Abstract
Objective:
To evaluate the conventional practice of endotracheal tube (ETT) cuff inflation and pressure measurement as compared to the instrumental method.
Study Design:
Prospective observational study.
Place and Duration of Study:
Department of Anaesthesia, King Saud University Hospital, Riyadh, Saudi Arabia (June 2014–July 2014).
Methods:
A total of 100 adult patients were observed according to the syringe size used Group-1 (10 ml) and Group-2 (20 ml) for ETT cuff inflation in general anesthesia. Patients with anticipated difficult intubation, risk for aspiration, known anatomical laryngotracheal abnormalities, and emergency cases were excluded. Trachea was intubated with size 8 or 8.5 mm and 7.0 or 7.5 mm ETT in male and female patients respectively. The ETT cuff was inflated with air by one of the anesthesia technician. Cuff pressures were measured using aneroid manometer. ETT cuff pressure of 20–30 cm of water was considered as standard.
Results:
In 69% of the patients, the cuff pressure measurements were above the standard. Age (P = 0.806), weight (P = 0.527), height (P = 0.850), and gender (P = 1.00) were comparable in both groups. The mean cuff pressure in Group-1 and Group-2 was 32.52 ± 6.39 and 38.90 ± 6.60 cm of water (P = 0.001). The cuff inflation with 20 ml syringe resulted in higher cuff pressure as compared to 10cc syringe 37.73 ± 4.23 versus 40.74 ± 5.01 (86% vs. 52%, P = 0.013).
Conclusion:
The conventional method for ETT cuff inflation and pressure measuring is unreliable. As a routine instrumental cuff pressure, monitoring is suggested.
Key words: Cuff pressure, endotracheal tube, measurement
Introduction
A critical function of the endotracheal tube (ETT) cuff is to seal the airway thus preventing leaks and aspiration of pharyngeal contents into the trachea during ventilation. In literature, catastrophic consequences of ETT cuff overinflation and insufficient inflation are reported. An ETT with a cuff is generally used for mechanically ventilated patients to prevent gas leakage and pulmonary aspiration. Excessive cuff pressure decreases tracheal capillary perfusion, and insufficient cuff pressure leads to pulmonary aspiration of oropharyngeal content.[1,2,3,4]
The ETT cuff pressure must be in a range that ensures delivery of the prescribed mechanical ventilation tidal volume, reduces the risk for aspiration of secretions that accumulate above the cuff without compromising the tracheal perfusion. A cuff pressure of 20–30 cm of water is recommended for the prevention of aspiration and ventilator-associated pneumonia.[5,6,7]
Postintubation sore throat is a common side effect of general anesthesia. This may partly result from ischemia of the oropharyngeal and tracheal mucosa due to over-inflation of the cuff. In general, in anesthesia practice ETT cuff pressure is assessed by palpation of cuff or cession of audible leak around the cuff is the end point for inflation. We have conducted an observational study to evaluate the efficacy of cuff inflation and assessment of conventional method and instrumental measurement of cuff pressure. The ETT cuff pressure of 20–30 cm of H2O was considered as standard.
Methods
This was a prospective observational study; Institutional Review Board approval was taken. Informed consent was obtained from the patients who met the eligibility criteria. One hundred adult patients above 18 years of age scheduled for elective surgical procedure requiring general anesthesia and endotracheal intubation were included in the study. Patients with anticipated difficult intubation or having a history of difficult intubation, high risk for aspiration, known anatomical laryngotracheal abnormalities, and emergency intubations were excluded. General anesthesia was induced using intravenous bolus of induction agents and paralysis was achieved with succinylcholine or a nondepolarizing muscle relaxant. Male patients’ trachea was intubated with an 8 or 8.5 mm internal diameter ETT and female patients trachea was intubated with a 7.0 or 7.5 mm internal diameter ETT. Anesthesia was maintained with sevoflurane, a volatile anesthetic agent, in a combination of air and oxygen. At least five patients were randomly selected from the routine elective surgical list in a day. The duration of the study was 1 month. The routine practice in our institution is that endotracheal intubation is done by anesthesiologist and ETT cuff is inflated by the qualified anesthesia technician. A 10 ml or 20 ml syringe was used as a routine in our institution for laryngeal mask airway and ETT cuff inflation. Adequacy of cuff inflation is generally assessed by palpation of the pilot balloon and sometimes readjusted by anesthetist by inflating just enough to stop an audible leak around the cuff. The cuff pressure was measured by one of the investigator within 60 min of induction (before positioning) of anesthesia using an aneroid manometer. The aneroid manometer (VBM, Sulz, Germany) was connected to the pilot balloon of the ETT cuff via a three-way stopcock, and ETT cuff pressure was measured and recorded.
