Abstract
Introduction
Existing studies of quantitative electroencephalography (qEEG) as a prognostic tool after cardiac arrest (CA) use methods that ignore the longitudinal pattern of qEEG data, resulting in significant information loss and precluding analysis of clinically important temporal trends. We tested the utility of group-based trajectory modeling (GBTM) for qEEG classification, focusing on the specific example of suppression ratio (SR).
Methods
We included comatose CA patients hospitalized from April 2010 to October 2014, excluding CA from trauma or neurological catastrophe. We used Persyst®v12 to generate SR trends and used semi-quantitative methods to choose appropriate sampling and averaging strategies. We used GBTM to partition SR data into different trajectories, and regression associate trajectories with outcome. We derived a multivariate logistic model using clinical variables without qEEG to predict survival, then added trajectories and/or non-longitudinal SR estimates and assessed changes in model performance.
Results
Overall, 289 CA patients had ≥36 hours of EEG yielding 10,404 hours of data (mean age 57 years, 81% arrested out-of-hospital, 33% shockable rhythms, 31% overall survival, 17% discharged to home or acute rehabilitation). We identified 4 distinct SR trajectories associated with survival (62%, 26%, 12% and 0%, P<0.0001 across groups) and CPC (35%, 10%, 4% and 0%, P<0.0001 across groups). Adding trajectories significantly improved model performance compared to adding non-longitudinal data.
Conclusions
Longitudinal analysis of continuous qEEG data using GBTM provides more predictive information than analysis of qEEG at single time-points after CA.
Search terms: Cardiac arrest, anoxic brain injury, quantitative electroencephalography, suppression ratio, prognosis
Introduction
The majority of patients hospitalized after sudden cardiac arrest (CA) are comatose.[1, 2] Seizures or other “malignant” electroencephalographic (EEG) patterns develop commonly in these patients and are associated with worse neurological outcomes. [3, 4] [5–7, 4, 8] EEG interpretation can be qualitative (e.g. “diffuse slowing with periods of attenuation”) or quantitative (e.g. spectral power or suppression ratio (SR)). Theoretical advantages to quantitative EEG analysis (qEEG) are reduced subjectivity and inter-observer variability, and the ability to detect subtle changes that may be imperceptible to the human eye.[9] Several qEEG metrics are associated with clinical outcomes after CA, including amplitude-integrated EEG,[10, 11] SR,[12–14] and bispectral index.[13, 14] Multiple qEEG metrics may be combined into composite prognostic tools.[15]
Previous studies of qEEG after CA have not accounted for the correlated, longitudinal nature of EEG data or dynamic evolution over time. Many report average qEEG measures within a given epoch, generally at baseline and fixed intervals thereafter. This results in significant information loss. This compression of continuous qEEG data is a specific example of a general problem for modern biomedical research: physiological variables are continuously recorded for extended durations with high time resolution, but not analyzed as such. Unfortunately, optimal analytical methods to approach intensively sampled longitudinal data in critically ill populations are not well established.
We sought to investigate longitudinal techniques for analysis of high-resolution time-series qEEG data and identify rational parameters for temporal and spatial averaging that minimize information loss. Group-based trajectory modeling (GBTM) is a specialized application of finite mixture modeling that determines trends in longitudinal data by identifying clusters of individuals with similar data evolution (trajectory) over time.[16] This approach leverages the power of repeated sampling.
We tested the utility of GBTM for qEEG analysis after CA, using the specific example of SR for methodological development. We hypothesized that GBTM could define distinct trajectories of SR that were associated with functional outcome at hospital discharge. Secondarily, we hypothesized that SR trajectory group membership would be an independent predictor of outcome and significantly improve prediction above and beyond non-longitudinal summary estimates of SR.
Methods
In this study, we aimed to (1) test whether global brain SR can be calculated from SR in individual EEG leads; (2) identify the optimal epoch length for comparing temporal trends in SR; (3) define prognostic SR trajectories that predict patient outcome; (4) test the minimum length of observation necessary to determine an SR trajectory; and (5) determine whether incremental information is gained when SR trajectories are added to a multivariable prognostic model using clinical variables to predict outcome.
Patients and setting
The University of Pittsburgh Institutional Review Board approved this study. We performed an observational cohort study of consecutive patients hospitalized at a single academic center from April 2010 to October 2014 with ≥6 hours of EEG monitoring. We maintain a registry of all patients treated by our Post-Cardiac Arrest Service including demographic and disease-specific baseline characteristics, treatments and outcomes. Our local standard of care is to monitor all comatose survivors of CA with continuous EEG,[17] and during the study period we cooled all comatose post-CA patients to 33°C We excluded patients from this analysis for arrest from trauma, exsanguination, or catastrophic neurological event (arrest secondary to subarachnoid hemorrhage, stroke or status epilepticus), for 24 hours, regardless of initial rhythm or arrest location. and those who died or were transitioned to comfort measures only within 6 hours of presentation.
EEG acquisition and processing
Our hospital has in-house EEG technologist coverage around-the-clock. EEG recordings generally started upon ICU arrival, an average of 6–8h after return of spontaneous circulation (ROSC). We applied 22 gold-plated cup electrodes to the scalp in the standard 10–20 International System of Electrode Placement and recorded data using XLTech Natus® Neuroworks digital video/EEG systems (Natus Medical, Pleasanton, CA). Clinical care, including antiepileptic and sedation management, was performed by the treating clinician according to standardized protocols (Supplemental Appendix 1). We continued EEG monitoring until awakening, death, or approximately 48h of recording without any actionable findings. It is our institutional protocol to stimulate patients sequentially using photic, auditory and tactile stimuli at the initiation of EEG monitoring. We included data derived during this stimulation period in the present analysis.
