Abstract
Background:
It is widely recognized that patients have increased anxiety before elective surgery, however, previous research investigating the effect of preassessment clinics (PACs) on anxiety levels has been limited specifically to patient information literature or multimedia use, rather than the consultation process itself. The aim was to investigate the effect attendance at PAC had on patients’ anxiety levels, associated with their subsequent surgery and anesthetic.
Materials and Methods:
This survey consisted of a cross-sectional, questionnaire-based, quantitative study investigating patients’ anxiety levels before and after attendance at the PAC. The questionnaire consisted of a series of statements concerning the surgery and anesthetic and rated using a Likert-type scale. All adult patients who attended an appointment at the PAC were eligible to participate in the study. Those unable to read and understand the questionnaire were excluded.
Results:
Overall 121 participants were included in the study. Participants felt less anxious about their subsequent surgery and anesthetic following consultation at the PAC (P < 0.001). This was true for both gender subgroups (P < 0.05) Concerns about intraoperative complications generated the most anxiety. Postoperatively, male participants were most anxious about pain and females about nausea and vomiting. Participants also reported high satisfaction rates for the service at the PAC.
Conclusions:
This study contributes to a greater understanding of preoperative anxiety and has important implications for PACs. This clinical survey has been able to demonstrate that consultation at the PAC has a statistically significant positive effect on alleviating patients’ anxieties in regards to their surgery and anesthetic.
Key words: Anesthesia, anxiety, preassessment, surgery
Introduction
Advancements in modern medicine have led to an increase in elective surgery worldwide contributing to increased pressures on healthcare resources.[1,2,3,4,5,6] The advent of preassessment clinics (PACs) has become vital in ensuring the continued productivity of nonemergency surgery.[7,8,9,10]
Patient satisfaction associated with PAC attendances is becoming a more prominent issue as patients are often considered as consumers of a service in a competitive marketplace.[7,11,12] Attendance at a PAC improves not only patient's satisfaction, but also their confidence to make an informed anesthetic consent.[13]
Anesthesia, unlike surgery, can appear abstract to the lay person.[14,15] Many factors have been identified as reasons for anxiety surrounding anesthesia including “fear of the unknown” and “loss of control.”[6,14,16,17] These factors contribute to the distorted viewpoint of what anesthesia entails and the associated risks.[16,18,19]
Clinicians have the benefit of a greater understanding of anesthesia, yet previous research suggests that it is difficult to predict patient anxieties in relation to anesthesia and surgery.[20,21]
Anxiety (a brooding fear of what may happen) has long been considered important in psychological literature since it was a central theme in Freud's psychoanalytic theory. Psychologists have argued that fear — a core emotion in psychopathology — is fundamentally an adaptive reaction to stressors which probably originated as an alarm signal to warn organisms of potential danger.[22]
As far back as the mid-20th century, we have been fascinated by the impact of fear from healthcare procedures on anxiety, attitudes and behavior.[23,24] This anxiety may be so great that it inhibits rather than facilitates concordance with medical treatment. By offering an intervention which explains a previously ununderstood process, a patient is less likely to feel vulnerable and a reduction in anxiety will be observed.[25]
Previous research has identified that patients have anxieties prior to elective surgery[3,4,26,27,28] but research investigating the effect of PACs on anxiety levels has been limited specifically to patient information literature or multimedia use, rather than the consultation process itself.[7,9,29,30,31] Since PACs have the potential to provide the patient with greater understanding of their anesthetic and surgery, the PAC at our hospital has the opportunity to reduce anxiety surrounding this.
The aim of this survey was to investigate the effect attendance and ensuing consultation at the PAC had on patients’ anxieties associated with their subsequent anesthetic and surgery.
Materials and Methods
A survey method was employed which consisted of a cross-sectional, questionnaire-based, quantitative study into patients’ anxiety levels before and after attendance at the PAC. The design of the questionnaire was created following careful review of the literature.[3,6,18,20,21]
The questionnaire consisted of a series of short statements which patients could rank appropriate to a Likert-type scale [Appendix A (156KB, pdf) ]. The first pair of statements (1 and 3) addressed generically the anxiety regarding the anesthetic and surgery. The second pair of statements (2 and 4) concerned specific aspects of the anesthetic which may induce anxiety, for example, induction of the anesthesia, intraoperative complications, and symptom management postprocedure. The final question (5) addressed general satisfaction with attendance at the PAC and was included in the postconsultation questionnaire only.
