Abstract
This retrospective study investigated the impact of endplate fracture on postoperative vertebral height loss and kyphotic deformity in 144 patients with osteoporotic vertebral compression fracture (OVCF), who received balloon kyphoplasty. Patients were divided into four groups: Group 1 had no superior endplate fracture, Group 2 had fractures on the anterior portion of the superior endplate, Group 3 had fractures on the posterior portion of the superior endplate, and Group 4 had complete superior endplate fractures. Anterior and middle vertebral body height, vertebral compression ratio, vertebral height loss rate, and kyphosis Cobb angle of each patient were measured and visual analogue scale (VAS) and Oswestry disability index (ODI) scores were recorded. The anterior vertebral height and kyphosis deformity of all groups significantly improved after the surgery, whereas substantial anterior vertebral height loss and increased Cobb angle were observed in all patients at the last follow-up. Although the vertebral height loss rate and the Cobb angle in Group 2, 3 and 4 were larger compared with Group 1 at the last follow-up, only the vertebral height loss rate in Group 4 and the increase in the Cobb angle in Group 2 and 4 were statistically different from those in Group 1. The VAS and ODI scores in all groups measured after the surgery and at the last follow-up were significantly lower compared with preoperative scores, but there was no significant difference among these groups. Balloon kyphoplasty significantly improved vertebral fracture height and kyphosis. Vertebral height loss and increased kyphotic deformity were observed in OVCF patients with endplate fractures after the surgery. Postoperative aggravation of kyphosis was observed in Group 2. Furthermore, severe vertebral height loss and increased kyphotic deformity were confirmed in Group 4 after the surgery. Our results suggested that postoperative vertebral height loss and aggravation of kyphosis may be associated with biomechanical changes in the vertebral body caused by endplate fracture. Therefore, surgery should not only restore compressed vertebral body height and correct kyphosis, but also correct the deformity of endplate to achieve an effective treatment of OVCF patients with endplate fracture.
Keywords: osteoporotic vertebral compression fracture, balloon kyphoplasty, endplate fracture, height loss, kyphosis
Introduction
Vertebral compression fracture is the most common complication for patients with osteoporosis, which often cause severe back pain, vertebral height loss, and kyphosis[1]. Although percutaneous vertebroplasty can effectively relieve pain and has received satisfactory results in the treatment of osteoporotic vertebral compression fracture (OVCF), it has several drawbacks including high cement leakage rate, and inability to restore vertebral body height and correct kyphosis. Balloon kyphoplasty is developed on the basis of percutaneous vertebroplasty, during which an expandable balloon is used to restore height. The procedure effectively reduces the occurrence of bone cement leakages, recovers vertebral body height, and corrects spinal kyphosis compared with other surgical approaches[2-3]. Nevertheless, the incidence of postoperative complications such as vertebral height loss, aggravation of kyphosis and vertebral fractures of adjacent segments remains high[4].
In recent years, with extensive application of balloon kyphoplasty and development in spinal biomechanics, the injection of polymethyl methacrylate (PMMA) increases the strength of fractured vertebral segments, but changes biomechanical distribution of adjacent segments, which may cause postoperative fracture of adjacent segments[5-8]. However, few studies have been performed to investigate the mechanisms of vertebral height loss and aggravation of kyphosis after balloon kyphoplasty. Furthermore, these studies even yield conflicting results. In a follow-up study by Dansie et al. of 51 OVCF patients treated with percutaneous vertebroplasty, the postoperative loss rate of anterior vertebral height was 18.0%[9], whereas it was 63.0% in another similar study[10]. It has been reported that vertebral height loss and aggravation of kyphosis after balloon kyphoplasty may be associated with preoperative severe osteoporosis, insufficient PMMA injection, necrosis of fractured vertebral body, and excessive restoration of vertebral height[11]. Nevertheless, mechanisms behind vertebral height loss and aggravation of kyphosis after balloon kyphoplasty remain inconclusive.
