Abstract
Anthracycline extravasation is a feared complication of intravenous (i.v.) chemotherapy due to the tissue toxicity of this group of drugs. We describe a 54-year-old woman with history of stage IIIa breast cancer, receiving adjuvant chemotherapy consisting of doxorubicin and cyclophosphamide. The chemotherapy was administered through a Poweport® device, the position of which was confirmed with fluoroscopy and function confirmed by flushing the line. Urgent intervention was required as patient was symptomatic and experienced severe right-sided pleuritic chest pain. Radiology also confirmed the extravasation of doxorubicin into the pleural space. Surgical washout of the pleural space and 3 days therapy with i.v. dexrazoxane were carried out to prevent tissue damage and long-term sequelae. Use of dexrazoxane should always be considered following intra-pleural extravasation because of its potential efficacy and reasonable tolerability. However, the best approach to extravasation injury is prevention by systematic implementation of careful, standardized, evidence-based administration techniques.
INTRODUCTION
Anthracycline extravasation is a feared complication of intravenous (i.v.) chemotherapy due to the tissue toxicity of this group of drugs. The reported incidence of the chemotherapy extravasation in the literature varies from 0.01% to 6% [1, 2]. However extravasation into thorax is rare, so far only 10 cases have been reported [1, 3]. A retrospective single centre study showed that improvement in staff training reduced the incidence of this complication by a factor of 10 (0.1–0.001%) over 15 years.
Vesicant injuries can progress within hours or days, resulting in lasting tissue injury and necrosis. Management is considered an emergency requiring combination of medical and surgical care.
Management of dermal extravasation is well established often requiring reconstructive surgical repair and use of DMSO which is a topical agent [2]. The effects of these agents into pleural or lung tissue are not well defined and there are no standard approaches in the management of accidental intra-pleural extravasation.
Our case report describes a 54-year-old female who presented with intra-pleural extravasation of doxorubicin from a malpositioned central venous catheter. Management consisted of urgent surgical intervention and dexrazoxane, which proved to be effective in the long run.
CASE REPORT
A 54-year-old woman (Mrs XY) was transferred from another facility for management of iatrogenic infusion of doxorubicin into the pleural space through a migrated central venous catheter.
Her only medical history was stage IIIA left breast cancer oestrogen receptor, progesterone receptor and human epidermal growth factor receptor 2 positive. Mrs XY underwent bilateral mastectomy and left axillary lymph node clearance with three out of seven lymph nodes positive.
Adjuvant chemotherapy was recommended following review of histopathology. Prior to the first cycle of chemotherapy, long-term central venous access was established using a Poweport® device. This was inserted through the right subclavian vein using Seldinger technique and no complications were noted at time of procedure. The line position was confirmed with fluoroscopy and function confirmed by flushing the line (see Fig. 1).
Figure 1:
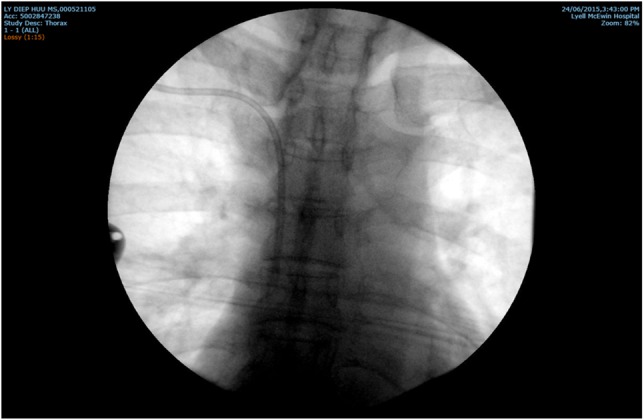
Position of the line confirmed with fluoroscopy and function confirmed by flushing the line
Routine chest X-ray following procedure demonstrated correct catheter position with no complications.
The first cycle of chemotherapy consisting of 85 mg of i.v. doxorubicin (60 mg/m2) in 50 ml of normal saline and 850 mg of cyclophosphamide (600 mg/m2) was given 5 days post-insertion of the port. Prior to the administration of the cytotoxic agents, it was noted that there was no withdrawal of blood from the port on aspiration. Doxorubicin infusion was commenced by nurses as they were able to infuse a flush solution without resistance. Following 6 ml (10 mg) of infused doxorubicin, Mrs XY complained of severe right-sided pleuritic chest pain. Fluoroscopy contrast study demonstrated that central venous catheter had curled unusually, causing perforation of superior vena cava or the azygos vein and migrated into the pleural space (see Fig. 2).