Sample size calculation was based on the standard cuff pressure in ETTs (20–30 cm H2O).[1] According to prior studies, it is established that a clinically important difference in mean cuff pressure is 20%.[1] Given an expected standard deviation (SD) of 7.0 cm H2O, we estimated that a sample size of 43 patients per group would be required for a significance level of 0.05 and power of 90%. However, considering the possible dropout, we recruited 50 patients in each group.
A IBM Statistical Package for Social Sciences (SPSS), USA, version-21 was used for data entry and analysis. Mean and SD were computed for quantitative variables such as age, weight, height, ETT cuff pressure, and tube size. Independent-samples t-test was applied for quantitative variables age, weight, height, and cuff pressure. Chi-square was applied for qualitative variable gender. The data were presented in percentages or SD where ever appropriate. P <0.05 was considered as significant.
Results
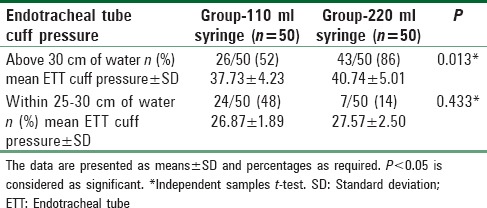
ETT cuff pressure was measured in 100 adult patients who underwent elective surgical procedures under general anesthesia requiring endotracheal intubation. We have divided the patients into two groups according to the syringe size used, Group-1 (10 ml, n = 50) and Group-2 (20 ml, n = 50). There was no significant difference in age (P = 0.806), weight (P = 0.527), height (P = 0.850), and gender (P = 1.00) in both groups [Table 1]. The overall incidence of ETT cuff pressures within the recommended range (25–30 cm of water) was 31% and in 69% it was above the recommended range [Table 2]. None of the measured cuff pressure was below the recommended range. The mean cuff pressure in Group-1 (10 ml) and Group-2 (20 ml) was 35.52 ± 6.39 cm of water and 38.90 ± 6.60 cm of water respectively, the difference was statistically significant (P = 0.001). The mean cuff pressure above the standard in Group-1 26/50 (52%) and Group-2 43/50 (86%) was 37.73 ± 4.23 and 40.74 ± 5.01 cm of water, the difference was statistically significant (P = 0.013) between groups. The mean cuff pressure within the standard in Group-1 (24/50, 48%) and Group-2 (7/50 (14%) was 26.87 ± 1.89 and 27.57 ± 2.50 cm of water, the difference was not statistically significant (P = 0.433) between groups.
Table 1.
Patient characteristics in Group-1 (10 ml syringe) and Group-2 (20 ml syringe)
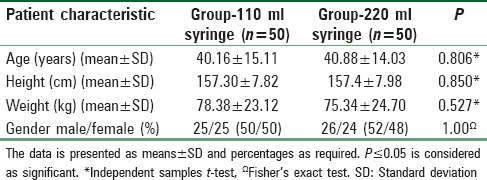
Table 2.