Postoperative vertebral height loss and aggravation of kyphosis of balloon kyphoplasty may cause chronic low back pain, affecting the surgical outcome. Silverman et al. have shown that kyphosis reduces daily activities and quality of life, and even increases mortality[12]. Therefore, it is important to study the mechanism of vertebral height loss and aggravation of kyphosis after balloon kyphoplasty for effective prevention of postoperative complications. The vertebral endplate bears 40%–75% of the pressure of the vertebral body, and is directly involved in transferring pressure from the vertebral disc to the vertebral body[13]. Biomechanical studies have confirmed that even a slight morphological change in endplate can lead to a dramatic reduction in motor function of the vertebral body[14]. OVCF is often accompanied by vertebral endplate fracture, which causes changes in endplate stress distribution. Such biomechanical changes in fractured vertebral body may be closely associated with vertebral height loss and kyphosis after balloon kyphoplasty. In this retrospective study, the impact of degree of endplate fracture on postoperative vertebral height loss and kyphotic deformity was investigated in OVCF patients treated with balloon kyphoplasty.
Patients and methods
Patients
A retrospective analysis was performed on patients with OVCF who received balloon kyphoplasty in the Division of Spinal Surgery at the First Affiliated Hospital of Nanjing Medical University from January 2009 to December 2012. Patients were selected according to the following criteria: 1) fresh single osteoporotic thoracolumbar vertebral compression fractures with high signal on MRI fat-suppressed T2 image, 2) with severe back pain which could not be resolved by conservative therapy, and 3) follow up duration at least one year. Exclusion criteria were 1) non-osteoporotic vertebral compression fractures such as pathologic fracture and thoracolumbar burst fracture, 2) dural sac and nerve root compression caused by incomplete posterial or collapsed vertebral body, 3) the degree of vertebral compression over 75%, and 4) infection or clotting dysfunction. Bone density of each patient was examined by X-ray, MRI, CT, and dual-energy X-ray.
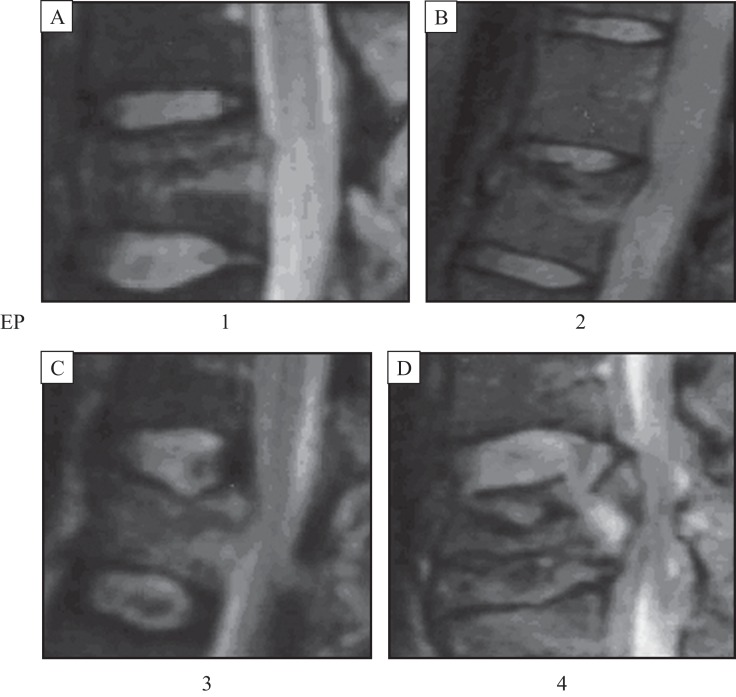
Patients were divided into the following four groups according to the preoperative degree of superior vertebral endplate fracture by MRI[15] (Fig. 1): Group 1 had no superior endplate fracture, Group 2 had fractures on the anterior portion of the superior endplate (showing discontinuous linear low-signal on MRI T1 images and discontinuous linear high-signal on MRI T2 or fat-suppressed images, and excluding old fractures and Schmorl's nodules), Group 3 had fractures on posterior portion of superior endplate, and Group 4 had complete superior endplate fractures.
Fig. 1. Grouping according End-plate Fracture. Patients were divided into four groups according to the preoperative degree of superior vertebral endplate fracture detected with MRI: Group 1 without any superior endplate fracture (A); Group 2 with fractures on anterior portion of superior endplate (showing discontinuous linear low-signal on MRI T1 images and discontinuous linear high-signal on MRI T2 or fat-suppressed images, and excluding old fractures and Schmorl's nodules) (B); Group 3 with fractures on posterior portion of superior endplate (C); Group 4 with complete superior endplate fractures (D).
