Abstract
Background
Fractional exhaled nitric oxide (FeNO) is an easy, sensitive, reproducible, and noninvasive marker of eosinophilic airway inflammation. Accordingly, FeNO is extensively used to diagnose and manage asthma. Patients with COPD who share some of the features of asthma have a condition called asthma–COPD overlap syndrome (ACOS). The feasibility of using FeNO to differentiate ACOS patients from asthma and COPD patients remains unclear.
Methods
From February 2013 to May 2016, patients suspected with asthma and COPD through physician’s opinion were subjected to FeNO measurement, pulmonary function test (PFT), and bronchial hyperresponsiveness or bronchodilator test. Patients were divided into asthma alone group, COPD alone group, and ACOS group according to a clinical history, PFT values, and bronchial hyperresponsiveness or bronchodilator test. Receiver operating characteristic (ROC) curves were obtained to elucidate the clinical functions of FeNO in diagnosing ACOS. The optimal operating point was also determined.
Results
A total of 689 patients were enrolled in this study: 500 had asthma, 132 had COPD, and 57 had ACOS. The FeNO value in patients with ACOS was 27 (21.5) parts per billion (ppb; median [interquartile range]), which was significantly higher than that in the COPD group (18 [11] ppb). The area under the ROC curve was estimated to be 0.783 for FeNO. Results also revealed an optimal cutoff value of >22.5 ppb FeNO for differentiating ACOS from COPD patients (sensitivity 70%, specificity 75%).
Conclusion
FeNO measurement is an easy, noninvasive, and sensitive method for differentiating ACOS from COPD. This technique is a new perspective for the management of COPD patients.
Keywords: fractional exhaled nitric oxide, chronic obstructive pulmonary disease, asthma, ACOS, cutoff point
Introduction
Asthma and COPD are common diseases of airways and lungs and share some common clinical characteristics. Asthma, a chronic disorder of the airways, is associated with two main characteristics: airway hyperresponsiveness (AHR) and airway inflammation. The airflow limitation is reversible.1 Meanwhile, COPD is a disease characterized by persistent, progressive airflow limitation and is also an inflammatory disease.2 Fractional exhaled nitric oxide (FeNO) is an easy, sensitive, reproducible, and noninvasive marker for directly detecting eosinophilic airway inflammation.3 Given that airway inflammation can be assessed through FeNO measurement, the American Thoracic Society clinical practice guideline recommends the use of FeNO to diagnose and monitor asthma.4 Some patients with COPD have the features of asthma; FeNO values are elevated in this specific category of patients with COPD, and this condition is called asthma–COPD overlap syndrome (ACOS).5 ACOS was proposed by the science committees of both Global Initiative for Asthma (GINA) and Global Initiative for Chronic Obstructive Lung Disease (GOLD) in 2015.6 However, the exact role of FeNO in patients with ACOS remains to be defined. In the present study, we performed a retrospective study that aimed to evaluate the diagnostic performance of FeNO, which may be able to indicate airway eosinophilic inflammation in patients with COPD and to differentiate ACOS from COPD.
Patients and methods
Patient population
Patients suspected to have COPD and asthma visiting the First Affiliated Hospital of Sun Yet-Sen University from February 2013 to May 2016 were retrospectively enrolled in this study. Inclusion criteria were physician-diagnosed asthma and COPD. All patients underwent pulmonary function test (PFT) and FeNO test. Subjects were excluded if they had other chronic obstructive lung diseases, including but not limited to bronchiectasis, cystic fibrosis, obliterative bronchiolitis, and reactive airway dysfunction syndrome. Subjects were also excluded if they were current smokers, had a respiratory tract infection within 6 weeks, or used any oral corticosteroid in the previous 4 weeks.
The Institutional Review Board of the First Affiliated Hospital of Sun Yat-sen University approved the study protocol and waived the need for written informed consent from patients due to no intervention trial and the retrospective nature of the study.
Methods
Patients were divided into three study groups: asthma alone, COPD alone, and ACOS.
