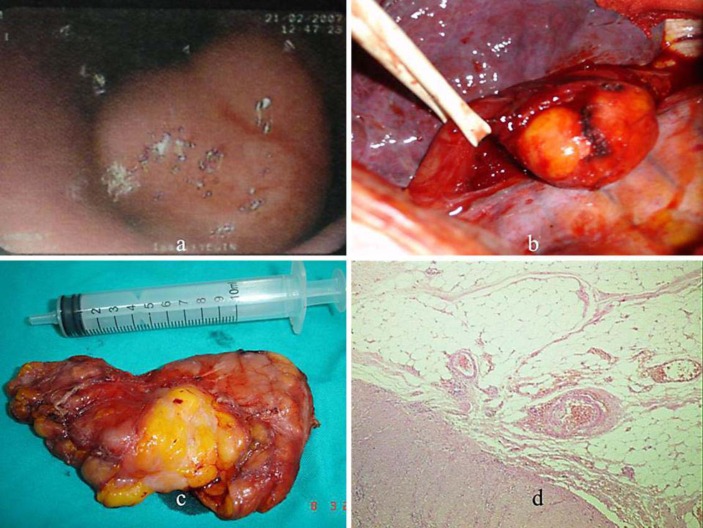
Fig. 1.
a On endoscopic examination, a yellowish-colored, polypoid mass with a smooth surface was observed. b Intraoperative image of the esophageal lipoma. c Macroscopic examination of the encapsulated, well-circumscribed mass after the operation. d Histopathologic examination revealed collection of matured adipose tissue.
Fig. 2.
a Thoracic CT revealing a posterior mediastinal mass. b The esophagus was pushed leftward due to the giant lipoma, and the mass was compressed between the vertebral column, aorta and heart. The arrow shows the esophagus. c A barium swallow test revealed intraluminal narrowing and filling defects (arrows).
A right-sided mini-thoracotomy was performed, the mediastinal pleura was opened and tumor location was identified. Enucleation of the lipoma was the planned operative strategy. The overlying muscle layer of the lower third of the esophagus was incised to expose the tumor, which was then completely enucleated (fig 1b, c). Expansive dilatation of the esophageal mucosa due to the outward pushing effect of the giant lipoma was observed on the barium-swallowed contrast study. After excision of the tumor, the mucosa of the esophagus, which expanded into the lumen, turned outside and led to a diverticulum (9 × 4 cm) on the right side of the esophageal wall. For confirmation of the diverticulum, a nasogastric catheter was inserted and deployed in the proximal part of diverticulum. The distal part of the diverticulum was obstructed manually; high-pressure air was applied through the catheter, and the diverticulum became more visible. Subsequently, diverticulectomy was added to surgery, and the operation was completed without complications. Gross examination of the mass showed a yellowish, well-circumscribed, encapsulated mass measuring 10 × 5 × 3 cm (fig 1c). Histopathologic examination revealed lipoma with a collection of matured adipose tissue next to the muscularis propria layer of the esophagus (fig 1d). The postoperative course was uneventful. The patient was discharged on the 7th postoperative day and was instructed to take her oral medication.
Discussion
Lipomas of the gastrointestinal system can be found in all areas of the digestive tract, most commonly in the colon, followed by the small bowel, stomach and esophagus. Therefore, lipomas of the esophagus in the digestive tract is the least common site and accounts for only 0.4% of all benign neoplasms of the digestive tract [1, 2]. Furthermore, the majority of esophageal lipomas occur in the cervical esophagus, a few of them being located in the thoracic part [1, 2, 4]. In a review by Akiyama et al. [4], seventeen esophageal lipoma cases have been reported in Japan; only two of them were located in the thoracic part of the esophagus. Esophageal tumor in our case was already diagnosed as lipoma and was located in the lower third of esophagus.
The correct diagnosis of an esophageal lipoma depends on careful consideration of the patient history, radiographic examinations of the thorax and inspection with endoscopy of the upper gastrointestinal system. Most esophageal lipomas are small in size and solitary without any symptoms and may be found incidentally during imaging [4, 5]. As they are asymptomatic and incidentally found tumors, the real incidence in the population is unknown. However, lipomas of the esophagus commonly present with dysphagia when they grow in size [2]. There may be other symptoms, including odynophagia, substernal fullness, regurgitation of undigested food, epigastralgia, weight loss, difficulty in swallowing, gastroesophageal reflux and melena [1, 2, 3]. Regurgitation of undigested foods is primary seen when the lipoma is located in the cervical part of the esophagus, with intraluminal growing and obstruction. Thus, when complete obstruction of the lumen occurs, weight loss and malnutrition are unavoidable. Although dysphagia is the most common symptom, Kau et al. [3] presented a case of esophageal fibrolipoma who had progressive odynophagia and required narcotic pain control [3]. Ulceration at the inferior cape of the mass may also occur when tumors are located in the lower third of the esophagus, which may lead to bleeding. Thus, melena can be seen.
