Abstract
Background:
Rotator cuff tears are a significant cause of shoulder morbidity. Surgical techniques for repair have evolved to optimize the biologic and mechanical variables critical to tendon healing. Double-row repairs have demonstrated superior biomechanical advantages to a single-row.
Methods:
The preferred technique for rotator cuff repair of the senior author was reviewed and described in a step by step fashion. The final construct is a knotless double row transosseous equivalent construct.
Results:
The described technique includes the advantages of a double-row construct while also offering self reinforcement, decreased risk of suture cut through, decreased risk of medial row overtensioning and tissue strangulation, improved vascularity, the efficiency of a knotless system, and no increased risk for subacromial impingement from the burden of suture knots.
Conclusion:
Arthroscopic knotless double row rotator cuff repair is a safe and effective method to repair rotator cuff tears.
Keywords: Double row, knotless repair, rotator cuff, shoulder transosseous
INTRODUCTION
Rotator cuff tears are common in an aging population,[1] are a significant source of shoulder morbidity, [2] and have significant direct and indirect societal economic burdens. [3] Although symptoms from rotator cuff tears can improve with nonsurgical treatment, [4] surgical repair of the ruptured tendon is often necessary to improve a patient’s function when nonsurgical measures fail. [5, 6] Additionally, repair of full thickness rotator cuff tears has been shown to be cost effective in all patient populations and produce net societal cost savings for patients under the age of sixty-one years. [3]. The goals of arthroscopic rotator cuff repair are to enhance shoulder function by improving motion and strength and reducing pain. Although some patients have been shown to experience short term benefits despite re-tear of their repaired rotator cuff tendons, long-term durability of functional improvement is likely dependent on maintenance of their healed tendon. [7] Improved objective and subjective outcomes of rotator cuff repair have been predictably achieved when the tendon has been documented to heal, [3, 8-11] therefore achieving tendon healing is a primary surgical goal. Primary healing and long term maintenance of the rotator cuff tendon-bone interface is dependent on both mechanical and biologic factors. [12] As such, surgical techniques have evolved to optimize both. Techniques have progressed from open to miniopen to arthroscopic. This general trend in approaches has also been accompanied by improvements in arthroscopic methods and fixation technology. Early in the evolution of rotator cuff repair techniques, failure of the repair construct was the most frequent cause of recurrent rotator cuff tear. A greater understanding of the biomechanical deficiencies of first generation repair techniques[13-16] has led to the trend from transosseous repairs to single-row suture anchor repairs, to double-row suture anchor repairs, and now to knotless, double-row, transosseous equivalent, bridging techniques. [17] While the biomechanical advantages of contemporary double-row techniques have been shown, clinical outcomes are conflicting and have yet to definitively demonstrate which scenarios necessitate their utilization. The advantages of a knotless, double-row, interconnected bridge technique utilizing suture tape includes self reinforcement, [18] decreased risk of suture cut through, [19] decreased risk of medial row overtensioning and tissue strangulation, [20] improved vascularity, [21] the efficiency of a knotless system, and no increased risk for subacromial impingement from the burden of suture knots. The purpose of this report is to provide a detailed description of the technical aspects of our technique.
SURGICAL TECHNIQUE
Set-Up
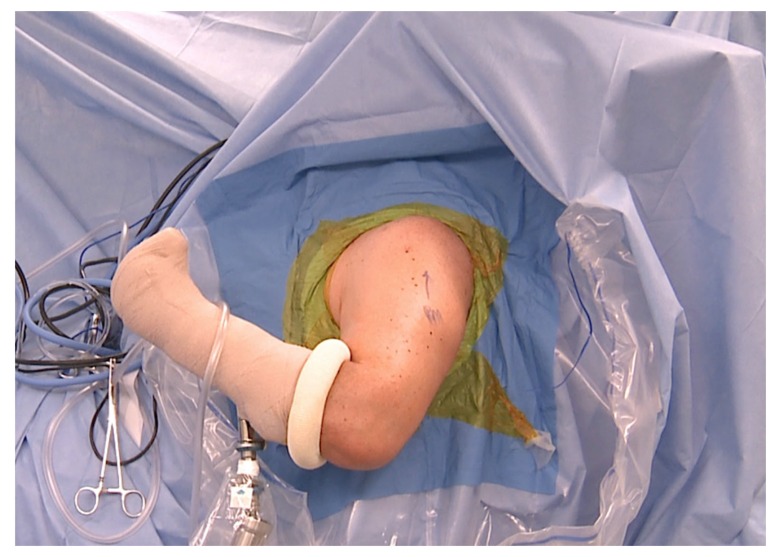
An interscalene block is placed prior to surgery to help with analgesia immediately postoperatively and during the initial rehabilitation process. The patient is anesthetized with a general anesthetic and placed in a modified beach-chair positioner (Tenet T-Max, Tenet Medical Engineering, Inc., Calgary, Alberta, Canada) (Fig. 1). After induction of general anesthesia the patient’s shoulder is examined for range-of-motion and stability. The shoulder is then prepared using a standard sterile technique and the arm is secured to a pneumatic arm holder (SPIDER arm positioner, Tenet Medical Engineering, Inc., Calgary, Alberta, Canada).
