Abstract
Alcohol misuse among adolescents is a common issue worldwide and is an emerging problem in China. This study aimed to investigate the prevalence of alcohol drinking and alcohol-related problems among Chinese adolescents and to explore their risk factors and connections.
A cross-sectional study using an anonymous questionnaire was conducted among junior and senior high school students between 2010 and 2012. Data on self-reported alcohol use, alcohol-related problems, school factors, family factors, and psychosocial factors were collected. Descriptive analyses were made of the proportions of sociodemographics, family, school, and psychosocial factors. Multilevel logistic regression models were conducted to analyze the risk factors for alcohol drinking and alcohol-related problems.
Of the 105,752 students who ranged in age from 9 to 21 years, the prevalence of current drinking among students was 7.3%, and 13.2% students reported having alcohol-related problems. Male students were 1.78 (95% confidence interval [CI] = 1.69–1.87) times more likely to be involved in current drinking and 1.86 (95% CI = 1.79–1.93) times more likely to have alcohol-related problems. Higher grade level students were at a higher risk of current drinking (adjusted odds ratio [AOR] = 1.09, 95% CI = 1.05–1.13) and having alcohol-related problems (AOR = 1.43, 95% CI = 1.42–1.58). Older students were more likely to report current drinking (AOR = 1.06, 95% CI = 1.04–1.17) and having alcohol-related problems (AOR = 1.83, 95% CI = 1.82–1.85). Having poor classmate relations (AOR = 1.28, 95% CI = 1.03–1.37), having poor relationships with teachers (AOR = 1.08, 95% CI = 1.00–1.16), and below average academic achievement (AOR = 1.50, 95% CI = 1.41–1.59) were positively associated with current drinking. Moreover, students with suicidal ideation were at a higher risk of current drinking (AOR = 1.70, 95% CI = 1.61–1.81) and having alcohol-related problems (AOR = 2.08, 95% CI = 1.98–2.16). Having higher Center for Epidemiology Scale for Depression scores was positively associated with current drinking (AOR = 1.09, 95% CI = 1.05–1.11) and having alcohol-related problems (AOR = 1.08, 95% CI = 1.06–1.18).
Alcohol drinking and alcohol-related problems among Chinese adolescents are major public health problems, and effective preventive programs will require full consideration of the individual, social, and environmental factors that facilitate and prevent alcohol use.
Keywords: adolescents, alcohol drinking, alcohol-related problems, China, large-scale
1. Introduction
Adolescence is a period filled with immense behavioral, psychological, and social changes and challenges.[1] This life stage is characterized by increased imitation and exploration along with a range of risky behaviors, including substance use.[2] Among adolescents, alcohol consumption is a common behavior in modern society; however, this behavior has some related negative traits that can inhibit an individual's growth and maturation.[3] Previous studies have demonstrated that adolescents might exhibit an idiosyncratic pattern of reactivity to alcohol that might expose them to higher risk of use and that alcohol use in adolescence might lead to alcohol abuse/dependence in adulthood.[4,5] A prior study on substance use among adolescents in a southwestern province in China in 2001 estimated that the prevalence of alcohol drinking was 1.6%,[6] and a study in Finland reported that alcohol-attributable mortality increased over the period 1998 to 2007.[7] According to the monitoring the future (MTF) reports in 2011, drinking is one of the leading causes of morbidity and mortality during adolescence as well as later in life.[8] Moreover, a global study in 2010 reported that mental and substance use disorders accounted for 183.9 million disability-adjusted life years globally.[9]
Social inequalities are one of the most important determinants of health and health-related behaviors.[10] Previous reports from the health behavior in school-aged children (HBSC) study in Europe have demonstrated that social inequalities in age, gender, and socioeconomic status dimensions were related to alcohol use and alcohol-related problems.[11,12] Moreover, prior studies also showed that young people living in low socioeconomic status households were less likely to have adequate access to health resources and more likely to be exposed to psychosocial problems.[13] In addition, many studies have found that alcohol drinking and alcohol-related problems were associated with mental disorders among adolescents. A previous study in Europe demonstrated that depression was associated with alcohol problems among European American students.[14] A recent meta-analysis found a significant association between alcohol use disorder and both suicidal ideation and suicide attempt.[15] Regarding the role of gender in the relationship between alcohol use and mental disorder, a previous study in the United States found that the association between alcohol abuse and mental illness was stronger among females than males.[16]
As discussed in a previous study, an individual's alcohol use and his problems with alcohol begin and develop in a cultural context, and social values can encourage or discourage young people's alcohol use.[17] Notably, China is a large country with a traditional alcohol culture, and it is a country that differs dramatically from Western countries in its approach to social, political, and economic policies. It is necessary to determine the sheer number of adolescents in China who use alcohol and whether alcohol-related problems and their correlates occur among Chinese adolescents in similar ways as they manifest among Western adolescents. With the rapid economic development, sociocultural changes, and globalization, Chinese adolescents are becoming more easily exposed to alcohol use and alcohol-related problems. Therefore, we conducted this large-scale cross-sectional study to investigate the prevalence of alcohol use and alcohol-related problems among Chinese adolescents and to explore risk factors and connections in order to help develop prevention and intervention programs to reduce adolescent alcohol use in China.
