Abstract
Pancreatic cancer, mostly pancreatic ductal adenocarcinoma (PDAC), is a leading cause of cancer-related death in the US, with a dismal median survival of 6 months. Thus, there is an urgent unmet need to identify ways to diagnose and to treat this deadly cancer. Although a number of genetic changes have been identified in pancreatic cancer, their mechanisms of action in tumor development, progression and metastasis are not completely understood. Hedgehog signaling, which plays a major role in embryonic development and stem cell regulation, is known to be activated in pancreatic cancer; however, specific inhibitors targeting the smoothened molecule failed to improve the condition of pancreatic cancer patients in clinical trials. Furthermore, results regarding the role of Hh signaling in pancreatic cancer are controversial with some reporting tumor promoting activities whereas others tumor suppressive actions. In this review, we will summarize what we know about hedgehog signaling in pancreatic cancer, and try to explain the contradicting roles of hedgehog signaling as well as the reason(s) behind the failed clinical trials. In addition to the canonical hedgehog signaling, we will also discuss several non-canonical hedgehog signaling mechanisms.
Keywords: hedgehog, pancreatic cancer, Gli1, non-canonical signaling, cancer metastasis
The hedgehog signaling pathway
In mammals, hedgehog (Hh) signaling plays a crucial role in embryonic development, adult tissue homeostasis and pathogenesis of human diseases[1-3]. In normal situation, Hh signaling is regulated by one of the three ligands: sonic hedgehog (Shh), Indian hedgehog (Ihh), and Desert hedgehog (Dhh). Hh ligands activate signaling in target cells by binding to the 12-pass transmembrane receptor patched (PTC). In the absence of these ligands, PTC prevents the 7-transmembrane protein, smoothened (SMO), from transducing signal to downstream Gli transcription factors, and the pathway is in the “off” state. Hedgehog binding to Ptch leads to SMO signaling to downstream effectors, leading to Gli-induced target gene expression, and the pathway is turned on. Numerous studies indicate a critical role of primary cilium for Hh signal transduction[4-7]. Primary cilium is a microtubule-based non-motile antenna-like structure that emanates from cell surface of virtually all mammalian cells. There are three mammalian Gli gene family members: Gli1, Gli2 and Gli3. Gli1 and Gli2 are generally regarded as transcriptional activators whereas Gli3 is often viewed as a repressor[8]. Activation of GLI proteins via the Hh-PTC-SMO route is regarded as the canonical Hh signaling pathway. In addition to the canonical pathway, the molecules can bypass the ligand-receptor signaling axis to activate Gli, and these types of regulation are regarded as non-canonical Hh signaling. RAS signaling[9-10], TGFβ[11], PI3K[12] and PKC[13] are reported to regulate Hh signaling via non-canonical pathways. Non-canonical Hh signaling is often observed in malignant diseases and have been summarized in another recent published review[14].
Pancreatic cancer
Pancreatic cancer is a devastating malignant disease with a very high mortality. Despite its low incidence (2% of all cancer cases), pancreatic cancer is the fourth leading cause of cancer-related deaths in the US and expected to become the second cause of cancer-related deaths in a few years[15-16]. After several decades of efforts, the 5-year survival rate of pancreatic cancer remains around 5%, without dramatic improvement[17]. The high mortality rate and poor prognosis are largely due to its aggressive and metastatic nature. By the time of diagnosis, more than 80% of cases are locally advanced or distally metastasized[18], and are not eligible for surgical resection, which is the most effective treatment option. Even in patients with resected pancreatic cancer, the outcomes are not as good as other resected solid tumors. For pancreatic cancer patients, the median survival is about 2 years after surgery and adjuvant therapy[19-21]. In contrast, patients with advanced disease can only survive a few months.
The most common histologic type of pancreatic cancer is pancreatic ductal adenocarcinoma (PDAC), accounting for >90% of pancreatic cancer cases. The exact cellular origin of PDAC is still not completely known. By histological studies and clinical observation, it is postulated that before the final formation of invasive cancer, there is a stepwise progression of precursor lesions, including pancreatic intraepithelial neoplasia (PanIN), intraductal papillary mucinous neoplasms (IPMN) and mucinous cystic neoplasms (MCN)[22]. PanIN, the most common precursor lesion of PDAC, is a type of microscopic precursor lesion[23]. Based on the degree of cytonuclear and architectural atypia, PanINs are divided in three grades: PanIN-1 (subdivided into PanIN-1A and PanIN-1B), PanIN-2 and PanIN-3/in situ carcinoma[23,24], reflecting a progressive increase in histologic grade. Recent genetic studies indicate a possibility that PDAC arises from acinar cells instead of ductal cells[25,26]. Clinically, pancreatic cancer can be divided into four stages (I, II, III, IV) based on the tumor size, and appearance of lymph node or distal metastasis[27]. Although whether the tumor is resectable or not will require radiology data, stage-I and some stage-II tumors are generally resectable or borderline resectable whereas all stage-IV and some stage-III tumors are not resectable.
