Summary
Objective
To analyze cases of compound, unfavorable and non-comminuted mandibular angle fractures treated by trans-osseous wiring, presenting postoperative complications, in a low resource center.
Materials and methods
This was a 13-year retrospective study of 1,324 fractures in 1,317 subjects. The predictor variables were age, gender, aetiology, time lag between injury and treatment, and concomitant mandibular and mid-facial fractures. The outcome variable was the development of complication(s) after treatment. Descriptive and bivariate statistics were computed with EPI INFO 7 version software, and the P value was set at 0.05.
Results
The sample size was composed of 63/1317 (4.8%) of patients with complications. There were 48 males and 15 females with male: female ratio of 3.2:1. The age of the patients ranged from 21 to 62 years (mean 37.4± 5.6 years). The test of significance showed statistically significant association between complications of mandibular angle fractures and increasing age (P<0.002), male gender (P<0.001), road traffic accident (P<0.001), longer time lag between injury and treatment of fractures (P<0.000), and concomitant mandibular fractures (P<0.000). Deranged occlusion (n=19, 28.8%) and limited mouth opening <35mm (n=16, 24.2%) were the common complications. The complications were successfully treated during follow-up.
Conclusion
The use of trans-osseous wire osteosynthesis gave good results, and can still be useful in centres that are less well equipped and where access to rigid internal fixation with mini plates is either limited or unavailable.
Funding
Self-funded
Keywords: Mandible, angle, fracture, trans-osseous wiring, complications
Introduction
The mandibular angle is a triangular and weak region of the mandible that is prone to fracture following high velocity impact.1, 2 The angle fractures are among the most common mandibular fracture, accounting for about 30% of all mandibular fractures.3–5 This is due to the presence of a thinner cross-sectional area of the angle relative to the neighboring segments of the mandible, and the third molars, particularly those that are impacted, which weaken the region.1–3 When these fractures occur they present with varying degrees of displacement of the fractured bone segments due to the influence of displacing forces within the oro-facial region that determine their positions. The controversy associated with the management of mandibular angle fractures is related to the anatomic relations and complex biomechanical aspects of that region of the mandible.6
Consequently, because of these clinical and surgical problems the treatment of mandibular angle fractures has evolved over the decades from closed reduction methods to open reduction techniques with wire or hardware osteosynthesis.7, 8 Certainly, it was because of the difficulty in reducing some of these fracture segments when mandibular angle is fractured, and the adverse effects of the displacing forces of the muscles of mastication that some surgeons decided to surgically expose the fractures and place inter-fragmentary devices to help stabilize the reduced fractures. This is because some fractures could not be satisfactorily treated with closed reduction techniques no matter how ingenious the techniques might be.
To overcome the instability at the reduced fracture sites after the treatment provided by inter-osseous wiring, more rigid hard-wares were later applied to mandibular angle fractures after reduction to achieve better rigidity, stability and immediate restoration of function by causing compression of the fractured bone fragments towards one another.6–9 As compression was found to greatly increase the rigidity of the internal fixation system and encourage primary bone union without the formation of callus, the method has improved the treatment of these fractures and patients' comfort postoperatively by enabling the jaws to be used during the healing phase of the fractures with good treatment outcomes.10–12 Consequently, because the indications for the various types of rigid internal fixations have been debated by various researchers and have evolved over the years, it is important to note that this newest technique offer more advantages than the older surgical methods, with no major additional disadvantages.13,14 However, due to unavailability, and unaffordability of hard-ware osteosynthesis by some patients, it is not used in some oro-facial injury treatment centres in the third world countries. This has compelled surgeons' practising in these parts of the world to use the older surgical treatment methods such as trans-osseous wire osteosynthesis with inter-maxillary fixation for the treatment of these fractures when they present. Therefore for the improved management of compound, unfavorable and non-comminuted mandibular angle fractures and prevention of complications, we examine retrospectively the impact of treating these fractures in our environment over a period of 13 years.
Methods
The retrospective study of patients who sustained compound, unfavorable and non-comminuted mandibular angle fractures which were complicated after treatment by trans-osseous wire osteosynthesis with inter-maxillary fixation was undertaken. The subjects presented at the Oral and Maxillofacial Surgery Clinic of our institution between January 2000 and December 2012. Due to the retrospective nature of this study, it was granted an exemption by the Institutional Research Ethics Review Board where the study was done. Those cases that were compound, unfavorable and non-comminuted mandibular angle fractures, with complete clinical data were included in the study, whereas favorable, comminuted angle fractures and cases with incomplete data were excluded.