2. Methods
2.1. Study design and participants
We performed a large-scale cross-sectional study and used a multistage, stratified cluster, random sampling method to obtain a representative sample of junior and senior high school students in China. In stage 1, we selected 7 large provinces to represent different regional features of southern China, divided each province into 3 economic stratifications by per capita gross domestic product (high-, middle-, and low-level), and then selected 2 representative cities (or primary sampling units) from each stratification by simple randomization using SAS 9.2 software (SAS Institute, Inc., Cary, NC, USA). In stage 2, schools (or secondary sampling units) in each representative city were divided into 3 categories based on the education quality: key junior/senior high schools, regular junior/senior high schools, and vocational high schools. Two key junior high schools, 2 key senior high schools, 2 regular junior high schools, 2 regular senior high schools, and 2 vocational high schools were randomly selected from each representative city. In stage 3, 2 classes (or the minimum sampling units) were randomly selected from each grade within the selected schools. All available students within the grade were surveyed; those not surveyed were absent or refused to participate and consisted of less than 1% of the student population. All the participants were fully informed of the purpose of the survey and were invited to participate voluntarily. A rigorous, anonymous method to collect the self-reported questionnaires was guaranteed. The questionnaires were administered by research assistants in the classrooms without the presence of teachers. It is important to stress that the questions formulated about substance use were based on an instrument proposed by the World Health Organization (WHO) and were adapted to the realities of China. Although self-reported data on alcohol use has always been subject to underreporting, the findings of a number of investigations indicate that such data can be extremely useful.[1,2]
2.2. Ethical statement
The study received approval from the Sun Yat-Sen University, School of Public Health Institutional Review Board. After the procedure had been fully explained, written informed consents were obtained from each participating student who was at least 18 years of age. If the student was under 18 years of age, written informed consent was obtained from one of the student's parents (or legal guardian). The methods were carried out in accordance with the approved guidelines.
2.3. Measures
2.3.1. Dependent variables
Current drinking is defined as any drinking, and binge drinking as consuming at least 5 drinks on 1 occasion, both in the past 30 days.[18]
Alcohol-related problems were measured by asking the students 1 question, “How often did you have the following problems over the last 12 months due to your drinking, that is, had trouble with parents, had problems at school, had problems with friends, and got into a physical fight?” Responses included “never”, “once”, “twice”, “3 to 4 times”, or “5 or more times”. Data on all 5 responses were later recorded into a dichotomous variable, alcohol-related problem (0 = no and 1 = yes).[19]
2.4. Independent variables
Demographic variables included age, gender (1 = male and 2 = female), grade (1 = grade 7, 2 = grade 8, 3 = grade 9, 4 = grade 10, 5 = grade 11, and 6 = grade 12), and the number of siblings (1 = none, 2 = 1–2 siblings, and 3 = more than 2 siblings).
School-level variables: Classmate relations and teacher–classmate relations were assessed based on the student's self-rating about their relationships with classmates and teachers, ranging from poor to good. Academic achievement was captured by a single item that asked for a personal appraisal of their performance or pressure relative to that of their classmates (responses were coded as “above average” = 1, “average” = 2, and “below average” = 3).
Family-level variables: Living arrangements were assessed by asking who lived in the student's primary home (responses were coded as “living with 2 biological parents” = 1, “living only with father or mother” = 2, and “living with others” = 3), and social economic status (SES) was measured by asking the student's perception of their family's current economic status (rated from below average to above average).
