Abstract
Introduction
Retinal structural changes in subjects with mild cognitive impairment (MCI) remain a subject of controversy.
Methods
We investigated the correlation between optical coherence tomography (OCT) of the retinal sublayers, including the retinal nerve fiber layer (RNFL), and cognitive function in subjects with amnestic MCI and compared the OCT findings with matched controls. We also performed a meta-analysis of the world literature using a random-effects model.
Results
We found no statistically significant differences in OCT between amnestic MCI (aMCI) and controls. In aMCI subjects, we found an inverse relationship between RNFL thickness and two cognitive tests (delayed story recall and a word-list learning test and the word-list test). The meta-analysis revealed a statistically significant decrease in RNFL thickness in MCI subjects.
Discussion
The inverse relationship between cognitive testing and RNFL thickness suggests that retinal involvement may include paradoxically increased thickness of the RNFL, which could suggest gliotic reactive changes.
Keywords: Alzheimer's disease, Mild cognitive impairment, Retinal nerve fiber layer, Optical coherence tomography, Biomarkers
1. Introduction
Dementia of Alzheimer's disease type (DAT) was first described nearly 110 years ago by the psychiatrist Alois Alzheimer [1]. Today, the definitive diagnosis of DAT is made at brain autopsy, whereas clinical diagnosis and staging involves relatively invasive and expensive techniques [2], [3]. Therefore, along with continued and redoubled efforts to understand the disease and develop new therapies, numerous groups have set out to identify more sensitive (and perhaps less invasive) diagnostic approaches. Hinton et al. [4] in 1986 identified histopathologic evidence of axonal degeneration of the optic nerve and reduced thickness of the retinal nerve fiber layer (RNFL) in patients with DAT, making the eye a potential surrogate organ to detect the pathologic changes of the disease. Since then, multiple studies have reported significant findings in the eyes of DAT patients, which was recently in a paper by by Javaid et al. [5], which revealed at least 12 different visual or ocular potential markers of the disease.
Over the past 25 years, optical coherence tomography (OCT) has emerged as a powerful tool aiding in the diagnosis and management of various ocular diseases and for identifying ocular involvement in systemic and neurologic diseases [6], [7], [8], [9], [10], [11]. Advantages of OCT include that it is noninvasive, readily available in most ophthalmology and many neurology clinics, and can provide high-resolution cross-sectional imaging of the RNFL and macula [12]. To date, many researchers have reported RNFL thinning on OCT in patients with DAT, and two recent meta-analyses noted RNFL thinning affected all quadrants of the optic nerve head [13], [14].
Finding RNFL thinning in DAT is a milestone toward validating the eye as a surrogate organ for disease detection and monitoring. However, many researchers argue that early detection should identify candidates for therapy before the onset of cognitive impairment, as the damage is likely irreversible once symptoms arise [15]. With this insight there is an interest in identifying early changes in subjects with mild cognitive impairment (MCI). MCI is a clinical condition which can represent a transition to dementia of the Alzheimer type and consists of cognitive impairment on standard tests but no impairment of activities of daily living. Thus, MCI increases risk for DAT [2]. In particular, amnestic MCI (aMCI), where episodic memory is impaired without impairment of executive function, language, or other domains, is viewed by some as prodromal DAT [1], [16].
Several studies have used OCT to examine the RNFL in subjects with a clinical diagnosis of MCI [17], [18], [19], [20], [21], [22], [23], [24], [25], [26]. Ascaso et al. [18] found all quadrants of the “peripapillary” RNFL (except nasal) to be significantly thinner in aMCI subjects compared with cognitively healthy controls. Similarly, Gao et al. [20] found the temporal quadrant significantly thinner, whereas Liu et al. [22] reported thinning in the superior quadrant. In contrast, two other studies did not find significant difference between aMCI and controls after adjusting for confounders [19], [25]. Coppola et al. [14] recently performed a meta-analysis of two OCT studies in MCI, finding all quadrants but superior significantly thinner. We believe that the controversy in these studies is likely related to high variability in the exclusion criteria, in cognitive testing, and in rigor of adjustment for confounders.