We generated qEEG metrics using Persyst® v12 (Persyst Development Co., Prescott, AZ) using standard processing engines. For SR, the software divides each lead’s data into 10-second epochs and calculates the total duration that epoch is “suppressed” (defined as a >0.5 seconds <3uV amplitude, the default threshold values in Persyst v12). The software calculates a 60-second running average to yield each channel’s SR. We used Persyst’s standard algorithm for artifact reduction (blind source separation) and exported qEEG trends in one-second epochs. We then combined these trends with patients’ baseline and outcomes data in a relational database using SQLServer®2014 (Microsoft, Redmond, WA).
Signal sampling and averaging
First, we determined whether important information was lost by averaging SR over the entire skull. Initial qEEG processing resulted second-by-second SR values for each channel in each patient. There is no theoretical limitation to the number of points that can be modeled using GBTM, but inclusion of non-informative data results in computationally intensive models that perform no better than more parsimonious models, and may perform worse if included data have a poor signal-to-noise ratio. By contrast, excessive down sampling leads to loss of information and statistical power.
Our clinical observation is that SR is highly spatially correlated across individual EEG channels and cerebral hemispheres. Thus, averaging hemispheric or whole-brain SR would result in little information loss and could improve signal-to-noise ratio by averaging out artifact from signal EEG leads. To test this, we selected a random sample of 10 patients and analyzed 75,000 SR data points. We calculated the correlation coefficient between left and right hemispheres to determine whether data from a single hemisphere was representative of whole brain SR. Next, we calculated all possible pairwise correlation coefficients between EEG channels to determine the range of correlations between leads. Finally, we used a generalized linear model with nested random effects to estimate the variance components for lead, observation, and random error (SPSS v22.0, IBM Corp, Armonk, NY). These were used to calculate the within-observation intraclass correlation coefficient (ICC) (i.e. the proportion of total variance accounted for by lead-to-lead variance).
Second, we hypothesized that clinically relevant changes in SR would occur over hours rather than seconds or minutes. Moreover, in patients with discontinuous backgrounds, large fluctuations in SR may reflect the intermittent EEG background activity rather than meaningful temporal evolution. To estimate the optimal duration for SR averaging, after developing our GBTM (see below), we repeated GBTM procedures varying epoch length (10 and 30 second; 1, 2, 5, 10, and 30 minute; 1, 2, 4 and 6 hour) and inspected the resultant trajectories for stability. We also compared the incremental change in Bayesian Information Criteria (BIC) after adjustment for the number of samples per trajectory and computational intensity between these models to identify an inflection point that balanced parsimony and information loss.
Third, we determined the minimum duration of observation necessary to accurately assign SR trajectories. GBTM requires that all trajectories be the same duration, so data from subjects with varying durations of monitoring could not be combined into a single model without censoring data at the shortest duration of observation. In our cohort, approximately one-third of subjects were monitored at least 48 hours. We performed GBTM (see below) in this subgroup using 48 hours of observation, then repeated GBTM procedures iteratively censoring the data at 42, 36, 30, 24, 18 and 12 hours. Using the 48-hour trajectories as a “gold standard,” we calculated percent misclassification for the censored data and plotted this and potential sample size against duration of observation.
Based on the results of these analyses (see Results), in our final GBTM models we used 36-hour observations of median hemispheric SR evaluated in consecutive 1-hour epochs.
Predictors, covariates and outcomes
Our fourth step was to examine trajectory group membership from GBTM as a predictor of neurological outcome at hospital discharge in regression modeling. As non-longitudinal alternative representations of SR, we used median SR at baseline (hour 0 to 1) and day one (hour 24 to 25) treated as a continuous predictors. Baseline SR measurements included data obtained during patient stimulation at EEG initiation.
We abstracted demographic and basic patient information from our registry, including patient age, gender, location of arrest (out-of-hospital versus in-hospital), presenting rhythm (ventricular tachycardia or fibrillation (VT/VF) versus pulseless electrical activity (PEA) or asystole), Charlson Comorbidity Index (CCI) and Pittsburgh CA Category (PCAC). The PCAC is a validated clinical prediction tool that stratifies CA survivors by risk of in-hospital death or neurological deterioration based on neurological examination and cardiopulmonary dysfunction in the first 6h after ROSC.[18] The tool stratifies survivors of CA into four categories that are strongly predictive of survival and functional outcome. PCAC I patients are by definition awake, and therefore excluded. Other standard CA covariates are collapse to cardiopulmonary resuscitation (CPR) and CPR to ROSC intervals, witnessed collapse, bystander-administered CPR resuscitation, and use of hypothermia. We have previously demonstrated arrest intervals,[19] witnessed collapse and bystander CPR,[20] to be unreliable reported in our care system, and so did not include them in our models. Temperature management during the study period was standardized across all eligible subjects (Supplemental Figure 3), excluding this as a covariate. Finally, we collected sedative and antiepileptic medication data, which we further stratified by observation period (0–17h and 18–36h).