Psychosocial-level variables: Suicidal ideation was defined as responding “one time or more” to the question “During the past 12 months, how many times did you seriously consider attempting suicide?” Depressive symptoms were measured by the 20-item version of the Center for Epidemiology Scale for Depression (CES-D). This version of CES-D is a valid instrument for both junior high and senior high school students in China.[20] Higher scores indicate more severe depressive symptomatology, with a maximum score of 60.[21]
2.5. Statistical analysis
All data were entered by 2 investigators independently using EpiData 3.1 (The EpiData Association, Odense, Denmark, Europe), and statistical analyses were conducted using IBM SPSS 21.0 (IBM, Armonk, NY) and SAS 9.2 (SAS Institute, Inc., Cary, NC). Descriptive analyses were used to describe demographic characteristics and the prevalence of current drinking and alcohol-related problems among the sampled adolescents. Considering that our study used a multistage sampling, students were grouped into schools, and therefore might not be independent, we performed 2-level analyses in which schools were treated as clusters by the PROC GLIMMIX procedure used to compute the generalized linear mixed models for alcohol drinking and alcohol-related problems among adolescents in SAS. All covariates that were statistically significant in the univariate analysis and that had been widely reported in the literature were further analyzed by multivariate analysis. Adjusted odds ratios (AORs) were obtained with 95% confidence intervals (95% CIs). All statistical tests were 2-sided in which a P value of less than 0.05 was considered significant.
3. Results
3.1. Demographic characteristics of the total sample
As shown in Table 1, of the 105,752 students whose questionnaires were completed and qualified for our survey, 48,906 (46.2%) were boys and 56,846 (53.8%) were girls, yielding a male-to-female ratio of 1:1.2. The students ranged in age from 9 to 21 years, and the mean age was 16.0 (±2.0) years. Overall, 75.3% (79,623) of the participants lived with 2 biological parents, 20.9% (22,138) reported that their SES was above average, and 31.1% (32,887) had no siblings. A total of 3.5% (3709) students admitted having poor classmate relations, and 6.4% (6754) reported having poor relationships with teachers. The proportion of students with suicidal ideation was 17.1% (18,095), and the median CES-D score among adolescents was 14.0 (interquartile range: 10). Notably, the prevalence of current drinking among students was 7.3%, and 13.2% (14,010) of students reported having alcohol-related problems.
Table 1.
Demographic characteristics of the total sample (n = 105,752).

3.2. Unadjusted ORs (95% CIs) for current drinking and alcohol-related problems by multi-level univariate logistic regression models