This study was approved and supervised by the Medical Ethics Committee at the First Affiliated Hospital of Nanjing Medical University.
Balloon kyphoplasty
All patients underwent surgical procedures under general anesthesia. The whole procedure was performed with a C-arm perspective machine. Core needles were inserted at 3:00 on the right side and 9:00 on the left side of the pedicle shadow until the lateral tip reached the posterior wall of the vertebral body, and the anteroposterior tip reached the medial edge of the pedicle shadow. The core needle was removed, and guide pin, expansion sleeve and working casing were placed inside the needle to establish a working channel in fractured vertebral body.
An expandable balloon was implanted in the vertebral body and dilated until vertebral body height was restored. The balloon was removed and PMMA cement [powder (g) : liquid (mL) = 2:1] was slowly injected into the vertebral body. The working channel was removed after PMMA was completely solidified, and the incision was sutured.
Assessment of efficacy
Imaging evaluation
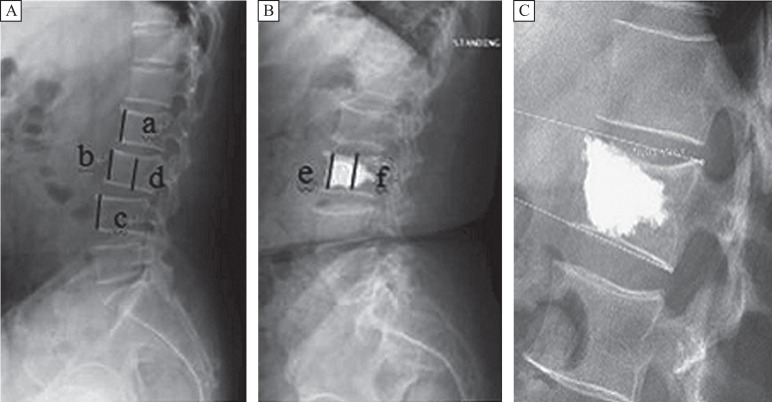
Anterior and middle vertebral height, anterior vertebral height ratio, anterior vertebral height restoration rate, anterior vertebral height loss rate, the Cobb angle, kyphosis correction degree, and the increase in Cobb angle were determined by X-ray examination before and after the surgery, and at the last follow-up visit. Anterior vertebral height ratio was calculated as the ratio of anterior height of fractured vertebral body to the average anterior height of adjacent vertebral bodies. If an old fracture or deformity existed in either of the adjacent vertebral bodies, the next adjacent vertebral body was measured. Anterior vertebral height restoration rate was calculated as the difference between pre-and postoperative anterior vertebral height ratios, and anterior vertebral height loss rate was calculated as the difference between anterior vertebral height ratios obtained immediately after the surgery and at the last follow-up. Cobb angle was defined as the angle formed between lines drawn parallel to the respective superior and inferior endplates of fracture. Kyphosis correction degree was calculated as the difference between pre- and postoperative Cobb angles. Increase in Cobb angle was the difference between Cobb angles measured immediately after the surgery and at the last follow-up (Fig. 2). Leakage of bone cement into intervertebral space in each group was also recorded (Fig. 3).
Fig. 2. Imaging evaluation of osteoporotic vertebral compression fractures with balloon kyphoplasty. Data were determined as follows: Initial anterior vertebral body height (Y)=the average anterior height of adjacent vertebral bodies, calculated as (a+c)/2. Anterior vertebral height restoration rate=(postoperative anterior vertebral height–preoperative anterior vertebral height)/initial anterior vertebral body height, (e-b)/Y*100%. Central vertebral height restoration rate=(f-d)/Y*100%. Cobb angle was defined as the angle formed between the lines drawn parallel to respective superior and inferior endplates of the fracture as shown in Fig. 2C.
Evaluation of efficacy
Visual analogue scale (VAS) and Oswsetry disability index (ODI) were assessed to reveal the degree of pain and the level of activity of patients before and after the surgery, and at the last follow-up visit.