Our primary outcome of interest was survival to hospital discharge, and our secondary outcome was functionally favorable survival, defined as discharge to home or acute rehabilitation.
Statistical methods
We used descriptive statistics to summarize baseline population characteristics and outcomes. We used GBTM with a censored normal distribution, and used Bayesian and Akaike information criteria (BIC and AIC) for GBTM model selection. To test the incremental value of including SR trajectory group membership, we constructed a series of adjusted logistic regression models. First, we developed a saturated “Clinical Model” including all potential baseline predictors of outcome except for EEG data. We included baseline predictors in this model regardless of their unadjusted association with outcome since our goal was to explain the maximum amount of variability in outcome possible without EEG data, rather than determining independent predictors of outcome. We then challenged this model to assess performance improvement by sequential addition of non-longitudinal SR (baseline and day 1 medians), and trajectory group membership. Given the low incidence of favorable outcomes in certain trajectory groups, we used Firth’s penalized likelihood approach to minimize bias in coefficient estimates.
We used several complementary methods to compare performances of the Clinical Model and models incorporating SR metrics. To compare models, we calculated C-statistics for each model and compared these values and AICs between models. We also calculated the Net Reclassification Improvement (NRI) between models using in-hospital mortality cutoffs of 15, 30, and 45%, and 5, 50 and 95%.[21] We used SAS v9.3 (SAS Institute, Cary NC).
Results
Cohort composition
During the study period, 1012 CA patients were treated, and 451 (45%) of these met both inclusion and exclusion criteria (Figure 1). In total, 37,447 hours of EEG data were obtained and analyzed (mean 83 hours/patient), and 289 patients had ≥36 hours of EEG data. Mean age was 58 years, 351 (78%) arrested out-of-hospital, and 132 (34%) had a shockable rhythm (Table 1). Survival to discharge was 30% and 16% had functionally favorable survival.
Figure 1.
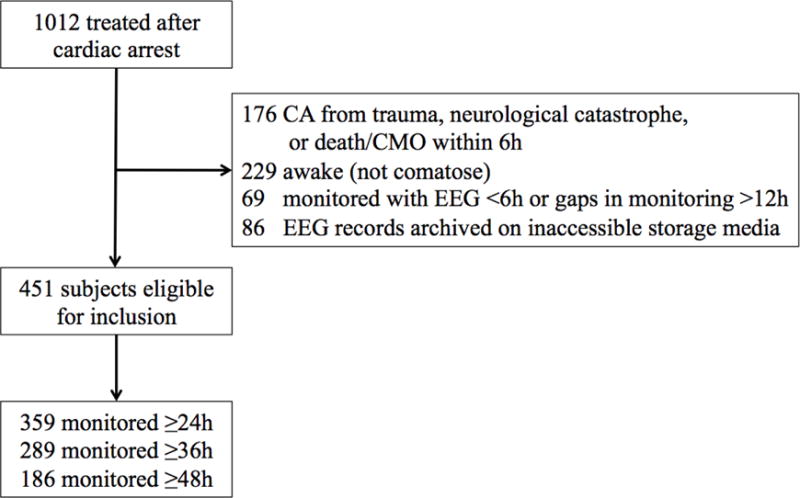
Subject accrual and exclusions
Table 1.
Baseline population characteristics and outcomes, overall and stratified by trajectory group membership
| Subjects included in trajectory analysis | |||||||
|---|---|---|---|---|---|---|---|
| Characteristic | Overall Cohort (n=451) |
Entire GBTM Cohort (n=289) |
Trajectory Group 1 (n=88) |
Trajectory Group 2 (n=85) |
Trajectory Group 3 (n=52) |
Trajectory Group 4 (n=64) |
|
| Age, years | 57.7 (16.4) | 57.1 (15.6) | 52.8 (15.9) | 58.7 (14.8) | 57.5 (16.0) | 60.4 (15.2) | |
| Female gender | 164 (36.4%) | 97 (33.6%) | 30 (34.1%) | 25 (29.4%) | 20 (38.5%) | 22 (34.4%) | |
| Out-of-hospital arrest | 352 (78.1%) | 235 (81.3%) | 70 (79.5%) | 67 (78.8%) | 44 (84.6%) | 54 (84.4%) | |
| Pittsburgh CA Category | |||||||
| II | 100 (24.0%) | 72 (26.5%) | 35 (42.2%) | 26 (32.9%) | 6 (12.2%) | 5 (8.2%) | |
| III | 55 (13.2%) | 37 (13.6%) | 17 (20.5%) | 11 (13.9%) | 5 (10.2%) | 4 (6.6%) | |
| IV | 256 (61.4%) | 163 (59.9%) | 31 (37.3%) | 42 (53.2%) | 38 (77.6%) | 52 (85.2%) | |
| Charlson comorbidity index | 1.0 (1.6) | 1.0 (1.6) | 1.0 (1.7) | 0.8 (1.4) | 0.8 (1.3) | 1.3 (1.8) | |
| Initial arrest rhythm | |||||||
| VF/VT | 132 (33.8%) | 95 (36.1%) | 39 (50.6%) | 31 (39.2%) | 15 (31.9%) | 10 (16.7%) | |
| PEA | 144 (36.8%) | 86 (32.7%) | 21 (27.3%) | 21 (26.6%) | 22 (46.8%) | 22 (36.7%) | |
