Abstract
This study was aimed to identify and evaluate the International Classification of Functioning (ICF) key codes for dysphagia in stroke patients. Thirty patients with dysphagia after stroke were enrolled in our study. To evaluate the ICF dysphagia scale, 6 scales were used as comparisons, namely the Barthel Index (BI), Repetitive Saliva Swallowing Test (RSST), Kubota Water Swallowing Test (KWST), Frenchay Dysarthria Assessment, Mini-Mental State Examination (MMSE), and the Montreal Cognitive Assessment (MoCA). Multiple regression analysis was performed to quantitate the relationship between the ICF scale and the other 7 scales. In addition, 60 ICF scales were analyzed by the least absolute shrinkage and selection operator (LASSO) method. A total of 21 ICF codes were identified, which were closely related with the other scales. These included 13 codes from Body Function, 1 from Body Structure, 3 from Activities and Participation, and 4 from Environmental Factors. A topographic network map with 30 ICF key codes was also generated to visualize their relationships. The number of ICF codes identified is in line with other well-established evaluation methods. The network topographic map generated here could be used as an instruction tool in future evaluations. We also found that attention functions and biting were critical codes of these scales, and could be used as treatment targets.
Keywords: correlation analysis, dysphagia, International Classification of Functioning (ICF), key codes, stroke
1. Introduction
Stroke is a leading cause of death in Asia.[1] Poor prognostic factors for acute ischemic stroke include increased age, inheritance, hypertension, heart disease, etc. The common complications of stroke include hemiplegia, urination disorders, and dysphagia.[2] Predictors of good outcome for patients with acute ischemic strokes (in terms of in-hospital mortality and cognitive and functional performance) include higher systolic blood pressure at admission, higher total cholesterol plasma levels, and a lower Charlson index.[3,4] Clinical evaluation of stroke patients often involves tests of swallowing dysfunction (i.e., dysphagia), as dysphagia is the most common clinical symptom and functional deficit following a stroke.[5] A medical complication of dysphagia includes aspiration pneumonia, dehydration, significant weight loss, and malnutrition.[6] Another complication of dysphagia in stroke patients is psychosocial because eating is a pleasurable and social activity, and inability to eat normally may affect patient morale and quality-of-life.[7]
The International Classification of Functioning (ICF), Disability, and Health was established in 2001 by the World Health Organization (WHO). ICF is a classification of health and health-related domains that provides the framework for measuring health and disability at both individual and population levels.[8] Since the establishment of the ICF, it has been widely used by clinicians. ICF can be performed by self-evaluation, by health care workers or community agencies, or a combination of these. It has been applied to patients with numerous neurological disorders, including spinal cord injury, stroke, Parkinson disease, leprosy, and polio. It is also used in clinical research and rehabilitation evaluation. For instance, ICF was used to assess limb spasticity of stroke patients and overall function of disability. The results of these studies confirmed that the scale is reliable and valid.
In 2007, Dr Threats[9] evaluated dysphagia of stroke patients by using 4 major components of the ICF: Body Structures, Body Functions, Activities, and Participation and Environmental Factors. However, this method was not practically feasible in the clinical practice, as it consisted of numerous, complicated items. Further, completing Dr Threat's 60 ICF codes is fairly time-consuming, which takes 40 to 60 minutes per patient—a length of time not feasible for busy clinics. Also problematic is that the Chinese diet is very different from that of Western countries. His study focused on general dysphagia and not specifically for the stroke patients. On the basis of Dr Threats’ study, and considering the characteristics of dysphagia following stroke, we systematically simplified Dr Threats’ 60 ICF codes and tested its accuracy in hospitalized patients in China.
2. Methods
2.1. Study subjects
Thirty patients with dysphagia following a stroke were enrolled in this study. All subjects were admitted between January 2014 and March 2014 to our hospital. Patients included in the study needed to fit well-defined inclusion criteria: (1) Subjects had to have cerebrovascular disease, which was evaluated on the basis of the diagnostic criteria contained in the seventh edition of Neurology[10]; (2) Subjects had dysphagia, as confirmed by Toronto Bedside Swallowing Screening Test (TOR-BSST)[7]; (3) Subjects were conscious with stable vital signs; and (4) Subjects were older than 18 years of age. Exclusion criteria included (1) Patients with severe cardiopulmonary dysfunction or liver or kidney disorders; (2) Patients with any malignant, metabolic, or gastrointestinal disease, or pulmonary infection; (3) Patients with any disease that affected swallowing function, such as severe diabetic peripheral neuropathy, Alzheimer disease, myopathy, or arthropathy. The experimental protocol was established, according to the ethical guidelines of the Helsinki Declaration and was approved by the Human Ethics Committee of The Second Xiangya Hospital of Central South University. Written informed consent was obtained from individual participants.
2.2. Classification
It is challenging to identify the pathogenesis and cause of patients with acute ischemic stroke, and thus no standard procedures for diagnosis are currently available. However, a widely used system for categorization of subtypes of ischemic stroke mainly based on etiology has been developed for the Trial of Org 10172 in Acute Stroke Treatment (TOAST). The TOAST classification denotes 5 subtypes of ischemic stroke: (1) large-artery atherosclerosis (LAA); (2) cardioembolism (CE); (3) small-vessel occlusion (SAA); (4) stroke of other determined etiology (SOE); and (5) stroke of undetermined etiology (SUE).[11] We used TOAST to classify our patients included in this study.