Table 2 shows that without adjusting for other variables, male students, higher grade level, and older age were positively correlated with alcohol drinking and alcohol-related problems (P < 0.05). Students living with others, classmate relations, relationships with teachers, and academic achievements were also associated with alcohol drinking and alcohol-related problems (P < 0.05). In addition, those with suicidal ideation and who were depressed were also more likely to be involved in alcohol drinking and alcohol-related problems (P < 0.05).
Table 2.
Unadjusted odds ratios (95% confidence intervals) for current drinking and alcohol-related problems by multilevel univariate logistic regression models.
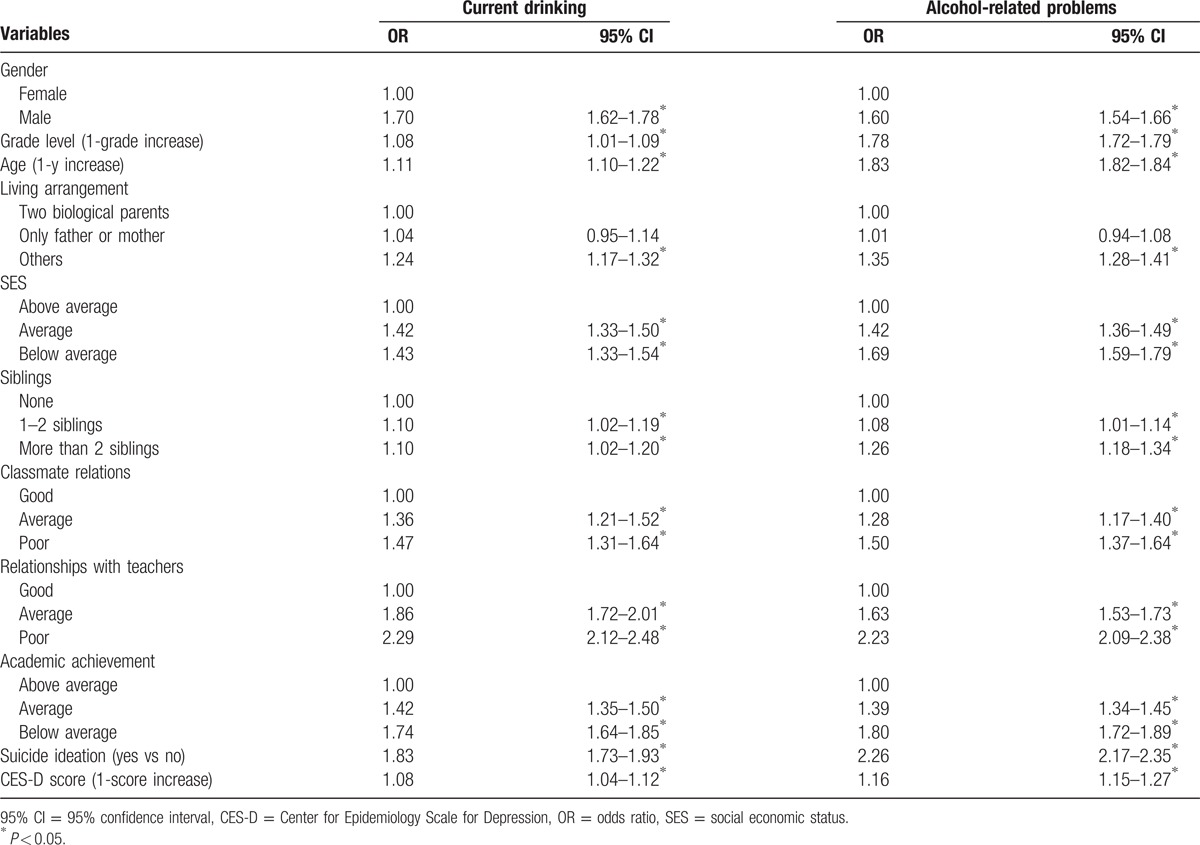
3.3. AORs (95% CIs) for current drinking and alcohol-related problems by multilevel multivariate logistic regression models
Table 3 illustrates the final factors associated with alcohol drinking. Male students were 1.78 (95% CI = 1.69–1.87) times more likely to be involved in current drinking. Higher grade level students (AOR = 1.09, 95% CI = 1.05–1.13) and older students (AOR = 1.06, 95% CI = 1.04–1.17) were at a higher risk of current drinking. Average SES (AOR = 1.18, 95% CI = 1.11–1.26), having poor classmate relations (AOR = 1.28, 95% CI = 1.03–1.37), having poor relationships with teachers (AOR = 1.08, 95% CI = 1.00–1.16), and below average academic achievement (AOR = 1.50, 95% CI = 1.41–1.59) were positively associated with current drinking. Students with suicidal ideation (AOR = 1.70, 95% CI = 1.61–1.81) and those who were depressed (AOR = 1.09, 95% CI = 1.05–1.11) were at a higher risk of current drinking than their corresponding groups.
Table 3.
Adjusted odds ratios (95% confidence intervals) for current drinking and alcohol-related problems by multilevel multivariate logistic regression models.

In addition, the final logistic regression model for alcohol-related problems is also presented in Table 3. Male students had a higher risk of having alcohol-related problems (AOR = 1.86, 95% CI = 1.79–1.93). Higher grade students (AOR = 1.43, 95% CI = 1.42–1.58) and older students (AOR = 1.83, 95% CI = 1.82–1.85) were more likely to report having alcohol-related problems. Notably, those with more than 2 siblings were at a higher risk than those without siblings (AOR = 1.14, 95% CI = 1.07–1.22). Average SES (AOR = 1.08, 95% CI = 1.03–1.14), average relationships with teachers (AOR = 1.37, 95% CI = 1.28–1.48), and poor relationships with teachers (AOR = 1.68, 95% CI = 1.56–1.82) were positively associated with alcohol-related problems. Students who had below average academic achievement were more likely to have alcohol-related problems (AOR = 1.51, 95% CI = 1.44–1.59). Students with suicidal ideation (AOR = 2.08, 95% CI = 1.98–2.16) and those who had higher CES-D scores (AOR = 1.08, 95% CI = 1.06–1.18) were at a higher risk of having alcohol-related problems.
