Abstract
Darier disease/dyskeratosis follicularis is a genodermatosis characterized by brown, oily keratotic papules and plaques in the seborrheic areas of the face and chest. Responsible for the disease are mutations in the ATP2A2 gene, encoding SERCA2, a calcium pump of the sarco-/endoplasmic reticulum. Mechanical trauma, heat, humidity, ultraviolet B radiation, oral corticosteroids and lithium are known trigger factors of the disorder. We report on a 48-year-old German woman with a flare-up of Darier disease under interferon-α-2a (IFNα-2a) therapy with clinical signs of lichen nitidus. Due to the fulminant course of the eruption, we suspected IFNα as a possible trigger. To our knowledge there are no reports regarding exacerbation of Darier disease during IFNα therapy. Possible pathogenetic mechanisms are being discussed.
Key Words: Darier disease, Interferon-α, Lichen nitidus, Psoriasis vulgaris
Introduction
Darier disease is a rare autosomal dominant inherited genodermatosis with onset around puberty, characterized by yellow to brown, oily keratotic papules and plaques primarily affecting the seborrheic areas of the face and chest. The disorder may show different clinical manifestations, such as palmoplantar pits and nail abnormalities [1]. In this report we describe a flare-up of Darier disease during treatment with interferon-α-2a (IFNα-2a).
Case Report
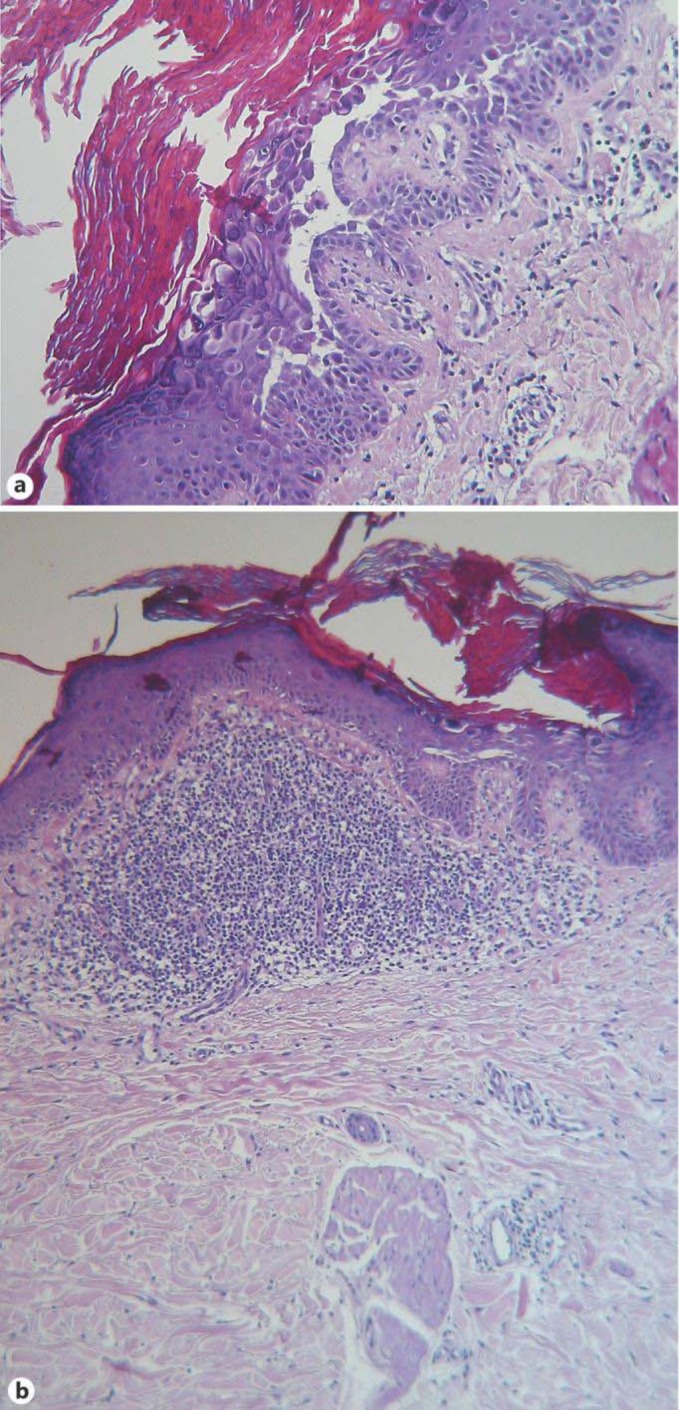
After excision and sentinel node biopsy of an amelanotic malignant melanoma located on the left lower leg, with a Breslow tumor thickness of 3.5 mm, our 48-year-old female patient was treated with subcutaneous injections of 3 million international units of IFNα-2a thrice weekly. The therapy was initially well tolerated. The patient had been diagnosed in puberty with Darier disease, affecting her face and sternum. Since then she had had almost yearly disease flare-ups, especially at the beginning of the summer period. One month after the initiation of IFNα-2a treatment the patient presented with an exacerbation of Darier disease, with multiple, disseminated, erythematous and brownish, partly follicular, hyperkeratotic papules on the trunk and extremities accompanied by severe itching (fig. 1). Some of the skin lesions, especially on the lower extremities, showed a glossy and lichenoid form (fig. 2). The nails were slightly dystrophic. Oral manifestation was not present. We discontinued IFNα-2a treatment and the patient was admitted to our inpatient department for further diagnostic investigation and therapy. Laboratory evaluation revealed no pathologic findings. Histopathologic examination of a skin lesion demonstrated focal areas with parakeratosis and orthohyperkeratosis. The epidermis showed irregular hyperplasia and partly significant suprabasal acantholysis with dyskeratotic keratinocytes (fig. 3a). Close to these areas a dense subepidermal, band-like, lymphocytic infiltration under a narrow epidermis was observed (fig. 3b). These findings were consistent with dyskeratosis follicularis and signs of lichen nitidus. A biopsy from another skin lesion demonstrated compact orthohyperkeratosis, acanthotic epidermis with scattered suprabasal areas with acantholysis and dyskeratosis. Corps ronds as well as slight superficial perivascular lymphocytic infiltrates were also detected.