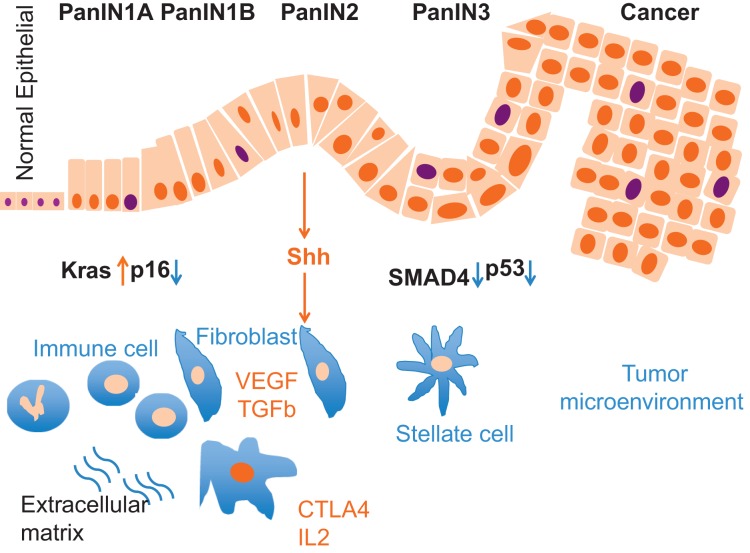
The most common genetic event in pancreatic cancer is oncogenic KRAS mutation, which is almost universally present in PDAC (>90%)[28]. Since over 90% of low-grade PanIN (PanIN-1) lesions also harbor oncogenic KRAS mutations[29], and mice conditionally expressing mutant KRAS develop PanIN[30], mutated KRAS is considered an early and initiating event in PDAC development. This mutation alone, however, may not be sufficient to drive the progression of invasive cancer. Molecular profiling studies revealed that during the PanIN-to-PDAC progression, inactivating mutations of three tumor suppressor genes are commonly found: telomere shortening (PanIN-1) p16/ CDKN2A (some PanIN-1B and most PanIN-2), tumor protein 53 (TP53, PanIN-3), BRCA2 (PanIN-3) and SMAD family member 4 (SMAD4, PanIN-3)[31] (Fig. 1). Deficiency in the p16/CDKN2A axis is detectable in the early PanIN lesions (30% of PanIN-1B)[32] and in nearly all PDAC[33-34], whereas inactivation of TP53 and SMAD4 is mainly found in PanIN-3, and is associated with tumor progression[23,35-36] (Fig. 1). In addition to these four frequently mutated genes (designated “mountains” in the genetic landscape of the PDAC genomes), comprehensive genetic analysis has also uncovered alterations of numerous candidate cancer genes at low frequency (designated “hills”) [37-40], indicating the complexity and heterogeneity of PDAC.
Fig. 1. Molecular alterations in pancreatic cancer development.
Development of pancreatic cancer is a multiple-step process, involving in formation of pancreatic intraepitheial lesions (PanIN) and carcinoma. In this process, the tumor compartment starts to have activated mutation of Kras and loss of p16 in early stages whereas loss of SMAD4 and p53 are often found in later stages. Accompanying the alterations in the tumor, accumulating changes in the stroma also occur, including expansion of fibroblasts, stellate cells, and an increase in tumor stromal fibers. These cellular changes are associated with elevated expression of many growth factors, cytokines and chemokines. Shh is one of the factors secreted from the tumor compartment to affect the tumor microenvironment.
Another important feature of pancreatic cancer is the dense stroma, which is composed of fibroblasts, stellate cells, extracellular matrix and immune cells. The direct regulation of TGFβ signaling on pancreatic cancer desmoplasia has been reviewed elsewhere, and will not be repeated here[41]. Moreover, rooted from genetic alterations, many cytokines, growth factors, and their receptors as well as the associated signaling pathways are involved in the development and maintenance of PDAC[31], reinforcing the heterogeneous features of this deadly disease. While genetic alterations during tumor development are well characterized, changes in PDAC metastasis are not well studied. Lack of typical symptoms at early stages, the complicated and heterogeneous genetic makeup of the tumor, the existence of extensive stroma and less well characterized metastatic tumors all increase the difficulty to make clinical advances. In the rest of the review, we will focus on the role of Hh signaling in pancreatic cancer.
Shh signaling and pancreatic cancer
Hh signaling in pancreas development
Activation of the Hh pathway is necessary for early embryonic specification of the gastrointestinal tract, but downregulation of the Hh pathway is critical for pancreatic development. Ectopic expression of Hh or aberrant activation of this pathway at the onset of pancreas organogenesis results in gain of tissues with duodenal properties and loss of pancreatic tissue[42,43], whereas the inactivation of Hh pathway promotes the development of pancreatic tissue[44,45]. In adult pancreas, the activity of the Hh pathway is very limited and restricted to beta-cells of the endocrine pancreas in regulation of insulin production[46], but is also required for regeneration of the exocrine pancreas under circumstances such as injury or disease[47].