Fig. (1).
The patient is placed in the modified beach chair position.
Portal Placement and Diagnostic Arthroscopy
A standard arthroscopic posterior viewing portal is placed in the soft spot that is palpable at the posterior glenohumeral joint line. Distances distal from the posterolateral acromial margin vary by patient size, therefore it is most helpful to place the skin incision at the approximation of the equator of the glenohumeral joint. As soft tissue swelling occurs due to fluid extravasation, the posterior skin incision will tend to migrate superiorly and the ideal angle of approach to the subacromial space can be compromised if the incision is not made inferior enough. An anterosuperior working portal is then established after localization with a spinal needle to confirm perpendicular placement relative to the anterior glenohumeral joint line. When necessary, ideal placement of the skin incision for this portal takes into consideration the trajectory needed to perform an efficient distal clavicle excision as well. A low profile 5-mm x 7cm cannula (Arthrex Inc., Naples, FL) is inserted through the rotator interval to facilitate instrumentation. Systematic diagnostic arthroscopy of the joint and surrounding structures dictated by the preoperative examination and advanced imaging is performed using a standard 30˚ arthroscope.
Concomitant pain generating pathology is identified and addressed. Limited subacromial decompression, subcoracoid decompression, distal clavicle excision and/or biceps tenodesis are performed selectively based on the patient’s pathoantomy. Synovitis within the rotator interval is debrided and the coracohumeral interval is examined. If the interval is less than 8mm in females or less than 10mm in males, [22, 23] coracoplasty is performed to reestablish the dimensions of the interval by anteriorizing, medializing, and superiorizing the margins of the coracoid with an arthroscopic bur. When coracoplasty is necessary, the subscapularis tendon is critically scrutinized and addressed as indicated, as it is often pathologically involved with a stenotic coracohumeral interval [23].
The arthroscope is then inserted into the subacromial space via the posterior portal. An anterolateral portal is created approximately 4cm-5cm lateral to the acromion and in line with the anterior margin of the clavicle. A liberal subacromial bursectomy is performed clearing gutters of the subdeltoid space completely to facilitate subsequent rotator cuff repair and ensure the entirety of the tear is adequately visualized. Acromioplasty with release of the coracoacromial ligament is performed using a modified cutting block technique if a type III acromion or impingement lesion is identified. If distal clavicle incision is planned, the anterior inferior acromioclavicular joint capsule is divided with electrocautery to allow access to the joint, and the distal 1cm of the clavicle is then excised with an arthroscopic burr.
Tear Recognition and Tendon/Bone Preparation
In order to anatomically restore the rotator cuff footprint, accurate recognition of the tear pattern is critical [24]. Once the rotator cuff is cleared of pathologic bursal attachments and degenerative margins are debrided, an arthroscopic cuff grasping forceps is utilized to mobilize the cuff to the greater tuberosity to plan for suture anchor positioning (Figs. 2a-2d) [25]. The rotator cuff footprint on the greater tuberosity is then lightly debrided to a bleeding surface to optimize healing potential. This is done carefully, balancing the need for adequate decortication to a stable rim with the potential to compromise suture anchor fixation with overzealous debridement to the level of softer cancellous bone.