The diagnostic imaging tools for determining esophageal masses are endoscopic examination of the upper gastrointestinal tract, CT of the chest and barium swallow tests [1, 2, 3]. Endoscopic examination of the upper gastrointestinal tract is known to be the best diagnostic tool. The most precious diagnostic finding during endoscopy is observing mucosal intactness of the esophageal lumen. Forceps biopsy is not recommended for esophageal lipoma, just as it is not recommended for other benign tumors of the esophagus. Transesophageal needle biopsy could be performed; however, this technique is usually not diagnostic [1, 2]. Useful signs to distinguish lipomas from other benign and malign lesions include a yellowish color and smooth surface. A barium swallow test usually reveals a dilated hypertrophic esophagus or may show a smooth, polypoid, intraluminal space-occupying lesion and filling defects. CT of the chest shows low-density absorption of the mass, which is characteristic of adipose tissue [1, 2, 3, 4, 5, 6]. On positron emission tomography, lower uptake values are useful for distinguishing lipomas from other malignant lesions [7].
Various treatment options are available, depending on tumor size and location, and additional pathology of the patient. Treatment options include excision via cervical incision, mini-thoracotomy, endoscopy or videothoracoscopy and esophagectomy [1, 2, 4, 5]. When tumors are pedunculated, it is possible to resect them by endoscopy. Videothoracoscopic resection is a current treatment method for these tumors [4, 5]. Kau et al. [3] described a successful resection of a large esophageal fibrolipoma via the transoral laser microsurgical approach. They discussed that small lesions and those that are attached at the level of the cricopharyngeus muscle may be candidates for transoral approaches. However, occasionally, esophagectomy could be added to surgery due to a giant tumor size, mucosal ulceration and erosion and broad, extensive mucosal involvement [2]. In our patient, mini-thoracotomy was a treatment option, and the mass was successfully removed with diverticulectomy.
Benign tumors of the esophagus (leiomyoma, fibroma or lipoma) are generally located in the submucosal and intramural layers of the esophagus. Usually, they show extraluminal growth and can be asymptomatic unless they reach a giant size [8]. In our case, the tumor was compressed between the vertebral column, aorta and heart so that it displayed intraluminal growth and caused expansion of the mucosa. After excision of the tumor, the expanded mucosa turned upside down or briefly, ‘inside out’; and a diverticulum became visible. This reason for the development of a diverticulum is not a familiar etiology for esophageal diverticula. The most common etiological factor for esophageal diverticula is pulsion diverticulum due to increased intraluminal pressure. We suggest that ‘internal pulsion diverticulum’ is the appropriate term for the classical type of pulsion diverticulum; however, ‘external pulsion diverticulum’ could be an even more suitable term in our case.
Surgery is the recommended treatment option for esophageal lipoma and other esophageal benign pathologies and provides curative healing. However, we emphasize that after the resection of these pathologies, the mucosal layer of the esophagus should be evaluated for the possibility of a diverticulum and mucosal expansion. It should be kept in mind that small diverticula and those having a wide basement can spontaneously regress, whereas large diverticula and sessile diverticula should be resected.
Statement of Ethics
The authors have no ethical conflicts to declare.
Disclosure Statement
The authors declare that there are no conflicts of interest to disclose.
References
- 1.Mayo CW, Pagutalunan PJG, Brown DJ. Lipoma of the alimentary tract. Surgery. 1963;53:598–603. [PubMed] [Google Scholar]
- 2.Algin C, Hacioglu A, Aydin T, İhtiyar E. Esophagectomy in esophageal lipoma: report of a case. Turk J Gastroenterol. 2006;17:110–112. [PubMed] [Google Scholar]
- 3.Kau RL, Patel AB, Hinni ML. Giant fibrolipoma of the esophagus. Case Rep Otolaryngol. 2012;2012:406167. doi: 10.1155/2012/406167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akiyama S, Kataoka M, Horisawa M, Inoue S, Sakai M, et al. Lipoma of the esophagus – report of a case and review of literature. Jpn J Surg. 1990;20:458–462. doi: 10.1007/BF02470832. [DOI] [PubMed] [Google Scholar]
- 5.Tsalis K, Antoniou N, Kalfadis S, Dimoulas A, Dagdilelis AKL, Lazaridis C. Laparoscopic enucleation of a giant submucosal esophageal lipoma. Case report and literature review. Am J Case Rep. 2013;14:179–183. doi: 10.12659/AJCR.883928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yekeler E, Ulutas H, Kabalar ME. Intramural Esophageal bronchogenic cyst mimicking malignity and support of PET-CT in the diagnosis. Eur J Gen Med. 2012;9(suppl 1):56–59. [Google Scholar]
- 7.Cassivi SD, Deschamps C, Nichols FC, Allen MS, Pairolero PC. Diverticula of the esophagus. Surg Clin North Am. 2005;85:495–503. doi: 10.1016/j.suc.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 8.Choong CK, Meyers BF. Benign esophageal tumors: introduction, incidence, classification, and clinical features. Semin Thorac Cardiovasc Surg. 2003;15:3–8. doi: 10.1016/s1043-0679(03)70035-5. [DOI] [PubMed] [Google Scholar]