Statements on page 1 were answered by patients before being seen by the anesthetist at the PAC. After finishing the consultation, patients answered the statements on page 2, which were identical to page 1. This allowed for a before and after comparison of each patient's anxieties.
All adult patients who attended an appointment at the PAC were eligible to participate in the study. Those unable to read and understand the questionnaire were excluded.
The PAC receptionist was responsible for issuing, reissuing after the consultation, and collecting the completed questionnaires from the patients. These were then folded and posted into a secure storage unit accessed only by the chief investigator.
Quantitative data extracted from the questionnaires was examined and interpreted using Microsoft Excel and the Statistical Package for Social Scientists (SPSS) version 21 (IBM, Armonk, New York, USA). A series of paired samples t-tests were conducted to investigate the difference in mean scores between pairs of statements before and after the preassessment appointment.
The study was reviewed by the Grampian Research Ethics Committee who found that this survey did not require ethical approval.
The PAC is nurse-led with clearly defined pathways to triage patients. Nurses with extensive experience on surgical wards are recruited to the preoperative assessment unit where they are trained by their peers with additional training by the consultant anesthetists. The clinic has full anesthetic support with a consultant anesthetist staffing clinics every Monday to Friday (reviewing those patients triaged to be seen by them, as well as dealing with any other problems identified by the nursing staff).
All patients in the PAC are initially seen by the nurse. They complete a validated questionnaire with the patient and investigations are performed according to National Institute for Clinical Excellence guidance.
All patients who are having minor surgery and are classified as American Society of Anesthesiologists (ASA) 1 or 2 are seen only by the nurse and provided with advice and information. This advice includes a verbal discussion of risks and benefits and the provision of information leaflets covering the hospital stay (generic-hospital or ward-specific dependent on the planned operation); surgery (provided by the surgeons); and possible anesthetic options (Royal College of Anesthetists patient information leaflets). Should the patients request further information they are booked to see the consultant anesthetist.
All patients having major surgery, who are ASA 3 or higher or who have abnormal blood results or electrocardiogram must be reviewed by the consultant anesthetist in the PAC. It is not feasible in our hospital for each anesthetist to assess their own cases. Therefore, a “generic” preoperative assessment is conducted whereby the consultant anesthetist will assess and discuss options with the patient. They may recommend a further course of action which might include: Scheduling for surgery (with or without recommendations for actions before or on admission dependent on coexisting conditions), referral back to the general practice, referral to other specialties (e.g., cardiac or respiratory), referral for further investigation (e.g., echocardiogram), or cancellation if the patient is not fit for their procedure.[32]
Results
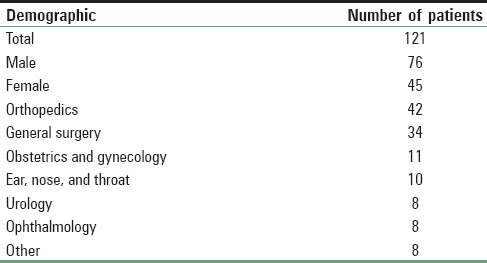
Table 1 demonstrates patient demographic information from the study group. In total 138 participants completed the questionnaire, 17 were not included because the questionnaire was incorrectly completed. The majority of these patients were male (63%). Orthopedics (35%) and general surgery (28%) were the most common surgical specialties for which patients were seen in the PAC.
Table 1.
Demographic information
For the study overall there was a statistically significant improvement in anxiety levels from baseline demonstrated for both sets of paired statements (P < 0.001). This was also true for both gender subgroups (P < 0.05).
The results for the statements regarding anxiety in relation to the anesthetic and surgery (Q1 and 3) are shown in Table 2. There was a higher baseline anxiety level associated with the surgery in comparison to the anesthetic. The anxieties associated with both surgery and anesthetic, were improved by an approximately equal proportion following consultation in the PAC. Similar observations were made for both gender subgroups.
Table 2.