| Asystole | 115 (29.4%) | 82 (31.2%) | 17 (22.1%) | 27 (34.2%) | 10 (21.3%) | 28 (46.7%) | |
| Hospital length of stay | |||||||
| Survivors | 18 (12 – 27) | 18.5 (13 – 27.5) | 18 (13 – 27) | 22 (13 – 32) | 14 (9 – 23) | 18 (18 – 18) | |
| Non-survivors | 4 (3 – 6) | 4 (4 – 6) | 5.5 (4 – 7) | 5 (4 – 9) | 4 (3 – 5) | 4 (3 – 6) | |
| Survival | 134 (30.1%) | 92 (31.8%) | 56 (63.6%) | 27 (31.8%) | 8 (15.4%) | 1 (1.6%) | |
| Favorable neurological outcome | 73 (16.5%) | 49 (17.0%) | 35 (39.8%) | 11 (12.9%) | 3 (5.8%) | 0 (0.0%) | |
| Mode of death& | |||||||
| Withdrawal for neurological prognosis | 211 (67.2) | 158 (81.0) | 22 (68.8) | 49 (84.5) | 40 (90.9) | 47 (77.1) | |
| Brain death | 32 (10.2) | 13 (6.7) | 0 (0) | 2 (3.5) | 1 (2.33) | 10 (16.4) | |
| Unstable | 56 (17.8) | 19 (9.7) | 9 (28.1) | 7 (12.1) | 1 (2.3) | 2 (3.3) | |
| Stable | 15 (4.8) | 5 (2.6) | 1 (3.1) | 0 (0) | 2 (4.6) | 2 (3.3) | |
GBTM cohort is comprised of subjects within the overall cohort with ≥36 hours of electroencephalographic monitoring
Reported as number and corresponding percentages of non-survivors.
Abbreviations: GBTM – Group-based trajectory modeling; CA – Cardiac arrest; VT/VF – Ventricular tachycardia or fibrillation; PEA – Pulseless electrical activity. Data are presented as mean (standard deviation), raw number with corresponding percentage and median [interquartile range] for length of stay.
Signal sampling and averaging
Calculating SR by EEG channel using a longitudinal bipolar montage resulted in approximately 2.16×108 data points (average 478,000 points/patient). Left and right hemisphere SRs were near-perfectly correlated (Pearson’s R=0.98). In all possible pairwise comparisons of SR across bipolar channels, median correlation coefficient was 0.87 (IQR 0.83–0.92, all Ps for pairwise correlations <0.0001). The ICC for SR was 0.85, indicating a strong correlation between simultaneously measured SR in across leads. Since signal quality in individual leads is may be degraded by noise or artifact, falsely reducing SR, we chose to analyze average SR averaged across a single cerebral hemisphere.
Overall, 186 subjects had ≥48 hours of EEG data. Using this 48-hour cohort and iteratively censoring data input into GBTM, we were able to calculate the rate of trajectory group misclassification using these censored data compared to the full model. Inspecting the plot of percent misclassification and sample size versus trajectory length (Supplemental Appendix, Figure 1a), we selected 36-hour trajectories for subsequent analyses and final modeling, yielding a cohort of 289 patients.
When we repeated GBTM modeling using varying epoch lengths, we found good stability of trajectories across models (Supplemental Appendix, Figure 2). Models using more than 25,000 data points (10-minute epochs or shorter) failed to converge. Comparing adjusted BICs and computational intensity across these models supported the use of either 40-minute or 60-minute epochs (Supplemental Appendix, Figure 1b). Consequently, we chose to use 60-minute epochs for subsequent analyses and final modeling.
Trajectory modeling
Using these sampling strategies and GBTM, a 4-group trajectory model best fit the data (Figure 2). Both survival and favorable neurological outcomes decreased by approximately 50% across increasing trajectory groups, then fell to near 0 for trajectory group 4 (Table 2).
Figure 2.
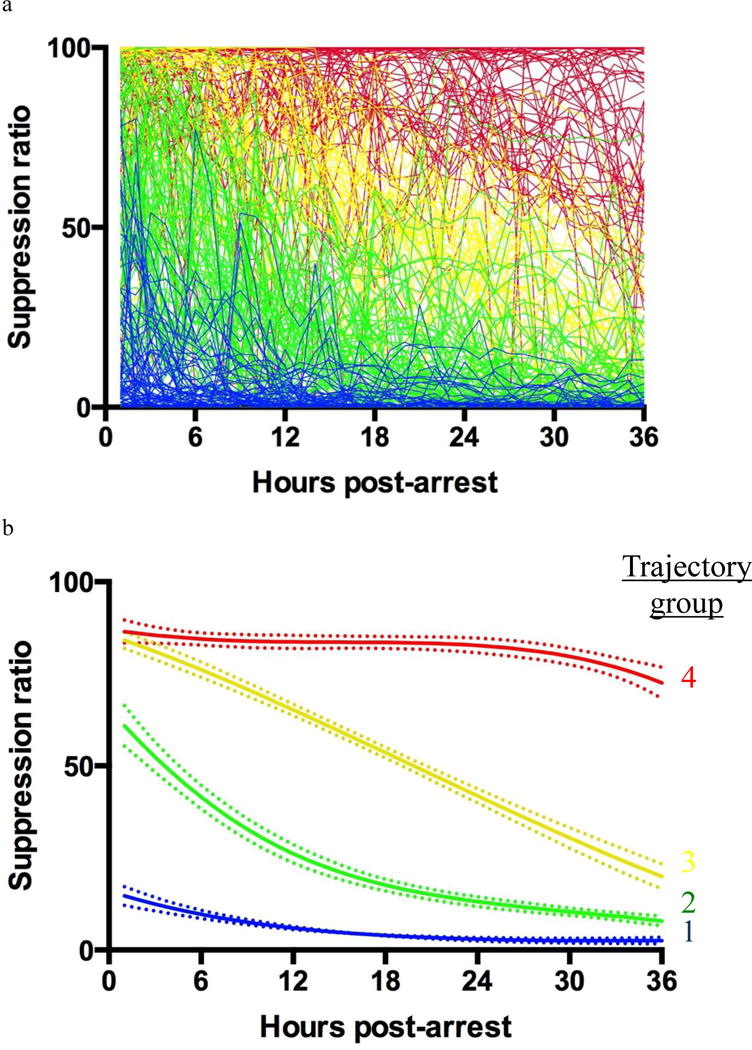
A) Raw suppression ratio data by subject, coded by final trajectory group membership; B) Final trajectory model with corresponding 95% confidence bands for suppression ratio in the first 36h after cardiac arrest
Table 2.