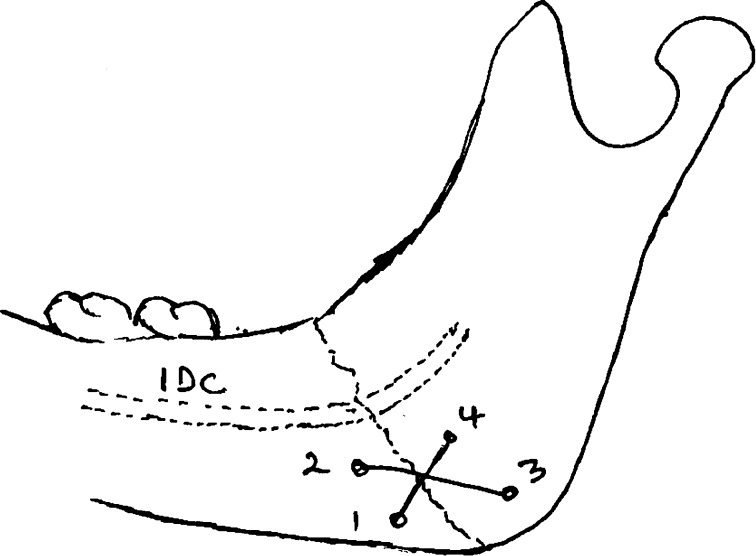
The patients were subjected to a thorough clinical examination before the radiological investigations. The unfavorable and non-comminuted mandibular angle fractures studied were diagnosed based on their anatomic location at the angle of the mandible. The radiographic views utilized for the complementary diagnoses were posterio-anterior (PA) of the jaws (Figure 1) and two oblique laterals of the mandible.
Figure 1.
Posterio-anterior radiograph of the jaws with arrows showing unfavorable, non-comminuted mandibular right angle and left body fractures.
The radiographs were certified as standardized by the local branch of the Association of Radiologists in Nigeria. The images were evaluated by three examiners: oral and maxillofacial surgeon who sub-specialized in trauma, senior resident in oral and maxillofacial surgery traumatology, and radiologist who specialized in traumatology.
For the diagnosis of the angle fractures, the examiners were given four options to choose from: 1). Favorable fracture, 2). Unfavorable fracture 3). No fracture and 4). Uncertain.
The criteria for the diagnosis of compound, unfavorable and non-comminuted mandibular angle fractures were: 1). Communication between the fracture line and the oral cavity or extra-oral or both. 2). There is only one fracture line. 3). Tooth bearing portion and posterior edentulous fragment were displaced and not making contact when viewed in the vertical or horizontal directions. 4). Displacement of the posterior edentulous fragment upwards, forwards and inwards causing both fractured fragments to separate or override.
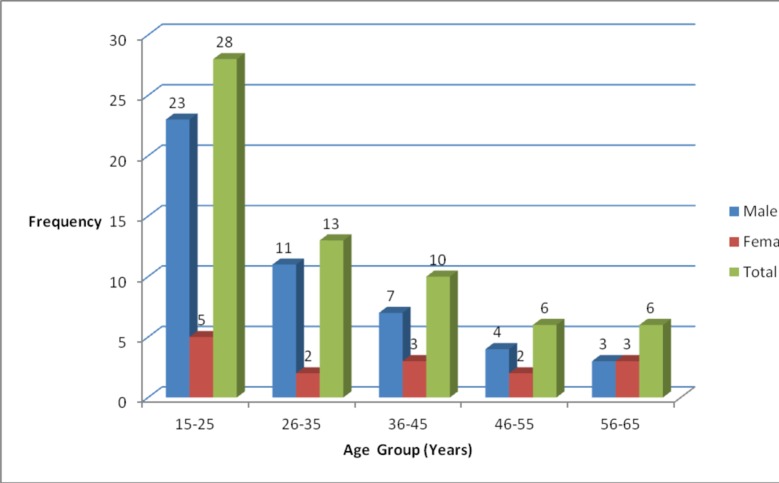
The surgical access to the fracture sites was by submandibular incision. Inter-maxillary fixation (IMF) using arch bars were done before the reduction of the bone fragments and this lasted within 30 minutes in all the cases treated. After reduction of the bony fragments, stainless steel wire (0.5mm) was used for fixation by placing figure of 8-wiring below the inferior dental canal above the lower border of the mandible after drilling four holes in the bony fragments (Figure 2). The complications were diagnosed after treatment, during the follow-up period.