Another potential explanation for the variable results could relate to the unexplored variable of gliosis in the pathogenesis of DAT in the eye. Gliosis may precede the onset of neuronal death and may therefore obfuscate the detection of RNFL thinning. Gliosis is defined as hypertrophy and proliferation of astrocytes and other glial cells and has been shown to occur in the brain of DAT patients, correlating with the duration of dementia [27], [28]. Although it remains unclear if gliosis is pathogenic, in animal models it has been found to occur early on in the disease and is currently being explored as a potential therapeutic target [29], [30], [31]. However, at this time, there have not been any histopathologic or clinical studies exploring gliosis in the eyes of aMCI subjects.
The present study was designed to address some of the limitations of previous studies, by using a case-control study design and strictly matching each aMCI subject to an age-, sex-, and race-matched control to minimize potential confounders [32], [33]. We also ensured that controls underwent the same rigorous cognitive testing as the aMCI participants. We examined the “peripapillary” RNFL thickness and retinal sublayers of the macula, particularly the ganglion cell layer and inner plexiform layer (GC-IPL), and explored their correlation with cognitive scores. Finally, we performed a meta-analysis of the current world literature.
2. Materials and methods
2.1. Research study
2.1.1. Study approval
The study was approved by the Institutional Review Board of Northwestern University, and written informed consent was obtained from all the participants.
2.1.2. Subjects
Twenty research participants with a clinical diagnosis of aMCI were recruited from the Clinical Core of the Northwestern Cognitive Neurology and Alzheimer's Disease Center (CNADC). The diagnosis of MCI was based on research diagnostic criteria including the following: scores falling 2 or more standard deviations below the mean on neuropsychological tests within a battery used across the National Institute on Aging ADC programs (i.e., the Uniform Data Set [UDS]) [34], [35] and the absence of impairments of activities of daily living as corroborated by a study partner [36]. Specifically, we recruited aMCI participants, identified as only having impairment in the memory domain. Participants had to be capable of undergoing retinal imaging and those with ocular pathology such as glaucoma, macular degeneration, diabetic retinopathy, retinal detachment, ocular trauma, and extensive cataracts were excluded. Further exclusion criteria included neurologic disorders such as multiple sclerosis and Parkinson's. Whenever possible, reported medical history was verified in the electronic medical record (EMR) to ensure that participants' reported history was accurate. Cognitively normal control participants (N = 20) were also recruited from the CNADC, after undergoing the same neuropsychological battery as the MCI sample. These participants were matched by age (within 3 years), race, and sex to the aMCI sample. Control subjects had no abnormal test scores on the UDS battery and all had normal activities of daily living as reported by their study partners.
2.1.3. Ophthalmological assessments
Ophthalmological assessments included administration of the National Eye Institute Visual Function Questionnaire (VFQ-25). The VFQ-25 is a questionnaire that includes a 25-item survey to evaluate self-reported vision-targeted health status. Each score indicates a vision specific, health-related quality of life measure. Participants underwent protocol refraction and best-corrected visual acuity assessment on each eye. Visual acuity was then measured using retro-illuminated ETDRS charts at a testing distance of 3.2 m. In addition, we tested contrast sensitivity in each eye sequentially and both eyes together using the Pelli Robson chart at 1 m. Color vision was evaluated using the FM-15 L'anthony desaturated panel and intra-ocular pressure using Tonopen (Reichert Technologies, Buffalo, NY, USA).
2.1.4. Cognitive assessment
Extensive cognitive testing within a year of participation in the present study had been performed by the CNADC. Participants in the CNADC are examined at baseline and annually with the neuropsychological test battery of the UDS, supplemented with the Rey Auditory Verbal Learning Test (RAVLT), a measure of the ability to learn and retain a list of 15 unrelated words [37]. The UDS includes tests of learning and immediate and delayed episodic memory, language, processing speed, attention, and executive function. Participants also undergo a research neurological examination, provide a detailed medical and family history, and designate a study partner from whom information is derived about instrumental activities of daily living (iADL). In the current study, we noted participants' scores on RAVLT, immediate and delayed recall of a short story [Logical Memory from the WMS-R (LMI and LMII)], and part B of the Trail Making Test (TMT-B), a test of executive attention. For all cognitive exams except TMT-B, a higher score means better cognition. TMTB is timed and, therefore, completing the test more quickly, or a lower number, indicates better performance.