Endotracheal tube cuff pressures in Group-1 (10 ml syringe) and Group-2 (20 ml syringe)
Discussion
The pressure exerted on the tracheal wall is one of the primary determinants of tracheal injury.[8] The intra-cuff pressure in intubated patients should be high enough to prevent macroscopic aspiration and an air leak to ensure adequate ventilation. The cuff pressure should be adequate enough not to impair the mucosal blood flow.[9] It has been shown that continuous lateral wall cuff pressure above 30 cm H2O compromises blood flow, and cuff pressure above 50 cm H2O completely obstruct the tracheal wall blood flow.[3] It has been shown that compromised blood flow for 15 min resulted in superficial damage to the tracheal mucosa.[10] It is reported that high ETT cuff pressure lasted more than 15 min resulted in obstructed mucosal blood flow, the columnar epithelium was destroyed, and basement membrane was exposed.[8,9,10] Damage to the trachea during intubation is inevitable as a result of the contact between the ETT and the trachea.[8] Digital balloon palpation corresponds poorly with the measured endotracheal cuff pressure, and anesthetist experience corresponds poorly with measured cuff pressures.[8,10,11,12] The instrumental measurement and adjustment of cuff pressure resulted in a significantly lower incidence of postprocedural sore throat, hoarseness, and blood-stained expectorant.[12] The pressure exerted on the tracheal wall depends on the compliance of the trachea and the pressure measured at the pilot balloon of an ETT cuff. ETT cuff pressure can be considered as a good estimate of the pressure exerted on the tracheal mucosa.[13] When conventionally adjusted cuff pressure was measured in different settings, the reported cuff pressures in most of the cases ranges between 40 and 62 cm H2O.[13,14,15] The highest recorded ETT cuff pressure in our study was 48 cm H2O, and most of the patients (69%) were having high cuff pressure. Our study showed that the overall compliance on the standards is far behind the expected levels and need immediate improvement. In our study, we observed that the use of bigger size syringe (20 ml) is one of the important factors for over inflating the ETT cuff, resulted in high cuff pressure. It was shown that there is linear relationship between the measured cuff pressure and the volume of air retrieved from the cuff. Sengupta et al.[1] showed that injected volumes between 2 and 4 ml usually produce cuff pressures between 20 and 30 cm H2O, independent of tube size for the same type of tube. Harm et al. reported that tracheal tube cuff pressures in patients intubated before aeromedical transport were too high and recommend the mandatory routine use of a cuff pressure manometer to avoid inappropriately high cuff pressures. He has suggested the use of a 5 ml syringe alternative to the traditional bigger size syringe.[16] This study has highlighted the issue of training and awareness among anesthesia personnel regarding cuff inflation and cuff pressure measurement technique. Minor but common complications like postoperative sore throat can be prevented using a routine simple aneroid instrument for cuff inflation and pressure measurement rather than relying on conventional methods.
A limitation of this study is that cuff pressure was evaluated just once 60 min after induction of anesthesia. It was unlikely that the cuff pressures varied much during the 1st h of the study cases as nitrous oxide was not used. The other limitation of our study was a lack of control or placebo group. Further studies are required to find out the incidence of postoperative sore throat after repeated instrumental measurement of cuff pressure in prolong surgeries and surgeries in different positions.