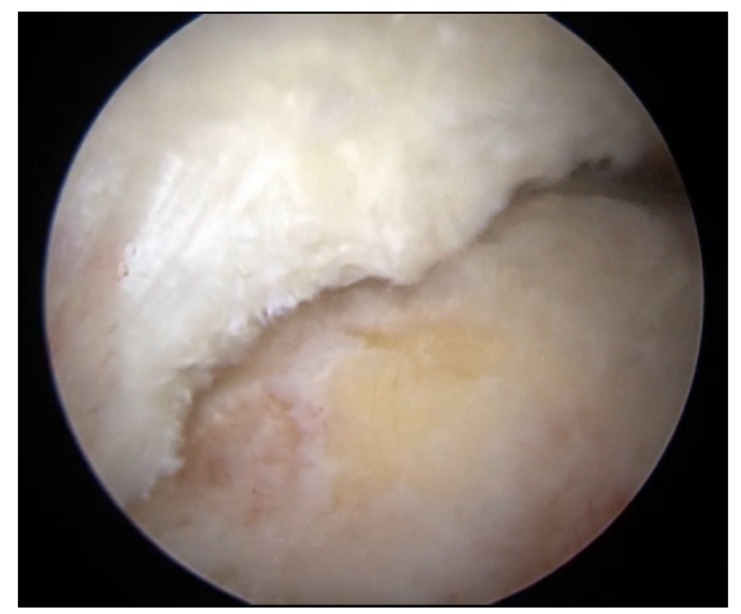
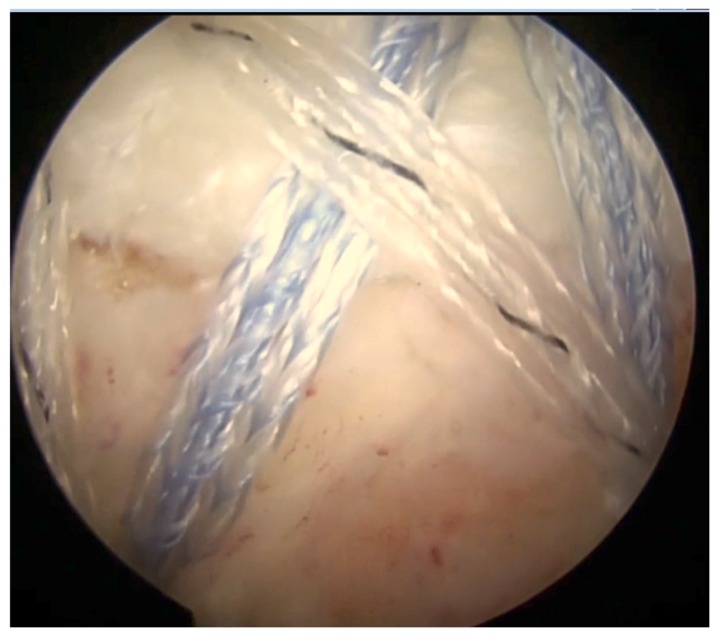
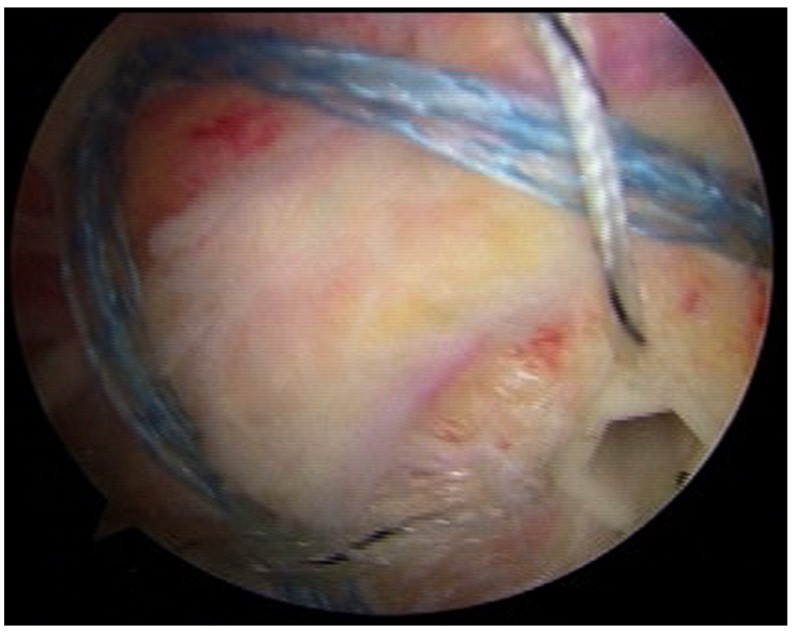
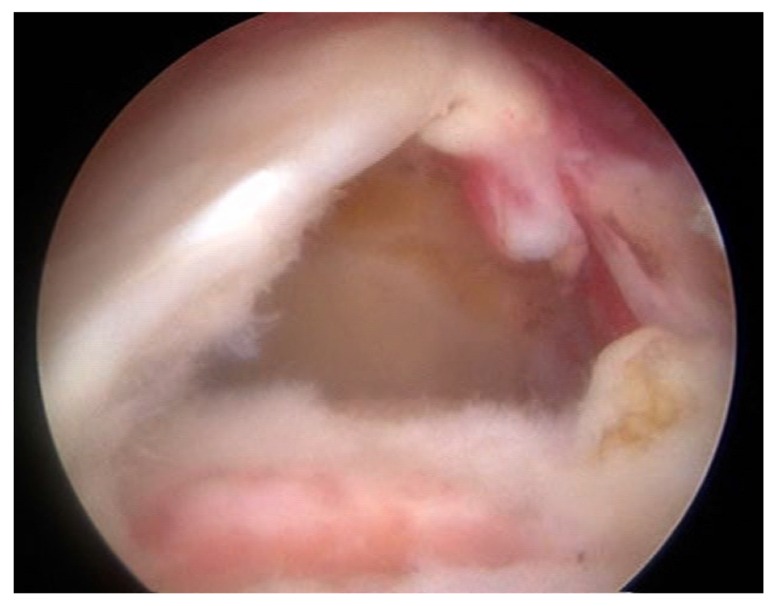
Fig. (2a).