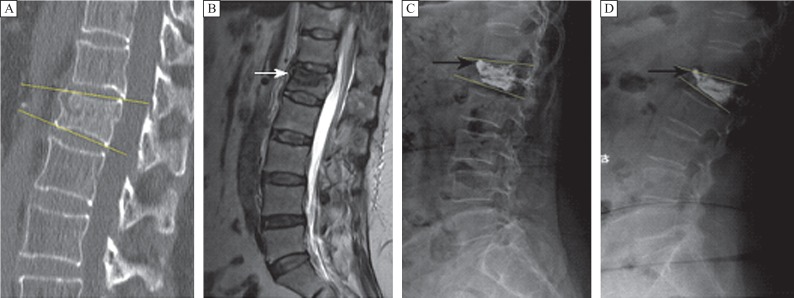
Fig. 3. Images of the lumbar vertebra of a 62-year-old female patient. A: T score in bone density test was -3.2, preoperative anterior vertebral height and Cobb angle was 21.5 mm and 18.0°, respectively. B: The MRI image of showing L1 lumbar vertebral compression fracture with anterior endplate fracture (marked by a white arrow). C: X-ray image showing leakage of bone cement into intervetebral space via anterior endplate fracture (marked by a black arrow). Preoperative anterior vertebral height and Cobb angle was 23.5 mm and 11.8°, respectively. D: X-ray image at 13 months after the surgery showing that anterior vertebral height and Cobb angle was 10.4 mm and 22.1°, respectively. Yellow lines represent Cobb angle.
Statistical analysis
All data were presented as mean ± SD, and analyzed using SPSS19.0 software package (SPSS Inc., Chicago, IL, USA). Age, bone density, duration of symptoms, the amount of bone cement, anterior vertebral height, vertebral column height, anterior vertebral height restoration rate, anterior vertebral height loss rate, Kobb angle, kyphosis correction degree, increase in Kobb angle, VAS and ODI scores of patients in different groups were compared by analysis of variance (ANOVA). P<0.05 was considered to be statistically significant.
Results
General information of patients
A total of 144 patients including 30 males and 114 females with a mean age of 69.1 ± 8.6 (range, 49-86 years) years were enrolled in this study. The number of patients in Group 1, 2, 3 and 4 was 56, 44, 28 and 16, respectively. While the mean age of Group 4 (73.6±10.0) was significantly higher than Group 1 (69.8±8.6, P<0.05), Group 2 (66.8±8.9, P<0.05), and Group 3 (68.9±6.6, P<0.05), and there were no significant differences in the mean age among Group 1, 2 and 3 (Table 1).
Table 1. General information of patients.
| Parameter | Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|---|
| The number of cases | 56 | 44 | 28 | 16 |
| Age | 69.8±8.6 | 66.8±8.9 | 68.9±6.6 | 73.6±10.0 |
| Gender (male/female) | 12/44 | 10/34 | 4/24 | 4/12 |
| Bone density (T score) | −2.9±0.5 | −2.9±0.2 | −3.0±0.3 | −2.9±0.4 |
| Thoracic vertebra | 28/56 | 14/44 | 10/28 | 0/16 |
| Lumbar vertebra | 28/56 | 30/44 | 18/28 | 16/16 |
| Duration of symptoms (days) | 9.2±6.9 | 9.1±4.9 | 17.4±13.5 | 17.0±10.2 |
| The amount of bone cement (mL) | 5.1±0.6 | 5.2±0.5 | 5.0±0.6 | 5.1±0.4 |
| Duration of follow up (months) | 14.3±2.5 | 14.0±2.3 | 13.2±1.5 | 13.0±1.0 |
Radiological outcomes
Preoperative anterior vertebral height in the four groups was 20.7±3.3 mm, 20.9±3.7 mm, 19.6±3.0 mm, and 19.7±3.8 mm, respectively, and preoperative Cobb angles were 13.7±6.2°, 12.5±3.6°, 13.1±6.7°, and 14.1±6.4°, respectively. Anterior vertebral height of each group (24.3±2.5 mm, 25.4±2.9 mm, 24.3±3.2 mm, and 23.8±3.8 mm, respectively, P<0.05) was significantly restored and the Cobb angle was significantly reduced (8.2±5.3°, 6.9±3.4°, 6.7±3.8°, and 9.5±6.0°, respectively, P<0.05) right after the surgery. Although the anterior vertebral height in each group (21.7±3.1 mm, 22.2±4.0 mm, 21.1±3.5 mm, and 19.0±3.9 mm, respectively) measured at the last follow-up was lower than those measured immediately after the surgery, anterior vertebral height in Group 1, 2 and 3 at the last follow-up was higher than preoperative height. There were no significant differences between the anterior vertebral height in Group 4 measured before surgery and at the last follow-up.