Figure 2.
Key:IDC: Inferior dental canal
Trans-osseous (figure eight) wire at the mandibular angle
Information obtained from the hospital register, case files and plain radiographs of the subjects were recorded in a pro-forma questionnaire. The information recorded were age, gender, aetiology, and presence of concomitant mandibular and mid-facial fractures. Other factors documented were time lag between injury and treatment of the mandibular angle fractures, and the complications that developed after treatment. The data obtained were analyzed using EPI INFO 7, 0.2.0, 2012 version software (CDC, Atlanta, GA, USA). For analysis, test of significance were used and depending on the type of variable, Pearson and Spearman correlation tests were utilized to determine their relationships with the incidence of complications. P values <0.05 are considered significant.
Results
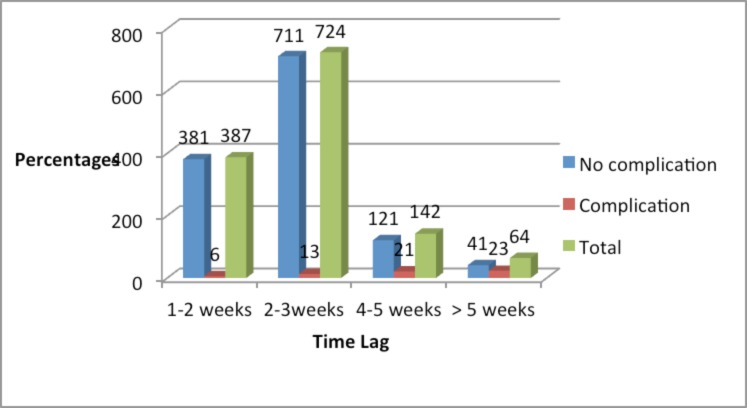
A total of 1,317 patients with 1,324 mandibular angle fractures were included in the study, and 63 patients had complications after treatment. The overall complication rate was 4.8% (63/1317) of the patients. The age and gender distribution of patients with complications are shown in Figure 3.
Figure 3.
Distribution of age and gender of patients with complications
Age (χ2= 142.592, df =7, p =0.02); Gender (χ2= 142.592, df=7, p=0.01).
There were 48 males and 15 females with male: female ratio of 3.2:1. The males outnumbered the females in all the age categories except the 56–65 years age groups where equal numbers of patients were recorded. The age of patients with complications ranged from 21 to 62 years (mean 37.4± 5.6 years). Also, more complications were recorded between 15–35 years (n=41/63, 65.0%) than 36–65 years (n=22/63, 35.0%). However, statistical test of significance between age and complications showed that the older the patient, the more the complications (p< 0.002) while for gender, males were more predisposed (p< 0.001). Furthermore, the gender (p= 0.01) and age (p= 0.02) distribution of patients with complications were significant.