Figure 2:

Fluoroscopy contrast study showing contrast medium flowed over the surface of the lung in the pleural cavity. The Port-A-Cath tubing tip is now in the pleural cavity.
Mrs XY was transferred to our institution for urgent surgical washout of the pleural space and i.v. dexrazoxane. She received i.v. dexrazoxane within 6 hours of extravasation. A dose of 1000 mg/m2 was used, administered immediately before the operation followed by 500 mg/m2 daily for 2 days post-operatively.
A right thoracoscopic-assisted pleural lavage was performed the same day. The tip of the central catheter was visually identified lodged in the pleural space but there was no frank pneumonitis or direct parenchymal injury to the lung. The catheter was not broken and sutures were found to be intact. It is unclear as to the circumstances that led to the catheter migration to this unusual position.
Three chest drains (2 × 28Fr Mallinckrodt® catheters through port sites and 1 × 12Fr Arrow® catheter into the axilla) were left in-situ for the purpose of administering 24 hours of ongoing saline infusion (see Fig. 3).
Figure 3:

Chest drain inserted for continuous irrigation post-procedure
Post-operatively Mrs XY recovered well. Drains were sequentially removed by post-operative day 5. Pain was a significant issue in this patient and our Acute Pain Service treated this with fentanyl patient-controlled anaesthesia and a ketamine infusion. She was discharged from hospital on the sixth post-operative day.
At cardio-thoracic review 3 weeks post-operatively, she was found to have a small right pleural effusion, which was treated conservatively and there were no other complications (see Fig. 4).
Figure 4:
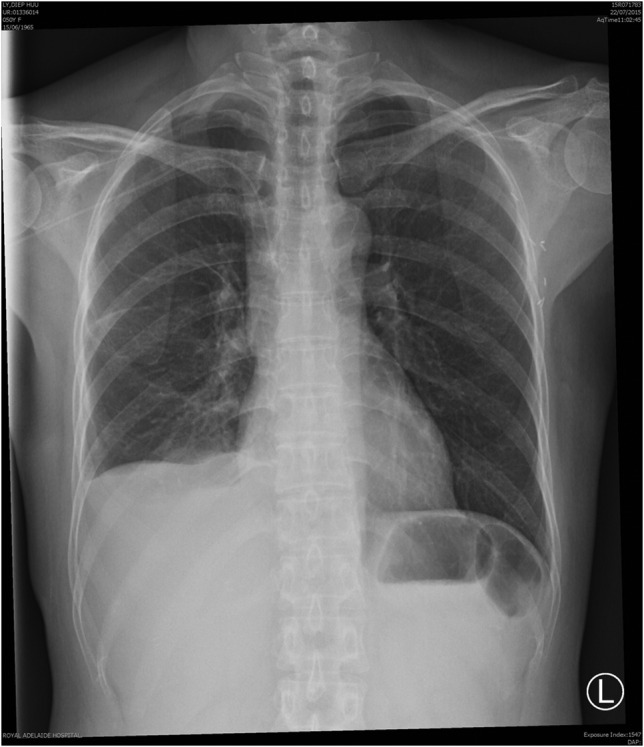
Chest X-ray just showing small right pleural effusion without any other abnormalities. Taken at 1 month after the incident.
She completed her adjuvant chemotherapy through a PICC line in 2015. Regular outpatient follow-up assured that Mrs XY is doing well and a repeat chest X-ray, taken 10 months after extravasation, only revealed small pleural effusion (see Fig. 5).
Figure 5:
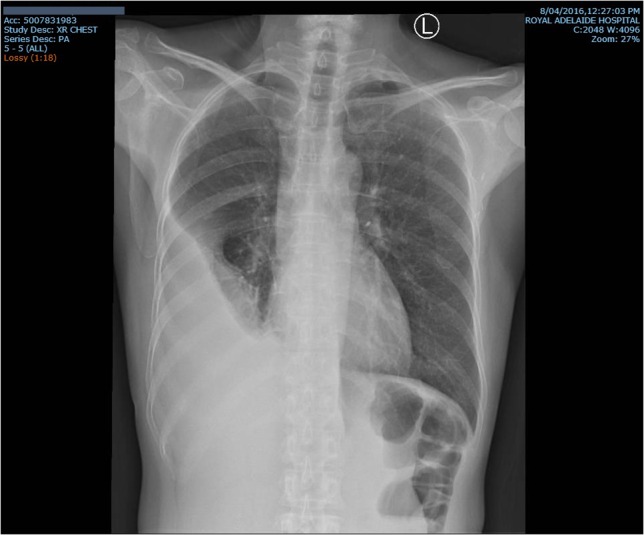
Repeat chest X-ray taken 10 months after extravasation again showing right pleural effusion without any other abnormalities
DISCUSSION
The anthracyclines (daunorubicin, idarubicin, epirubicin and doxorubicin) are widely utilized in the treatment of solid tumours and haematological malignancies.