COPD patients were diagnosed according to the GOLD criterion, ie, bronchodilator forced expiratory volume in 1 second to forced vital capacity ratio (FEV1/FVC) of <0.70.7 COPD severity was also classified according to the PFT values and GOLD guidelines.7 The included COPD patients were in a stable phase.
Asthma patients were diagnosed according to a clinical history of wheezing, cough, or shortness of breath, as well as the presence of either bronchial hyperresponsiveness or positive broncodilator test (>12% and >200 mL), based on the GINA guidelines.8
There are currently no internationally accepted criteria for the diagnosis of ACOS. Thus, in this study, we defined ACOS patients as having a diagnosis of COPD, positive bronchodilator test with >12% and 200 mL gain in FEV1, and presence of clinical characteristics of asthma (previous history of asthma/wheezing).
Medical information, patient characteristics, and data (including height, weight, body surface area, smoking status, pack years of tobacco use, FeNO values, PFT values, and current medication information) were obtained from the patients’ medical charts.
Measurements
PFT
PFT was performed using a pneumotachograph-based system in accordance with the recommendations of the European Respiratory Society.9 Percentage predicted values (% pred) were calculated based on previously determined reference values for healthy Chinese adults. All subjects were asked to undergo PFT in a reproducible way, and the best values were retained.
Bronchial hyperresponsiveness test
PFT values were assessed prior to histamine challenge. Airway responsiveness is expressed as the provocative concentration of histamine required to induce a 20% decrease in FEV1 (PC20), and for this study, the positive response was defined as PC20 ≤8 mg/mL.
Bronchodilator reversibility test
After baseline evaluation, PFT was repeated 15 minutes after two inhalations of a salbutamol metered dose inhaler through a spacer device. Three forced expiratory maneuvers were obtained, and postbronchodilator FEV1 (% pred) was recorded. The positive response was defined as improvement in FEV1 >200 mL and >12% after salbutamol inhalation.
Measurement of FeNO
FeNO level was measured according to the American Thoracic Society/European Respiratory Society recommendations using an NO analyzer (NIOX MINO Analyzer; Aerocrine AB, Solna, Sweden). Patients were instructed to inhale NO-free air to total lung capacity and immediately exhale fully into the device at a flow rate of 50 mL/s for 10 seconds.10
Statistical analysis
All analyses were performed by using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). Results are expressed as mean ± standard deviation (SD) for quantitative variables, or median (interquartile range) for non-normal variables when appropriate, or number (%) of patients. Continuous variables were compared using the Student’s t-test for those that were normally distributed and the Kruskal–Wallis tests for those that were not. The chi-squared test was used to compare categorical variables. Comparison between tests was performed by constructing receiver operating characteristic (ROC) curve and measuring the area under the curve (AUC). The optimal cutoff value was determined, and sensitivity and specificity were also calculated. Statistical significance was defined as P<0.05.
Results
Characteristics of study subjects
A total of 689 patients were enrolled in this study. According to the diagnostic criterion, they were divided into asthma alone (72.57 %), ACOS (8.27 %), and COPD alone (19.16 %). Most asthma patients had normal PFT values. Patients with asthma showed higher PFT values and FeNO levels than the other two groups (P<0.001). The characteristics of the patients analyzed in this study are listed in Table 1.
Table 1.
