Highlights
-
•
Painful, discolored umbilical swelling in women may be primary endometriosis.
-
•
Abdominal tomography must be carried out to exclude concomitant pelvic endometriosis.
-
•
To avoid recurrens of primary umbilical endometriosis: Total umbilical resection.
Keywords: Endometriosis, Primary umbilical endometriosis, Total umbilical resection
Abstract
Background
Primary umblikal endometriosis is a rare illness. In this report we aimed to discuss the management of this rare condition.
Case summary
A 28-year-old nulliparous woman was present at our clinic who was suffering from painful swelling in the umbilicus during her menstruation for the last 3 months. Her examination showed a dark-color sensitive nodule of 20 × 15 mm in size in the umbilicus. A lower abdominal tomography was performed to exclude the presence of a concomitant pelvic endometriosis, and it showed increased density consistent with subcutaneous inflammation in the umbilicus. Her medical history and physical examination suggested primary umbilical endometriosis. A total resection including umbilicus was performed.
Discussion
Primary umbilical endometriosis is a rare benign disease and clinically difficult to differentiate from other diseases that cause umbilical nodule. Imaging modalities have no pathognomonic findings for diagnosis. Surgical exploration and excision are the definitive and safe treatment of primary umbilical endometriosis.
Conclusion
Total umbilical resection should be preferred to avoid local recurrent.
1. Introduction
Endometriosis is defined as the presence of functional endometrium tissue outside the uterine cavity in which it is normally localized. It affects 10–15% of all women of childbearing age and 6% of perimenopauses women [1], [2] Endometriosis is often localized in the vulva, vagina, cervix, ovaries, and pelvic peritoneum. Its extra genital localization including the intestinal tract, urinary tract, peritoneum, omentum, lungs, thoracic cage, surgical scars, abdominal wall, inguinal area and umbilicus are less by 12%. Cutaneous endometriosis (secondary) occurs on the abdominal and pelvic scars of gynecologic surgeries such as hysterectomy, episiotomy, cesarean section, and laparoscopy [3], [4], [5], [6], [7], [8]. Primary (spontaneous) umbilical endometriosis (PUE) is a very rare case and not associated with surgical procedure. In this report we aimed to discuss the management of this rare condition.
2. Presentation of case
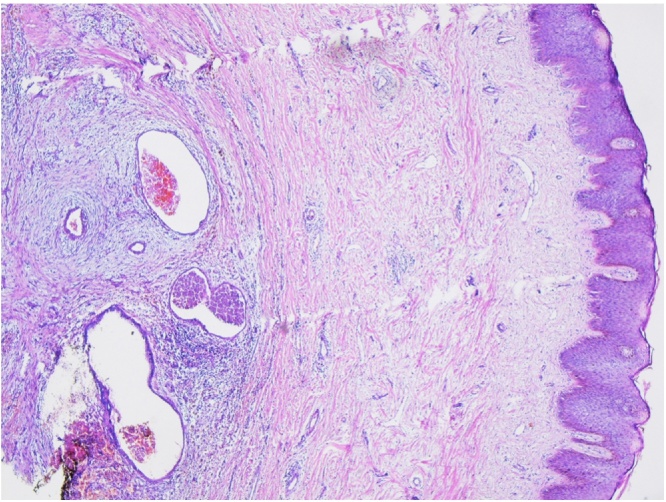
A 28-year-old nulliparous woman, who had been married for 1 year, suffering from a slowly growing swelling in the umbilicus that she noticed 3 months ago presented at gynecologic polyclinic. She also had umbilical pain during her menstruation for the last 3 months. She had no operations and did not receive any medication. She did not describe dysmenorrhea, abdominal pain or dyspareunia. She had regular menstrual cycles and did not use oral contraceptive. The physical examination showed a dark-color sensitive nodule of 20 × 15 mm in size localized in the umbilicus [Fig. 1]. Umbilical endometriosis was suspected based on her medical history and physical examination findings. Superficial USG performed for umbilical area revealed a heterogeneous tissue area of 9.5 × 6 × 7 mm at 7.5 mm deep plane of the skin. An oral and intravenous contrast lower abdominal tomography was performed to exclude the presence of a concomitant pelvic endometriosis, which showed an increased density consistent with inflammation in the subcutaneous tissue at umbilicus level, but no intraabdominal extension was observed [Fig. 2]. Preoperative hemogram, biochemical and coagulation profile was normal. The patient was advised to receive preoperative and postoperative medical treatment. However, the patient said that she wanted to have a baby and she denied medical treatment. The existing lesion was totally resected with umbilicus under general anesthesia [Fig. 3]. In preoperative abdominal tomography there was no any suspect about pelvic endometriosis. Therefore, during the operation any more invasive pelvic assessment was not be necessary. She had no complications during postoperative period. In the histopathological examination of resected tissues, a well-circumscribed endometriosis foci was identified with dilated glands localized in the deep dermis under the epidermis with stratified squamous epithelium under small magnification (H&E ×40) [Fig. 4]. The larger magnification (H&E ×100) showed a stroma that was surrounded with edematous and fusiform cells and had dilated endometrial gland structures. The eosinophilic secretion was apparent in the stroma. The maximum magnification (H&E ×200) showed a stroma that had endometrial glands with stratified columnar epithelium and was surrounded by edematous and fusiform cells and partially inflammatory cells. After a 19-month follow up, no signs of local recurrence were present.