Anthracycline extravasation is a highly feared local complication of i.v. administration. Compared with other types of injectable anti-tumour drugs, anthracyclines have the potential to cause the most damage or complications because of their mechanism of action on tissue when they extravasate. Anthracyclines bind to the nucleic acids in the DNA of healthy tissues when they leak out of a vein. This process causes cell death and continues to do so as more drug is released into the surrounding tissue. These injuries can become larger, deeper and more painful as the cycle repeats itself [2].
Central venous catheters are frequently used for infusion of vesicant drugs as they provide reliable venous access, high-flow rates and rapid drug dilution. Unfortunately, they may also involve complications, including drug extravasation.
Implementation of proper guidelines regarding use of venous catheters for chemotherapy can minimize or prevent complications. Location of the catheter tip should be in high-flow vessels to prevent cytostatic accumulation, which may lead to catheter thrombosis and vessel wall perforation [1]. Prior to anthracycline administration, it is critical to ensure port or peripheral catheter patency and position radiographically. Furthermore, it is necessary to reconfirm the positioning of the catheter when it is not possible to draw blood or infuse a flush solution prior to start of the chemotherapy infusion [4]. In this case, by means of brief aspiration of blood before giving anthracycline, followed by flushing of sodium chloride or glucose solution may have resulted in the detection of the catheter displacement.
Indications of extravasation include symptoms of pain or fever. Lab investigations most frequently reveal leucocytosis. Radiology, most preferably CT scan, should be used for diagnosis of extravasation [1, 3, 4].
Immediate discontinuation of the infusion and aspiration of as much solution as possible through the central venous catheter must be done in all cases of extravasation [3]. Identification of local extravasation and surgical intervention wherever feasible to remove as much of the agent as possible [3] and at the same time administering dexrazoxane must be instituted to prevent major complications [4].
Before the approval of dexrazoxane for anthracycline extravasation, topical DMSO, ice application and/or use of steroids were recommended as a plausible approach. In the review of intrathoracic extravasation of chemotherapeutic agents from implanted ports by Bozkurt et al., anthracycline extravasation was reported in two cases and one case was in combination with five fluorouracil. Most of the patients developed pleural effusion like our Mrs. XY or pericardial effusion. Management consisted of aspiration of the residual drug as much as possible before removing the catheter, flushing of the cavities with normal saline and/or systemic administration of steroids. Surprisingly, all of them had a favourable outcome [3].
In 2007, the U.S. Food and Drug Administration (FDA) approved dexrazoxane for injection for the treatment of extravasation resulting from i.v. anthracycline chemotherapy [5]. Dexrazoxane acts as a reversible topoisomerase II inhibitor and ring chelating agent, thereby reducing the formation of anthracycline–iron complexes, which are toxic to surrounding tissue [2, 4].
In Europe, two prospective clinical studies of the efficacy of dexrazoxane (TT01 and TT02) in preventing the potentially devastating effects of biopsy-proven anthracycline extravasation in the skin demonstrated that dexrazoxane treatment is highly effective both on a short and long-term basis. Epirubicin was involved in 56% of the cases, 41% were treated with doxorubicin while two received daunorubicin. Four out of 57 had extravasation involving central venous access device and none of them required surgical intervention. The 3 day treatment schedule with dexrazoxane consisting of a daily dose of 1000 mg/m2 on days 1–2 and 500 mg/m2 on day 3 proved effective in preventing surgery-requiring necrosis. Haematological toxicities and transient elevation of liver enzymes associated with dexrazoxane were manageable [2, 6].