Baseline characteristics of the study population
| Parameter | Asthma (N=500) |
COPD (N=132) |
ACOS (N=57) |
|---|---|---|---|
| Mean age, years | 41.92±15.23 | 63.52±9.58 | 63.17±9.17 |
| Sex (M:F), n | 215:285 | 109:23 | 37:20 |
| Height (cm) | 162.41±7.35 | 165.20±6.98 | 163.26±7.70 |
| Weight (kg) | 59.40±10.06 | 60.18±9.58 | 59.05±8.96 |
| Body surface area (m2) | 1.63±0.15 | 1.65±0.15 | 1.63±0.14 |
| FVC (% predicted) | 96.99±15.59 | 75.80±17.73 | 77.42±17.56 |
| FEV1 (% predicted) | 88.49±19.38 | 50.81±19.30 | 51.01±18.64 |
| FEV1/FVC (%) | 76.89±11.37 | 51.44±12.37 | 51.88±11.70 |
| PEF (% predicted) | 78.16±21.07 | 43.88±17.06 | 46.95±17.27 |
| MEF (% predicted) | 75.87±31.33 | 26.58±17.46 | 26.88±17.72 |
| MEF25 (% predicted) | 73.47±38.75 | 21.29±15.41 | 26.04±22.25 |
| MEF50 (% predicted) | 70.73±30.61 | 24.36±18.10 | 24.91±17.28 |
| MEF75 (% predicted) | 75.71±27.94 | 27.89±17.13 | 29.35±21.76 |
| MVV (% predicted) | 86.76±21.72 | 53.93±22.88 | 51.30±21.27 |
| VC (% predicted) | 91.15±14.82 | 71.77±18.25 | 73.16±15.36 |
| FeNO (ppb), median (interquartile range) | 41.0 (45.0) | 18 (11) | 27 (21.5) |
| Smoking history, n (%) | 129 (25.80) | 98 (74.24) | 23 (40.35) |
Notes: Measured pulmonary function values are presented as a percentage of predictive. Data shown as mean ± standard deviation unless indicated otherwise.
Abbreviations: M, male; F, female; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; PEF, peak expiratory flow; MEF, maximal midexpiratory flow; MEF25, forced expiratory flow after 25% of the FVC; MEF50, forced expiratory flow after 50% of the FVC; MEF75, forced expiratory flow after 75% of the FVC; MVV, maximal voluntary ventilation; VC, vital capacity; FeNO, fractional exhaled nitric oxide; ppb, parts per billion; ACOS, asthma–COPD overlap syndrome.
Comparison of FeNO levels among the three groups
There was a significant difference in FeNO levels among the three groups (P<0.001). The FeNO value in patients with ACOS was 27 (21.5) parts per billion (ppb; median [interquartile range]), which was significantly higher than that of the COPD group (18 [11] ppb; P<0.001). The FeNO value in patients with asthma was 41.0 (45.0) ppb, which was significantly higher than that of the other groups (P<0.001; Figure 1)
Figure 1.
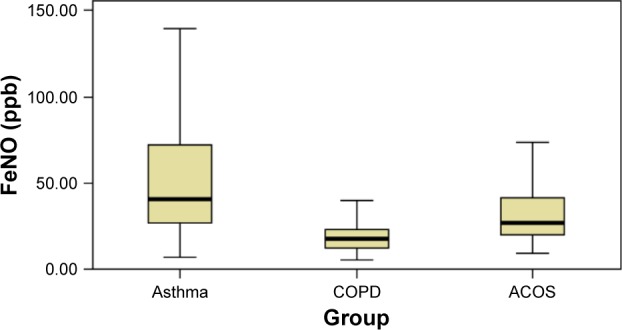
Comparison of FeNO values among the three groups.
Abbreviations: FeNO, fractional exhaled nitric oxide; ppb, parts per billion; ACOS, asthma–COPD overlap syndrome.
Figure 2 shows the FeNO values of patients with COPD according to the GOLD severity stage. Differences were observed across the groups in terms of PFT, but no differences existed in FeNO levels among the groups. A total of eight patients (6.06%) corresponded to stage I (23.0 [4.5] ppb), 55 (41.67%) to stage II (14.0 [10.0] ppb), 46 (34.85%) to stage III (18.0 [7.25] ppb), and 23 (17.42%) to stage IV (19.0 [11.0] ppb).
Figure 2.
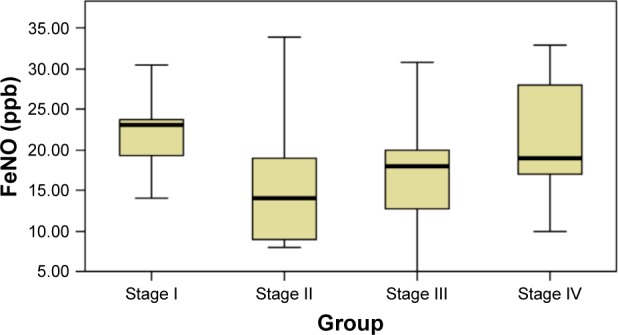
FeNO values by GOLD stage of COPD severity.