Fig. 1.
a Confluent reddish-brownish papules in the seborrheic areas of the chest. b Darier disease. Multiple keratotic papules on the lower extremities.
Fig. 2.

Lichen nitidus-like lesions. Grouped, lichenoid, glossy papules close to a histologically proven histiocytoma on the left forefoot.
Fig. 3.
a Routine hematoxylin-eosin stain showed suprabasal acantholysis with dyskeratotic keratinocytes (×100). b Subepidermal lymphocytic infiltration under a narrow epidermis (×80).
Oral antihistaminics and external application of steroids, urea and polidocanol improved both the skin lesions and itching. As we had ruled out drug eruption, we continued the treatment with IFNα-2a at the same dose, and the patient was further monitored in the context of postsurgical tumor follow-up. Despite the initial improvement of the lesions, they did not heal and persisted during the therapy with IFNα-2a.
Discussion
Darier disease, also known as dyskeratosis follicularis or Darier-White disease, is a rare autosomal dominant inherited skin disorder which usually becomes apparent in the second decade of life [1]. Its prevalence has been estimated to be 1: 55,000–1: 100,000. Mutations in the ATP2A2 gene, encoding SERCA2, a calcium pump of the sarco-/endoplasmic reticulum, are responsible for the disorder [2]. Abnormal interkeratinocyte adhesion and aberrant epidermal keratinization are the primary histologic features. However, the mechanism by which decreased activity of the SERCA2 calcium pump leads to these changes is still under investigation [3]. Mechanical trauma, heat, humidity, ultraviolet B radiation and oral corticosteroids are known trigger factors of the disease. Moreover, lithium is a recognized exacerbating factor of Darier disease. Süle et al. [4] suggested that lithium exacerbates the symptoms of Darier disease through reducing the epidermal levels of SERCA2 to a critical point, promoting the acantholytic and other histologic disturbances of the disorder. Diltiazem has also been reported to worsen the disease, acting possibly on the same axis with the gene defect of the disorder [5].
Our patient had flare-ups of the disease in the face and chest almost every year at the beginning of the summer period, but this flare-up came extremely early, with a remarkable, unexpected manifestation on the extremities, partly with lesions that resembled lichen nitidus. Lichen nitidus is a rare skin eruption characterized by multiple, small, discrete, glistening, flesh-colored papules that may occur anywhere in the skin. Due to this fulminant course of the eruption, we suspected IFNα as a possible trigger.