Anxiety in relation to anesthetic and surgery
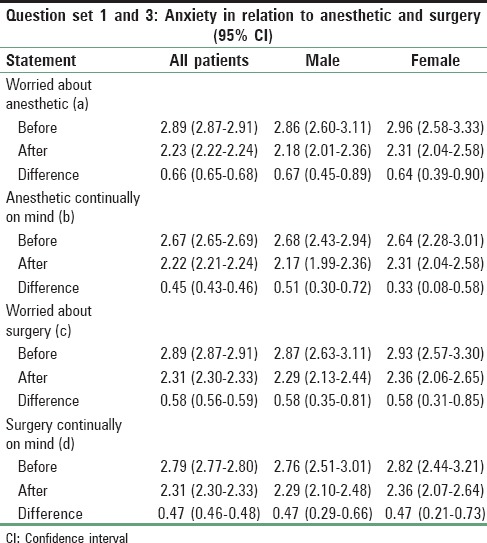
Table 3 displays the results for the questions in relation to specific aspects of the anesthetic (Q2 and 4). Overall baseline anxiety was highest in regards to intraoperative complications while patients felt least anxious about receiving an injection.
Table 3.
Anxiety in relation to specific aspects of anesthesia
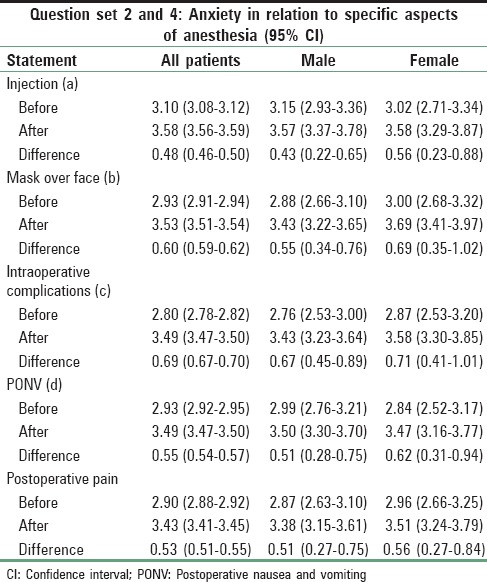
There was a difference between the gender subgroups for both the questions relating to induction of anesthesia and the postoperative period. Female patients expressed no difference in anxiety level between receiving an injection and having a mask over their face, while males were more anxious about having a mask over their face as opposed to getting an injection. Male patients were more concerned about pain postoperatively whereas the female subgroup found postoperative nausea and vomiting (PONV) a more anxiety inducing complication.
The female subgroup demonstrated a greater change from baseline anxiety after consultation for all five aspects specifically relating to anesthesia in comparison to the male subgroup. An unpaired t-test was performed to analyze these gender differences but no statistically significant difference was observed (P > 0.1).
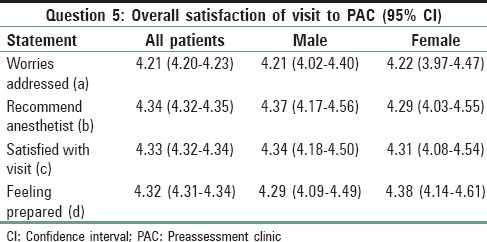
Table 4 demonstrates the results for the question relating to the participant's overall satisfaction of their visit to the PAC. High participant satisfaction rates were observed overall; 84% of patients felt that their worries had been addressed; 87% of patients would recommend their anesthetist and were satisfied with their visit to preassessment, and 86% of patients felt prepared for their surgery. There were no differences between the gender subgroups.
Table 4.
Overall satisfaction of visit to preassessment clinic
Discussion
This clinical survey aimed to investigate the effect attendance at the PAC had on patients’ anxieties regarding their anesthetic and surgery. The results have demonstrated that the PAC had a statistically significant positive effect on alleviating patient's anxieties in regards to their anesthetic and surgery.
Previous research has identified the significance of anxiety in patients during preassessment.[4,7,9,26,31] Earlier research studies have used similar methods of nonvalidated patient questionnaires to study patient anxieties — But this has not been focused around the anesthesia.
Three studies have demonstrated improvement in patient satisfaction following consultation at the PAC, including an earlier study by Mactier and McKendrick which was undertaken in the same PAC as this study. DeMaria et al. investigated the use of primary care style interviewing, while Salzwedel et al. studied a trial of patient information in a multimedia format.