Abbreviations: FeNO, fractional exhaled nitric oxide; ppb, parts per billion; GOLD, Global Initiative for Chronic Obstructive Lung Disease.
In the ACOS group, FeNO values were categorized by low (<25 ppb), intermediate (25–50 ppb), and high (>50 ppb) values, as summarized in Table 2. The number of cases with low FeNO values were 25 (43.85%), with intermediate values were 20 (35.09%), and with high values were 12 (21.05%). No differences in PFT values were observed between the groups. The characteristics of patients with ACOS analyzed in this study are listed in Table 2.
Table 2.
Comparison of characteristics and PFT values among the groups having low, intermediate, and high FeNO levels
| Parameter | FeNO >50 ppb (N=12) |
25≤ FeNO ≤50 ppb (N=20) |
FeNO <25 ppb (N=25) |
|---|---|---|---|
| Mean age, years | 63.25±9.17 | 60.40±9.91 | 65.28±8.30 |
| Sex (M:F), n | 7:5 | 12:8 | 18:7 |
| Height (cm) | 161.17±6.04 | 163.70±5.82 | 163.92±9.58 |
| Weight (kg) | 57.75±7.47 | 58.50±8.01 | 60.12±10.41 |
| Body surface area (m2) | 1.60±0.11 | 1.63±0.11 | 1.65±0.17 |
| FVC (% predicted) | 72.75±19.33 | 77.65±15.82 | 79.48±18.28 |
| FEV1 (% predicted) | 51.67±19.46 | 50.25±16.97 | 51.32±20.20 |
| FEV1/FVC (%) | 56.67±12.77 | 51.00±9.56 | 50.28±12.55 |
| PEF (% predicted) | 45.75±16.00 | 48.30±22.29 | 46.44±18.79 |
| MEF (% predicted) | 28.42±18.72 | 28.95±19.33 | 24.48±16.28 |
| MEF25 (% predicted) | 28.00±22.62 | 29.08±27.64 | 22.08±16.91 |
| MEF50 (% predicted) | 24.42±17.88 | 24.45±16.93 | 25.52±19.11 |
| MEF75 (% predicted) | 34.00±30.84 | 29.05±17.44 | 27.36±20.32 |
| MVV (% predicted) | 57.00±23.89 | 52.45±21.77 | 47.64±19.68 |
| VC (% predicted) | 72.42±14.49 | 70.85±14.99 | 75.36±16.32 |
| Smoking history, n (%) | 5 (41.67) | 6 (30.00) | 12 (48.00) |
Notes: Measured pulmonary function values are presented as a percentage of predictive. Data shown as mean ± standard deviation unless indicated otherwise.
Abbreviations: M, male; F, female; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; PEF, peak expiratory flow; MEF, maximal midexpiratory flow; MEF25, forced expiratory flow after 25% of the FVC; MEF50, forced expiratory flow after 50% of the FVC; MEF75, forced expiratory flow after 75% of the FVC; MVV, maximal voluntary ventilation; VC, vital capacity; FeNO, fractional exhaled nitric oxide; ppb, parts per billion; ACOS, asthma–COPD overlap syndrome; PFT, pulmonary function test.
Optimal FeNO level to define ACOS
The constructed ROC curve (Figure 3) defines the optimal cutoff value for FeNO level and was used to differentiate ACOS from COPD. The ROC AUC was estimated to be 0.783 for FeNO. The optimal diagnostic cutoff point was 22.5 ppb (with 70% sensitivity and 75% specificity). Table 3 shows the sensitivity and specificity values for different criteria tested.
Figure 3.