2.3. Assessment of dysphasia
The Toronto Bedside Swallowing Screening Test (TOR-BSST) is a screening instrument to identify dysphagia in stroke survivors across the continuum of care, and mainly applied in stroke patients in the acute phase and recovery period.[12] Dr Threats proposed 60 codes for the ICF,[13] which included 15 Body Structures, 27 Body Functions, 8 Activities and Participation, and 10 Environmental Factors. All ICF codes had qualifiers that indicate the severity of the limitation or restriction. These universal qualifiers attached to the ICF codes ranged from 0 (no problem or within normal limits) to 4 (complete or profound problem). In addition, a value of 8 indicates unspecific information, while 9 indicates that it was unavailable. The letter C indicates a complication related to health and function. The Toronto Bedside Swallowing Screening Test (TOR-BSST) was performed as a confirmation of dysphagia in stroke patients.[12] We used the TOR-BSST experiment to first identify whether the patient had a swallowing dysfunction. We then determined which patients qualified for the study. Lastly, we evaluated these patients with the 60 ICF codes.
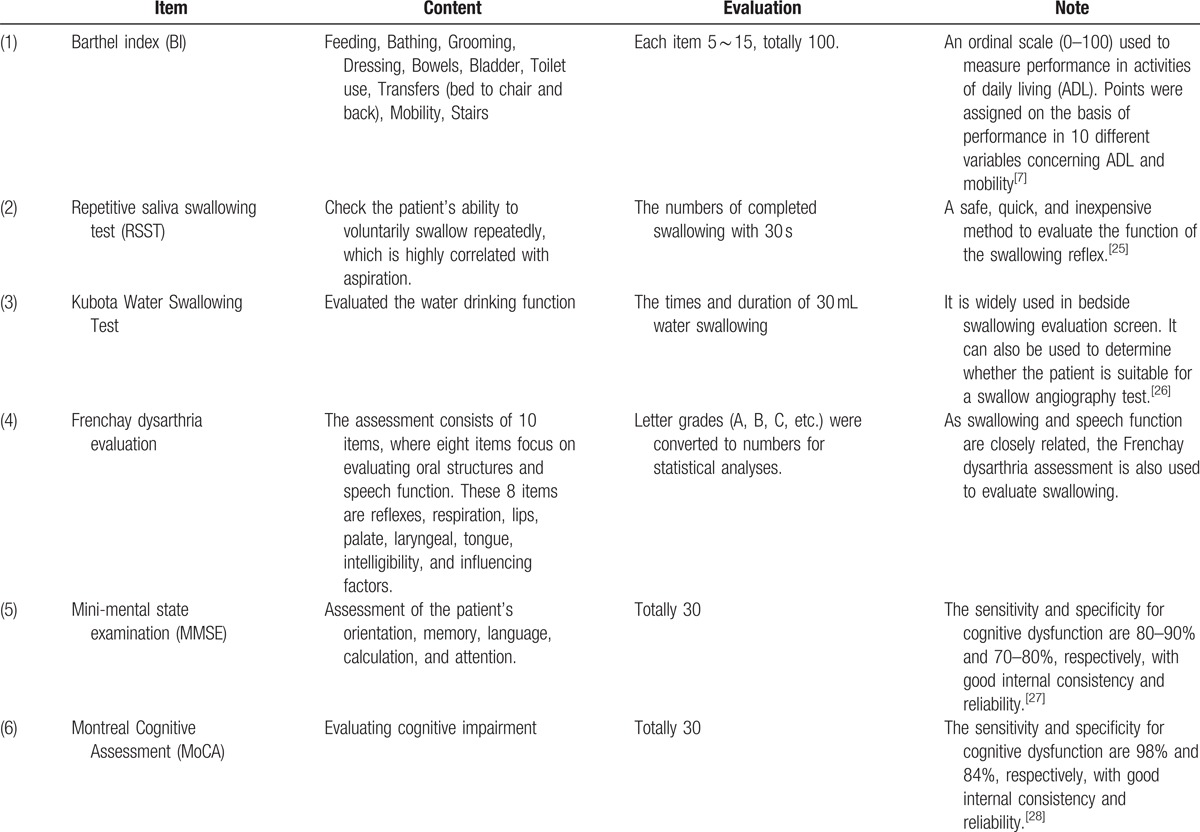
All 6 of the following scales were used to assess dysphasia following a stroke in all 30 subjects included in our study: Barthel index (BI), Repetitive saliva swallowing test (RSST), Kubota Water Swallowing Test, Frenchay dysarthria evaluation, mini-mental state examination (MMSE), and the Montreal Cognitive Assessment (MoCA) (Table 1).
Table 1.
Scales of dysphasia assessment.