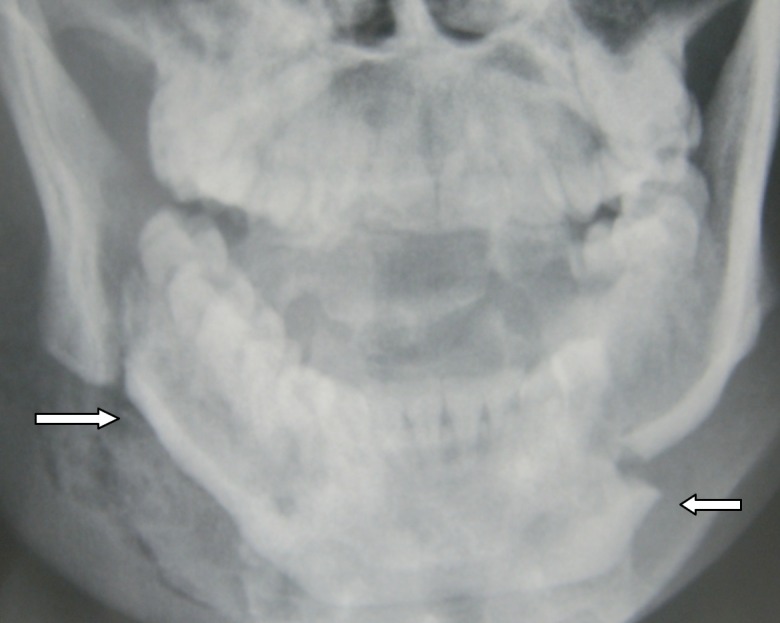
Road traffic accidents (RTA) were the major (n=54/63, 85.7%) cause of fractures that resulted in complications while assault accounted for 9/63 (14.3%). The test of significance between etiology and incidence of complications was in favour of RTA (p< 0.001). Figure 4 showed complications increased with increased time lag between injury and treatment of mandibular angle fractures, and this was significant (p=0.001). The test of significance between the time of injury and treatment and incidence of complications was statistically significant (p< 0.000).
Figure 4.
Distribution of time lag between injury and treatment of mandibular angle fractures
The distributions of complications according to the concomitant mandibular fractures are shown in Table 1. The complications associated with concomitant mandibular fractures were 90.5% (57/63) and others without similar fractures were 9.5% (6/63). The test of significance between associated mandibular fractures and incidence of complications was statistically significant (P< 0.000).
Table 1.
Distribution of complications according to concomitant mandibular fractures
| No complication | Complication | Total | ||||
| Number | % | Number | % | Number | % | |
| Concomitant fractures | ||||||
| Not present | 203 | 97.1 | 6 | 2.9 | 209 | 100 |
| Present | 1051 | 94.9 | 57 | 5.1 | 1108 | 100 |
| Distribution of concomitant fractures | ||||||
| Symphysis/body/condyle | 217 | 19.6 | 17 | 1.5 | 234 | 21.1 |
| Symphysis/parasymphysis/body | 208 | 18.8 | 15 | 1.4 | 223 | 20.2 |
| Parasymphysis | 165 | 14.9 | 8 | 0.7 | 173 | 15.6 |
| Body | 161 | 14.5 | 4 | 0.4 | 165 | 14.9 |
| Parasymphysis/body | 156 | 14.1 | 6 | 0.5 | 162 | 14.6 |
| Symphysis/condyle | 144 | 13.0 | 7 | 0.6 | 151 | 13.6 |
| Total | 1051 | 94.9 | 57 | 5.1 | 1108 | 100.0 |
Also symphysis/body/condyle and symphysis/parasymphysis/body fracture combinations resulted in more complications than the other concomitant mandibular fracture combinations. Furthermore, Table 2 showed the distribution of complications according to concomitant fractures of mid-facial bones. These concomitant fractures associated with complications were 29/63 (46.0%) whereas 34/63 (54.0%) occurred without their involvement.
Table 2.
Distribution of complications according to concomitant fractures of the middle third of the facial bones.
| No complications | Complications | Total | ||||
| Concomitant fracture | Number | % | Number | % | Number | % |
| Not present | 955 | 96.6 | 34 | 3.4 | 989 | 100 |
| Present | 299 | 91.2 | 9 | 8.8 | 328 | 100 |
| Distribution of concomitant fractures | ||||||
| Type of fracture | ||||||
| Le Fort 1, 11, zygomatic complex | 80 | 24.4 | 9 | 2.8 | 89 | 27.2 |
| Le Fort 1, 11, 111 | 73 | 22.3 | 7 | 2.1 | 80 | 24.4 |
| Le fort 11, 111, nasal | 62 | 18.9 | 5 | 1.5 | 67 | 20.4 |
| Zygomatic complex | 47 | 14.3 | 5 | 1.5 | 52 | 15.8 |
| Le Fort 1, 11 | 37 | 11.3 | 3 | 0.9 | 40 | 12.2 |
| Total | 299 | 91.2 | 29 | 8.8 | 328 | 100.0 |
The test of significance between associated mid-facial fractures and incidence of complications was statistically insignificant (p< 0.64). Also more subjects were recorded with fracture combinations of Le fort 1, 11, zygomatic complex and Le fort 1, 11, 111. All the patients with compound, unfavorable and non-comminuted mandibular angle fractures were treated with trans-osseous wire osteosynthesis and inter-maxillary fixation. All the fractures in patients that had complications were also accessed through submandibular incision. The inter-maxillary fixation (IMF) was released between four to six weeks postoperatively.