Association of trajectory group membership with outcomes
| Trajectory Group Membership | Survival to discharge | Discharged with favorable outcome | ||
|---|---|---|---|---|
| Percentage (95% CI) | Unadjusted OR (95% CI) | Percentage (95% CI) | Unadjusted OR (95% CI) | |
| Overall (n = 289) | 32% (27 – 38%) | – | 17% (13 – 22%) | – |
| Group 1 (n = 88) | 64% (53 – 74%) | 250 (13.2 to >999) | 40% (29 – 51%) | 83.3 (4.88 to >999) |
| Group 2 (n = 85) | 32% (22 – 43%) | 66.7 (3.76 to >999) | 13% (7 – 22%) | 20.4 (1.16 to 333) |
| Group 3 (n = 52) | 15% (7 – 28%) | 21.7 (1.17 to 500) | 6% (1 – 16%) | 9.35 (0.46 to 200) |
| Group 4 (n = 64) | 2% (0 – 8%) | Ref | 0% (0 – 6%) | Ref |
Abbreviations: OR – Odds ratio; CI – Confidence interval.
Comparison of prognostic models
The best performing prognostic model included clinical predictors, baseline SR and trajectory group membership. Adding baseline SR and trajectory group membership individually or in combination to the base clinical model improved discriminatory power (Supplemental Table 1). Adding baseline SR and trajectory group membership individually and in combination also resulted in significantly improved NRI (P<0.0001 for all three comparisons).
Discussion
We present results from a large cohort study of EEG after cardiac arrest, and the first to use longitudinal methods to analyze these data. We set forth a methodological framework to analyze these intensively sampled, time-series data. Using GBTM to describe the evolution of SR over time, we identified 4 strongly prognostic trajectories that describe these data. Incorporating these trajectories into prognostic modeling significantly improves the discriminatory power of these models to predict outcome compared to models that use only clinical and non-longitudinal EEG data.
Our results are consistent with, and expand upon, work recently published by Oh, et al., who report the association of time-to-normalization of single-channel amplitude-integrated EEG (aEEG) after CA with outcome.[22] Consistent with Oh’s results, we find that qEEG in the first 36 hours after CA identifies a subpopulation of patients with uniformly poor outcomes. Oh, et al., describe their reliance on a single EEG channel as a potential limitation, and others have called for validation of simplified EEG montages before widespread use.[23] To our knowledge, our work is the first to support this strategy. The degree of spatial correlation we demonstrate between individual EEG leads in this population demonstrates that simplified montages are unlikely to result in information loss about SR, although other qEEG measures may differ. This lack of spatial heterogeneity between hemispheres may be a reflection of the relatively diffuse brain injury, in contrast to the more focal lesions found after cerebrovascular accident or brain trauma. Similarly, the lack of other regional variation in spectral power, for example between frontal and occipital regions, may reflect a relatively static (over the 36h observation period we selected) and diffuse post-anoxic cortical network failure in contrast to that observed in focal brain trauma or in response to sedation.[24]
Currently, guidelines recommend delaying neurological prognostication for at least 72 hours after CA because, prior to this time no clinical sign, test or combination of findings short of progression to brain death preclude a favorable outcome.[25–32] Our work strengthens the assertion that qEEG, in combination with clinical findings, might shorten the time to accurate neurological prognostication. While patients following trajectory group 4 had no favorable outcomes, the 95% confidence interval for our point estimate was 0 to 6%. Withdrawal of life-sustaining therapy is uniformly fatal in this population, so new methods must be thoroughly evaluated to prevent avoidable mortality resulting from inaccurate prognostication and subsequent withdrawal. EEG and qEEG are two of multiple modalities available to inform accurate prognostication, and SR is just one quantitative metric that can be derived from the complex and information-rich EEG signal. Further work is also needed to elucidate which of many qEEG metrics are the most informative, alone or in combination, for prognostication. Before consideration of prognostication earlier than 72 hours after CA, our results must be replicated by others to establish external validity and narrow confidence intervals around the final point estimate of outcome. To avoid self-fulfilling prophecies, this validation should be prospective, and carried out in a cohort of patients who are consistently monitored for at least 36 hours without exposure to withdrawal of life-sustaining therapy based on perceived neurological prognosis.