2.4. Statistics
The ICF swallowing disorder scale and the other 6 scales were analyzed by multivariate regression in SPSS 16.0 statistical software. We consolidated several similar variables into a few unified categories[13] in order to identify the most important ICF codes associated. Threats’ 60 ICF codes were regarded as the independent variables, whereas the BI, Frenchay dysarthria assessment, MMSE, MoCA, KWST, and RSST were regarded as the dependent variables. A stepwise regression analysis was performed. The inclusion criterion was P < 0.05, exclusion criterion was P > 0.1, and the standardized regression coefficient of 1 indicated significant correlation. Stepwise regression analysis with so many variables can cause problems of low sensitivity and specificity.[10] Data were therefore also analyzed by the “least absolute shrinkage and selection operator” (LASSO) method.[14,15] LASSO is a shrinkage and selection method for linear regression that is widely used in large regression analyses. The method minimizes the sum of squared errors with a cap on the sum of the absolute values of the coefficients. ICF codes were again the independent variables, and the dysphasia assessments were regarded as dependent variables.[14]
3. Results
3.1. General information
A total of 30 stroke patients with swallowing disorders but stable vital signs were enrolled in our study. The male:female ratio was 18:12, ages ranged from 21 to 82 years (63.13 ± 15.65 years), body weight ranged from 49 to 78 kg (66.10 ± 9.56 kg), and height ranged from 155 to 178 cm (166.87 ± 8.73 cm). The education level was from 0 to 16 years (10.83 ± 5.02). Among these 30 cases, 2 patients had CE, 19 had LAA, and 9 patients had SAA. Notably, the majority of these patients had LAA, and the rest of them had either SAA or CE. We did not enroll the patients with SUE or SOE.
Regarding the duration from the initiation of clinical symptoms to the time point that patient was enrolled in the study, 6 cases had less than 30 days, 16 cases had 31 to 180 days, and 8 patients had more than 180 days. Eleven cases had a lesion on the left side, 13 had lesions on the right side, 3 cases had bilateral multiple lesions, and 3 patients had brainstem lesions.
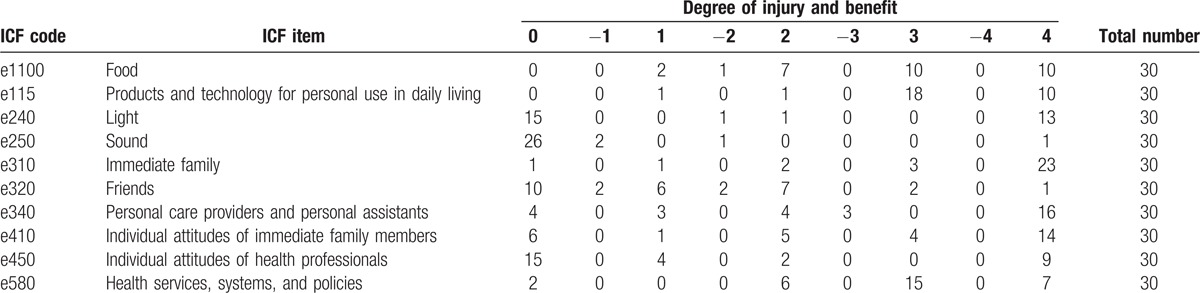
3.2. ICF swallowing disorder scale
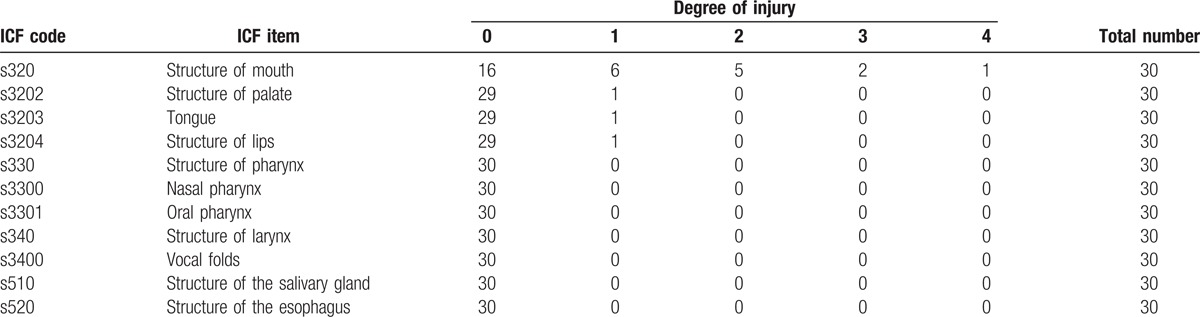
The ICF evaluation form published by Dr Threats was used to assess patients’ swallowing function. The scores of these 60 codes from 30 patients were evenly distributed, and are summarized in Tables 2–5.
Table 2.
Body Functions evaluation.