The mean follow-up period after the treatment of mandibular angle fractures was 21.7± 6.3 months (range six weeks–5.8 years). The diagnosis of the complications was made during follow-up between 2 days to 38.4 months (mean 16.4± 1.7 months) after the treatment of the compound, unfavorable and non-comminuted mandibular angle fractures. The complications diagnosed are shown in Table 3.
Table 3.
Distribution of complications
| Complications | Frequency | % |
| Deranged occlusion | 19 | 28.8 |
| Limited mouth opening <35mm | 16 | 24.2 |
| Facial asymmetry | 11 | 16.7 |
| Numbness of lower lip/tongue | 9 | 13.7 |
| Hypertrophied scar | 5 | 7.6 |
| Keloid | 2 | 3.0 |
| Hemorrhage | 2 | 2.0 |
| Infection | 2 | 3.0 |
| Total | 66 | 3.0 |
Deranged occlusion and limited mouth opening <35mm (n=35, 53.0%) were the most common. These complications were treated by jaw exercises/physiotherapy for limited mouth opening; occlusal grinding and equilibration for deranged occlusion and facial asymmetry (i.e. minimal occlusal deviation that lead to facial asymmetry were corrected by occlusal grinding and equilibration); excision for keloid; topical application of neopresol on hypertrophied scar and the excised keloid scar; and the use of clindamycin for the treatment of infection (Table 4).
Table 4.
Treatment of complications
| Complications | Frequency | % |
| Jaw exercises | 25 | 32.0 |
| Physiotherapy | 18 | 23.1 |
|
Occlusal grinding/equilibration |
13 | 16.7 |
| No treatment | 11 | 14.1 |
| Topical neopresol | 7 | 9.0 |
| Excision of keloid | 2 | 2.6 |
| Clindamycin | 2 | 2.6 |
| Total | 78 | 100.1 |
Numbness of the lower lip/tongue resolved spontaneously between 8.2 weeks and 3.6 years, while one case each of deranged occlusion and limited mouth opening also resolved without treatment. Cases of reactionary hemorrhage were controlled by packing with gauze, biting and digital pressure. All the complications were successfully treated during follow-up.
Discussion
This study shows that following the treatment of compound, unfavorable and non-comminuted mandibular angle fractures caused by RTA and assault by trans-osseous wiring and inter-maxillary fixation, complications occurred in certain subjects, and increased with increasing age, male gender, RTA, longer time lag between injury and treatment of fractures, and when there are associated concomitant mandibular fractures. The complication rate of 4.8% obtained is within the range of 0–32.0% that was earlier reported when hard-ware osteosynthesis was used as a method of fixation; although these previous studies were not restricted to compound, unfavorable and non-comminuted mandibular angle fractures.7,8,15,16 However, the complication rate obtained in each study will depend on the sample size, study duration, type of mandibular angle fracture, time lag between injury and treatment, surgical approach, treatment employed, material used for the fixation after reduction and the genetic makeup of the patient among others.7,8
Consequently, the complication rate obtained in this study may be due to the angle fractures being compound, non-comminuted and unfavorable, not diagnosed and treated early, IMF used for the treatment of the fractures and treatment concentrated on other fractures of the mandible and mid-facial bones, coupled with insufficient jaw exercises after release of inter-maxillary fixation that might have followed. In a recent study in this environment it was stated that some patients do not seek early dental care which may be the reason for the delayed treatment.17 Consequently, it is also possible that some patients who developed complications were not identified because they did not return for evaluation and treatment. All these factors acting in isolation or together with the genetic disposition of the patients may have accounted for the prevalence of complications obtained in this study.
Rigid internal fixation differ from non-rigid fixation such as trans-osseous wiring in that it provides fixation forces that exceed functional forces across the fracture site after reduction leading to primary bone union and limited postoperative physiological function.9 The advantages of rigid internal fixation over non-rigid fixation such as trans-osseous wire osteosynthesis, therefore, cannot be overemphasized as it leads to early mobilization and restoration of jaw functions, improved nutritional status, better oral hygiene, patient comfort and earlier return to work and social activities.7,8,18 This enhances and improves the patients' wellbeing in the postoperative period thereby leading to better patient satisfaction and treatment outcome. Therefore it is the preferred treatment of choice of compound, unfavorable and comminuted mandibular angle fractures in well equipped centres across the globe.