Our findings also suggest the significance of baseline EEG suppression after CA may be limited. Most of our subjects fell into trajectories with baseline SR above 50%. Although baseline SR was associated with outcome, improvement in SR over the first 36 hours portended significantly better outcomes than persistent suppression. This is consistent with non-quantitative analyses by from Cloostermans, et al.,[5] which demonstrate favorable outcomes in some patients with early burst suppression that resolves over 18–24h. The reason for this phenomenon remains unclear. EEG activity may be suppressed by early, reversible neurological injury from ischemia and reperfusion, sedation, hypothermia, or a combination of these factors. We note, for example that the dynamic periods in temperature trajectories corresponding to rewarming (Supplemental Figure 3) coincide with the epochs of maximum change in SR trajectories. SR can also be affected by metabolic confounders such as evolving renal function, malignant EEG patterns such as seizures, sedation and antiepileptic therapy (Supplemental Table 2) and cerebral hypoperfusion. GBTM is not well suited in its current stage of development to explore these potentially important covariates in robust adjusted analyses. Future longitudinal analyses may address the effects of concurrent potential confounders.
The ability to rapidly and accurately identify patients at high-risk of future neurological deterioration or death has clear importance for clinical research, particularly interventional trials. Our findings suggest that qEEG evolution over time can improve risk stratification in this population, as previously proposed by Friberg, et al.[23] Such analysis holds the promise of allowing targeted therapies to be initiated for selected patients in response to real-time EEG changes or titrated based on dynamic EEG responsive to therapy. For example, energy supply-demand mismatch resulting from cerebral hypoperfusion leads ultimately to energetic failure, loss of membrane potential and suppression of electrical activity (i.e. increased SR).[33–35] If prolonged or severe, this can result in neuronal apoptosis and/or necrosis and ultimately irrecoverable injury. Thus, increased SR might provide an actionable warning of early energy imbalance that could be corrected before irreversible damage occurs. This type of EEG-guided titration of care is somewhat akin to titrating vasoactive medications in response to continuous measures of arterial pressure and end-organ perfusion, rather than infrequent, discrete blood pressure measurements. Such a concept merits future investigation.
Our study has several limitations. Our primary outcome of interest was neurological outcome at hospital discharge, which can be confounded by withdrawal of life-sustaining therapy based on anticipated prognosis. Care limitations create the risk of self-fulfilling prophecies, whereby qEEG characteristics such as high SR might prompt clinicians to limit life-sustaining therapy, inadvertently increasing mortality in those subjects who follow a trajectory of prolonged EEG suppression. We note that median length of stay did not differ across trajectory groups, suggesting that life-sustaining therapy was not systematically withdrawn earlier in patients following specific trajectories of SR, nor did the proportion of subjects exposed to withdrawal for neurological prognosis differ across trajectories. Second, since GBTM requires equal length observations across subjects, we excluded subjects with less than 36h of data available from our final analyses. This may limit the generalizability of our findings to the broader post-CA patient population. However, baseline characteristics did not differ between the entire cohort and those with >36h of data, suggesting against biased sampling. The single-center design of our study limits generalizability. We established hospital-wide care protocols including routine use of targeted temperature management, continuous EEG, aggressive seizure control and best-practice critical care.[17] This decreased variability in care improves the internal validity of our study, but our results must be replicated in other care systems.
In conclusion, we have described a methodological framework to analyze intensively sampled, time-series qEEG data and demonstrated the value added by using GBTM to model SR after CA. We identified strongly prognostic SR trajectories, which if validated could substantially shorten the time to accurate neurological prognostication, be used to enroll high-risk subjects in clinical research or identify dynamic treatment responsiveness. More broadly, these methods leverage the power of high-resolution data and are likely to be increasingly utilized in biomedical research.
Supplementary Material
Table 3.
Final adjusted model predicting in-hospital mortality with optimal performance characteristics
| Characteristic | Odds ratio (95% CI) |
|---|---|
| Age | 1.01 (0.99 – 1.03) |
| Female Gender | 0.76 (0.37 – 1.60) |
| Initial rhythm | |
| VT/VF | Ref |
| PEA | 1.96 (0.79 – 4.91) |
| Asystole | 1.72 (0.67– 4.45) |
| Unknown | 1.67 (0.50 – 5.59) |
| Out-of-hospital cardiac arrest | 0.85 (0.35 – 2.09) |
| Pittsburgh CA Category | |
| II | 0.20 (0.09 – 0.44) |
| III | 0.21 (0.08 – 0.55) |
| IV | Ref |
| Charlson Comorbidity Index | 1.03 (0.83 – 1.29) |
| Baseline SR | 1.03 (1.01 – 1.04) |
| Trajectory group membership | |
| 1 | 0.05 (0.003 – 0.97) |
| 2 | 0.06 (0.004 – 0.87) |
| 3 | 0.07 (0.004 – 1.21) |
| 4 | Ref |
Abbreviations: VT/VF – Ventricular tachycardia or fibrillation; PEA – Pulseless electrical activity; CA – Cardiac arrest.
Acknowledgments
Funding: Dr. Elmer’s research time is supported by NIH grant 5K12HL109068.
Footnotes
Supplemental data files: Supplemental Table 1, Supplemental Figures 1a, 1b and 2, Supplemental Appendix.