A crescent shaped tear of the rotator cuff is visualized. This tear pattern provides excellent mobility of the tear margins allowing for a tension-free repair directly back to the greater tuberosity.
Fig. (2d).
A massive crescent shaped tear is identified. If the rotator cuff tendon is of good quality and can be mobilized, this tear pattern can often be repaired using an extended knotless double row technique.
REPAIR TECHNIQUE
To optimize communication of marrow contents with the repair site, we prefer the use of vented, cannulated suture anchors (Swivelock; Arthrex, Naples, FL). Most large tears are amenable to repair with a 4-bar interconnected, double-row, knotless, self-reinforcing technique. However, the described technique can be extended to include additional anchors dictated by the size and pattern of the tear [26-28].
Two anchors pre-loaded with 2mm suture tape (Fibertape, Arthrex, Naples, FL) are used to create a medial row. The medial anchors are placed at the anterior and posterior margins of the tear approximately 1-2mm lateral to the articular margin (Fig. 3). Placement of the anchors begins anteriomedially. A bone socket is first created with a punch inserted through a lateral portal. To avoid tangential skiving during anchor placement, the pneumatic arm holder should be utilized to reposition the proximal humerus to allow for bone sockets to be created perpendicular to the cortical rim. The anchor is advanced with a mallet until the body of the anchor contacts the bone, and then it is advanced clockwise until the superficial margin of the anchor is even with the cortex (Fig. 4). Each limb of the suture tape is then passed though the rotator cuff tendon approximately 2-3 mm lateral to the musculotendinous junction to avoid overtensioning and/or suture cut through. Great care is taken to capture any delaminated portions of the cuff tendon with passage of each limb of the suture tape. The limbs of the suture tape are then docked in the posterior portal while attention is turned towards placement of the posteromedial anchor and suture tape in a similar fashion.
Fig. (3).
A medial anchor is placed anterior and posterior to the margins of the rotator cuff tear. The anchor is placed 1-2 mm lateral to the articular margin.
Fig. (4).
The anchor is advanced with a mallet until the body of the anchor contacts the bone and the superficial margin of the anchor is even with the cortex.
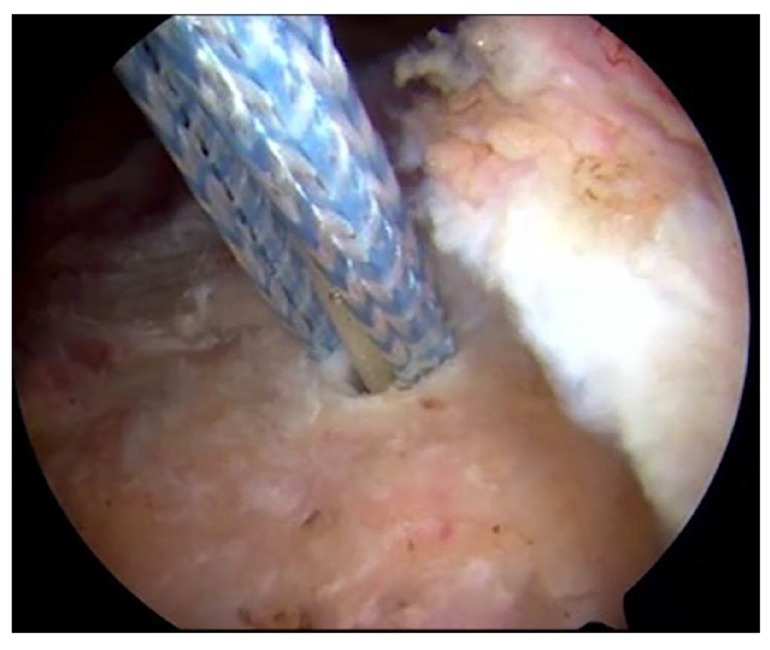
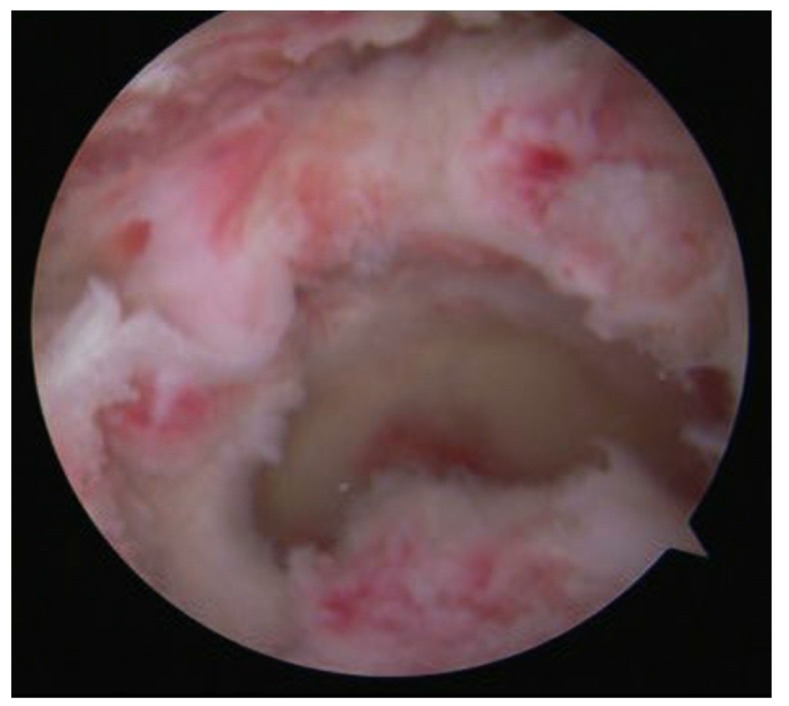
Creation of the lateral bridging portion of the construct is then undertaken. One limb of suture tape from each medial anchor is then retrieved from the lateral portal through a 6mm threaded cannula (Twist-in, Arthrex, Naples, FL). The suture tapes are then loaded into the eyelet of another knotless suture anchor (Swivelock; Arthrex, Naples, FL). Soft tissue is cleared from the intended site of insertion with electrocautery, approximately 5-10mm lateral to the edge of the greater tuberostiy [29]. A bone socket is then created with a punch as was done for the medial anchors. The eyelet of the anchor is then seated into the socket. In order to restore the rotator cuff to its footprint and provide sufficient compression, the limbs of the suture tape are then individually tensioned before advancing the body of the anchor. Once the anatomy of the footprint is restored, the body of the anchor is advanced clockwise to secure the fiber tape. Theses steps are repeated for the posterolateral anchor, thus creating the final bridging, interconnected construct (Figs. 5a, 5b).