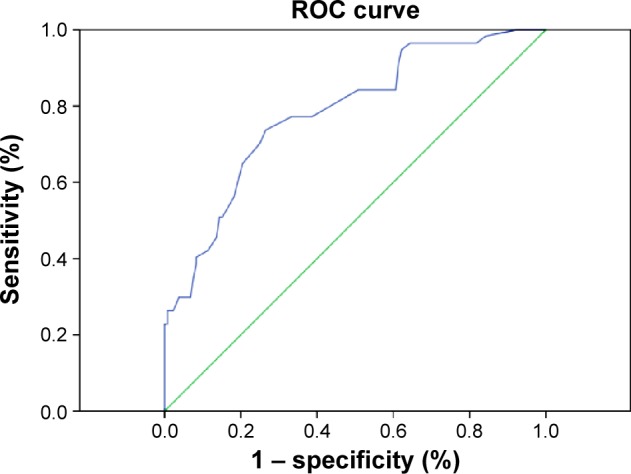
ROC curve analysis of the sensitivity and specificity of FeNO for ACOS diagnosis.
Abbreviations: ROC, receiver operating characteristic; FeNO, fractional exhaled nitric oxide; ACOS, asthma–COPD overlap syndrome.
Table 3.
Sensitivity and specificity of different cutoff points used to diagnose ACOS
| Threshold | Sensitivity | Specificity | |
|---|---|---|---|
| FeNO value | >18.5 ppb | 77.2 | 61.4 |
| FeNO value | >19.5 ppb | 77.2 | 66.7 |
| FeNO value | >20.5 ppb | 73.7 | 73.5 |
| FeNO value | >21.5 ppb | 71.9 | 74.2 |
| FeNO value | >22.5 ppb | 70.2 | 75.0 |
| FeNO value | >23.5 ppb | 64.9 | 79.5 |
| FeNO value | >24.5 ppb | 56.1 | 81.8 |
Abbreviations: ACOS, asthma–COPD overlap syndrome; FeNO, fractional exhaled nitric oxide; ppb, parts per billion.
Discussion
We performed a retrospective study to define and use FeNO value to differentiate ACOS from asthma and COPD. Results showed that the measurement of FeNO was useful in the diagnosis of ACOS, with an optimal cutoff value of 22.5 ppb.
Airway inflammation is considered to be a key element in asthma. In recent years, FeNO has been used as a surrogate marker of eosinophilic inflammation and is a useful tool for the diagnosis and monitoring of asthma. Studies have shown that FeNO is elevated in asthmatic patients and is correlated with airway inflammation.11–13 In the present study, FeNO was significantly higher in the asthma group than in the other two groups (P<0.001).
COPD is also an inflammatory disease, but the FeNO value does not differ significantly between patients with COPD and healthy volunteers because neutrophilic inflammation is predominant.14 FeNO values are increased only in a subgroup of patients with COPD, these COPD patients share some common features with asthma.15 This condition is called ACOS, whose definition basically depends on the patient’s symptoms or the physician’s opinion. Many studies have shown that ACOS patients have higher rates of exacerbation, rapid decline in pulmonary function, and poor quality of life compared with those having COPD or asthma alone.16–18 These data indicate the importance of finding a biomarker that differentiates ACOS from asthma and COPD as early as possible. A number of preliminary studies have measured FeNO in COPD, but literature defining the role of FeNO in patients with ACOS is minimal. In the present study, we found that the FeNO values were substantially higher in COPD patients with ACOS than in those with COPD alone (P<0.01). These results confirmed a new perspective concerning the potential role of FeNO as a biomarker.
Our results showed that 57 patients had a diagnosis of both asthma and COPD, and the prevalence of ACOS was ~30.16% in patients with COPD. This finding was consistent with the number reported by other investigators who suggested that ACOS exists in 15%–45% of COPD patients.17,19,20 We compared the features of patients with ACOS, COPD, and asthma. Patients with asthma were younger than those in the other groups. The PFT values for patients with asthma were better than those in the other groups. PFT values did not significantly differ between the COPD and the ACOS groups (P>0.05). It was easy to differentiate ACOS from asthma because of the clinical characteristics and PFT values, but it was difficult to differentiate ACOS from COPD through PFT values.