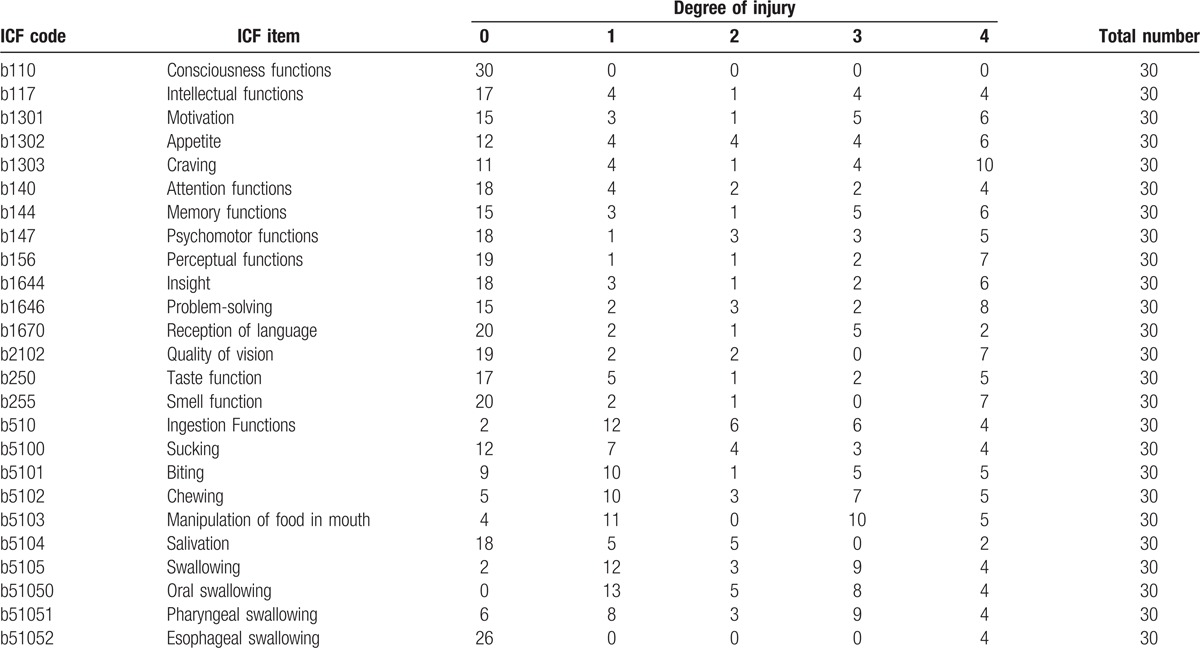
Table 5.
Activities and Participation evaluation.
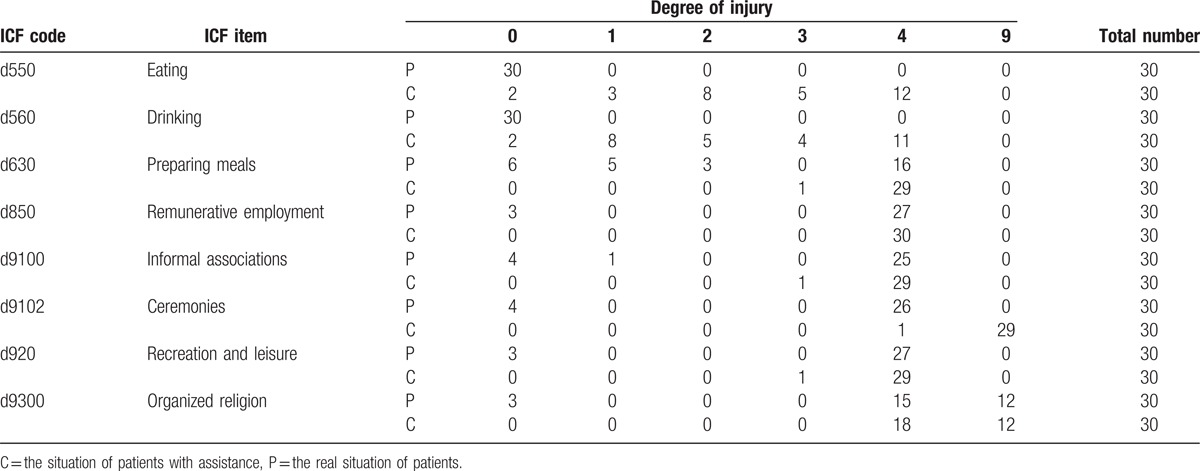
Table 3.
Environmental Factors evaluation.
3.3. Relationship between ICF scale and other rating scales
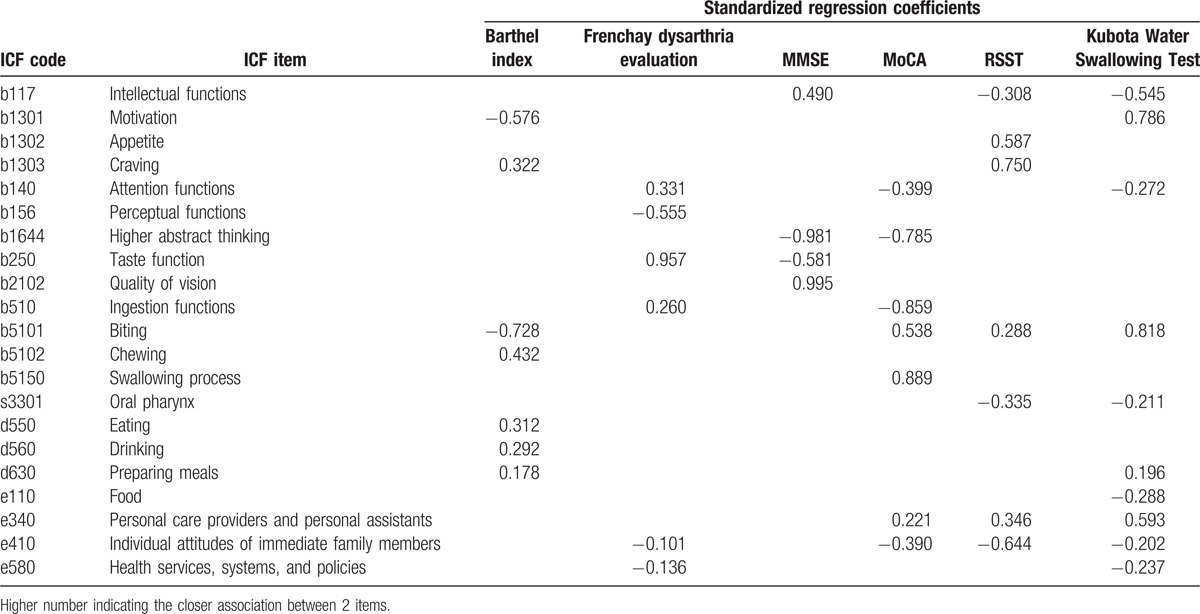
Among the 60 items from the ICF scale, 21 of them were associated with the other 6 scales. These included 13 Body Functions codes (b1644: higher abstract thinking, b250: taste function, b2102: quality of vision, b510: ingestion functions, b5101: biting, b5102: chewing, b117: intellectual functions, b1301: motivation, b1302: appetite, b1303: craving, b140: attention functions, b156: perceptual functions, b5150: swallowing process), 1 Body Structure code (s3301: oral pharynx), 3 Activities and Participation codes (d550: eating, d560: drinking, d630: preparing meals), and 4 Environmental Factors codes (e110: food, e340: personal care providers and personal assistants, e410: individual attitudes of immediate family members, e580: health services, systems, and policies). The standardized regression coefficients of each scale are listed in Table 6.