Fig. (5a).
The final linked, knotless double row repair construct is visualized.
Fig. (5b).
The linked knotless double row repair construct can be expanded to include additional anchors if necessary.
If pathology of the long head of the biceps tendon was identified during intraarticular debridement and it was tenotomized, the procedure is concluded with an open subpectoral biceps tenodesis. Our preferred technique is to utilize a small cosmetic incision in the axillary fold to identify and deliver the tendon from the interval between the pectoralis major and conjoint tendons, and fix the tendon in a 7 mm or 8 mm unicortical socket with a polyetheretherketone (PEEK) tenodesis screw (Arthrex Inc., Naples, FL) .
POSTOPERATIVE REHABILITATION
The stability of the fixation construct achieved through this technique allows for immediate passive range-of-motion of the shoulder in most scenarios. Rehabilitation progression should ultimately be guided by the patient’s tissue quality, concomitant risk factors that may adversely affect their healing milieu, and assessment of their compliance. Following fixation of a large tear, with good tissue quality, in a compliant patient without additional risk factors for repair failure, an abduction sling is placed (SlingShot, Bregg, Inc., Carlsbad, CA). Physical therapy begins the first postoperative day and full passive range-of-motion is permitted as tolerated. The sling is worn for 3-4 postoperative weeks when active-assisted and active motion are initiated. Progressive strengthening is generally started at 8 weeks. Most patients are permitted to return to unrestricted activity at 4 months.
THE AUTHOR’S EXPERIENCE
The senior surgeon (PJM) has performed over 600 rotator cuff repairs using the described technique. Early clinical results in 22 patients undergoing a primary rotator cuff repair demonstrated significant improvements in pain levels and postoperative outcomes scores [6]. In addition, the mean patient satisfaction was 9.8 out of 10 and patients where able to return to full activities at four months. Another study in which the majority of rotator cuff repairs were performed using a double row knotless interconnected technique noted that a larger acromial index was associated with larger rotator cuff tears [5]. Again, all clinical outcomes scores significantly improved. A recent study examined the results of rotator cuff repair in recreational athletes over 70 years of age [1]. Thirty four out of the 49 shoulders underwent repair using the knotless linked double row repair. The mean postoperative American Shoulder and Elbow Surgeons (ASES) score was 90.3 at the time of final follow up and 77% of patients were able to return to sporting levels at or near their preinjury level.