Cobb angle of each group at the last follow-up (11.1±5.8°, 11.8±3.6°, 10.9±6.1°, and 15.6±5.1°, respectively) was significantly higher than that measured immediately after surgery, whereas the angles in Group 2, 3 and 4 at the last follow-up were not significantly different from preoperative angles (Table 2). In addition, there were no significant differences in postoperative anterior vertebral height restoration rates among each group (14.4±9.5%, 16.4±10.0%, 18.8±10.0%, and 14.3±9.7%, respectively). Vertebral height loss rate at the last follow-up was 10.4±8.5%, 11.6±11.4%, 13.0±7.4%, and 16.7±8.8%, respectively, and a significant difference in loss rate existed only between EP1 and Group 4 (P<0.05). There were no significant differences among postoperative kyphosis correction degrees (5.6±4.6, 5.7±3.7, 6.4±6.3, and 4.7±3.4, respectively), and increase of Cobb angle at the last follow-up was 2.9±3.0, 4.9±2.9, 4.2±3.7, and 6.1±4.4, respectively, with significant differences between Group 1 and 2 (P<0.05), and between Group 1 and Group 4 (P<0.05) (Table 3).
Table 2. Vertebral body height and Cobb angle in each group determined before and right after surgery, and at the last follow-up.
| Parameter | Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|---|
| N | 56 | 44 | 28 | 16 |
| Preoperative anterior vertebral body height (mm) | 20.7±3.3 | 20.9±3.7 | 19.6±3.0 | 19.7±3.8 |
| Postoperative anterior vertebral body height (mm) | 24.3±2.5 | 25.4±2.9 | 24.3±3.2 | 23.8±3.8 |
| Anterior vertebral body height at the last follow-up (mm) | 21.7±3.1 | 22.2±4.0 | 21.1±3.5 | 19.0±3.9 |
| Preoperative Cobb angle | 13.7±6.2 | 12.5±3.6 | 13.1±6.7 | 14.1±6.4 |
| Postoperative Cobb angle | 8.2±5.3 | 6.9±3.4 | 6.7±3.8 | 9.5±6.0 |
| Cobb angle at the last follow-up | 11.1±5.8 | 11.8±3.6 | 10.9±6.1 | 15.6±5.1 |
| Difference in vertebral body height (P value) | ||||
| Pre-/post operative | 0.000 | 0.000 | 0.000 | 0.001 |
| Preoperative/last follow-up | 0.012 | 0.003 | 0.001 | 0.314 |
| Postoperative/last follow-up | 0.000 | 0.000 | 0.000 | 0.000 |
| Difference in Cobb angle (P value) | ||||
| Pre-/post operative | 0.000 | 0.000 | 0.000 | 0.000 |
| Preoperative/last follow-up | 0.001 | 0.197 | 0.121 | 0.210 |
| Postoperative/last follow-up | 0.000 | 0.000 | 0.000 | 0.000 |
Table 3. Vertebral height restoration rate, kyphosis correction degree, and rate of intervertebral bone cement leakage right after surgery, and vertebral height loss.
| Parameter | Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|---|
| Vertebral height restoration rate right after the surgery (%) | 14.4±9.5 | 16.4±10.0 | 18.8±10.0 | 14.3±9.7 |
| Vertebral height loss rate at the last follow-up (%) | 10.4±8.5 | 11.6±11.4 | 13.0±7.4 | 16.7±8.8 |
| Kyphosis correction degree right after the surgery | 5.6±4.6 | 5.7±3.7 | 6.4±6.3 | 4.7±3.4 |
| Increase in Cobb angle at the last follow-up | 2.9±3.0 | 4.9±2.9 | 4.2±3.7 | 6.1±4.4 |
| Rate of intervertebral bone cement leakage right after the surgery (%) | 0(0%) | 9(20.45%) | 3(10.71%) | 6(37.5%) |
The number of cases of intervertebral bone cement leakage was 0 (0%), 9 (20.45%), 3 (10.71%), and 6 (37.5%), respectively.
