Introduction
Amyloidosis is a group of conditions that involve the deposition of amyloid proteins in various tissues. It is generally classified as either systemic or cutaneous. Primary localized cutaneous nodular amyloidosis (PLCNA) is the rarest form of cutaneous amyloidosis with the amyloid depositing in the dermis, subcutis, and blood vessel walls.
Management of PLCNA is challenging, as there is no consistently effective treatment, and local recurrence is common. Management options include surgical excision, dermabrasion, electrodessication and curettage, cryotherapy, carbon dioxide laser, pulse dye laser, intralesional steroids, and cyclophosphamide. We report a case of PLCNA in which intralesional methotrexate has been used with good effect.
Case report
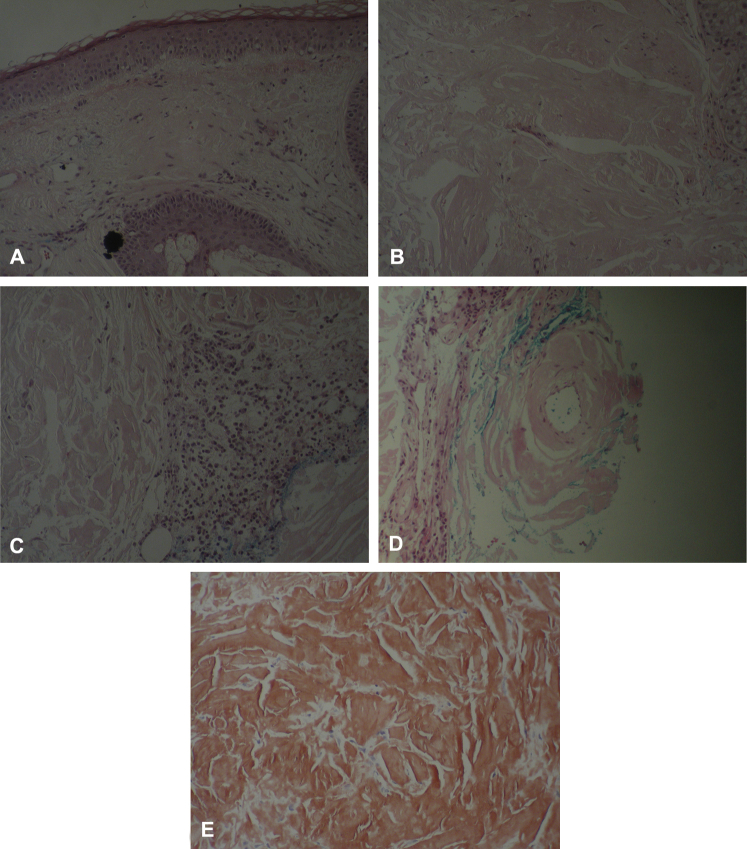
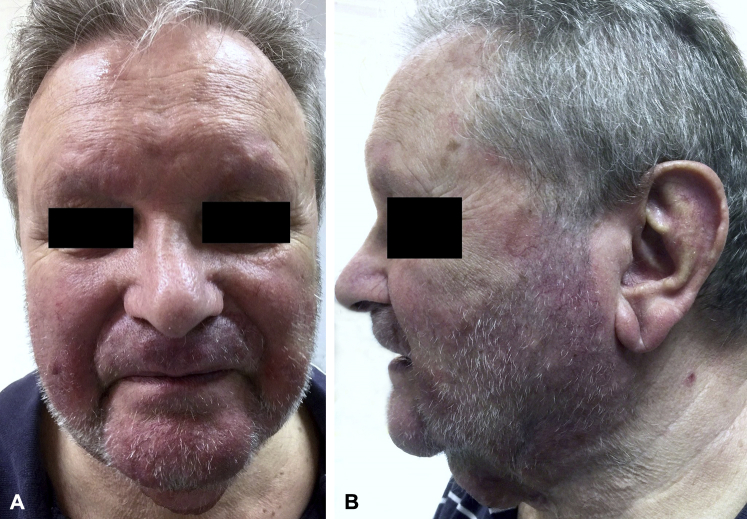
A 77-year-old man was referred to a dermatologist for management of large firm nodules and plaques on his lower face and neck. The lesions had been present for approximately 2 months before dermatology review. No treatments were trialled before dermatology referral (Fig 1). A biopsy of a lesion on the patient's chin found nodular deposits of eosinophilic hyalinized globular material for the whole thickness of the dermis, patchy plasmacytic chronic inflammatory infiltrate in adjacent stroma, and normal epidermis. Stains with Periodic acid–Schiff crystal violet and Congo red were strongly positive, and polarized light of Congo red–stained sections showed characteristic yellow-green birefringence. Histologic findings were classic for PLCNA (Fig 2). Similar lesions were present on the patient's neck but were not biopsied. Routine blood test results showed abnormal blood protein levels, and subsequent serum electrophoresis confirmed monoclonal gammopathy of unknown significance. The potential for secondary systemic amyloidosis was then investigated with serum and urine protein electrophoresis, echocardiogram and bone marrow biopsy. In the absence of investigation findings for secondary systemic amyloidosis, the condition was classified as primary cutaneous amyloidosis in conjunction with histopathology findings.
Fig 1.

PLCNA pretreatment with intralesional methotrexate.
Fig 2.
A-E, Histology findings.