CONCLUSION
Arthroscopic rotator cuff repair techniques have evolved immensely to their current state, striving for anatomic footprint restoration while optimizing both mechanical and biologic healing variables. While double-row constructs improve the contact area of the footprint, decrease the risk of gap formation, increase footprint compression, and have a higher load to failure relative to single-row techniques, [3, 30-33] the knotless, transosseous equivalent technique described has several additional benefits. The construct’s interconnectivity and self-reinforcement are its greatest strengths. Shear stresses are converted into compressive forces reinforcing the repair under conditions that would be more detrimental to traditional repairs [18]. Theoretically, with more rigid fixation, rehabilitation can be accelerated in the hope of improving early outcomes while maintaining durable long term improvements in shoulder function. Additionally, the knotless technique described optimizes local biology by utilizing suture tape with a greater ability to distribute load across the repaired tendon, decreasing the risk of tissue cut through and strangulation. Vented anchors also augment the local environment by facilitating the communication of marrow contents with the repair site. Finally, knotless techniques are simple, may reduce operative time, and decrease the risk of impingement from the repair itself by completely eliminating the subacromial knot burden. Although early clinical results are promising, comparative prospective evaluation with long-term follow-up will be critical to thoroughly demonstrating the clinical benefits of this biomechanically superior technique.
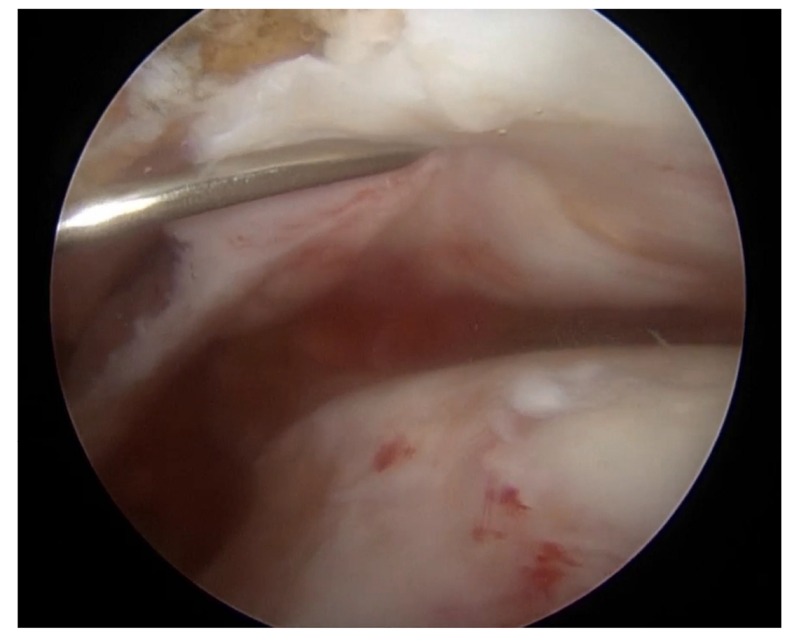
Fig. (2b).
An L shaped tear of the rotator cuff is visualized. Margin convergence is often performed followed by direct repair of the remaining free margin to the greater tuberosity.
Fig. (2c).
A U shaped tear is identified. With U shaped tears, the mobility is often severely reduced. Therefore margin convergence is often utilized.
ACKNOWLEDGEMENTS
Declared none.
CONFLICT OF INTEREST
The authors report the following potential conflict of interest or source of funding: WRM, JAG, PJM. receive support from Steadman Philippon Research Institute. Corporate sponsorship for Steadman Philippon Research Institute is received from Ossur, Smith & Nephew Endoscopy, Siemens Medical Solutions, and Arthrex. P.J.M. also receives support from Arthrex, Myos, GameReady, and VuMedi.