Conclusion
The conventional method for ETT cuff inflation and balloon pressure measuring is unreliable. Instrumental cuff pressure monitoring is simple and inexpensive[17,18] and suggested to be used as a routine.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sengupta P, Sessler DI, Maglinger P, Wells S, Vogt A, Durrani J, et al. Endotracheal tube cuff pressure in three hospitals, and the volume required to produce an appropriate cuff pressure. BMC Anesthesiol. 2004;4:8. doi: 10.1186/1471-2253-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sole ML, Su X, Talbert S, Penoyer DA, Kalita S, Jimenez E, et al. Evaluation of an intervention to maintain endotracheal tube cuff pressure within therapeutic range. Am J Crit Care. 2011;20:109–17. doi: 10.4037/ajcc2011661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nseir S, Brisson H, Marquette CH, Chaud P, Di Pompeo C, Diarra M, et al. Variations in endotracheal cuff pressure in intubated critically ill patients: Prevalence and risk factors. Eur J Anaesthesiol. 2009;26:229–34. doi: 10.1097/eja.0b013e3283222b6e. [DOI] [PubMed] [Google Scholar]
- 4.Blot SI, Poelaert J, Kollef M. How to avoid microaspiration? A key element for the prevention of ventilator-associated pneumonia in intubated ICU patients. BMC Infect Dis. 2014;14:119. doi: 10.1186/1471-2334-14-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 6.Safdar N, Dezfulian C, Collard HR, Saint S. Clinical and economic consequences of ventilator-associated pneumonia: A systematic review. Crit Care Med. 2005;33:2184–93. doi: 10.1097/01.ccm.0000181731.53912.d9. [DOI] [PubMed] [Google Scholar]
- 7.Rubes D, Klein AA, Lips M, Rulisek J, Kopecky P, Blaha J, et al. The effect of adjusting tracheal tube cuff pressure during deep hypothermic circulatory arrest: A randomised trial. Eur J Anaesthesiol. 2014;31:452–6. doi: 10.1097/EJA.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 8.Seegobin RD, van Hasselt GL. Endotracheal cuff pressure and tracheal mucosal blood flow: Endoscopic study of effects of four large volume cuffs. Br Med J (Clin Res Ed) 1984;288:965–8. doi: 10.1136/bmj.288.6422.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernhard WN, Yost L, Joynes D, Cothalis S, Turndorf H. Intracuff pressures in endotracheal and tracheostomy tubes. Related cuff physical characteristics. Chest. 1985;87:720–5. doi: 10.1378/chest.87.6.720. [DOI] [PubMed] [Google Scholar]
- 10.Liu J, Zhang X, Gong W, Li S, Wang F, Fu S, et al. Correlations between controlled endotracheal tube cuff pressure and postprocedural complications: A multicenter study. Anesth Analg. 2010;111:1133–7. doi: 10.1213/ANE.0b013e3181f2ecc7. [DOI] [PubMed] [Google Scholar]
- 11.Hoffman RJ, Parwani V, Hahn IH. Experienced emergency medicine physicians cannot safely inflate or estimate endotracheal tube cuff pressure using standard techniques. Am J Emerg Med. 2006;24:139–43. doi: 10.1016/j.ajem.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 12.Stein C, Berkowitz G, Kramer E. Assessment of safe endotracheal tube cuff pressures in emergency care – Time for change? S Afr Med J. 2011;101:172–3. doi: 10.7196/samj.4469. [DOI] [PubMed] [Google Scholar]
- 13.Sultan P, Carvalho B, Rose BO, Cregg R. Endotracheal tube cuff pressure monitoring: A review of the evidence. J Perioper Pract. 2011;21:379–86. doi: 10.1177/175045891102101103. [DOI] [PubMed] [Google Scholar]
- 14.Sathish Kumar S, Young PJ. Over-inflation of the tracheal tube cuff: A case for routine monitoring. Crit Care. 2002;6(Suppl 1):P37. [Google Scholar]
- 15.Braz JR, Navarro LH, Takata IH, Nascimento Júnior P. Endotracheal tube cuff pressure: Need for precise measurement. Sao Paulo Med J. 1999;117:243–7. doi: 10.1590/s1516-31801999000600004. [DOI] [PubMed] [Google Scholar]
- 16.Harm F, Zuercher M, Bassi M, Ummenhofer W. Prospective observational study on tracheal tube cuff pressures in emergency patients – Is neglecting the problem the problem? Scand J Trauma Resusc Emerg Med. 2013;21:83. doi: 10.1186/1757-7241-21-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nseir S, Rodriguez A, Saludes P, De Jonckheere J, Valles J, Artigas A, et al. Efficiency of a mechanical device in controlling tracheal cuff pressure in intubated critically ill patients: A randomized controlled study. Ann Intensive Care. 2015;5:54. doi: 10.1186/s13613-015-0054-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gillilanda L, Perriea H, Scribantea J. Endotracheal tube cuff pressures in adult patients undergoing general anaesthesia in two Johannesburg Academic Hospitals. South Afr J Anaesth Analg. 2015;21:81–4. [Google Scholar]