Initially, the patient was given betamethasone dipropionate 0.1% twice daily for the nodules on the face and neck. After 4 weeks of topical corticosteroid treatment, there was no improvement in the patient's condition. Two intralesional corticosteroid injections (triamcinolone, 40 mg/mL) were administered to the nodular lesions over a 2-month period without any improvement in conjunction with topical betamethasone dipropionate 0.1% twice daily on a second weekly basis. Intralesional methotrexate injections were then started for lesions on cheeks, upper lip, and chin. Initially, only 2 nodules on the cheeks were treated, but eventually all nodules on both cheeks, upper lip, and chin region were injected. Excision or pulse dye laser therapy is being considered for lesions on the neck, as they are less conspicuous.
The initial dose of methotrexate was 12.5 mg, which was titrated up to 25 mg then 40 mg then 50 mg. The period between treatments ranged between 2 and 4 weeks in the early stages to determine whether the patient would tolerate methotrexate. Upon ascertaining tolerance, 50-mg injections were administered on a weekly basis over a 6-month period without folic acid. This regimen resulted in a significant reduction in size of the treated lesions, and they remain stable (Fig 3). However, untreated nodules have recently started growing, and new lesions are developing in untreated areas on the back of the patient's neck and eyebrows. Weekly to fortnightly monitoring of full blood count, electrolytes, urea & creatinine, and liver function tests (LFTs) found some minor LFT abnormalities resulting in cessation of injections.
Fig 3.
A and B, PLCNA posttreatment with intralesional methotrexate.
Discussion
Treatment of PLCNA is challenging, and various modalities are used in its management. A 585-nm pulsed dye laser has been used with few complications, but multiple treatments are required to achieve the desired clinical effect.1 Intralesional corticosteroids are ineffective and may actually accelerate amyloid deposition.2 Dermabrasion is effective in nodular amyloidosis,3 but the limitation is that the amyloid is often deposited more deeply in the skin with PLCNA. Carbon dioxide laser has been used with good cosmetic results, but residual amyloid may persist, and there are concerns about tissue friability along with achieving hemostasis.4 Cryotherapy is unsuccessful in the treatment of PLCNA, but curettage and cautery produces an acceptable cosmetic result.5 Surgical excision with or without split skin graft yields satisfactory cosmetic results.6
Tong et al7 presented a case of PLCNA in which the patient was treated with multiple immunosuppressive agents with little effect on the number or size of lesions. Systemic cyclophosphamide and prednisolone were used in combination, which resulted in healing of the patient's ulcers, stabilization of existing nodules, and no development of new nodules.7
We contend that the delivery of an extremely high concentration of intralesional methotrexate produces a much increased localized antimitotic effect. But it remains unclear whether methotrexate administered intralesionally is superior to systemic treatment. Tong et al7 used systemic methotrexate, 25 mg weekly for 3 months, without success, and their patient subsequently developed abnormal LFTs.2 Our patient received intralesional methotrexate with a dose up to 50 mg weekly for 6 months with the development of minor LFT derangement at that time. A direct comparison cannot be made between these patients given the dosage discrepancy. But we believe that intralesional methotrexate yields high localized tissue concentrations that cannot be achieved with systemic dosing because of potential toxicity. The systemic methotrexate levels in our patient were inadequate to produce shrinkage of distant untreated nodules. But the clinical improvement seen in our patient denotes a role for the use of intralesional methotrexate as a treatment option in patients who have localized lesions and are poor candidates for surgery or invasive procedures or patients who do not wish to risk potential postsurgical scarring. The only disclaimers are that it is too early to determine if there will be recurrence in treated areas and whether systemic amyloidosis will develop. Strict ongoing monitoring is in place with respect to these issues along with ongoing review of the patient's monoclonal gammopathy of unknown significance status.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Alster T.S., May R., Manaloto P. Nodular Amyloidosis Treated with a Pulsed Dye Laser. Dermatol Surg. 1999;25:133–135. doi: 10.1046/j.1524-4725.1999.08097.x. [DOI] [PubMed] [Google Scholar]
- 2.Grattan E.H., Burton J.L., Dahl M.G. Two cases of nodular cutaneous amyloid with positive organ-specific antibodies, treated by shave excision. Clin Exp Dermatol. 1988;13:187–189. doi: 10.1111/j.1365-2230.1988.tb01967.x. [DOI] [PubMed] [Google Scholar]
- 3.Lien M.H., Divya R., Nelson B.R. The efficacy of dermabrasion in the treatment of nodular amyloidosis. J Am Acad Dermatol. 1997;36:315–316. doi: 10.1016/s0190-9622(97)80406-9. [DOI] [PubMed] [Google Scholar]
- 4.Lesiak A., Rakowski A., Brzezinska A. Effective Treatment of Nodular Amyloidosis with Carbon Dioxide Laser. J Cutan Med Surg. 2012;16:372–374. doi: 10.1177/120347541201600519. [DOI] [PubMed] [Google Scholar]
- 5.Vestey J.P., Tidman M.J., McLaren K.M. Primary nodular cutaneous amyloidosis – long term follow-up and treatment. Clin Exp Dermatol. 1994;19:159–162. doi: 10.1111/j.1365-2230.1994.tb01148.x. [DOI] [PubMed] [Google Scholar]
- 6.Bozikov K., Janezic T. Excision and split thickness skin grafting in the treatment of nodular primary localized cutaneous amyloidosis. Eur J Dermatol. 2006;16:315–316. [PubMed] [Google Scholar]
- 7.Tong P.L., Walker W.A., Glancy R.J., Cooney J.P., Gebauer K. Primary localized cutaneous amyloidosis successfully treated with cyclophosphamide. Australas J Dermatol. 2013;54:12–15. doi: 10.1111/j.1440-0960.2011.00770.x. [DOI] [PubMed] [Google Scholar]