4. Discussion
In this current study, the results demonstrated that alcohol use was prevalent among Chinese adolescents; in fact, the prevalence of current drinking was 7.3%. This result was consistent with that from the MTF reports in 2009, which demonstrated that alcohol was the most widely used substance by today's teenagers and that 3.9% drank daily[8]; the results were lower than was described in a recent study of the 2013 Minnesota Student Survey suggesting that approximately 13% of 9th and 11th graders had engaged in alcohol use.[22] A possible explanation for the variation in the prevalence could be differences in the nature of the samples, the definition of alcohol use, the development of economic level, or the different national policy. In this study, we also found that 13.2% students had alcohol-related problems. Similarly, previous studies have demonstrated that alcohol drinking effects the physical and mental health of people with intellectual disabilities, leading to many alcohol-related problems (i.e., behavioral and social problems).[23,24] It seems likely that young people are less concerned about the dangers of using alcohol, which is likely because they are widely used for experience or release. However, previous studies have demonstrated that compared with adults, adolescents seemed to be more sensitive to the neurotoxic effects of alcohol use, such as greater predisposition to memory impairment and judgment impairment, and that alcohol use in adolescence might lead to abuse, impulsiveness, and dependence in adulthood.[4] These findings suggest that the Chinese government should strengthen regulations to limit the sale of alcohol to adolescents or to delay alcohol use until adulthood.
Previous studies have demonstrated that younger people's health or health-related behaviors are particularly affected by social inequalities and that social inequalities include not only SES but also age, gender, ethnicity, and living arrangements.[11,13] Consistent with previous studies, our final logistic regression models found significant differences in alcohol use and alcohol-related problems between the genders; male students had a higher level of alcohol use and alcohol-related problems than female students. These findings agree with a similar report conducted as part of the Youth Risk Behavior Surveillance Studies in the United States that showed that gender differences were significant for current alcohol use and that boys may be more likely to use alcohol repeatedly[25]; they were also consistent with a previous study in Taiwan that reported that the rate of alcohol use among boys was considerably higher than that among girls.[26] This gender difference is most likely related to the fact that, unlike girls, boys are more likely to engage in certain risky behaviors and dangerous activities, such as alcohol use.
Prior studies have shown that income inequality has powerful psychosocial and behavioral effects.[13,27] Similarly, our study demonstrated that students in average SES were at a higher risk of alcohol drinking and alcohol-related problems compared with those of above average SES. These results might be related to the fact that a lower SES is stressful because it reduces people's control over their lives and work; thus, people in a lower socioeconomic status might use alcohol to cope with stress.[28] However, in this study, our results did not find significant associations between below average SES and both alcohol drinking and alcohol-related problems, which might be related to the fact that students in very low SES may have less access (such as pocket money per month) to alcohol. In addition, one of the most significant findings was that having more than 2 siblings had effects on adolescents’ alcohol-related problems in our study. The effect of having siblings is complex, and we cannot completely disentangle the direction of this effect for our study based on different cultural, psychosocial, and genetic populations. In addition, adolescence is a period of transition when young people face the developmental task of differentiating themselves from parents and family and forging independent identities. In this light, having harmonious family relationships and well behaved siblings may protect an adolescent from substance use.[29] Furthermore, we found that alcohol use and alcohol-related problems were significantly related to the respondents’ appraisal of poor academic achievement, poor classmate relations, and poor relationships with teachers; these results were in line with previous reports showing that school achievement emerges as an important recurring correlate of substance use behavior.[30] One striking difference between Chinese and American adolescents is the salience of school and academic achievements relative to other concerns.[31] In addition, frequent substance use is negatively associated with school-related factors.[32] In this study, we found that students who had poor relationships with teachers were more likely to engage in alcohol use and to have alcohol-related problems. This finding is consistent with previous studies that have suggested that engagement and positive teacher–pupil relationships are strongly, negatively associated with all substance use categories.[33] A number of studies reported that poor mental health was significantly more common among drinkers than among their nondrinking classmates.[34–36] Alcohol may be a risk factor for suicide for several reasons and can exacerbate the intensity and duration of depression[37]; a recent report showed that depressive symptoms in adolescence result in substance use impairment.[38] Consistent with this notion, our study demonstrated that students with suicidal ideation and who had higher CES-D scores were at a higher risk of current drinking and of experiencing alcohol-related problems.