Moreover, the mean age of patients with COPD was 63.52±9.58 years (mean ± standard deviation), and the percentages of patients with GOLD stages I, II, III, and IV were 6.06%, 41.67%, 34.85%, and 17.42%, respectively. We also observed that FeNO values were not linearly associated with GOLD classification, similar to that described by other researchers.14,21
FeNO is a good predictor for differentiating ACOS from COPD, with an ROC AUC of 0.783. Taking 22.5 ppb as a cutoff point to diagnose ACOS, FeNO measurement indicated a sensitivity of 70% and a specificity of 75%, which agreed with previous studies. Donohue et al14 showed an FeNO level of 20 ppb in COPD patients with a previous diagnosis of asthma. Some authors have observed that patients with a cutoff point of 35 ppb can be classified as ACOS, whether or not they have allergic rhinitis.15 Corticosteroids are known to increase the risk for pneumonia and other diseases in COPD patients,14,22 but ACOS patients positively respond to treatment with inhaled corticosteroids. Given that FeNO could differentiate ACOS from COPD, FeNO could offer additional advantages for the management of COPD patients.
This is a retrospective study and several limitations exist. First, the diagnosis was confirmed by PFT, which may have yielded false-positive and -negative results. Second, FeNO is a biomarker whose values are influenced by many factors, such as atopy. We made the best attempt to exclude subjects with other diseases that may influence the FeNO levels. We further excluded current smokers, but not ex-smokers, whose NO production may have been affected. Although the conclusions about the relevance of FeNO levels and smoking history in different COPD studies are contradictory. Wagener et al23 reported that smoking history does not affect FeNO, while Kharitonov et al24 reported that current smokers have lower levels of exhaled NO. We do not think the conclusion would be biased by the exclusion of current smokers, but we should admit that the optimal cutoff point and the sensitivity and specificity of FeNO may be different if we had enrolled current smokers. Finally, although we have tried vigorously to standardize the method of FeNO testing, we should be cautious in extrapolating absolute values obtained in this center to those obtained in other centers.
Conclusion
We found that FeNO measurement is an alternative diagnostic tool to conventional lung function tests for diagnosing asthma. The majority of patients with COPD do not exhibit high FeNO levels, but a high FeNO level of a COPD patient may predict that this patient has ACOS. FeNO measurement is a simple, reproducible, and noninvasive method of differentiating ACOS from COPD, which may have implications in the management of patients with COPD. However, we need additional large-scale prospective studies to expand the clinical application of FeNO measurement.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343–373. doi: 10.1183/09031936.00202013. [DOI] [PubMed] [Google Scholar]
- 2.Vestbo J, Anderson W, Coxson HO, et al. Evaluation of COPD longitudinally to identify predictive surrogate end-points (ECLIPSE) Eur Respir J. 2008;31:869–873. doi: 10.1183/09031936.00111707. [DOI] [PubMed] [Google Scholar]
- 3.Alving K, Malinovschi A. Basic aspects of exhaled nitric oxide. In: Horvath I, de Jongste JC, editors. Exhaled Biomarkers European Respiratory Society Monographs. Sheffield: European Respiratory Society; 2010. pp. 1–31. [Google Scholar]
- 4.Dweik RA, Boggs PB, Erzurum SC, et al. An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am J Respir Crit Care Med. 2011;184(5):602–615. doi: 10.1164/rccm.9120-11ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drazen JM, Postma DS, Rabe KF. The asthma–COPD overlap syndrome. N Engl J Med. 2015;373(13):1241–1249. doi: 10.1056/NEJMra1411863. [DOI] [PubMed] [Google Scholar]
- 6.Global Initiative for Asthma [webpage on the Internet] Diagnosis of Diseases of Chronic Airflow Limitation: Asthma COPD and Asthma-COPD Overlap Syndrome (ACOS) [Accessed May 7, 2015]. Available from: http://www.ginasthma.org/local/uploads/files/ACOS_2015.pdf [updated 2015]
- 7.The Global Strategy for the Diagnosis, Management and Prevention of COPD [webpage on the Internet] Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2013. [Accessed April 22, 2014]. Available from: http://www.goldcopd.org/
- 8.Global Initiative for Asthma Global strategy for asthma management and prevention [revised 2010] [Accessed March 16, 2012]. Available from: www.ginasthma.org.