Hh signaling in pancreatic cancer
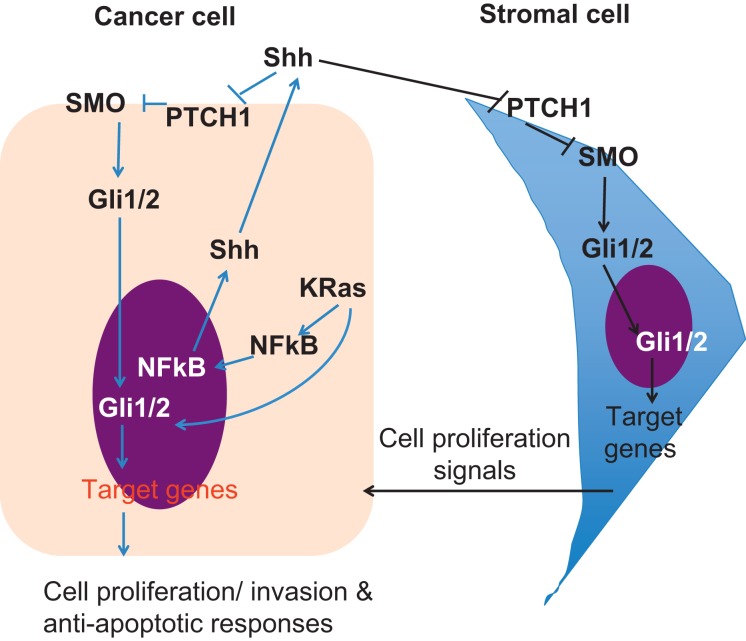
The aberrant activation of the Hh pathway in human pancreatic cancer was first reported by two independent studies[48,49]. Overexpression of Shh is observed in both pre-invasive and invasive epithelium of 70% of human pancreatic cancer samples, and detectable as early as PanIN1 and throughout all disease progression, but is absent in normal pancreas[48]. Conversely, aberrant Hh ligand expression has been identified in the majority of pancreatic cancer cell lines. This observation in human PDAC was also confirmed in a genetically engineered mouse model[50]. The aberrant expression of Shh is directly associated with oncogenic Kras expression in PDAC. Ectopic expression of oncogenic KrasG12D in normal human pancreatic ductal cells leads to increase of Shh transcript[51], indicating that Shh is a downstream effector of oncogenic KrasG12D in pancreatic cancer development. It was further shown that NF-κB is constitutively active in pancreatic cancer[52], and Shh is a target gene of NF-κB[53,54]. The human SHH promoter region contains putative NF-κB binding sites and activation of NF-κB can promote the transcriptional activity of Shh in cell-based and in vivo models[54]. Moreover, oncogenic Kras is known to be an activator for NF-κB transcriptional activity[55,56]. Thus, it is possible that oncogenic Kras promotes Shh expression via NF-κB signaling (Fig. 2).
Fig. 2. Hh signaling in the cancer and stromal cells.
In the cancer cell, Shh expression is induced by Kras and NFkB pathways. As a result, Shh can either activate Hh signaling in the cancer cell or the stromal cell, through canonical Hh signaling. In addition, other signaling pathways, such as Kras, can also induce Gli transcriptional activity (non-canonical Hh signaling) in the tumor compartment. As a result of Hh signaling activation, cancer cells will be more proliferative, more invasive and more resistant to apoptosis. Conversely, Hh signaling activation in the stromal cells can feedback to stimulate cancer cell proliferation.
Despite the above promising data, recent studies indicate that the roles of Hh pathway for pancreatic cancer may not be that simple. Initially, it was thought that overexpressed Shh by cancer or pre-cancer cells promotes PDAC by activation of Hh signaling in the stroma or in the tumor proper, and application of Hh inhibitors will bring hope for patients with pancreatic cancer. However, gene knockout of Smo in the pancreas has no effects on Kras-mediated pancreatic cancer development[57], and removal of stromal Hh signaling actually accelerates Kras-mediated tumor development[58], a result opposite to the prediction. Below we will discuss activation and function of Hh signaling in the stroma and cancer cells of PDAC (Fig. 2).
Paracrine hh signaling in tumor stroma
One of the notorious features of PDAC is desmoplasia, characterized by activation and proliferation of fibroblasts and production of collagens, laminin, and fibronectin by stromal cells. Shh ligand secreted from cancerous epithelial cells can activate Smo-dependent signaling in adjacent stromal cells according to the canonical Hh pathway, leading to desmoplasia[57,59,60]. Fibroblasts in tumor microenvironment, also named cancer-associated fibroblasts (CAFs), are widely considered to promote cancer development, and this theory is also evidenced in PDAC. Co-culture of fibroblasts, isolated from resected pancreatic adenocarcinoma samples, increased proliferation, migration, invasion, and colony formation of cancer cells. Fibroblasts also increases gemcitabine resistance in vitro and promoted tumor growth and metastasis in vivo[61]. Using mouse embryonic fibroblasts (MEFs) as a substitute for CAFs, the growth of tumor after co-injection with SMO-deficient MEFs was much slower compared with those from cancer cells plus wild type MEFs[60]. Furthermore, orthotopic xenograft of pancreatic tumor cell line ectopically expressing Shh induces primary tumor size and promotes metastasis[62]. Taken together, all these data demonstrate that epithelium-derived Shh is a major regulator of fibrosis in PDAC, and the activated stroma promotes tumor in PDAC progression. In another word, cancer or pre-cancer cells communicate with its surroundings via Shh to create a favorable environment for PDAC development. Pharmacologic blockade of the canonical Hh pathway with Smo antagonist, such as cyclopamine, HhAntag and Shh ligand-blocking antibody 5E1 has been reported to reduce the growth and distal metastases of human pancreatic tumors in immunodeficient mice[48,49,60,62-64], and also in one genetically engineered mouse (GEM) model[51]. These results reinforce the tumor promoting function of Shh.