Table 6.
ICF codes associated with other scales and standardized regression coefficients.
3.4. Relationship between codes of the ICF scale
The conditional connection was obtained by the LASSO method and the relationships between them were visualized in a network topographic map (Fig. 1). Lines with arrows in the network indicate the connection between dependent variable and variable. As seen in Fig. 2, the left column of this network contains 39 codes and are collectively called the “main component.”[10] In this main component, attention functions (b140) and biting (b5101) were the most prominent, with 9 directly connection (Tables 4 and 5).
Figure 1.
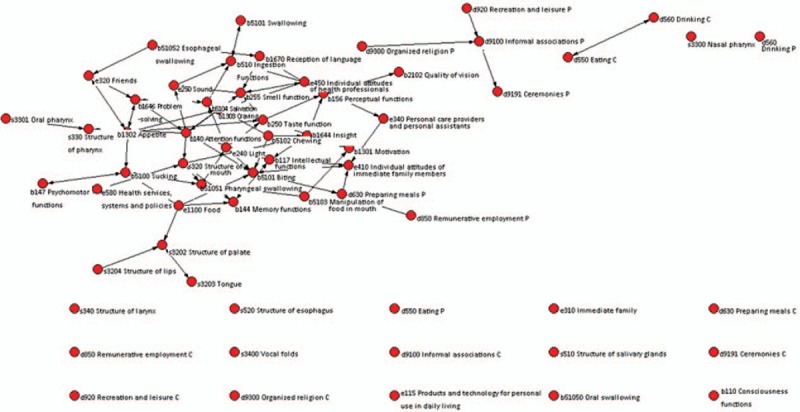
ICF codes are key points and nodes of this complex map. Each node is an ICF code and is connected with several other nodes in the network. The degree of connectivity gives a k value, where the greater the k value, the greater the node structure stability with network effects. The left side of the network contains 39 codes and are collectively considered the “main component.”[12] P: the real situation of patients; C: the situation of patients with assistance. The listed items in the end have no relationship with the other items.
Figure 2.
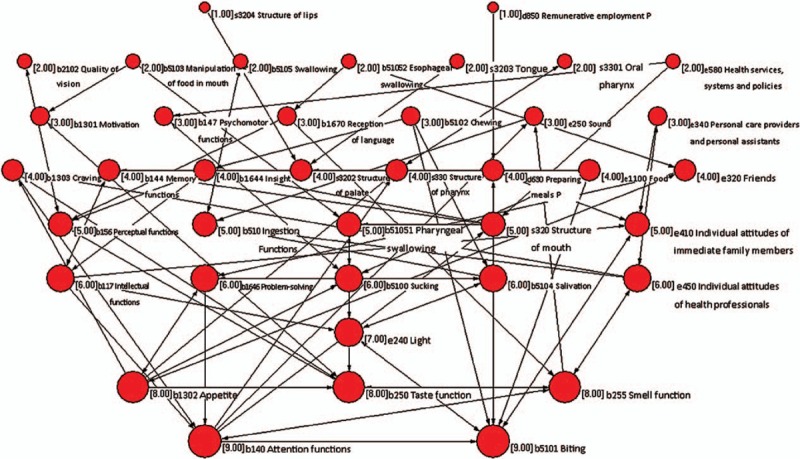
The numbers in front of each code represent the numbers of other codes that are related to that code. Attention functions (b140) and Biting (b5101) codes are the center of main component, with 9 variables directly connecting.
Table 4.
Body Structures evaluation.
4. Discussion
We identified 21 key codes from the original 60 codes. These 21 codes proficiently evaluate stroke patients using 4 major ICF components, including Body Structures, Body Functions, Activities, and Participation and Environmental Factors.