On the contrary, the use of inter-osseous wires like in trans-osseous wiring does not provide sufficient inter-fragmentary stability to permit use of the jaw during healing.7–9 The inter-maxillary fixation provided the true stabilization of the fractures, while the trans-osseous wiring only served the purpose of realignment of parts of the fractured bone segments and prevent their displacement by the muscles of mastication.8,9 Also, patients who received inter-maxillary fixation will lose more weight and take longer period to regain pre-injury mouth opening.7,8
As a result of the prevalence obtained in this study (n=63/1317, 4.8%), it is certain that majority of the patients with compound, unfavorable and non-comminuted mandibular angle fractures did not have complications. It has been stated that all successful treatment of mandibular fractures depends on undisturbed healing in the correct anatomic position under stable conditions, and failure results in complications such as infection, malocclusion, nonunion and mal-union.6 Consequently, operative treatment such as trans-osseous wire osteosynthesis must provide the predictable means of maintaining the pre-injury bone position throughout the course of healing.6–8 Furthermore, contributing to the successful treatment in the present study may also have been that the patients' complied with the postoperative instructions including during the period of post inter-maxillary fixation.
The mandibular angle fractures and its complications can occur at any age and in both gender.7,19 Earlier researchers have stated that the younger the age of the patient, the less the chances of developing complications.20,21 The rich vascularized lamellar bony structures in adolescents and young adults with greater exuberant osteoblastic activity and reparative potentials are less prone to developing complications than the sclerotic lamellar bony structures in matured adults.8, 22 However, because more of these fractures occurred in the younger age groups, and in males more than females, may be the reasons for the higher complications in these groups.
When mandibular angle fractures occur, it is often associated with concomitant fractures of other parts of the mandible which leads to further increase in mandibular arch. This increase in size of the mandibular arch was shown to be associated with the development of complications.23, 24 In the present study, majority, 90.5% (57/63) of the patients with complications had concomitant mandibular fractures.
This is closely similar to the report of Xiang et al.25 who recorded associated anterior mandibular fractures in 13/16 (81.3%) of their patients with complications.
The mandibular angle fractures pose a unique challenge for surgeons because they have the highest reported postoperative complication rate of any mandibular area as the relatively small cross section of the angular region and the oblique and irregular fracture configuration make treatment unfavorable.8,26 The complications and their treatments recorded in the present study have been documented earlier when either rigid internal fixation or non-rigid fixation was used as the treatment method.3,7,8 The reactionary hemorrhage that occurred may have resulted from the submandibular incision used in accessing the fragments of the fractured mandibular angle. Susceptibility to infection is related to stability of bone fragments after reduction and fixation. It should be noted that lack of adequate stabilization leads to chronic inflammation which impairs the normal healing process, and can result in complications such as delayed union, non-union, or infection.27 Also, the infection may not have been due to the stainless steel wire used for osteosynthesis since it is an inert substance and does not give rise to inflammation or irritation of the tissues unless sepsis has been introduced.8 Also, as reported in the present study, the most common long-term complications are loss of sensation in the lower lip, cheek and tongue due to injury to inferior alveolar and lingual nerve.26, 27
The main cause of this nerve impairment in mandibular angle fractures has been reported to be the degree of displacement of the fragments.10,11,16 Clinical evidence shows that the bulk of the displacement occurs at the time of injury and is probably due to activation of the stretch reflex in the pterygo-masseteric sling by the injuring force.9 The posterior fragment is held in its displaced position by the reflex spasm imposed upon the muscles by pain while the tooth bearing fragment is secondarily displaced in an anterior and contra-lateral direction.8–9 Furthermore, fractures at the angle prevents the elevator muscles attached to the ascending ramus from having any direct effect on the tooth bearing fragment, and there is a tendency for the posterior fragment to ride upwards, forwards and inwards as the medial pterygoid muscle exerts its action medially at about 30 degrees to the vertical axis.7–9 The hypertrophied scar and keloid formed were due to the extra-oral surgical approach employed in accessing the fractures as some patients particularly black skinned people are more prone to it. The limited mouth opening resulted from the use of inter-maxillary fixation for immobilization after fixation by trans-osseous wiring.