Based on these results that enhanced our understanding of the risk factors for alcohol use and alcohol-related problems among adolescents, we suggest that effective prevention and intervention programs should be established and the role of the government and social settings should be considered. First, the WHO definition of health promotion is the process of enabling people to increase control over, and to improve, their health.[39] The WHO also proposed that health promotions focusing on achieving equality in health and the role of the government were crucial for public health.[40,41] The US government has established several national systems (e.g., MTF, National Survey on Drug Use and Health), and the European Union has also conducted the HBSC to oversee and control such health-risk behaviors among adolescents. With the global development of health policies,[10] a proper surveillance system is suggested to be developed by the Chinese government to monitor and control the alcohol use among adolescents in the long term, and the national government should try to provide equal health services to adolescents to promote resilience among adolescents involved in current drinking or with alcohol-related problems. In addition, the goals of health promotion should be incorporated to the health system in all countries to prevent an increase of alcohol abuse. Second, as social environment is a well known risk factor for poor health, the WHO has put forward the Healthy Cities project.[10,41–44] This project promotes a comprehensive and systematic policy and plan for health. Motivated by this project, we suggest that policy-makers aiming to reduce Chinese adolescent alcohol use should consider the involvement of local government, community, family, and school. Local government has significant power to implement the national government's policies; therefore, encouraging local government to engage in the process of reducing adolescent alcohol use plays a significant role. The creation of healthier communities is rooted in health promotion, which can make people—as members of the community—more involved in the activities to reduce adolescent alcohol use. Peers or neighbors may either serve as role models, influence personal attitudes toward alcohol use or provide access to, encourage, and provide a social setting for alcohol use.[45] A healthy community can decrease the adverse influence of peers or neighbors. As previous studies have mentioned, the health communities approach promises to be one of the key strategies to achieve human health development in the 21st century.[43] Regarding the role of family and school, the traditional Chinese culture style of parenting and schooling treats students in a strict manner and always requires them to not drink alcohol or have alcohol-related problems. Along these lines, parents and schools should focus on alcohol use among adolescents, particularly among those who struggle in family- or school-related relationships. Moreover, as the change of traditional Chinese culture is a result of global financial and political developments, and this change might have an influence on consumption of alcohol in adolescents and students in China, we should also take the change of traditional Chinese culture into consideration when promoting suitable political policies to prevent adolescent alcohol abuse. Third, closer attention should be paid to students who have depressive symptoms, are involved in alcohol use, or have alcohol-related problems. Psychological services should be established and provided to those students, and educational campaigns that are directed toward students are needed to improve awareness of the serious consequences of alcohol use; moreover, regular health education should be offered to every student.
There are some limitations in this study that should be considered. First, this is a cross-sectional study, so no casual inference can be made regarding the observed associations. Second, considering that we used a structured self-report questionnaire to collect data, we could not completely rule out the possibility of recall bias. Third, the study sample only included school students and did not include individuals who had dropped out of school or were not present in school on the day of survey administration; students involved in current drinking, who had alcohol-related problems, and had depressive symptoms may be more common among those adolescents who were absent.
Despite these limitations, the noteworthy strength of this study is that the data were collected from a large-scale sample of Chinese high school students, and the relatively high response rate ensured that our findings might be generalized to this population. Furthermore, we used multilevel logistic regression models to examine these associations.
In summary, Chinese adolescent alcohol use is a major public health problem nationally, and alcohol-related problems among Chinese adolescents are also prevalent; an adolescent's family, school, and psychosocial factors influence their alcohol use habits. Although our world is full of inequalities that lead to different health performance, the government, schools, and families should strive to prevent students’ involvement with alcohol use and development of alcohol-related problems. Our study recommends strengthening regulations to limit the sale of alcohol to adolescents, establishing a surveillance system to monitor and control the adolescent alcohol use, and providing health services to promote resilience among adolescents involved in current drinking or who have alcohol-related problems.
Acknowledgments
We specifically thank all of the participants in our study.
Footnotes
Abbreviations: CES-D = Center for Epidemiology Scale for Depression, CI = confidence interval, HBSC = health behavior in school-aged children, MTF = monitoring the future, SES = social economic status, WHO = World Health Organization.
LG and JD contributed equally to the article.
Author contributions: CL and W-HZ designed the study. JD and YH managed the literature searches and summaries of previous related work. XD, JH, GH, and XG carried out the field research. LG and JD undertook the statistical analysis and wrote the first draft of the manuscript. All authors reviewed the manuscript.
Funding/support: This study was funded by the Centre for ADR monitoring of Guangdong grant number: GZSW11175FT4055.
The authors have no conflicts of interest to disclose.