Disclosures: The authors have no additional funding or conflicts of interest to report.
References
- 1.Coppler PJ, Elmer J, Calderon L, Sabedra A, Doshi AA, Callaway CW, et al. Validation of the Pittsburgh Cardiac Arrest Category illness severity score. Resuscitation. 2015 doi: 10.1016/j.resuscitation.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laver S, Farrow C, Turner D, Nolan J. Mode of death after admission to an intensive care unit following cardiac arrest. Intensive care medicine. 2004;30(11):2126–8. doi: 10.1007/s00134-004-2425-z. [DOI] [PubMed] [Google Scholar]
- 3.Rittenberger JC, Popescu A, Brenner RP, Guyette FX, Callaway CW. Frequency and timing of nonconvulsive status epilepticus in comatose post-cardiac arrest subjects treated with hypothermia. Neurocritical care. 2012;16(1):114–22. doi: 10.1007/s12028-011-9565-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rossetti AO, Carrera E, Oddo M. Early EEG correlates of neuronal injury after brain anoxia. Neurology. 2012;78(11):796–802. doi: 10.1212/WNL.0b013e318249f6bb. [DOI] [PubMed] [Google Scholar]
- 5.Cloostermans MC, van Meulen FB, Eertman CJ, Hom HW, van Putten MJ. Continuous electroencephalography monitoring for early prediction of neurological outcome in postanoxic patients after cardiac arrest: a prospective cohort study. Critical care medicine. 2012;40(10):2867–75. doi: 10.1097/CCM.0b013e31825b94f0. [DOI] [PubMed] [Google Scholar]
- 6.Crepeau AZ, Rabinstein AA, Fugate JE, Mandrekar J, Wijdicks EF, White RD, et al. Continuous EEG in therapeutic hypothermia after cardiac arrest: prognostic and clinical value. Neurology. 2013;80(4):339–44. doi: 10.1212/WNL.0b013e31827f089d. [DOI] [PubMed] [Google Scholar]
- 7.Mani R, Schmitt SE, Mazer M, Putt ME, Gaieski DF. The frequency and timing of epileptiform activity on continuous electroencephalogram in comatose post-cardiac arrest syndrome patients treated with therapeutic hypothermia. Resuscitation. 2012;83(7):840–7. doi: 10.1016/j.resuscitation.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rossetti AO, Urbano LA, Delodder F, Kaplan PW, Oddo M. Prognostic value of continuous EEG monitoring during therapeutic hypothermia after cardiac arrest. Critical care. 2010;14(5):R173. doi: 10.1186/cc9276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Foreman B, Claassen J. Quantitative EEG for the detection of brain ischemia. Critical care. 2012;16(2):216. doi: 10.1186/cc11230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rundgren M, Westhall E, Cronberg T, Rosen I, Friberg H. Continuous amplitude-integrated electroencephalogram predicts outcome in hypothermia-treated cardiac arrest patients. Critical care medicine. 2010;38(9):1838–44. doi: 10.1097/CCM.0b013e3181eaa1e7. [DOI] [PubMed] [Google Scholar]
- 11.Oh SH, Park KN, Kim YM, Kim HJ, Youn CS, Kim SH, et al. The prognostic value of continuous amplitude-integrated electroencephalogram applied immediately after return of spontaneous circulation in therapeutic hypothermia-treated cardiac arrest patients. Resuscitation. 2013;84(2):200–5. doi: 10.1016/j.resuscitation.2012.09.031. [DOI] [PubMed] [Google Scholar]
- 12.Wennervirta JE, Ermes MJ, Tiainen SM, Salmi TK, Hynninen MS, Sarkela MO, et al. Hypothermia-treated cardiac arrest patients with good neurological outcome differ early in quantitative variables of EEG suppression and epileptiform activity. Critical care medicine. 2009;37(8):2427–35. doi: 10.1097/CCM.0b013e3181a0ff84. [DOI] [PubMed] [Google Scholar]
- 13.Seder DB, Fraser GL, Robbins T, Libby L, Riker RR. The bispectral index and suppression ratio are very early predictors of neurological outcome during therapeutic hypothermia after cardiac arrest. Intensive care medicine. 2010;36(2):281–8. doi: 10.1007/s00134-009-1691-1. [DOI] [PubMed] [Google Scholar]
- 14.Selig C, Riegger C, Dirks B, Pawlik M, Seyfried T, Klingler W. Bispectral index (BIS) and suppression ratio (SR) as an early predictor of unfavourable neurological outcome after cardiac arrest. Resuscitation. 2014;85(2):221–6. doi: 10.1016/j.resuscitation.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 15.Tjepkema-Cloostermans MC, van Meulen FB, Meinsma G, van Putten MJ. A Cerebral Recovery Index (CRI) for early prognosis in patients after cardiac arrest. Critical care. 2013;17(5):R252. doi: 10.1186/cc13078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annual review of clinical psychology. 2010;6:109–38. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- 17.Rittenberger JC, Guyette FX, Tisherman SA, DeVita MA, Alvarez RJ, Callaway CW. Outcomes of a hospital-wide plan to improve care of comatose survivors of cardiac arrest. Resuscitation. 2008;79(2):198–204. doi: 10.1016/j.resuscitation.2008.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rittenberger JC, Tisherman SA, Holm MB, Guyette FX, Callaway CW. An early, novel illness severity score to predict outcome after cardiac arrest. Resuscitation. 2011;82(11):1399–404. doi: 10.1016/j.resuscitation.2011.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frisch A, Reynolds JC, Condle J, Gruen D, Callaway CW. Documentation discrepancies of time-dependent critical events in out of hospital cardiac arrest. Resuscitation. 2014;85(8):1111–4. doi: 10.1016/j.resuscitation.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 20.Rittenberger JC, Martin JR, Kelly LJ, Roth RN, Hostler D, Callaway CW. Inter-rater reliability for witnessed collapse and presence of bystander CPR. Resuscitation. 2006;70(3):410–5. doi: 10.1016/j.resuscitation.2005.12.015. [DOI] [PubMed] [Google Scholar]