Of the 13 ICF Body Structure codes, we found significant regression coefficients between the MMSE scale and higher abstract thinking (b1644; -0.981) as well as with quality of vision (b2102; 0.995; Table 2). Thus, these ICF codes seem to be consistent with MMSE assessment of cognitive functions. If a patient has poor stroke-induced cognitive function, then he/she is unable to complete the first stage of swallowing, and thus suffers of a wallowing disorder.
The complete swallowing process can be divided into 5 discernable stages: Cognition stage, Preparation stage, Oral phase stage, Pharyngeal stage, and Esophagus stage. The first stage involves sensing the solidity, bite size, temperature, and the taste and smell of the food. The speed and volume of eating is then evaluated. This shows that it is thus a conscious act.[16] In addition, cognitive input was required to achieve the optimal effect. Other codes such as intellectual functions (b117), motivation (b1301), appetite (b1302), craving (b1303), attention functions (b140), insight (b1644), taste function (b250), and quality of vision (b2102) were also components of this cognitive input. The dysfunction of these codes would increase the risk of choking on water, slow eating, or aspiration and suffocation.[17] For this reason, consciousness functions (b110) are important to evaluate in order to know whether the patient can complete the swallow process. This code was unable to be evaluated here, as all subjects were alert with normal consciousness. Taste function (b250) and quality of vision (b2102) were related to the cognitive input of color, flavor, and taste of food before eating. It will be important to improve these codes in order to help patients with dysphasia to take in food appropriately.
Taste function (b250) was negatively correlated to MMSE, thus suggesting that patients with less cognitive function impairment require high-quality food with good color, flavor, and taste. As patients in the hospital consume plain food with limited condition, taste function of these patients is usually substantially impaired. A possible solution would be to provide delicious food to patients in order to meet their needs and eating habits as well as to improve patients’ eating motivation. However, care should be taken not to compromise the nutritive qualities of meals (e.g., salty, greasy, etc.).
Oral Transit Phase consists of a few steps: tongue propulsion of the bolus for passage to the pharynx, the pharyngeal phase of the swallow, and forcing the food downward from pharynx to the esophagus.[18] These steps are assessed by b510 ingestion, b5101 biting, b5102 chewing, and b5150 swallowing process. It should be noted that regional differences, social-cultural background, and eating habits may also affect swallowing dysfunction and ICF codes. All subjects in our study were from the urban area of Nanjing, China, and have similar eating habits. As many of our patients are nonreligious, the results for the ICF code, organized religion (d9300), may not be representative of other cultures.
Swallowing disorders can be categorized into structural swallowing disorders and functional neurological swallowing disorders. Our subjects did not have any structural disorders, but had neurological swallowing dysfunction. This was due to temporary loss of muscle neural control and lack of coordination between muscles and bones.[19] In some cases, oropharyngeal structures were damaged by nasogastric tubes, pharyngitis, or swollen tonsils.[20]
We found that 3 ICF Activities and Participation, namely eating (d550; 0.312), drinking (d560; 0.292), and preparing meals (d630; 0.178), are related to the BI. These results are in line with the BI for evaluating patients’ ability to swallow independently. It should be noted that the swallowing function scale focuses mainly on the simple functions of eating and drinking and do not take into account patients’ functions in everyday lives.[9] As eating is a social behavior, we also need to address dysphagia in patients’ daily living activities and socializing. In fact, this is the main purpose of the modern rehabilitation concept and is a notable advantage of the ICF scale. The Activities and Participation codes dealing directly with the intake of food and liquid (Fig. 1) also have positive or negative effects on swallow function of the patients. Two value limits are used in Activities and Participation. The first level limit (P) refers to the ability in the real environment (ability + environment), while the second level limit (C) refers to the ability in environment without assistance. We observed that most patients have some level of difficulty with the second level limit. The first level limit of Activity and Participation was significantly reduced, or even disappeared. As shown in Fig. 1, positive environmental factors have positive effects on the activity and function of patients.
With regard to employment, we considered several factors involved in these impairments: (1) Stroke patients were older and usually retired; (2) All subjects were hospitalized and left their jobs temporarily; (3) As strokes can be severely debilitating, some patients are not capable to continue working; and finally (4) Discrimination from social employment. Due to this discrimination, most patients were reluctant to participate in social activities with friends or family members.[21] Other stroke-induced disabilities also limit activities between patients and social acquaintances. Environmental factors are therefore critical in activation and participation. Imperfect social barrier-free facilities limit the activity of stroke patients, particularly when they are alone. Every effort should be made to provide favorable environmental factors for these patients.[22–26]
The Environmental Factor codes for food (e1100), personal care providers and personal assistants (e340), individual attitudes of immediate family members (e410), and health services, systems, and policies (e580) also have effects on the prognosis of patients’ dysphagia.
Environmental factors of ICF have both positive and negative effects on swallowing disorder. For example, appropriate viscosity of food (e110), the individual attitudes of immediate family members (e410), and the skills and abilities of personal care providers and personal assistants (e340) play a positive role in patients’ swallowing function. Other factors reduce the risk of choking and aspiration. Health services, systems, and policies (e580) as well as patients’ individual medical insurance policies play key roles for most patients.