VAS and ODI scores
There were no significant differences in preoperative VAS and ODI scores among each group. Postoperative VAS and ODI scores in all groups were significantly lower than preoperative scores (Table 4) although there were no significant differences among these groups.
Table 4. VAS and ODI scores before and right after surgery, and at the last follow-up.
| Parameter | Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|---|
| N | 56 | 44 | 28 | 16 |
| Preoperative VAS | 7.9±0.7 | 8.1±0.7 | 8.2±0.8 | 8.3±0.4 |
| Postoperative VAS | 0.9±0.7 | 0.4±0.7 | 0.7±0.8 | 0.5±0.7 |
| VAS at the last follow-up | 0.5±0.6 | 0.3±0.5 | 0.2±0.4 | 0.4±0.5 |
| Preoperative ODI | 63.5±5.0 | 65.1±4.0 | 65.9±4.9 | 65.1±5.9 |
| Postoperative ODI | 9.5±3.7 | 9.7±2.2 | 11.8±4.1 | 10.9±2.2 |
| ODI at the last follow-up | 6.0±2.6 | 7.5±2.4 | 6.9±2.1 | 6.9±2.7 |
| Difference in VAS (P value) | ||||
| Pre-/post operative | 0.000 | 0.000 | 0.000 | 0.000 |
| Preoperative/last follow-up | 0.000 | 0.000 | 0.000 | 0.000 |
| Postoperative/last follow-up | 0.000 | 0.244 | 0.000 | 0.164 |
| Difference in ODI (P value) | ||||
| Pre-/post operative | 0.000 | 0.000 | 0.000 | 0.000 |
| Preoperative/last follow-up | 0.000 | 0.000 | 0.000 | 0.000 |
| Postoperative/last follow-up | 0.000 | 0.000 | 0.000 | 0.000 |
Discussion
OVCF is the most common complication in patients with osteoporosis, and often causes severe back pain, vertebral height loss, and kyphosis[1]. Balloon kyphoplasty is developed on the basis of percutaneous vertebroplasty, during which an expandable balloon is used to restore vertebral height. It has several advantages over percutaneous vertebroplasty such as low rate of bone cement leakage, restoration of vertebral body height, and correction of kyphosis[8]. However, problems including the loss of vertebral height, aggravation of kyphosis, and fracture in adjacent vertebral segments often occur after surgery[4]. Postoperative vertebral height loss and kyphosis always lead to chronic low back pain, which reduces daily activities and life quality, and even increases mortality rate[14]. Therefore, it is important to study the mechanism of postoperative vertebral height loss and aggravation of kyphosis for effective prevention of complications after the surgery.
OVCF is often accompanied by vertebral endplate fracture. Vertebral endplate bears 40%-75% of the pressure of the vertebral body, and is directly involved in transferring the pressure from the vertebral disc to the vertebral body[9]. Biomechanical studies have demonstrated that even a slight morphological change in endplate can lead to a dramatic reduction in motor function of the vertebral body[14]. While the maximum stress was found in the center of healthy endplate and underlying cancellous bone due to axial pressure[16], and found in the lateral areas of the endplates of elderly patients due to disc degeneration, osteoporosis, and etc[17]. It was also confirmed that the highest effective stress was located in the anterior part of the vertebral body by a 3D finite element dynamic response analysis[18]. In addition, Grangt et al. identified the maximum compressive stress in the posterior-lateral part of the vertebral endplate under normal physiological conditions, but the lowest stress in the central part[19]. Therefore, the stress loaded on the anterior and lateral parts of endplate increases in elderly patients with osteoporosis, while the strength of the anterior and central parts significantly decreases, which makes these parts most commonly prone to fractures when subjected to excessive load. It also explains why the anterior part of endplate is always lower than the posterior part in OVCF patients[18]. Postoperative vertebral height loss is often resulted from failure to completely correct deformity of endplate during surgery which causes increased stress in the surrounding part of the vertebral body in patients with both vertebral and endplate fractures. Furthermore, Oner, et al. showed that the aggravation of vertebral kyphosis might be related to the embedding of disc in the vertebral body or endplate after endplate fracture[15]. Therefore, the vertebral height loss and kyphosis after balloon kyphoplasty are closely associated with vertebral biomechanical changes caused by changes in stress distribution of endplate after a fracture. Our study demonstrated that postoperative vertebral height loss and aggravated kyphosis are associated with endplate fracture. While progressive kyphosis was observed in OCVF patients with endplate fracture especially anterior endplate fracture after the surgery, both severe vertebral height loss and aggravated kyphosis were identified in patients with complete endplate fracture.