The deranged occlusion and facial asymmetry may have resulted from poor stabilization of the fractured fragments after reduction, fixation and immobilization. However, it should be noted that the occurrence of some complications may also be due to the inability of the patients to overcome the different neuromuscular and functional problems associated with the repositioning of the fractured segments.28
Follow-up of patients in this environment is poor; consequently the complications that might have developed later were not included. Because of unaffordability and unavailability, rigid internal fixation was not used for the treatment of the mandibular angle fractures. The use of rigid internal fixations would have improved the patients' wellbeing in the post-operative period, enhanced the treatment outcome, and reduced complications.
Conclusion
This study showed that post-traumatic complications occurred in certain subjects that had compound, unfavorable and non-comminuted mandibular angle fractures treated with trans-osseous wire osteosynthesis and inter-maxillary fixation. The major factors associated with it were increasing age, male gender, RTA, increase in time lag between injury and treatment of angle fractures, and concomitant mandibular fractures. Although there were complications which were managed successfully, the use of trans-osseous wire osteosynthesis gave good results. This will suggest that in contemporary practice, this method can still be useful specifically in centers that are less well equipped and where access to rigid internal fixation is limited.
Acknowledgement
We wish to express our sincere gratitude to Mrs Adiaha Ofem of the Department of Health Records and Information Management of this tertiary institution for her assistance in sorting out the case files of the subjects.
References
- 1.Boffano P, Roccia F. Bilateral mandibular angle fractures: clinical consideration. J Craniofac Surg. 2010;21:328–321. doi: 10.1097/SCS.0b013e3181cf5fbc. [DOI] [PubMed] [Google Scholar]
- 2.Anyanechi CE. Mandibular fractures associated with domestic violence in Calabar, Nigeria. Ghana Med J. 2010;44:155–158. doi: 10.4314/gmj.v44i4.68909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kyrgidis A, Koloutsos G, Kommata A, Lazarides N, Antoniades K. Incidence, aetiology, treatment outcome and complications of maxillofacial fractures. A retrospective study from Northern Greece. J Cranio-Maxillofac Surg. 2013;41:637–643. doi: 10.1016/j.jcms.2012.11.046. [DOI] [PubMed] [Google Scholar]
- 4.Pektas ZO, Bayram B, Balcik C, Develi T, Uckan S. Effects of different mandibular fracture patterns on the stability of miniplate screw fixation in angle mandibular fractures. Int J Oral Maxillofac Surg. 2012;41:339–343. doi: 10.1016/j.ijom.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 5.Myall RWT. Management of mandibular fractures in children. Oral Maxillofac Surg Clin North Am. 2009;21:197–201. doi: 10.1016/j.coms.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 6.Assael LA. Treatment of mandibular angle fractures: plate and screw fixation. J Oral Maxillofac Surg. 1994;52:757–761. doi: 10.1016/0278-2391(94)90495-2. [DOI] [PubMed] [Google Scholar]
- 7.Banks P, Brown A. Fractures of the Facial Skeleton. ed 2. Oxford, Woburn: Butterworth-Heinemann; 2001. [Google Scholar]
- 8.Malik NA. Textbook of Oral and Maxillofacial Surgery. ed 2. New Delhi: Jaypee Brothers; 2008. [Google Scholar]
- 9.Ellis E., III . The internal fixation of fractures: historical perspectives. In: Tucker MR, Terry BC, White RP, Van Sickel JE, editors. Rigid Fixation for Maxillofacial Surgery. Philadelphia: JB Lippincott; 1991. pp. 3–24. [Google Scholar]