On the basis of patients’ overall conditions, all ICF codes have complex correlations. According to Fig. 1, ICF codes are key points and nodes of this complex map. Each node is connected with several other nodes in the subnetwork. The number of nodes give a k value, where the greater the k value, the greater the node structure stability with network effects.[26] According to Fig. 2, 21 ICF codes are particularly important, with attention function (b140) and biting (b5101) as the most important in this network. By using topographic maps, the relationship between ICF codes is more easily visualized, which aids in simplifying the evaluation process. For example, for patients with neurological dysfunctions, we can quickly identify the ICF codes associated with this characteristic on the topographic map. Clinicians are therefore better able to solve a problem and develop a plan of rehabilitation.
The function map can be utilized in real life to resolve clinical problems. In particular, pharynx oral structure (s330), olfactory structure (s320), olfactory function (b255), biting (b5101), sound (e250), problem resolving (b1646), addiction (b1303), intelligence (b117), and attention (b140) are all extremely relevant. It is also reasonable to postulate that sound of environment may also affect attention function of patients eating. Patients with impaired olfactory function and swallowing dysfunction may also affect attention. However, taste function (b250) is not directly related to attention function, but is closely related to olfactory function and affects attention function. Patients with disrupted attention dysfunction have greater intelligence functions and problem-solving skills. These patients tend to have food addictions.
The relationships between attention function (b140), light (e240), chewing (b5102), preparing meals (d630), food (e110), immediate family member (e410), and biting (b5101) can be easily observed in real life. For example, chewing and biting are processes that grind food in the mouth. Further, attention function has an effect on biting, and thus the patient with more attention can bite more. In contrast, patients with less attention dysfunction have problems with biting. It appears that there is no relationship between meal preparation and bite. However, if patients can prepare meals by themselves, or are involved in preparation, they can prepare food that they like. In addition, immediate family members, light of environment, and personal attitudes are relevant with the biting. The improvement of biting also has a positive effect on immediate family members. Therefore, patients with good relationships with family members and increasing attention function will be more likely to improve biting.
Compared with original 60 ICF codes, our key items contained only 21 ICF codes, thus 66% less than the number of original codes. Undoubtedly, we can shorten the time of clinical evaluation, and improve working efficiency. We will also confirm these findings in the future clinical work. In addition, our study addressed that the key codes of evaluation are attention function and biting.
This study has several limitations, such as the relatively small sample size. We are collecting more cases for large sample study. Our study focused on the local Hunan patients. It should be noted that the different area of China had different diet habitation, which might interfere with study results. Future studies will expand the sample size analyzed here. In addition, we plan to further simplify the 21 ICF codes and make clinical observations for reliability and validity.
5. Conclusion
Our study identified 21 ICF codes for swallowing disorders after stroke, which agree with other methods of dysphasia assessment. Our topographic network map of swallowing disorder function could be used as a guidance tool for future dysphasia assessments. These analyses identified attention function (b140) and biting (b5101) as particularly important as treatment targets. It will be important for future such studies to expand the sample size and to include multiple geographical regions with multiple study groups. Most importantly, it is essential to establish amended ICF code criteria in order to improve the assessment of dysphasia following stroke.[24] The revised codes reported here will be valuable for clinicians and rehabilitation staff.
Footnotes
Abbreviations: ADL = activities of daily living, BI = Barthel Index, ICF = International Classification of Functioning, KWST = Kubota Water Swallowing Test, LASSO = least absolute shrinkage and selection operator, MMSE = Mini-Mental State Examination, MoCA = Montreal Cognitive Assessment, RSST = Repetitive Saliva Swallowing Test, TOR-BSST = Toronto Bedside Swallowing Screening Test.
YD and C-JZ are cofirst authors.
The authors have no conflicts of interest to disclose.
References
- 1.Hoy DG, Rao C, Hoa NP, et al. Stroke mortality variations in South-East Asia: empirical evidence from the field. Int J Stroke 2013; 8 (Suppl A100):21–27. [DOI] [PubMed] [Google Scholar]
- 2.Huo Yang GZ-y, Gao X-G. Influencing factors for the prognosis of acute stroke patients. Chin J Geriatr Heart Brain Vessel Dis 2014; 16:240–242. [Google Scholar]
- 3.Tuttolomondo A, Di Raimondo D, Di Sciacca R, et al. Effects of clinical and laboratory variables at admission and of in-hospital treatment with cardiovascular drugs on short term prognosis of ischemic stroke. The GIFA study. Nutr Metab Cardiovasc Dis 2013; 23:642–649. [DOI] [PubMed] [Google Scholar]