The present study demonstrated that endplate fracture caused not only an increased incidence of postoperative vertebral height loss and kyphosis, but also a significant higher rate of bone cement leakage (P<0.05). Previous studies have shown that endplate damages, iatrogenic penetrating injuries, and the lack of a clear gap in the vertebral body are main reasons for the leakage of bone cement into the intervertebral space[20]. In a quantitative study of pressure in the center of vertebral body during PKP surgery by Weisskopf et al., a low pressure was observed when empty vertebral cavity was not completely filled with bone cement, whereas the pressure surged when injecting bone cement into a full cavity and the leakage might easily occur with the presence of endplate fracture[21]. The impact of intervertebral bone cement leakage on the efficacy of outcome in OCVF patients remains quite controversial. Mirovsky et al. showed no association between the leakage and efficacy of surgery[22]. In this study, intervertebral cement leakage did not cause severe symptoms, and VAS and ODI scores improved after surgery and at the last follow-up. We still believe that endplate fracture not only led to aggravated postoperative vertebral height loss and kyphosis, but also caused higher incident of intervertebral cement leakage, further aggravating vertebral height loss and kyphosis. Therefore, intervertebral cement leakage should be avoided during the surgery for OCVF patients with endplate fracture. Bone cement should be filled in anterior column in the vertebral body with anterior fracture that resists the major compression forces to decrease the risk of postoperative compression. In contrast, the vertebral body should be completely filled with bone cement to correct deformity of endplate in patient with compete endplate fracture.
Balloon kyphoplasty can effectively relieve pain, and significantly improve vertebral height and kyphosis. However, problems including postoperative vertebral height loss and kyphosis often occur. Our study demonstrated that endplate fracture was not only associated with increased incidence of postoperative vertebral height loss and kyphosis, but also a significant cause of bone cement leakage. It is important to note that sample sizes are few and have certain influence to the result. Nonetheless, intervertebral cement leakage should be avoided, and endplate deformity should be corrected during surgery for OCVF patients with endplate fracture.
Acknowledgments
This work was supported by National Natural and Science Foundation (81271988), Jiangsu Natural and Science Foundation (BK2012876).
References
- [1].Meunier PJ, Delmas PD, Eastell R, et al. Diagnosis and management of osteoporosis in postmenopausal women: clinical guidelines. International Committee for Osteoporosis Clinical Guidelines[J]. Clin Ther, 1999, 21(6): 1025-1044. [DOI] [PubMed] [Google Scholar]
- [2].Hiwatashi A, Sidhu R, Lee RK, et al. Kyphoplasty versus vertebroplasty to increase vertebral body height: a cadaveric study[J]. Radiology, 2005, 237(3): 1115-1119. [DOI] [PubMed] [Google Scholar]
- [3].Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial[J]. Lancet, 2009, 373(9668): 1016-1024. [DOI] [PubMed] [Google Scholar]
- [4].Black DM, Arden NK, Palermo L, et al. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group[J]. J Bone Miner Res, 1999, 14(5): 821-828. [DOI] [PubMed] [Google Scholar]
- [5].Fribourg D, Tang C, Sra P, et al. Incidence of subsequent vertebral fracture after kyphoplasty[J]. Spine, 2004, 29(20): 2270-2276; discussion 2277. [DOI] [PubMed] [Google Scholar]