In contrast to our findings, Salzwedel et al. demonstrated no improvement of patients’ baseline anxiety at the PAC. However, Bondy et al. found a statistically significant improvement in patients’ anxiety with the use of multimedia patient information. In comparison, this study does not focus on patient information literature or multimedia and focuses entirely on the effect the consultation with an anesthetist at the PAC has on patients’ anxiety.
Previous research has shown females to be more anxious than their male counterparts.[4,20] In contrast, this survey demonstrated similar baseline anxiety levels between genders.
The results of this survey suggest a difference between gender groups with regards to postoperative complications. The male subgroup was more concerned about pain whereas the female subgroup was more concerned about PONV. Previous literature has suggested that this may be related to the increased risk of PONV in the female population.[4,33,34,35]
The response to the final question highlighted that the patients are highly satisfied with the service they receive from the PAC. Many outcomes are expected from the PAC from both patient and the anesthetist, so it is important to note that although this survey mostly screens for anxiety, this patient group were happy with the overall service they received on their visit to the PAC. This supports earlier literature.[7,9,13]
During the study, a number of potential limitations were identified. The questionnaire only covered a select few aspects of the anesthetic that patients may feel anxious about. The questionnaire may therefore bias toward these specific aspects when the patient may be anxious about a number of other factors. The results will ultimately focus toward the statements on the questionnaire which may not offer a true reflection of the study sample's anxiety levels.
It should be acknowledged that there are other demographic factors that may influence the results of this study. Previous research recognizes that patient age, previous experience of anesthesia and surgery, and surgical diagnosis (benign vs. malignant) will affect anxiety and may be confounding factors in the interpretation of results.[4,20,21,36]
The patient management software being used was unable to provide a record of patient numbers seen in the PAC during the study period. It is therefore unknown what percentage of patients agreed to participate in the study. This may have introduced selection bias and affected the final results.
Due to the small sample size, a subgroup analysis according to type of surgical procedure was not performed. In addition, gender differences in baseline anxiety were not statistically significant. These limitations may be addressed by collecting data over a longer period of time.
This study contributes to a greater understanding of preoperative anxiety and has important implications for PACs. Unlike previous research this study focuses exclusively on the effect the consultation at the PAC has on patients’ anxieties in regards to their anesthetic and surgery. Overall it has been able to demonstrate a statistically significant positive effect in alleviating patients’ anxieties in the preoperative period and stimulates further research into this topic.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Assistance with the study: The authors would like to thank the staff at the PAC, Dr. Gray's Hospital, Elgin who provided care for study patients, with a special thanks to the admin staff who distributed and collected surveys during the study period.
References
- 1.Leff DR, Bhutiani RP. Give the patients the choice — The ‘walk in walk out’ hernia clinic. [Last accessed on 2015 Mar];Ambul Surg. 2006 12:125–9. Available from: http://www.ovidsp.uk.ovid.com/sp-3.17.0a/ovidweb.cgi . [Google Scholar]