Fig. 1.
A dark-color sensitive nodule of 20 × 15 mm.
Fig. 2.
An increased density in the subcutaneous tissue of umbilicus.
Fig. 3.
Total resection of the lesion.
Fig. 4.
Dilated glands localized in the deep dermis (HE ×40).
3. Discussion
Primary (spontaneous) umbilical endometriosis was first defined by Villar in 1886. It accounts for 0.5–1% of all cases of extra genital endometriosis [9], [10], [11]. The pathogenesis of endometriosis has been a much debated issue. According to hypothesis proposed by Sampson in 1920, endometriosis was caused by retrograde menstruation passing thorough the fallopian tube in the pelvis [5]. However, there are other theories such as caulomic metaplasia, direct spread, iatrogenic spread, lymphatic or hematogenous spread [3]. The theory of lymphatic and hematogenic transplantation is suggested for cases of umbilical endometriosis with pelvic endometriosis. But the disease may occur through metaplasia of urachus residues in a case of isolated umbilical endometriosis [9]. Secondary umbilical endometriosis may occur through iatrogenic spread of endometrial cells after operations such as cesarean section and laparoscopy [3], [4], [5], [6], [7], [8], [12].
In many cases of primary umbilical endometriosis, there is an umbilical nodule concurrent with menstruation, which causes periodic pain in the umbilicus and may have a bleeding tendency. There may be a constant pain rather than periodic pain. The nodule can be a brown, blue or faint spot. In differential diagnosis of umbilical nodules, benign diseases such as secondary endometriosis, hemangioma, umbilical hernia, sebaceous cyst, granuloma, lipoma, abscess, keloid, and urachus anomaly, and malignant diseases such as Sister Mary Joseph’s nodule, melanoma, sarcoma, adenocarcinoma, and lymphoma should always be considered [13].
Sensitivity and specifity of ultrasonography, computerized tomography and magnetic resonance are low in the diagnosis of umbilical endometriosis. None of these imaging techniques primer have a pathognomonic finding of umbilical endometriosis.Ultrasonography can provide some information on the size of the nodule and its cohesion to adjacent tissues [13], [14].
The treatment of umbilical endometriosis has not been standardized yet due to limited number of cases. The medical treatment including progesterone, danazol, norethysterone, and analogous to gonadotropin-releasing hormone has not provided reliable results. However, some authors have reported success in the reduced size of nodule and improvement of symptoms using medical hormonal therapies [2], [15]. In the review by Victory et al., almost 70% of patients required surgical treatment [12]. Surgical choices include either total umbilical resection with or without repair of underneath fascia and peritoneum, or local excision of endometrial nodule with preserving umbilicus. Total resection of umbilicus is mostly preferred. Local excision of endometrial lesion should be performed by achieving adequate edge of the surrounding normal tissue in order to avoid local recurrence [2], [15]. Several authors suggested total umbilical excision independent of the size of endometrial nodule [16], [17]. We also performed total umbilical resection on our case that is rather chosen.
4. Conclusion
If primary umbilical endometriosis is always considered as a potential diagnosis in women who have painful, sometimes discolored umbilical swelling, then this can be identified earlier and treated optimally. Total umbilical resection should be preferred to avoid local recurrent.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
None.
Funding
None.
Research registration unique identifying number (UIN)
ISJP_2016_4.
Authors contribution
Bedri Aras Pektaş: Data collections, Interpretation of data; Conception of the study.
Semih Hot: Literature review; Data analysis.
Seracettin Eğin: Design of the study; Interpretation of data; Writing the paper; Related literature review; Final approval of the version to be submitted.
Veli Mihmanlı: Data analysis; Suggestion for the case report.
Guarantor
Dr. Seracettin Eğin.
Contributor Information
Seracettin Eğin, Email: seracettin_egin@hotmail.com.
Bedri Aras Pektaş, Email: araspektas@gmail.com.