Since FDA approval of dexrazoxane, subsequent clinical case reports have supported the above-mentioned study findings, and the systemic antidotal treatment has shown value in anthracycline extravasation. Promising results were obtained from a 2007 to 2010 Belgian survey involving 41 patients treated with dexrazoxane from 29 centres. It showed that surgical debridement due to anthracycline extravasation could be avoided in 95.1% of cases (39/41 extravasations) with use of dexrazoxane with manageable toxicities reported in only 8/41 cases [2].
A similar survey in UK was published consisting of 12 cases in which dexrazoxane was administered. These cases did not require surgery and 92% of them continued the chemotherapy as scheduled [2].
There was another identifiable case report by Uges et al. [4] regarding the evolution and management of intra-pleural extravasation through a CVAD using dexrazoxane resulting in a favourable long-term outcome with similar strategy.
In conclusion, prevention is the best approach for managing chemotherapy extravasation. Prior to using venous catheters, their position and function should be adequately checked, with adherence to surgical and oncological procedures. Anthracyclines should be administered as a short infusion only in the presence of healthcare professionals with oncology training.
A prospective clinical trial involving the use of dexrazoxane in intra-pleural extravasation is unlikely. Therefore, the use of dexrazoxane in intrathoracic extravasation depends on reports of individual cases and its access, keeping in mind the financial toxicities.
Use of dexrazoxane due to its potential benefits and relatively mild side effects along with urgent thoracic intervention should always be considered following intra-pleural extravasation [4].
ACKNOWLEDGEMENTS
1. Cardiothoracic team of Royal Adelaide Hospital; 2. Patient, Mrs XY for giving consent; 3. Dr Nick Murray, for helping me write this case report.
CONFLICT OF INTEREST STATEMENT
I, Rachael Chang, solemnly and truthfully declare that the contents of this paper are solely my own work and I have no financial or any other interest in any of the drugs and their manufacturers mentioned in this paper, any associated companies or organizations. I further declare that in the writing of this paper I have no known conflict of interest.
FUNDING
This is a case report and no funding was required.
ETHICAL CONSIDERATIONS
This paper is a case report and does not require any ethical considerations. The patient's confidentiality has been maintained and her permission was sought prior to writing this report. Publication of this paper will not result in harm to the patient.
CONSENT
Patient permission was sought prior to writing this report.
GUARANTOR
I, Rachael Chang, will be the guarantor of this case report.
REFERENCES
- 1.Quintanar Verdúguez T, Blanco Jarava A, Martínez-Barbeito MB, Pangua Méndez C, López Gómez L, Andrade Santiago J, et al. . Mediastinal extravasation of doxorubicin. Clin Transl Oncol 2008;10:128–30. DOI:10.1007/s12094-008-0167-z. [DOI] [PubMed] [Google Scholar]
- 2.Conde-Estévez D, Mateu-de Antonio J. Treatment of anthracycline extravasations using dexrazoxane. Clin Transl Oncol 2014;16:11–7. DOI:10.1007/s12094-013-1100-7. [DOI] [PubMed] [Google Scholar]
- 3.Bozkurt AK, Uzel B, Akman C, Ozgüroğlu M, Molinas Mandel N. Intrathoracic extravasation of antineoplastic agents: case report and systematic review. Am J Clin Oncol 2003;26:121–3. [DOI] [PubMed] [Google Scholar]
- 4.Uges JW, Vollaard AM, Wilms EB, Brouwer RE. Intrapleural extravasation of epirubicin, 5-fluouracil, and cyclophosphamide, treated with dexrazoxane. Int J Clin Oncol 2006;11:467–70. Epub 2006 Dec 25. DOI:10.1007/s10147-006-0598-x. [DOI] [PubMed] [Google Scholar]
- 5.Kane Robert C. David McGuinn W. Jr, Dagher Ramzi, Justice Robert, Pazdur Richard . 2008, Dexrazoxane (Totect™): FDA review and approval for the treatment of accidental extravasation following intravenous anthracycline chemotherapy. The Oncologist 13, 445–50. DOI:10.1634/theoncologist.2007-0247 [DOI] [PubMed] [Google Scholar]
- 6.Mouridsen1 H. T., Langer S. W., Buter J., Eidtmann H., Rosti G, de Wit M, et al. . Treatment of anthracycline extravasation with Savene (dexrazoxane): results from two prospective clinical multicentre studies. Ann Oncol 2007;18:546–50. DOI:10.1093/annonc/mdl413. [DOI] [PubMed] [Google Scholar]