- 10.Guimond C, Johnson JV, Marchena JM. Fixation of mandibular angle fractures with a 2mm 3 dimensional curved angle strut plate. Oral Maxillofac Surg. 2005;63:209–214. doi: 10.1016/j.joms.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 11.Juergen Z, Olivier L, Tateyuki L. Use of straight and curved 3 dimensional titanium miniplates for the fracture fixations at the mandibular angle. Oral Maxillofac Surg. 2007;65:1758–1763. doi: 10.1016/j.joms.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 12.Mehra P, Murad H. Internal fixation of mandibular angle fractures: comparisons of 2 techniques. Oral Maxillofac Surg. 2008;66:2254–2260. doi: 10.1016/j.joms.2008.06.024. [DOI] [PubMed] [Google Scholar]
- 13.Feledy J, Caterson EJ, Steger S. Treartment of mandibular angle fractures with a matrix miniplates: A preliminary report. Plast Reconstr Surg. 2004;114:1711–1716. doi: 10.1097/01.prs.0000142477.77232.f7. [DOI] [PubMed] [Google Scholar]
- 14.Hochuli-Vieira E, Ha TK, Pereira-Filho VA, Landes CA. Use of rectangular grid miniplates for the fracture fixations at the mandibular angle. J Oral Maxillofac Surg. 2011;69:1436–1441. doi: 10.1016/j.joms.2010.06.182. [DOI] [PubMed] [Google Scholar]
- 15.Haug RH, Prather J, Indresano AT. An epidemiological survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990;48:926–932. doi: 10.1016/0278-2391(90)90004-l. [DOI] [PubMed] [Google Scholar]
- 16.Lizuka T, Lindqvist C. Rigid internal fixation of fractures in the angular region of the mandible: An analysis of factors contributing to different complications. Plat Reconstr Surg. 1993;91:265–271. [PubMed] [Google Scholar]
- 17.Anyanechi CE, Saheeb BD. Reasons underlying failure to seek early dental treatment among patients presenting in a Nigeria Tertiary Hospital. J Med Biomed Res. 2013;12:37–45. [Google Scholar]
- 18.Ellis E. Treatment method of fractures of the mandibular angle. Int J Oral Maxillofac Surg. 1999;28:243–252. [PubMed] [Google Scholar]
- 19.Goth S, Sawatari Y, Peleg M. Management of Pediatric Mandible Fractures. J Craniofac Surg. 2012;23:47–56. doi: 10.1097/SCS.0b013e318240c8ab. [DOI] [PubMed] [Google Scholar]
- 20.Oji C. Fractures of the facial skeleton in children: A survey of patients under the age of 11 years. J Craniomaxillary Surg. 1998;6:322–326. doi: 10.1016/s1010-5182(98)80062-0. [DOI] [PubMed] [Google Scholar]
- 21.Arotiba GT. Fractures due to road traffic accident in Lagos, Nigeria. Nig Med J. 1996;30:66–69. [Google Scholar]
- 22.Remi M, Christine MC, Gael P, Soizick P, Joseph-Andre J. Mandibular fractures in children: long term results. Int J Pediatr Otorhinolaryngol. 2003;67:25–30. doi: 10.1016/s0165-5876(02)00288-4. [DOI] [PubMed] [Google Scholar]
- 23.Ellis E., III Complications of mandibular condylar fractures. Int J Oral Maxillofac Surg. 1998;27:255–259. doi: 10.1016/s0901-5027(05)80506-5. [DOI] [PubMed] [Google Scholar]
- 24.Arakeri G, Kusanale A, Zaki GA, Brennan PA. Pathogenesis of post-traumatic ankylosis of the temporo-mandibular joint: a critical review. Br J oral Maxillofac Surg. 2012;50:8–12. doi: 10.1016/j.bjoms.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 25.Xiang GL, Long X, Deng MH, Han QC, Meng QG, Li B. A retrospective study of temporomandibular joint ankylosis secondary to surgical treatment of mandibular condylar fractures. Br J Oral Maxillofac Surg. 2014;52:270–274. doi: 10.1016/j.bjoms.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 26.Perez R, Oeltien JC, Thaller SR. A review of mandibular angle fractures. Craniomaxillofac Trauma Reconstr. 2011;4:69–72. doi: 10.1055/s-0031-1272903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hung W, Li Z. Do traumatic brain injuries result in accelerated mandibular fracture healing? J Oral Maxillofac Surg. 2012;70:2135–2142. doi: 10.1016/j.joms.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 28.Worsaae N, Thorn JJ. Surgical versus non-surgical treatment of unilateral dislocated low subcondylar fractures: a clinical study of 52 cases. J Oral Maxillofac Surg. 1994;52:353–360. doi: 10.1016/0278-2391(94)90436-7. [DOI] [PubMed] [Google Scholar]