- 4.Tuttolomondo A, Di Sciacca R, Di Raimondo D, et al. Effects of clinical and laboratory variables and of pretreatment with cardiovascular drugs in acute ischaemic stroke: a retrospective chart review from the GIFA study. Int J Cardiol 2011; 151:318–322. [DOI] [PubMed] [Google Scholar]
- 5.Ho YH, Liu HY, Huang ST. The prevalence and signs of dysphagia among stroke patients in rehabilitation units. Hu Li Za Zhi 2014; 61:54–62. [DOI] [PubMed] [Google Scholar]
- 6.Martino R, Pron G, Diamant N. Screening for oropharyngeal dysphagia in stroke: insufficient evidence for guidelines. Dysphagia 2000; 15:19–30. [DOI] [PubMed] [Google Scholar]
- 7.Vesey S. Dysphagia and quality of life. Br J Commun Nurs 2013; 18:S14–S19. [DOI] [PubMed] [Google Scholar]
- 8.Geyh S, Cieza A, Schouten J, et al. ICF core sets for stroke. J Rehabil Med 2004; 135–141. [DOI] [PubMed] [Google Scholar]
- 9.Threats TT. Use of the ICF in dysphagia management. Semin Speech Lang 2007; 28:323–333. [DOI] [PubMed] [Google Scholar]
- 10.Ballert C, Oberhauser C, Biering-Sorensen F, et al. Explanatory power does not equal clinical importance: study of the use of the Brief ICF Core Sets for Spinal Cord Injury with a purely statistical approach. Spinal Cord 2012; 50:734–739. [DOI] [PubMed] [Google Scholar]
- 11.Lang Q, Zhou M, Feng H, et al. Research on the relationship between fibrinogen level and subtypes of the TOAST criteria in the acute ischemic stroke. BMC Neurol 2013; 13:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martino R, Silver F, Teasell R, et al. The Toronto Bedside Swallowing Screening Test (TOR-BSST): development and validation of a dysphagia screening tool for patients with stroke. Stroke 2009; 40:555–561. [DOI] [PubMed] [Google Scholar]
- 13.Lee YC, Chen SS, Koh CL, et al. Development of two Barthel index-based supplementary scales for patients with stroke. PLoS One 2014; 9:e110494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strobl R, Stucki G, Grill E, et al. Graphical models illustrated complex associations between variables describing human functioning. J Clin Epidemiol 2009; 62:922–933. [DOI] [PubMed] [Google Scholar]
- 15.Becker S, Strobl R, Cieza A, et al. Graphical modeling can be used to illustrate associations between variables describing functioning in head and neck cancer patients. J Clin Epidemiol 2011; 64:885–892. [DOI] [PubMed] [Google Scholar]
- 16.Radhakrishnan S, Menon UK, Anandakuttan A. A combined approach of bedside clinical examination and flexible endoscopic evaluation of swallowing in poststroke dysphagia: a pilot study. Ann Indian Acad Neurol 2013; 16:388–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kamide A, Hashimoto K, Miyamura K, et al. Assessment of feeding and swallowing in children: validity and reliability of the Ability for Basic Feeding and Swallowing Scale for Children (ABFS-C). Brain Dev 2015; 37:508–514. [DOI] [PubMed] [Google Scholar]
- 18.Poorjavad M, Jalaie S. Systemic review on highly qualified screening tests for swallowing disorders following stroke: validity and reliability issues. J Res Med Sci 2014; 19:776–785. [PMC free article] [PubMed] [Google Scholar]
- 19.Kim JH, Byun HY, Son S, et al. Retrospective assessment of the implementation of critical pathway in stroke patients in a single university hospital. Ann Rehabil Med 2014; 38:603–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Acciarresi M, De Luca P, Caso V, et al. Acute stroke symptoms: do differences exist between sexes? J Stroke Cerebrovasc Dis 2014; 23:2928–2933. [DOI] [PubMed] [Google Scholar]
- 21.Ma EP, Worrall L, Threats TT. The International Classification of Functioning, Disability and Health (ICF) in clinical practice. Semin Speech Lang 2007; 28:241–243. [DOI] [PubMed] [Google Scholar]
- 22.Nund RL, Scarinci NA, Cartmill B, et al. Application of the International Classification of Functioning, Disability and Health (ICF) to people with dysphagia following non-surgical head and neck cancer management. Dysphagia 2014; 29:692–703. [DOI] [PubMed] [Google Scholar]
- 23.Stucki G, Reinhardt JD, Grimby G, et al. Developing “Human Functioning and Rehabilitation Research” from the comprehensive perspective. J Rehabil Med 2007; 39:665–671. [DOI] [PubMed] [Google Scholar]
- 24.Tschiesner U, Stier-Jarmer M, Strieth S, et al. Development of an ICF-based clinical practice guideline for the assessment of function in head and neck cancer. Laryngorhinootologie 2013; 92:314–325. [DOI] [PubMed] [Google Scholar]
- 25.Paanalahti M, Alt Murphy M, Lundgren-Nilsson A, et al. Validation of the Comprehensive ICF Core Set for stroke by exploring the patient's perspective on functioning in everyday life: a qualitative study. Int J Rehabil Res 2014; 37:302–310. [DOI] [PubMed] [Google Scholar]
- 26.Wang P, Li H, Guo Y, et al. The feasibility and validity of the comprehensive ICF core set for stroke in Chinese clinical settings. Clin Rehabil 2014; 28:159–171. [DOI] [PubMed] [Google Scholar]
- 27.Pasi M, Salvadori E, Poggesi A, et al. White matter microstructural damage in small vessel disease is associated with Montreal Cognitive Assessment but not with mini mental state examination performances: Vascular Mild Cognitive Impairment Tuscany study. Stroke 2015; 46:262–264. [DOI] [PubMed] [Google Scholar]
- 28.Dag E, Ornek N, Ornek K, et al. Mini mental state exam versus Montreal cognitive assessment in patients with age-related macular degeneration. Eur Rev Med Pharmacol Sci 2014; 18:3025–3028. [PubMed] [Google Scholar]