- 9.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 10.American Thoracic Society, European Respiratory Society ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005. Am J Respir Crit Care Med. 2005;171(8):912–930. doi: 10.1164/rccm.200406-710ST. [DOI] [PubMed] [Google Scholar]
- 11.Al-Ali MK, Eames C, Howarth PH. Exhaled nitric oxide: relationship to clinicophysiological markers of asthma severity. Respir Med. 1998;92:908–913. doi: 10.1016/s0954-6111(98)90189-5. [DOI] [PubMed] [Google Scholar]
- 12.Jatakanon A, Lim S, Kharitonov SA, Chung KF, Barnes PJ. Correlation between exhaled nitric oxide,sputim eosinophils,and methacholine responsiveness in patients with mild asthma. Thorax. 1998;53:91–95. doi: 10.1136/thx.53.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lim S, Jatakanon A, Meah S, Oates T, Chung KF, Barnes P. Relationship between exhaled nitric oxide and mucosal eosinophilc inflammation in mild to moderately severe asthma. Thorax. 2000;55:184–188. doi: 10.1136/thorax.55.3.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Donohue JF, Herje N, Crater G, Rickard K. Characterization of airway inflammation in patients with COPD using fractional exhaled nitric oxide levels: a pilot study. Int J Chronic Obstructive Pulm Dis. 2014;9:745–751. doi: 10.2147/COPD.S44552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tamada T, Sugiura H, Takahashi T, et al. Biomarker-based detection of asthma-COPD overlap syndrome in COPD populations. Int J Chronic Obstructive Pulm Dis. 2015;10:2169–2176. doi: 10.2147/COPD.S88274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kauppi P, Kupiainen H, Lindqvist A, et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma. 2011;48:279–285. doi: 10.3109/02770903.2011.555576. [DOI] [PubMed] [Google Scholar]
- 17.Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax. 2009;64:728–735. doi: 10.1136/thx.2008.108027. [DOI] [PubMed] [Google Scholar]
- 18.Andersén H, Lampela P, Nevanlinna A, Sänääangas O, Keistinen T. High hospital burden in overlap syndrome of asthma and COPD. Clin Respir J. 2013;7:342–346. doi: 10.1111/crj.12013. [DOI] [PubMed] [Google Scholar]
- 19.Soriano JB, Davis KJ, Coleman B, Visick G, Mannino D, Pride NB. The proportional Venn diagram of obstructive lung disease: two approximations from the United States and the United Kingdom. Chest. 2003;124(2):474–481. doi: 10.1378/chest.124.2.474. [DOI] [PubMed] [Google Scholar]
- 20.Beeh KM, Kornmann O, Beier J, Ksoll M, Buhl R. Clinical application of a simple questionnaire for the differentiation of asthma and chronic obstructive pulmonary disease. Respir Med. 2004;98(7):591–597. doi: 10.1016/j.rmed.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 21.Alcázar-Navarrete B, Romero-Palacios PJ, Ruiz-Sancho A, Ruiz-Rodriguez O. Diagnostic performance of the measurement of nitric oxide in exhaled air in the diagnosis of COPD phenotypes. Nitric Oxide. 2016;54:67–72. doi: 10.1016/j.niox.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 22.Karampitsakos T, Gourgoulianis KI. Asthma-COPD Overlap Syndrome (ACOS): single disease entity or not? Could exhaled nitric oxide be a useful biomarker for the differentiation of ACOS, asthma and COPD? Med Hypotheses. 2016;91:20–23. doi: 10.1016/j.mehy.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 23.Wagener AH, De Nijs SB, Lutter R, et al. External validation of blood eosinophils, FENO and serum periostin as surrogates for sputum eosinophils in asthma. Thorax. 2015;70:115–120. doi: 10.1136/thoraxjnl-2014-205634. [DOI] [PubMed] [Google Scholar]
- 24.Kharitonov SA, Robbins RA, Yates D, Keatings V, Barnes PJ. Acute and chronic effects of cigarette smoking on exhaled nitric oxide. Am J Respir Crit Care Med. 1995;152(2):609–612. doi: 10.1164/ajrccm.152.2.7543345. [DOI] [PubMed] [Google Scholar]