- 2.Mitchell M. Patient anxiety and modern elective surgery: A literature review. J Clin Nurs. 2003;12:806–15. doi: 10.1046/j.1365-2702.2003.00812.x. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell M. General anesthesia and day-case patient anxiety. J Adv Nurs. 2010;66:1059–71. doi: 10.1111/j.1365-2648.2010.05266.x. [DOI] [PubMed] [Google Scholar]
- 4.Mitchell M. Anesthesia type, gender and anxiety. J Perioper Pract. 2013;23:41–7. doi: 10.1177/175045891302300301. [DOI] [PubMed] [Google Scholar]
- 5.Paterson HM, McMillan R, Nixon SJ. True day surgery or 23-hour admission for unselected elective laparoscopic cholecystectomy? Ambul Surg. 2006;12:177–80. [Google Scholar]
- 6.Pritchard MJ. Identifying and assessing anxiety in pre-operative patients. Nurs Stand. 2009;23:35–40. doi: 10.7748/ns.23.51.35.s46. [DOI] [PubMed] [Google Scholar]
- 7.DeMaria S, Jr, DeMaria AP, Silvay G, Flynn BC. Use of the BATHE method in the preanesthetic clinic visit. Anesth Analg. 2011;113:1020–6. doi: 10.1213/ANE.0b013e318229497b. [DOI] [PubMed] [Google Scholar]
- 8.Fischer SP. Development and effectiveness of an anesthesia preoperative evaluation clinic in a teaching hospital. Anesthesiology. 1996;85:196–206. doi: 10.1097/00000542-199607000-00025. [DOI] [PubMed] [Google Scholar]
- 9.Salzwedel C, Petersen C, Blanc I, Koch U, Goetz AE, Schuster M. The effect of detailed, video-assisted anesthesia risk education on patient anxiety and the duration of the preanesthetic interview: A randomized controlled trial. Anesth Analg. 2008;106:202–9. doi: 10.1213/01.ane.0000287665.96156.72. [DOI] [PubMed] [Google Scholar]
- 10.Starsnic MA, Guarnieri DM, Norris MC. Efficacy and financial benefit of an anesthesiologist-directed university preadmission evaluation center. J Clin Anesth. 1997;9:299–305. doi: 10.1016/s0952-8180(97)00007-x. [DOI] [PubMed] [Google Scholar]
- 11.Mead N, Bower P, Hann M. The impact of general practitioners’ patient-centredness on patients’ post-consultation satisfaction and enablement. Soc Sci Med. 2002;55:283–99. doi: 10.1016/s0277-9536(01)00171-x. [DOI] [PubMed] [Google Scholar]
- 12.Snyder-Ramos SA, Seintsch H, Böttiger BW, Motsch J, Martin E, Bauer M. Patient satisfaction and information gain after the preanesthetic visit: A comparison of face-to-face interview, brochure, and video. Anesth Analg. 2005;100:1753–8. doi: 10.1213/01.ANE.0000153010.49776.E5. [DOI] [PubMed] [Google Scholar]
- 13.Mactier K, McKendrick D. Association of Anaesthetists of Great Britain and Ireland. London: Wiley Blackwell; 2014. Communication, patient satisfaction and ability to make an informed consent after pre-assessment. [Google Scholar]
- 14.Kakinuma A, Nagatani H, Otake H, Mizuno J, Nakata Y. The effects of short interactive animation video information on preanesthetic anxiety, knowledge, and interview time: A randomized controlled trial. Anesth Analg. 2011;112:1314–8. doi: 10.1213/ANE.0b013e31820f8c18. [DOI] [PubMed] [Google Scholar]
- 15.Klafta JM, Roizen MF. Current understanding of patients’ attitudes toward and preparation for anesthesia: A review. Anesth Analg. 1996;83:1314–21. doi: 10.1097/00000539-199612000-00031. [DOI] [PubMed] [Google Scholar]
- 16.Matthey PW, Finegan BA, Finucane BT. The public's fears about and perceptions of regional anesthesia. Reg Anesth Pain Med. 2004;29:96–101. doi: 10.1016/j.rapm.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Mitchell M. Conscious surgery: Influence of the environment on patient anxiety. J Adv Nurs. 2008;64:261–71. doi: 10.1111/j.1365-2648.2008.04769.x. [DOI] [PubMed] [Google Scholar]
- 18.Lam E, Lee M, Brull R, Wong DT. Effect of anesthesia consultation on patients’ preoperative concerns. Can J Anaesth. 2007;54:852–3. doi: 10.1007/BF03021718. [DOI] [PubMed] [Google Scholar]
- 19.Sosis MB, Parnass SM, McCarthy RJ, Braverman B, Watson G, Halter T. Spinal phobia: Survey results of patient attitudes and preferences regarding anesthesia. J Clin Anesth. 1995;7:389–94. doi: 10.1016/0952-8180(95)00068-s. [DOI] [PubMed] [Google Scholar]