The desmoplastic feature of PCAC not only facilitates tumor growth but also protect them from chemotherapy. It is proposed that failure to treat this disease by chemotherapy is likely due to an inability of the drugs to penetrate the dense stroma to reach cancer cells. Using a KPC mouse model (Pdx1-Cre; LSL-KrasG12D; Trp53R172H/+ or Pdx1-Cre; LSL-KrasG12D; Trp53R270H/+), Olive and colleagues found that tumors contain an extensive stroma and poor vascular density and lead to the limitation of the chemotherapeutic agent delivery and reduction of the effectiveness of chemotherapy[65]. SMO inhibitor treatment can decrease the fibroblastic components and transiently increases blood perfusion in the tumor by increasing vasculature density. Combination of SMO antagonist and gemcitabine leads to increased gemcitabine accumulation in the tumor, leading to enhanced mouse survival[65]. These studies further support that elimination of desmoplasia by Shh inhibitors in PDAC will result in effective delivery of chemotherapeutic agents to the tumor, and thus better clinical outcomes.
However, these promising data fail to lead to better outcomes in clinical trials. Clinical trials using Smo inhibitors in PDAC patients have shown little to no efficacy when combined with gemcitabine[66]. Another phase II clinical trial of SMO inhibitor IPI-926 in com bination with gemcitabine on PDAC was suspended because patients receiving the combination had a worse outcome when compared to the placebo group (Infinity Corp reports, 2012). Furthermore, recent published studies from two groups revealed that either genetic ablation of Shh in KPC mice or prolonged exposure to Hh inhibitors led to more frequent ADM and PanIN lesions, less well-differentiated, more proliferative and metastatic tumors compared with the control litter-mates[58,67,68]. These dogma-challenging studies indicate that the stromal cells may play a restraining role during PDAC development by promoting differentiation and inhibiting aggressiveness of cancer cells, a mechanism also reported in bladder cancer[69]. Taken together, it is possible that the impact of stroma on pancreatic cancer is highly circumstantial, probably determined by temporal stage of cancer progression. Further studies are definitely needed to delineate the biological function of stroma in PDAC, and more importantly, SMO inhibitor should be more carefully applied in cancer patients before better understanding of stromal functions for cancer development.
Hh signaling in tumor cells
Earlier studies suggested that cancer cell-derived Shh signals both via paracrine fashion to communicate with stromal cells and via autocrine signaling to support self-survival. The evidence for autocrine signaling is that in vivo Hh signaling pathway components such as SMO and PTC are also expressed in PDAC and in pancreatic cancer cell lines[48]. More recent studies revealed that Hh signaling is restricted to the stromal compartment during pancreatic carcinogenesis and PDAC cells do not respond to Hh ligand.
In the PDAC GEM mouse model based on oncogenic Kras expression, conditional deletion of Smo in the same cells has no effects on pancreas development or on the multistage development of PDAC, indicating that the canonical Hh signaling is indispensable for PDAC progression[70]. Expression of SmoM2, an oncogenic Smoothened, using pdx1 promoter-driven cre recombinase does not result in Hh signaling activation, and has no impact on KrasG12V-induced tumor development[57]. SmoM2, however, is able to transduce Hh signaling in several pancreatic cancer cell lines and orthotopic mouse models[59]. Additionally, in a subcutaneous xenograft model, Yauch and colleagues showed that tumors from mouse xenografts displayed significant inhibition of tumor growth after treatment with a SMO inhibitor, followed by decreased expression of mouse Hh target genes without effects on human counterpart[60].
Taken all these data together, it seems that canonical (ligand-dependent) Hh signaling is not activated in the tumor compartment of PDAC. However, it is hard to rule out the possibility of non-canonical Hh signaling in human PDAC and a potential role for Hh signaling in a minor subpopulation of epithelial tumor cells, such as cancer initiating cells. In our studies, we found that Smo signaling inhibition in orthotopic xenografts of human pancreatic cancer almost completely suppresses Hh signaling in the stromal cells but only reduces 50% of the Hh signaling activity in cancer cells as indicated by Hh target gene expression (our unpublished data). These results indicate the coexistence of canonical and non-canonical Hh signaling in pancreatic cancer cells. We also found that Smo signaling inhibition in vitro reduces stem cell population, suggesting a role of ligand-dependent Hh pathway in the maintenance of cancer stem cell population in PDAC[71]. Recently, Sharma and colleagues also demonstrated that NVP-BEZ-235, another Smoothened inhibitor, can also inhibit the self-renewal of pancreatic cancer stem cells (CSCs) by suppressing the ligand dependent Hh signaling pathway[72]. Thus, Hh may play different roles in different cell types within the same tumor.