References
- 1.Crockett LJ, Beal SJ. The life course in the making: gender and the development of adolescents’ expected timing of adult role transitions. Dev Psychol 2012; 48:1727–1738. [DOI] [PubMed] [Google Scholar]
- 2.Li S, Huang H, Xu G, et al. Substance use, risky sexual behaviors, and their associations in a Chinese sample of senior high school students. BMC Public Health 2013; 13:295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Newcomb MD, Bentler PM. Substance use and abuse among children and teenagers. Am Psychol 1989; 44:242–248. [DOI] [PubMed] [Google Scholar]
- 4.Camarini R, Pautassi R. Alcohol Abuse in Adolescents: Relevance of Animal Models and Experimental Results in Adolescent Animals. Drug Abuse in Adolescence. 2016; Cham Heidelberg New York Dordrecht London: Springer, 101–112. [Google Scholar]
- 5.Noal RB, Menezes AM, Araujo CL, et al. Experimental use of alcohol in early adolescence: the 11-year follow-up of the 1993 Pelotas (Brazil) birth cohort study. Cad Saude Publica 2010; 26:1937–1944. [DOI] [PubMed] [Google Scholar]
- 6.Liu Z, Zhou W, Lian Z, et al. The use of psychoactive substances among adolescent students in an area in the south-west of China. Addiction 2001; 96:247–250. [DOI] [PubMed] [Google Scholar]
- 7.Martikainen P, Makela P, Peltonen R, et al. Income differences in life expectancy: the changing contribution of harmful consumption of alcohol and smoking. Epidemiology 2014; 25:182–190. [DOI] [PubMed] [Google Scholar]
- 8.Johnston LD, Malley PMO, Bachman JG, et al. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2011. Bethesda, Maryland: Institute for Social Research, The University of Michigan; 2012. [Google Scholar]
- 9.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 2013; 382:1575–1586. [DOI] [PubMed] [Google Scholar]
- 10.Leischik R, Dworrak B, Strauss M, et al. Plasticity of health. Ger J Med 2016; 1:1–17. [Google Scholar]
- 11.Inchley J, Currie D, Young T, et al. Growing Up Unequal: Gender and Socioeconomic Differences in Young People's Health and Well-being. Health Behaviour in School-aged Children (HBSC) Study: International Report from the 2013/2014 Survey. Copenhagan: WHO; 2016. [Google Scholar]
- 12.Verdurmen J, Monshouwer K, van Dorsselaer S, et al. Alcohol use and mental health in adolescents: interactions with age and gender-findings from the Dutch 2001 Health Behaviour in School-Aged Children survey. J Stud Alcohol 2005; 66:605–609. [DOI] [PubMed] [Google Scholar]
- 13.Wilkinson RG, Pickett KE. Income inequality and population health: a review and explanation of the evidence. Soc Sci Med 2006; 62:1768–1784. [DOI] [PubMed] [Google Scholar]
- 14.Dennhardt AA, Murphy JG. Associations between depression, distress tolerance, delay discounting, and alcohol-related problems in European American and African American college students. Psychol Addict Behav 2011; 25:595–604. [DOI] [PubMed] [Google Scholar]
- 15.Darvishi N, Farhadi M, Haghtalab T, et al. Alcohol-related risk of suicidal ideation, suicide attempt, and completed suicide: a meta-analysis. PLoS One 2015; 10:e126870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lo CC, Monge AN, Howell RJ, et al. The role of mental illness in alcohol abuse and prescription drug misuse: gender-specific analysis of college students. J Psychoactive Drugs 2013; 45:39–47. [DOI] [PubMed] [Google Scholar]
- 17.Ozgur II, Yildirim F, Demirbas H, et al. Alcohol use prevalence and sociodemographic correlates of alcohol use in a university student sample in Turkey. Soc Psychiatry Psychiatr Epidemiol 2008; 43:575–583. [DOI] [PubMed] [Google Scholar]
- 18.Huang R, Ho SY, Wang MP, et al. Sociodemographic risk factors of alcohol drinking in Hong Kong adolescents. J Epidemiol Community Health 2016; 70:374–379. [DOI] [PubMed] [Google Scholar]
- 19.Wong MM, Brower KJ. The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. J Psychiatr Res 2012; 46:953–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang L, Jia CX, Qin P. Reliability and validity of the Center for Epidemiologic Studies Depression Scale (CES-D) among suicide attempters and comparison residents in rural China. BMC Psychiatry 2015; 15:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Radloff, Sawyer L. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977; 1:385–401. [Google Scholar]