- 20.Fekrat F, Sahin A, Yazici KM, Aypar U. Anaesthetists’ and surgeons’ estimation of preoperative anxiety by patients submitted for elective surgery in a university hospital. Eur J Anaesthesiol. 2006;23:227–33. doi: 10.1017/S0265021505002231. [DOI] [PubMed] [Google Scholar]
- 21.Shafer A, Fish MP, Gregg KM, Seavello J, Kosek P. Preoperative anxiety and fear: A comparison of assessments by patients and anesthesia and surgery residents. Anesth Analg. 1996;83:1285–91. doi: 10.1097/00000539-199612000-00027. [DOI] [PubMed] [Google Scholar]
- 22.LeDoux JE. The Emotional Brain: The Mysterious Underpinnings of Emotional Life. New York: Simon & Schuster; 1994. [Google Scholar]
- 23.Janis IL, Feshbach S. Effect of fear-arousing communications. J Abnorm Psychol. 1953;48:78–92. doi: 10.1037/h0060732. [DOI] [PubMed] [Google Scholar]
- 24.Janis IL, Terwilliger RF. An experimental study of psychological resistance to fear-arousing communications. J Abnorm Soc Psychol. 1962;65:403–10. doi: 10.1037/h0047601. [DOI] [PubMed] [Google Scholar]
- 25.McGuire WJ. Personality and susceptibility to social influence. In: Borgatta EF, Lambert WW, editors. Handbook of Personality: Theory and Research. Chicago, IL: Rand-McNally; 1968. [Google Scholar]
- 26.Bondy LR, Sims N, Schroeder DR, Offord KP, Narr BJ. The effect of anesthetic patient education on preoperative patient anxiety. Reg Anesth Pain Med. 1999;24:158–64. doi: 10.1016/s1098-7339(99)90078-0. [DOI] [PubMed] [Google Scholar]
- 27.Cassady JF, Jr, Wysocki TT, Miller KM, Cancel DD, Izenberg N. Use of a preanesthetic video for facilitation of parental education and anxiolysis before pediatric ambulatory surgery. Anesth Analg. 1999;88:246–50. doi: 10.1097/00000539-199902000-00004. [DOI] [PubMed] [Google Scholar]
- 28.McCleane GJ, Cooper R. The nature of pre-operative anxiety. Anesthesia. 1990;45:153–5. doi: 10.1111/j.1365-2044.1990.tb14285.x. [DOI] [PubMed] [Google Scholar]
- 29.Lee A, Gin T. Educating patients about anesthesia: Effect of various modes on patients’ knowledge, anxiety and satisfaction. Curr Opin Anaesthesiol. 2005;18:205–8. doi: 10.1097/01.aco.0000162842.09710.d5. [DOI] [PubMed] [Google Scholar]
- 30.Soltner C, Giquello JA, Monrigal-Martin C, Beydon L. Continuous care and empathic anaesthesiologist attitude in the preoperative period: Impact on patient anxiety and satisfaction. Br J Anaesth. 2011;106:680–6. doi: 10.1093/bja/aer034. [DOI] [PubMed] [Google Scholar]
- 31.Valenzuela Millán J, Barrera Serrano JR, Ornelas Aguirre JM. Anxiety in preoperative anesthetic procedures. Cir Cir. 2010;78:147–51. [PubMed] [Google Scholar]
- 32.McKendrick DR, Cumming GP, Lee AJ. A 5-year observational study of cancellations in the operating room: Does the introduction of preoperative preparation have an impact? Saudi J Anaesth. 2014;8(Suppl 1):S8–14. doi: 10.4103/1658-354X.144053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Islam S, Jain PN. Post-operative nausea and vomiting (PONV): A review article. [Last accessed on 2014 Nov];Indian J Anaesth. 2004 48:253–8. Available from: http://www.ovidsp.uk.ovid.com/sp-3.17.0a/ovidweb.cgi . [Google Scholar]
- 34.Lerman J. Surgical and patient factors involved in postoperative nausea and vomiting. Br J Anaesth. 1992;69(7 Suppl 1):24S–32S. doi: 10.1093/bja/69.supplement_1.24s. [DOI] [PubMed] [Google Scholar]
- 35.Macario A, Weinger M, Carney S, Kim A. Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesth Analg. 1999;89:652–8. doi: 10.1097/00000539-199909000-00022. [DOI] [PubMed] [Google Scholar]
- 36.Caddick J, Jawad S, Southern S, Majumder S. The power of words: Sources of anxiety in patients undergoing local anaesthetic plastic surgery. Ann R Coll Surg Engl. 2012;94:94–8. doi: 10.1308/003588412X13171221501267. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