Although the involvement of the upstream part of the canonical Hh signaling pathway in pancreatic cancer cells is controversial, Gli proteins, the downstream transcription factors, do play a role in pancreatic cancer development. Nolan-Stevaux et al.[70] demonstrated that conditional deletion of Smo doesn’t affect Gli1 expression in cancer cells, indicating that Gli transcription in cancer cells is regulated through non-canonical Hh signaling. In other studies, Rajurkar et al. showed that targeted ectopic expression of GLI1 in the pancreatic cells accelerates PDAC initiation by mutant Kras[73]. Furthermore, inhibition of Gli transcriptional activity by dominant negative Gli3 reduced the incidence of Kras-driven PanINs and PDAC, indicating the importance of Gli transcription factors in pancreatic tumorigenesis[73]. Recently, it has been found that GLI1 promotes the growth and migration of pancreatic cancer cells via regulation of the transcription of eukaryotic translation initiation factor 5A2 (EIF5A2)[74].
Kras activating mutation is almost universal in sporadic PDAC, and it is reported that the Kras-MEK-ERK cascade increases Gli transcriptional activity. Ectopic expression of oncogenic Kras in normal human pancreatic cell line HPDE-c7 or BXPC3, a pancreatic cancer cell line with wild type Kras, increases transcription activity of Gli molecules[9,70]. Depletion of oncogenic Kras with specific mutant Kras-targeted siRNAs inhibits Gli transcription activity, as indicated by expression of Gli1 and Ptch1 in PDAC cell lines[9]. It is not clear how the RAS/RAF/MEK cascade affects Gli1 transcriptional activity remains to be elucidated. It is known that Gli transcriptional activity is regulated by the pattern of Gli phosphorylation[75]. Ser130 of Gli1 protein can be phosphorylated by Erk2[76], but it is not clear whether this mechanism is responsible for Gli1 function in pancreatic cancer. In the mouse model of pancreatic cancer, after Smo knockout, TGFβ treatment causes marked elevation of Gli1 and Gli3[70]. Other ligand-independent Hh signaling mechanisms in pancreatic cancer include altered expression of the co-receptor for Hh ligands[77] and epigenetic regulation of Hh signaling molecules HIP and PTCH1[78,79].
Taken together, increasing evidence indicates that the transcription activity of Gli protein may be directly regulated by phosphorylation of the Kras-MEK-ERK cascade in the tumor compartment. On the other hand, ligand-dependent Hh signaling may be responsible for Hh signaling activation in the tumor stroma.
Perspectives
It becomes clear that Hh signaling is activated in both the tumor stroma and in the tumor compartment in pancreatic cancer. However, the mechanisms underlying Hh signaling activation in these two compartments are not the same. While ligand-dependent Hh signaling is mainly responsible for stromal Hh signaling, both canonical and non-canonical Hh signaling occurs in the tumor compartment. In addition to different types of Hh signaling activation, the roles of Hh signaling for pancreatic cancer development, progression and metastasis are not well studied. The poorly understood biology of Hh signaling in pancreatic cancer may account for the failed clinical trials using Smo signaling inhibitors.
With further efforts in deciphering the Hh signaling mechanisms in pancreatic cancer, we predict a new wave of novel strategies to suppress Hh signaling. To that end, we believe that efforts are needed to answer the following questions: 1) What is the role of stromal Hh signaling for tumor development of pancreatic cancer? 2) What is the best way to suppress Hh signaling in the tumor compartment? 3) In addition to tumor development, is Hh signaling responsible for pancreatic cancer metastasis? 4) Does the current GEM model (KPC) recapitulate all the features of PDAC in the humans or only a subset of them?
Acknowledgements
Current research in my laboratory is supported by grants from the National Cancer Institute CA155086, Riley Children’s Foundation, Jeff Gurdon Children’s Research Foundation and Wells Center for Pediatric Research. Due to space limit, we cannot include many important findings in this review but want to take this opportunity to thank all the investigators in this field for their works.