- 22.Chatterjee D, McMorris B, Gower A, et al. Experience of abuse, household dysfunction, and early use of alcohol and marijuana among Minnesota youth: the moderating role of internal assets. J Adolesc Health 2016; 58:S12–S13. [Google Scholar]
- 23.Carballo JJ, Oquendo MA, Giner L, et al. Alcohol-related problems in adolescents and young adults admitted to psychiatric emergency rooms. Nord J Psychiatry 2007; 61:310–311. [DOI] [PubMed] [Google Scholar]
- 24.Sellman JD, Connor JL, Joyce PR. How to reduce alcohol-related problems in adolescents: what can parents do and what can the government do? Aust N Z J Psychiatry 2010; 44:771–773. [DOI] [PubMed] [Google Scholar]
- 25.Frieden TR, Jaffe HW, Stephens JW, et al. Youth Risk Behavior Surveillance-United States, 2011. Atlanta: Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 26.Yang MS, Yang MJ, Liu YH, et al. Prevalence and related risk factors of licit and illicit substances use by adolescent students in southern Taiwan. Public Health 1998; 112:347–352. [DOI] [PubMed] [Google Scholar]
- 27.Wilkinson R. Why is violence more common where inequality is greater? Ann N Y Acad Sci 2004; 1036:1–12. [DOI] [PubMed] [Google Scholar]
- 28.O’Hara RE, Armeli S, Tennen H. Alcohol and cannabis use among college students: substitutes or complements? Addict Behav 2016; 58:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trinidad DR, Chou CP, Unger JB, et al. Family harmony as a protective factor against adolescent tobacco and alcohol use in Wuhan, China. Subst Use Misuse 2003; 38:1159–1171. [DOI] [PubMed] [Google Scholar]
- 30.Resnick MD, Bearman PS, Blum RW, et al. Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA 1997; 278:823–832. [DOI] [PubMed] [Google Scholar]
- 31.Gong J, Li Y, Xg C, et al. [A baseline survey on the association of smoking onset and life events on adolescents in Wuhan, China]. Zhonghua Liu Xing Bing Xue Za Zhi 2004; 25:142–145. [PubMed] [Google Scholar]
- 32.Hotton T, Haans D. Alcohol and drug use in early adolescence. Health Rep 2004; 15:9–19. [PubMed] [Google Scholar]
- 33.Markham WA, Young R, Sweeting H, et al. Does school ethos explain the relationship between value-added education and teenage substance use? A cohort study. Soc Sci Med 2012; 75:69–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA 1990; 264:2511–2518. [PubMed] [Google Scholar]
- 35.Merikangas KR, Mehta RL, Molnar BE, et al. Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addict Behav 1998; 23:893–907. [DOI] [PubMed] [Google Scholar]
- 36.Zeitlin H. Psychiatric comorbidity with substance misuse in children and teenagers. Drug Alcohol Depend 1999; 55:225–234. [DOI] [PubMed] [Google Scholar]
- 37.Kandel DB, Raveis VH, Davies M. Suicidal ideation in adolescence: depression, substance use, and other risk factors. J Youth Adolesc 1991; 20:289–309. [DOI] [PubMed] [Google Scholar]
- 38.McCarty CA, Wymbs BT, Mason WA, et al. Early adolescent growth in depression and conduct problem symptoms as predictors of later substance use impairment. J Abnorm Child Psychol 2013; 41:1041–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization. Ottawa Charter for Health Promotion, 1986. Ottawa: World Health Organization; 1986. [Google Scholar]
- 40.Vilhjalmsson R. Public views on the role of government in funding and delivering health services. Scand J Public Health 2016; 44:446–454. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization. Global Strategy on Diet, Physical Activity and Health. Geneva: World Health Organization; 2004. [Google Scholar]
- 42.Moore M, Gould P, Keary BS. Global urbanization and impact on health. Int J Hyg Environ Health 2003; 206:269–278. [DOI] [PubMed] [Google Scholar]
- 43.Hancock T. Healthy cities and communities: past, present, and future. Natl Civic Rev 1997; 86:11–21. [Google Scholar]
- 44.World Health Organization. Healthy Cities. Geneva: World Health Organization; 2016. [Google Scholar]
- 45.Kokkevi AE, Arapaki AA, Richardson C, et al. Further investigation of psychological and environmental correlates of substance use in adolescence in six European countries. Drug Alcohol Depend 2007; 88:308–312. [DOI] [PubMed] [Google Scholar]