- [6].Harrop JS, Prpa B, Reinhardt MK, et al. Primary and secondary osteoporosis' incidence of subsequent vertebral compression fractures after kyphoplasty[J]. Spine, 2004, 29(20): 2120-2125. [DOI] [PubMed] [Google Scholar]
- [7].Belkoff SM, Mathis JM, Jasper LE, et al. An ex vivo biomechanical evaluation of a hydroxyapatite cement for use with vertebroplasty[J]. Spine, 2001, 26(14): 1542-1546. [DOI] [PubMed] [Google Scholar]
- [8].Berlemann U, Ferguson SJ, Nolte LP, et al. Adjacent vertebral failure after vertebroplasty. A biomechanical investigation[J]. J Bone Joint Surg Br, 2002, 84(5): 748-752. [DOI] [PubMed] [Google Scholar]
- [9].Dansie DM, Luetmer PH, Lane JI, et al. MRI findings after successful vertebroplasty[J]. AJNR Am J Neuroradiol, 2005, 26(6): 1595-1600. [PMC free article] [PubMed] [Google Scholar]
- [10].Lin WC, Lee YC, Lee CH, et al. Refractures in cemented vertebrae after percutaneous vertebroplasty: a retrospective analysis[J]. Eur Spine J, 2008, 17(4): 592-599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Li X, Lou X, Lin X, et al. Refracture of osteoporotic vertebral body concurrent with cement fragmentation at the previously treated vertebral level after balloon kyphoplasty: a case report[J]. Osteoporos Int, 2014, 25(5): 1647-1650. [DOI] [PubMed] [Google Scholar]
- [12].Silverman SL. The clinical consequences of vertebral compression fracture[J]. Bone, 1992, 13(Suppl 2): S27-S31. [DOI] [PubMed] [Google Scholar]
- [13].Hollowell JP, Vollmer DG, Wilson CR, et al. Biomechanical analysis of thoracolumbar interbody constructs. How important is the endplate?[J] Spine, 1996, 21(9): 1032-1036. [DOI] [PubMed] [Google Scholar]
- [14].Adams MA, Freeman BJ, Morrison HP, et al. Mechanical initiation of intervertebral disc degeneration[J]. Spine, 2000, 25(13): 1625-1636. [DOI] [PubMed] [Google Scholar]
- [15].Oner FC, van Gils AP, Faber JA, et al. Some complications of common treatment schemes of thoracolumbar spine fractures can be predicted with magnetic resonance imaging: prospective study of 53 patients with 71 fractures. Spine, 2002, 27(6): 629-636. [DOI] [PubMed] [Google Scholar]
- [16].Rohlmann A, Neller S, Claes L, et al. Influence of a follower load on intradiscal pressure and intersegmental rotation of the lumbar spine[J]. Spine, 2001, 26(24): E557-E561. [DOI] [PubMed] [Google Scholar]
- [17].Kurowski P, Kubo A. The relationship of degeneration of the intervertebral disc to mechanical loading conditions on lumbar vertebrae[J]. Spine, 1986, 11(7): 726-731. [DOI] [PubMed] [Google Scholar]
- [18].Hakim NS, King AI. A three dimensional finite element dynamic response analysis of a vertebra with experimental verification[J]. J Biomech, 1979, 12(4): 277-92. [DOI] [PubMed] [Google Scholar]
- [19].Oxland TR, Grant JP, Dvorak MF, et al. Effects of endplate removal on the structural properties of the lower lumbar vertebral bodies[J]. Spine, 2003, 28(8): 771-777. [PubMed] [Google Scholar]
- [20].Koh YH, Han D, Cha JH, et al. Vertebroplasty: magnetic resonance findings related to cement leakage risk[J]. Acta Radiol, 2007, 48(3): 315-320. [DOI] [PubMed] [Google Scholar]
- [21].Weisskopf M, Ohnsorge JA, Niethard FU. Intravertebral pressure during vertebroplasty and balloon kyphoplasty: an in vitro study[J]. Spine, 2008, 33(2): 178-182. [DOI] [PubMed] [Google Scholar]
- [22].Mirovsky Y, Anekstein Y, Shalmon E, et al. Intradiscal cement leak following percutaneous vertebroplasty[J]. Spine, 2006, 31(10): 1120-1124. [DOI] [PubMed] [Google Scholar]