References
- [1].Jiang J, Hui CC. Hedgehog signaling in development and cancer[J]. Dev Cell, 2008, 15(6): 801-812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Varjosalo M, Taipale J. Hedgehog: functions and mechanisms[J]. Genes Dev, 2008, 22(18): 2454-2472. [DOI] [PubMed] [Google Scholar]
- [3].Yang L, Xie G, Fan Q, et al. Activation of the hedge-hog-signaling pathway in human cancer and the clinical implications[J]. Oncogene, 2010, 29(4): 469-481. [DOI] [PubMed] [Google Scholar]
- [4].Goetz SC, Ocbina PJ, Anderson KV. The primary cilium as a Hedgehog signal transduction machine[J]. Methods Cell Biol, 2009, 94: 199-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wong SY, Reiter JF. The primary cilium at the crossroads of mammalian hedgehog signaling[J]. Curr Top Dev Biol, 2008, 85: 225-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Eggenschwiler J. Hedgehog signaling and the cilium: in the zone[J]. Dev Cell, 2012, 23(4): 677-678. [DOI] [PubMed] [Google Scholar]
- [7].He M, Subramanian R, Bangs F, et al. The kinesin-4 protein Kif7 regulates mammalian Hedgehog signalling by organizing the cilium tip compartment[J]. Nat Cell Biol, 2014, 16(7): 663-672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Hui CC, Angers S. Gli proteins in development and disease[J]. Annu Rev Cell Dev Biol, 2011, 27: 513-537. [DOI] [PubMed] [Google Scholar]
- [9].Ji Z, Mei FC, Xie J, et al. Oncogenic KRAS activates hedgehog signaling pathway in pancreatic cancer cells[J]. J Biol Chem, 2007, 282(19): 14048-14055. [DOI] [PubMed] [Google Scholar]
- [10].Seto M, Ohta M, Asaoka Y, et al. Regulation of the hedge-hog signaling by the mitogen-activated protein kinase cascade in gastric cancer[J]. Mol Carcinog, 2009, 48(8): 703-712. [DOI] [PubMed] [Google Scholar]
- [11].Dennler S, Andre J, Alexaki I, et al. Induction of sonic hedgehog mediators by transforming growth factor-beta: Smad3-dependent activation of Gli2 and Gli1 expression in vitro and in vivo[J]. Cancer Res, 2007, 67(14): 6981-6986. [DOI] [PubMed] [Google Scholar]
- [12].Stecca B, Mas C, Clement V, et al. Melanomas require HEDGEHOG-GLI signaling regulated by interactions between GLI1 and the RAS-MEK/AKT pathways[J]. Proc Natl Acad Sci U S A, 2007, 104(14): 5895-5900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Cai Q, Li J, Gao T, et al. Protein kinase Cdelta negatively regulates hedgehog signaling by inhibition of Gli1 activity[J]. J Biol Chem, 2009, 284(4): 2150-2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Siegel R, Ma J, Zou Z, et al. Cancer statistics, 2014[J]. CA Cancer J Clin, 2014, 64(1): 9-29. [DOI] [PubMed] [Google Scholar]
- [15].Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States[J]. Cancer Res, 2014, 74(11): 2913-2921. [DOI] [PubMed] [Google Scholar]
- [16].Vogelzang NJ, Benowitz SI, Adams S, et al. Clinical cancer advances 2011: Annual Report on Progress Against Cancer from the American Society of Clinical Oncology[J]. J Clin Oncol, 2012, 30(1): 88-109. [DOI] [PubMed] [Google Scholar]
- [17].Gudjonsson B. Cancer of the pancreas. 50 years of surgery[J]. Cancer, 1987, 60(9): 2284-2303. [DOI] [PubMed] [Google Scholar]
- [18].Neoptolemos JP, Stocken DD, Friess H, et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer[J]. N Engl J Med, 2004, 350(12): 1200-1210. [DOI] [PubMed] [Google Scholar]
- [19].Oettle H, Post S, Neuhaus P, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients under going curative-intent resection of pancreatic cancer: a randomized controlled trial[J]. JAMA, 2007, 297(3): 267-277. [DOI] [PubMed] [Google Scholar]
- [20].Neoptolemos JP, Stocken DD, Bassi C, et al. Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection: a randomized controlled trial[J]. JAMA, 2010, 304(10): 1073-1081. [DOI] [PubMed] [Google Scholar]
- [21].Hruban RH, Maitra A, Kern SE, et al. Precursors to pancreatic cancer[J]. Gastroenterol Clin North Am, 2007, 36(4): 831-849, vi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hruban RH, Takaori K, Klimstra DS, et al. An illustrated consensus on the classification of pancreatic intraepithelial neoplasia and intraductal papillary mucinous neo-plasms[J]. Am J Surg Pathol, 2004, 28(8): 977-987. [DOI] [PubMed] [Google Scholar]
- [23].Koorstra JB, Hustinx SR, Offerhaus GJ, et al. Pancreatic carcinogenesis[J]. Pancreatology, 2008, 8(2): 110-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Shi G, DiRenzo D, Qu C, et al. Maintenance of acinar cell organization is critical to preventing Kras-induced acinar-ductal metaplasia[J]. Oncogene, 2013, 32(15): 1950-1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Habbe N, Shi G, Meguid RA, et al. Spontaneous induction of murine pancreatic intraepithelial neoplasia (mPanIN) by acinar cell targeting of oncogenic Kras in adult mice[J]. Proc Natl Acad Sci U S A, 2008, 105(48): 18913-18918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hong SM, Park JY, Hruban RH, et al. Molecular signatures of pancreatic cancer[J]. Arch Pathol Lab Med, 2011, 135(6): 716-727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Kanda M, Matthaei H, Wu J, et al. Presence of somatic mutations in most early-stage pancreatic intraepithelial neo-plasia[J]. Gastroenterology, 2012, 142(4): 730-733 e739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Hingorani SR, Petricoin EF, Maitra A, et al. Preinvasive and invasive ductal pancreatic cancer and its early detection in the mouse[J]. Cancer Cell, 2003, 4(6): 437-450. [DOI] [PubMed] [Google Scholar]