REFERENCES
- 1.Bhatia S., Greenspoon J.A., Horan M.P., Warth R.J., Millett P.J. Two-year outcomes after arthroscopic rotator cuff repair in recreational athletes older than 70 years. Am. J. Sports Med. 2015;43(7):1737–1742. doi: 10.1177/0363546515577623. [DOI] [PubMed] [Google Scholar]
- 2.Oh L.S., Wolf B.R., Hall M.P., Levy B.A., Marx R.G. Indications for rotator cuff repair: a systematic review. Clin. Orthop. Relat. Res. 2007;455(455):52–63. doi: 10.1097/BLO.0b013e31802fc175. [DOI] [PubMed] [Google Scholar]
- 3.Mather R.C., III, Koenig L., Acevedo D., Dall T.M., Gallo P., Romeo A., Tongue J., Williams G., Jr The societal and economic value of rotator cuff repair. J. Bone Joint Surg. Am. 2013;95(22):1993–2000. doi: 10.2106/JBJS.L.01495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seida J.C., LeBlanc C., Schouten J.R., Mousavi S.S., Hartling L., Vandermeer B., Tjosvold L., Sheps D.M. Systematic review: nonoperative and operative treatments for rotator cuff tears. Ann. Intern. Med. 2010;153(4):246–255. doi: 10.7326/0003-4819-153-4-201008170-00263. [DOI] [PubMed] [Google Scholar]
- 5.Ames J.B., Horan M.P., Van der Meijden O.A., Leake M.J., Millett P.J. Association between acromial index and outcomes following arthroscopic repair of full-thickness rotator cuff tears. J. Bone Joint Surg. Am. 2012;94(20):1862–1869. doi: 10.2106/JBJS.K.01500. [DOI] [PubMed] [Google Scholar]
- 6.Vaishnav S., Millett P.J. Arthroscopic rotator cuff repair: scientific rationale, surgical technique, and early clinical and functional results of a knotless self-reinforcing double-row rotator cuff repair system. J. Shoulder Elbow Surg. 2010;19(2) Suppl.:83–90. doi: 10.1016/j.jse.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 7.Galatz L.M., Ball C.M., Teefey S.A., Middleton W.D., Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J. Bone Joint Surg. Am. 2004;86-A(2):219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Lafosse L., Brozska R., Toussaint B., Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J. Bone Joint Surg. Am. 2007;89(7):1533–1541. doi: 10.2106/JBJS.F.00305. [DOI] [PubMed] [Google Scholar]
- 9.Lichtenberg S., Liem D., Magosch P., Habermeyer P. Influence of tendon healing after arthroscopic rotator cuff repair on clinical outcome using single-row Mason-Allen suture technique: a prospective, MRI controlled study. Knee Surg. Sports Traumatol. Arthrosc. 2006;14(11):1200–1206. doi: 10.1007/s00167-006-0132-8. [DOI] [PubMed] [Google Scholar]
- 10.Liem D., Bartl C., Lichtenberg S., Magosch P., Habermeyer P. Clinical outcome and tendon integrity of arthroscopic versus mini-open supraspinatus tendon repair: a magnetic resonance imaging-controlled matched-pair analysis. Arthroscopy. 2007;23(5):514–521. doi: 10.1016/j.arthro.2006.12.028. [DOI] [PubMed] [Google Scholar]
- 11.Liem D., Lichtenberg S., Magosch P., Habermeyer P. Magnetic resonance imaging of arthroscopic supraspinatus tendon repair. J. Bone Joint Surg. Am. 2007;89(8):1770–1776. doi: 10.2106/JBJS.F.00749. [DOI] [PubMed] [Google Scholar]
- 12.Millett P.J., Horan M.P., Maland K.E., Hawkins R.J. Long-term survivorship and outcomes after surgical repair of full-thickness rotator cuff tears. J. Shoulder Elbow Surg. 2011;20(4):591–597. doi: 10.1016/j.jse.2010.11.019. [DOI] [PubMed] [Google Scholar]
- 13.Barber F.A., Coons D.A., Ruiz-Suarez M. Cyclic load testing of biodegradable suture anchors containing 2 high-strength sutures. Arthroscopy. 2007;23(4):355–360. doi: 10.1016/j.arthro.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 14.Bardana D.D., Burks R.T., West J.R., Greis P.E. The effect of suture anchor design and orientation on suture abrasion: An in vitro study. Arthroscopy. 2003;19(3):274–281. doi: 10.1053/jars.2003.50032. [DOI] [PubMed] [Google Scholar]
- 15.Bynum C.K., Lee S., Mahar A., Tasto J., Pedowitz R. Failure mode of suture anchors as a function of insertion depth. Am. J. Sports Med. 2005;33(7):1030–1034. doi: 10.1177/0363546504271746. [DOI] [PubMed] [Google Scholar]
- 16.Hanypsiak B.T., DeLong J.M., Simmons L., Lowe W., Burkhart S. Knot strength varies widely among expert arthroscopists. Am. J. Sports Med. 2014;42(8):1978–1984. doi: 10.1177/0363546514535554. [DOI] [PubMed] [Google Scholar]