To our knowledge there are no reports regarding exacerbation of Darier disease during IFNα therapy. Dry skin, itching, mild hair loss and induction or exacerbation of psoriasis vulgaris are known cutaneous side effects of IFNα. There are reports of flare-up of psoriasis vulgaris after starting IFNα therapy for several diseases. The pathogenetic interpretation of these findings is difficult due to the lack of a convincing etiologic concept [6].
In order to understand the mechanism of such an association, we should take into account the functions of IFNα in the skin. It induces immune activation through enhancement of interleukin-22 (IL-22)-producing T cells and provides the interface between immune activation and epidermal remodeling by increasing keratinocyte responsiveness to IL-1 [7]. Tohyama et al. [8] demonstrated that IFNα strengthens the responsiveness of epidermal keratinocytes to IL-22, an important mediator in the pathogenesis of psoriasis, via increased IL-22 receptor expression. This supports the theory that IFNα triggers the development of psoriatic lesions. However, this mechanism is not specific to psoriasis. It is also known that IFNα activates the Jak-STAT pathway, whose cytokine components play a crucial role in common skin disorders, including psoriasis vulgaris and atopic dermatitis [9, 10]. However, whether IFNα really worsens the course of Darier disease remains unclear. Possible underlying mechanisms should be further investigated.
Statement of Ethics
The patient has given written informed consent for publication of this case report.
Disclosure Statement
The authors declare that there are no conflicts of interest.
References
- 1.Engin B, Kutlubay Z, Erkan E, Tüzün Y. Darier disease: a fold (intertriginous) dermatosis. Clin Dermatol. 2015;33:448–451. doi: 10.1016/j.clindermatol.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 2.Zheng L, Jiang H, Mei Q, Chen B. Identification of two novel Darier disease-associated mutations in the ATP2A2 gene. Mol Med Rep. 2015;12:1845–1869. doi: 10.3892/mmr.2015.3605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Müller EJ, Caldelari R, Kolly C, Williamson L, Baumann D, Richard G, Jensen P, Girling P, Delprincipe F, Wyder M, Balmer V, Suter MM. Consequences of depleted SERCA2-gated calcium stores in the skin. J Invest Dermatol. 2006;126:721–731. doi: 10.1038/sj.jid.5700091. [DOI] [PubMed] [Google Scholar]
- 4.Süle N, Tészás A, Kálmán E, Szigeti R, Miseta A, Kellermayer R. Lithium suppresses epidermal SERCA2 and PMR1 levels in the rat. Pathol Oncol Res. 2006;12:234–236. doi: 10.1007/BF02893419. [DOI] [PubMed] [Google Scholar]
- 5.Nath AK, Udayashankar C. Diltiazem worsens Darier's disease. Int J Dermatol. 2014;53:e1. doi: 10.1111/ijd.12111. [DOI] [PubMed] [Google Scholar]
- 6.Wölfer LU, Goerdt S, Schröder K, Zouboulis CC, Orfanos CE. Interferon-alpha-induced psoriasis vulgaris. Hautarzt. 1996;47:124–128. doi: 10.1007/s001050050388. [DOI] [PubMed] [Google Scholar]
- 7.Conrad C, Gilliet M. Type I IFNs at the interface between cutaneous immunity and epidermal remodeling. J Invest Dermatol. 2012;132:1759–1762. doi: 10.1038/jid.2012.149. [DOI] [PubMed] [Google Scholar]
- 8.Tohyama M, Yang L, Hanakawa Y, Dai X, Shirakata Y, Sayama K. IFN-α enhances IL-22 receptor expression in keratinocytes: a possible role in the development of psoriasis. J Invest Dermatol. 2012;132:1933–1935. doi: 10.1038/jid.2011.468. [DOI] [PubMed] [Google Scholar]
- 9.Arulampalam V, Kolosenko I, Hjortsberg L, Björklund AC, Grandér D, Tamm KP. Activation of STAT1 is required for interferon-alpha-mediated cell death. Exp Cell Res. 2011;317:9–19. doi: 10.1016/j.yexcr.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 10.Palanivel JA, Macbeth AE, Chetty NC, Levell NJ. An insight into JAK-STAT signalling in dermatology. Clin Exp Dermatol. 2014;39:513–518. doi: 10.1111/ced.12273. [DOI] [PubMed] [Google Scholar]