- [29].Hezel AF, Kimmelman AC, Stanger BZ, et al. Genetics and biology of pancreatic ductal adenocarcinoma[J]. Genes Dev, 2006, 20(10): 1218-1249. [DOI] [PubMed] [Google Scholar]
- [30].Wilentz RE, Geradts J, Maynard R, et al. Inactivation of the p16 (INK4A) tumor-suppressor gene in pancreatic ductlesions: loss of intranuclear expression[J]. Cancer Res, 1998, 58(20): 4740-4744. [PubMed] [Google Scholar]
- [31].Schutte M, Hruban RH, Geradts J, et al. Abrogation of the Rb/p16 tumor-suppressive pathway in virtually all pancreatic carcinomas[J]. Cancer Res, 1997, 57(15): 3126-3130. [PubMed] [Google Scholar]
- [32].Caldas C, Hahn SA, da Costa LT, et al. Frequent somatic mutations and homozygous deletions of the p16 (MTS1) gene in pancreatic adenocarcinoma[J]. Nat Genet, 1994, 8(1): 27-32. [DOI] [PubMed] [Google Scholar]
- [33].Maitra A, Adsay NV, Argani P, et al. Multicomponent analysis of the pancreatic adenocarcinoma progression model using a pancreatic intraepithelial neoplasia tissue microarray[J]. Mod Pathol, 2003, 16(9): 902-912. [DOI] [PubMed] [Google Scholar]
- [34].Wilentz RE, Iacobuzio-Donahue CA, Argani P, et al. Loss of expression of Dpc4 in pancreatic intraepithelial neoplasia: evidence that DPC4 inactivation occurs late in neoplastic progression[J]. Cancer Res, 2000, 60(7): 2002-2006. [PubMed] [Google Scholar]
- [35].Biankin AV, Waddell N, Kassahn KS, et al. Pancreatic cancer genomes reveal aberrations in axon guidance pathway genes[J]. Nature, 2012, 491(7424): 399-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Jones S, Zhang X, Parsons DW, et al. Core signaling pathways in human pancreatic cancers revealed by global genomic analyses[J]. Science, 2008, 321(5897): 1801-1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Kawahira H, Scheel DW, Smith SB, et al. Hedgehog signaling regulates expansion of pancreatic epithelial cells[J]. Dev Biol, 2005, 280(1): 111-121. [DOI] [PubMed] [Google Scholar]
- [38].Apelqvist A, Ahlgren U, Edlund H. Sonic hedgehog directs specialised mesoderm differentiation in the intestine and pancreas[J]. Curr Biol, 1997, 7(10): 801-804. [DOI] [PubMed] [Google Scholar]
- [39].Hebrok M, Kim SK, Melton DA. Notochord repression of endodermal Sonic hedgehog permits pancreas development[J]. Genes Dev, 1998, 12(11): 1705-1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Kim SK, Melton DA. Pancreas development is promoted by cyclopamine, a hedgehog signaling inhibitor[J]. Proc Natl Acad Sci U S A, 1998, 95(22): 13036-13041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Thomas MK, Rastalsky N, Lee JH, et al. Hedgehog signaling regulation of insulin production by pancreatic beta-cells[J]. Diabetes, 2000, 49(12): 2039-2047. [DOI] [PubMed] [Google Scholar]
- [42].Fendrich V, Esni F, Garay MV, et al. Hedgehog signaling is required for effective regeneration of exocrine pancreas[J]. Gastroenterology, 2008, 135(2): 621-631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Thayer SP, di Magliano MP, Heiser PW, et al. Hedgehog is an early and late mediator of pancreatic cancer tumorigenesis[J]. Nature, 2003, 425(6960): 851-856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Berman DM, Karhadkar SS, Maitra A, et al. Widespread requirement for Hedgehog ligand stimulation in growth of digestive tract tumours[J]. Nature, 2003, 425(6960): 846-851. [DOI] [PubMed] [Google Scholar]
- [45].Hingorani SR, Wang L, Multani AS, et al. Trp53R172H and KrasG12D cooperate to promote chromosomal instability and widely metastatic pancreatic ductal adenocarcinoma in mice[J]. Cancer Cell, 2005, 7(5): 469-483. [DOI] [PubMed] [Google Scholar]
- [46].Feldmann G, Habbe N, Dhara S, et al. Hedgehog inhibition prolongs survival in a genetically engineered mouse model of pancreatic cancer[J]. Gut, 2008, 57(10): 1420-1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Algul H, Adler G, Schmid RM. NF-kappaB/Rel transcriptional pathway: implications in pancreatic cancer[J]. Int J Gastrointest Cancer, 2002, 31(1-3): 71-78. [DOI] [PubMed] [Google Scholar]
- [48].Nakashima H, Nakamura M, Yamaguchi H, et al. Nuclear factor-kappaB contributes to hedgehog signaling pathway activation through sonic hedgehog induction in pancreatic cancer[J]. Cancer Res, 2006, 66(14): 7041-7049. [DOI] [PubMed] [Google Scholar]
- [49].Kasperczyk H, Baumann B, Debatin KM, et al. Characterization of sonic hedgehog as a novel NF-kappaB target gene that promotes NF-kappaB-mediated apoptosis resistance and tumor growth in vivo[J]. FASEB J, 2009, 23(1): 21-33. [DOI] [PubMed] [Google Scholar]