- 17.Millett P.J., Warth R.J., Dornan G.J., Lee J.T., Spiegl U.J. Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J. Shoulder Elbow Surg. 2014;23(4):586–597. doi: 10.1016/j.jse.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 18.Burkhart S.S., Adams C.R., Burkhart S.S., Schoolfield J.D. A biomechanical comparison of 2 techniques of footprint reconstruction for rotator cuff repair: the SwiveLock-FiberChain construct versus standard double-row repair. Arthroscopy. 2009;25(3):274–281. doi: 10.1016/j.arthro.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 19.Barber F.A., Drew O.R. A biomechanical comparison of tendon-bone interface motion and cyclic loading between single-row, triple-loaded cuff repairs and double-row, suture-tape cuff repairs using biocomposite anchors. Arthroscopy. 2012;28(9):1197–1205. doi: 10.1016/j.arthro.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 20.Cho N.S., Yi J.W., Lee B.G., Rhee Y.G. Retear patterns after arthroscopic rotator cuff repair: single-row versus suture bridge technique. Am. J. Sports Med. 2010;38(4):664–671. doi: 10.1177/0363546509350081. [DOI] [PubMed] [Google Scholar]
- 21.Voigt C., Bosse C., Vosshenrich R., Schulz A.P., Lill H. Arthroscopic supraspinatus tendon repair with suture-bridging technique: functional outcome and magnetic resonance imaging. Am. J. Sports Med. 2010;38(5):983–991. doi: 10.1177/0363546509359063. [DOI] [PubMed] [Google Scholar]
- 22.Ferreira Neto A.A., Almeida A.M., Maiorino R., Zoppi Filho A., Benegas E. An anatomical study of the subcoracoid space. Clinics (Sao Paulo) 2006;61(5):467–472. doi: 10.1590/S1807-59322006000500015. [DOI] [PubMed] [Google Scholar]
- 23.Gerber C., Terrier F., Ganz R. The role of the coracoid process in the chronic impingement syndrome. J. Bone Joint Surg. Br. 1985;67(5):703–708. doi: 10.1302/0301-620X.67B5.4055864. [DOI] [PubMed] [Google Scholar]
- 24.Millett P.J., Warth R.J. Posterosuperior rotator cuff tears: classification, pattern recognition, and treatment. J. Am. Acad. Orthop. Surg. 2014;22(8):521–534. doi: 10.5435/JAAOS-22-08-521. [DOI] [PubMed] [Google Scholar]
- 25.Dugas J.R., Campbell D.A., Warren R.F., Robie B.H., Millett P.J. Anatomy and dimensions of rotator cuff insertions. J. Shoulder Elbow Surg. 2002;11(5):498–503. doi: 10.1067/mse.2002.126208. [DOI] [PubMed] [Google Scholar]
- 26.van der Meijden O.A., Wijdicks C.A., Gaskill T.R., Jansson K.S., Millett P.J. Biomechanical analysis of two-tendon posterosuperior rotator cuff tear repairs: extended linked repairs and augmented repairs. Arthroscopy. 2013;29(1):37–45. doi: 10.1016/j.arthro.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 27.Warth R.J., Greenspoon J.A., Bhatia S., Millett P.J. Arthroscopic double row rotator cuff repair using a knotless interconnected technique. Oper. Tech. Orthop. 2015;25(1):43–48. doi: 10.1053/j.oto.2014.10.003. [DOI] [Google Scholar]
- 28.Greenspoon J.A., Petri M., Millett P.J. Arthroscopic knotless, double-row, extended linked repair for massive rotator cuff tears. Arthrosc. Tech. 2016;5(1):e127–e132. doi: 10.1016/j.eats.2015.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tingart M.J., Apreleva M., Lehtinen J., Zurakowski D., Warner J.J. Anchor design and bone mineral density affect the pull-out strength of suture anchors in rotator cuff repair: which anchors are best to use in patients with low bone quality? Am. J. Sports Med. 2004;32(6):1466–1473. doi: 10.1177/0363546503262644. [DOI] [PubMed] [Google Scholar]
- 30.Park M.C., Cadet E.R., Levine W.N., Bigliani L.U., Ahmad C.S. Tendon-to-bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques. Am. J. Sports Med. 2005;33(8):1154–1159. doi: 10.1177/0363546504273053. [DOI] [PubMed] [Google Scholar]
- 31.Park M.C., ElAttrache N.S., Tibone J.E., Ahmad C.S., Jun B.J., Lee T.Q., Part I. Part I: Footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J. Shoulder Elbow Surg. 2007;16(4):461–468. doi: 10.1016/j.jse.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 32.Park M.C., Pirolo J.M., Park C.J., Tibone J.E., McGarry M.H., Lee T.Q. The effect of abduction and rotation on footprint contact for single-row, double-row, and modified double-row rotator cuff repair techniques. Am. J. Sports Med. 2009;37(8):1599–1608. doi: 10.1177/0363546509332506. [DOI] [PubMed] [Google Scholar]
- 33.Park M.C., Tibone J.E., ElAttrache N.S., Ahmad C.S., Jun B.J., Lee T.Q., Part I.I. Part II: Biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J. Shoulder Elbow Surg. 2007;16(4):469–476. doi: 10.1016/j.jse.2006.09.011. [DOI] [PubMed] [Google Scholar]