- 21.Pencina MJ, D’Agostino RB, Sr, D’Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157–72. doi: 10.1002/sim.2929. discussion 207–12. [DOI] [PubMed] [Google Scholar]
- 22.Oh SH, Park KN, Shon YM, Kim YM, Kim HJ, Youn CS, et al. Continuous Amplitude-Integrated Electroencephalographic Monitoring is a Useful Prognostic Tool for Hypothermia-Treated Cardiac Arrest Patients. Circulation. 2015 doi: 10.1161/CIRCULATIONAHA.115.015754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Friberg H, Westhall E, Rosen I, Rundgren M, Nielsen N, Cronberg T. Clinical review: Continuous and simplified electroencephalography to monitor brain recovery after cardiac arrest. Critical care. 2013;17(4):233. doi: 10.1186/cc12699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chennu S, O’Connor S, Adapa R, Menon DK, Bekinschtein TA. Brain Connectivity Dissociates Responsiveness from Drug Exposure during Propofol-Induced Transitions of Consciousness. PLoS Comput Biol. 2016;12(1):e1004669. doi: 10.1371/journal.pcbi.1004669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kamps MJ, Horn J, Oddo M, Fugate JE, Storm C, Cronberg T, et al. Prognostication of neurologic outcome in cardiac arrest patients after mild therapeutic hypothermia: a meta-analysis of the current literature. Intensive care medicine. 2013;39(10):1671–82. doi: 10.1007/s00134-013-3004-y. [DOI] [PubMed] [Google Scholar]
- 26.Bouwes A, Binnekade JM, Kuiper MA, Bosch FH, Zandstra DF, Toornvliet AC, et al. Prognosis of coma after therapeutic hypothermia: a prospective cohort study. Annals of neurology. 2012;71(2):206–12. doi: 10.1002/ana.22632. [DOI] [PubMed] [Google Scholar]
- 27.Rossetti AO, Koenig MA. Prognostication after cardiac arrest: a tale of timing, confounders, and self-fulfillment. Neurology. 2011;77(14):1324–5. doi: 10.1212/WNL.0b013e318231533b. [DOI] [PubMed] [Google Scholar]
- 28.Cronberg T, Horn J, Kuiper MA, Friberg H, Nielsen N. A structured approach to neurologic prognostication in clinical cardiac arrest trials. Scandinavian journal of trauma, resuscitation and emergency medicine. 2013;21:45. doi: 10.1186/1757-7241-21-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cronberg T, Brizzi M, Liedholm LJ, Rosen I, Rubertsson S, Rylander C, et al. Neurological prognostication after cardiac arrest–recommendations from the Swedish Resuscitation Council. Resuscitation. 2013;84(7):867–72. doi: 10.1016/j.resuscitation.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 30.Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S, Quality Standards Subcommittee of the American Academy of N Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67(2):203–10. doi: 10.1212/01.wnl.0000227183.21314.cd. [DOI] [PubMed] [Google Scholar]
- 31.Sandroni C, Cariou A, Cavallaro F, Cronberg T, Friberg H, Hoedemaekers C, et al. Prognostication in comatose survivors of cardiac arrest: an advisory statement from the European Resuscitation Council and the European Society of Intensive Care Medicine. Resuscitation. 2014;85(12):1779–89. doi: 10.1016/j.resuscitation.2014.08.011. [DOI] [PubMed] [Google Scholar]
- 32.Golan E, Barrett K, Alali AS, Duggal A, Jichici D, Pinto R, et al. Predicting neurologic outcome after targeted temperature management for cardiac arrest: systematic review and meta-analysis. Critical care medicine. 2014;42(8):1919–30. doi: 10.1097/CCM.0000000000000335. [DOI] [PubMed] [Google Scholar]
- 33.Hofmeijer J, Tjepkema-Cloostermans MC, van Putten MJ. Burst-suppression with identical bursts: a distinct EEG pattern with poor outcome in postanoxic coma. Clinical neurophysiology: official journal of the International Federation of Clinical Neurophysiology. 2014;125(5):947–54. doi: 10.1016/j.clinph.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 34.Niedermeyer E, Sherman DL, Geocadin RJ, Hansen HC, Hanley DF. The burst-suppression electroencephalogram. Clin Electroencephalogr. 1999;30(3):99–105. doi: 10.1177/155005949903000305. [DOI] [PubMed] [Google Scholar]
- 35.Thomke F, Brand A, Weilemann SL. The temporal dynamics of postanoxic burst-suppression EEG. Journal of clinical neurophysiology: official publication of the American Electroencephalographic Society. 2002;19(1):24–31. doi: 10.1097/00004691-200201000-00003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