Semih Hot, Email: semihhot@hotmail.com.
Veli Mihmanlı, Email: velimihmanli@yahoo.com.
References
- 1.Spaziani E., Picchio M., Di Filippo A., De Cristofano C., Ceci F., Stagnitti F. Spontaneous umbilical endometriosis: a case report with one-year follow-up. Clin. Exp. Obstet. Gynecol. 2009;36:263–264. [PubMed] [Google Scholar]
- 2.Rosina P., Pugliarello S., Colato C., Girolomoni G. Endometriosis of umbilical cicatrix: case report and review of the literature. Acta Dermatovenerol. Croat. 2008;16:218–221. [PubMed] [Google Scholar]
- 3.Catalina-Fernández I., López-Presa D., Sáenz-Santamaria J. Fine needle aspiration cytology in cutaneous and subcutaneous endometriosis. Acta Cytol. 2007;51:380–384. doi: 10.1159/000325751. [DOI] [PubMed] [Google Scholar]
- 4.Agarwal A., Fond Y.F. Cutaneous endometriosis. Singap. Med J. 2008;49:704–709. [PubMed] [Google Scholar]
- 5.Arava S., Iyer V.K., Mathur S.R. Cytological diagnosis of peritoneal endometriosis. J. Cytol. 2010;27:77–78. doi: 10.4103/0970-9371.70757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaushik R., Gulati A. Inguinal endometriosis. A case report. J. Cytol. 2008;25:73–74. [Google Scholar]
- 7.Pathan Z.A., Dinesh U.S., Rao R. Scar endometriosis. J. Cytol. 2010;27:106–108. doi: 10.4103/0970-9371.71877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Medeiros F.C., Cavalcante D.I., Medeiros M.A., Eleuterio J., Jr Fine needle aspiration cytology of scar endometriosis: study of seven cases and literature review. Diagn. Cytopathol. 2011;39:18–21. doi: 10.1002/dc.21319. [DOI] [PubMed] [Google Scholar]
- 9.Teh W.T., Vollenhoven B., Harris P.I. Umbilical endometriosis, a pathology that a gynecologist may encounter when inserting Veres needle. Fertil. Steril. 2006;86(1764):e1–2. doi: 10.1016/j.fertnstert.2006.03.070. [DOI] [PubMed] [Google Scholar]
- 10.Khaled A., Hammami H., Fazaa B., Zermani R., Ben Jilani S., Kamoun M.R. Primary umbilical endometriosis: a rare variant of extragenital endometriosis. Pathologica. 2008;100:473–475. [PubMed] [Google Scholar]
- 11.Bimolchandra L., Devi H.B., Rameshwar M., Devi R.K.P., Singh Y.A., Devi K.A. Primary umbilical endometrioma: a case report. JMS. 2008;22:85–86. [Google Scholar]
- 12.Victory R., Diamond M.P., Johns D.A. Villar’s nodule: a case report and systematic literature review of endometriosis externa of the umbilicus. J. Minim. Invasive Gynecol. 2007;14:23–32. doi: 10.1016/j.jmig.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 13.Hensen J.H., Van Breda Vriesman A.C., Puylaert J.B. Abdominal wall endometriosis: clinical presentation and imaging features with emphasis on sonography. AJR Am. J. Roentgenol. 2006;186:616–620. doi: 10.2214/AJR.04.1619. [DOI] [PubMed] [Google Scholar]
- 14.Savelli L., Manuzzi L., Di Donato N., Salfi N., Trivella G., Ceccaroni M., Seracchioli R. Endometriosis of the abdominal wall: ultrasonographic and Doppler characteristics. Ultrasound Obstet. Gynecol. 2012;39:336–340. doi: 10.1002/uog.10052. [DOI] [PubMed] [Google Scholar]
- 15.Bagade P.V., Giurguis M.M. Menstruating from the umbilicus as a rare case of primary umbilical endometriosis: a case report. J. Med. Case Rep. 2009;3:9326. doi: 10.1186/1752-1947-3-9326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mechsner S., Bartley J., Infanger M., Loddenkemper C., Herbel J., Ebert A.D. Clinical management and immunohistochemical analysis of umbilical endometriosis. Arch. Gynecol. Obstet. 2009;280:235–242. doi: 10.1007/s00404-008-0900-4. [DOI] [PubMed] [Google Scholar]
- 17.Dadhwal V., Gupta B., Dasgupta C., Shende U., Deka D. Primary umbilical endometriosis: a rare entity. Arch. Gynecol. Obstet. 2011;283:119–120. doi: 10.1007/s00404-010-1809-2. [DOI] [PubMed] [Google Scholar]