- [50].Mizumoto Y, Kyo S, Kiyono T, et al. Activation of NF-kappaB is a novel target of KRAS-induced endome-trial carcinogenesis[J]. Clin Cancer Res, 2011, 17(6): 1341-1350. [DOI] [PubMed] [Google Scholar]
- [51].Ling J, Kang Y, Zhao R, et al. KrasG12D-induced IKK2/beta/NF-kappaB activation by IL-1alpha and p62 feed-forward loops is required for development of pancreatic ductal adenocarcinoma[J]. Cancer Cell, 2012, 21(1): 105-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Tian H, Callahan CA, DuPree KJ, et al. Hedgehog signaling is restricted to the stromal compartment during pancreatic carcinogenesis[J]. Proc Natl Acad Sci U S A, 2009, 106(11): 4254-4259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Rhim AD, Oberstein PE, Thomas DH, et al. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma[J]. Cancer Cell, 2014, 25(6): 735-747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Bailey JM, Swanson BJ, Hamada T, et al. Sonic hedge-hog promotes desmoplasia in pancreatic cancer[J]. Clin Cancer Res, 2008, 14(19): 5995-6004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Yauch RL, Gould SE, Scales SJ, et al. A paracrine requirement for hedgehog signalling in cancer[J]. Nature, 2008, 455(7211): 406-410. [DOI] [PubMed] [Google Scholar]
- [56].Hwang RF, Moore T, Arumugam T, et al. Cancer-associated stromal fibroblasts promote pancreatic tumor progression[J]. Cancer Res, 2008, 68(3): 918-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Bailey JM, Mohr AM, Hollingsworth MA. Sonic hedge-hog paracrine signaling regulates metastasis and lym phangiogenesis in pancreatic cancer[J]. Oncogene, 2009, 28(40): 3513-3525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Feldmann G, Fendrich V, McGovern K, et al. An orally bioavailable small-molecule inhibitor of Hedgehog signaling inhibits tumor initiation and metastasis in pancreatic cancer[J]. Mol Cancer Ther, 2008, 7(9): 2725-2735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Feldmann G, Dhara S, Fendrich V, et al. Blockade of hedgehog signaling inhibits pancreatic cancer invasion and metastases: a new paradigm for combination therapy in solid cancers[J]. Cancer Res, 2007, 67(5): 2187-2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Olive KP, Jacobetz MA, Davidson CJ, et al. Inhibition of Hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer[J]. Science, 2009, 324(5933): 1457-1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Lee JJ, Perera RM, Wang H, et al. Stromal response to Hedgehog signaling restrains pancreatic cancer progression[J]. Proc Natl Acad Sci U S A, 2014, 111(30): E3091-3100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Ozdemir BC, Pentcheva-Hoang T, Carstens JL, et al. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival[J]. Cancer Cell, 2014, 25(6): 719-734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Shin K, Lim A, Zhao C, et al. Hedgehog signaling restrains bladder cancer progression by eliciting stromal production of urothelial differentiation factors[J]. Cancer Cell, 2014, 26(4): 521-533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Nolan-Stevaux O, Lau J, Truitt ML, et al. GLI1 is regulated through Smoothened-independent mechanisms in neoplastic pancreatic ducts and mediates PDAC cell survival and transformation[J]. Genes Dev, 2009, 23(1): 24-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Gu D, Liu H, Su GH, et al. Combining hedgehog signaling inhibition with focal irradiation on reduction of pancreatic cancer metastasis[J]. Mol Cancer Ther, 2013, 12(6): 1038-1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Rajurkar M, De Jesus-Monge WE, Driscoll DR, et al. The activity of Gli transcription factors is essential for Kras-induced pancreatic tumorigenesis[J]. Proc Natl Acad Sci U S A, 2012, 109(17): E1038-1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Niewiadomski P, Kong JH, Ahrends R, et al. Gli protein activity is controlled by multisite phosphorylation in vertebrate Hedgehog signaling[J]. Cell Rep, 2014, 6(1): 168-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Whisenant TC, Ho DT, Benz RW, et al. Computational prediction and experimental verification of new MAP kinase docking sites and substrates including Gli transcription factors[J]. PLoS Comput Biol, 2010, 6(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Mathew E, Zhang Y, Holtz AM, et al. Dosage-dependent regulation of pancreatic cancer growth and angiogenesis by hedgehog signaling[J]. Cell Rep, 2014, 9(2): 484-494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Olsen CL, Hsu PP, Glienke J, et al. Hedgehog-interacting protein is highly expressed in endothelial cells but down-regulated during angiogenesis and in several human tumors[J]. BMC Cancer, 2004, 4(43). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Pan S, Dong Q, Sun LS, et al. Mechanisms of inactivation of PTCH1 gene in nevoid basal cell carcinoma syndrome: modification of the two-hit hypothesis[J]. Clin Cancer Res, 2010, 16(2): 442-450. [DOI] [PubMed] [Google Scholar]