2.1.5. OCT imaging
Spectral domain OCT imaging was obtained with Spectralis HRA + OCT (Heidelberg Engineering, Heidelberg, Germany). “peripapillary” RNFL thickness and macular volume scans were performed. Dilation of each eye was performed before imaging.
2.1.6. Macular sublayer segmentation
For each macular volumetric scan, the macular sublayer thicknesses were extracted semiautomatically, as previously described using validated segmentation software, Duke Optical Coherence Tomography Retinal Analysis Program (DOCTRAP) [38]. Briefly, the software defined six retinal sublayers including GCL/IPL. Automated grading was followed by a two-grader quality-control procedure to further examine segmentation boundaries and perform any manual corrections, as previously described [39]. Sublayer thicknesses were automatically measured in each scan, and average macular sublayer thicknesses were calculated for each volumetric scan. OCT graders were masked to participant group assignment.
2.1.7. Statistical analysis
Statistical analysis was performed using the Statistical Analysis System, version 9.4 (SAS Institute, Raleigh, NC, USA). aMCI and control groups were compared regarding OCT thickness measures using repeated-measures analysis of variance accounting for layer and eye within person. Analysis of covariance (ANCOVA) was used to relate the thickness measures to the cognitive scores. Regression coefficients were calculated to identify the change in thickness measure per unit change in cognitive scores. Effect size was also calculated to determine if the small sample size was the main variable affecting results. ANCOVA was then used to adjust for hypertension and diabetes.
2.2. Meta-analysis
2.2.1. Key question
We conducted a meta-analysis of the world literature to determine if RNFL thinning is a consistent marker in subjects with MCI.
2.2.2. Search strategy
A computerized search of PubMed, Medline, Scopus, Google Scholar, Web of Science, and Cochrane Library was performed. Reference lists from reviews and studies were also manually searched. Keywords included mild cognitive impairment, MCI, optical coherence tomography, OCT, retinal nerve fiber layer thickness, “peripapillary” RNFL, and retinal thickness.
2.2.3. Study assessment and data extraction
Full-text articles were included if they met the following criteria: (1) the study was designed to compare RNFL thickness between MCI and control participants using OCT and included analysis of all quadrants of the RNFL (superior, temporal, nasal, and inferior quadrants); (2) the study actively excluded participants who had confounding ocular and neurologic diseases; (3) the study adjusted for age differences between MCI and controls; (4) the study performed rigorous cognitive examination of both MCI and control participants; and (5) the study had an MCI and control group with all OCT data available in the article. We were unable to limit our meta-analysis to aMCI because most studies did not distinguish this subgroup from other forms of MCI.
One investigator (BK) conducted the literature search and two investigators (BK and JS), masked to names of authors and journals, independently reviewed each of the identified manuscripts to rate their quality as good, fair, or poor based on the criteria specified previously. Discrepancies were resolved by adjudication of a third reviewer (AAF).
2.2.4. Statistical analysis
The meta-analysis was conducted following the Cochrane Collaboration guidelines and was analyzed using Comprehensive Meta-Analysis (Biostat, Englewood, NJ, USA) [40]. “peripapillary” RNFL thickness was extracted including the mean ± standard deviation from each article. The I2 statistic was calculated to determine heterogeneity among the tests [41]. The meta-analysis was performed using a random-effects model based on the I2 value, also per the Cochrane Collaboration guidelines. Effect size is reported as Hedges g given the small sample sizes [42]. Finally, Egger test for publication bias was calculated [43]. A P value <.05 was considered statistically significant.
3. Results
3.1. Experimental study
Of the 20 aMCI participants recruited, 3 were excluded: 2 because of an established diagnosis of glaucoma in the EMR and 1 because of macular degeneration discovered on OCT imaging. One eye of a study participant was excluded because of trauma in childhood. The remaining eligible participants were 17 aMCI subjects (33 eyes). Characteristics of the case-control groups are listed in Table 1. Although the mean TMT-B score for the aMCI group was worse than for controls, the overall value was within normal range for age and the difference between groups was not statistically significant. Thus, TMT-B was excluded from further analysis.
Table 1.
Participant demographics and cognitive characteristics
| Study group | aMCI (n = 17) | Matched controls (n = 17) | P value |
|---|---|---|---|
| Variables | |||
| Female | 13 | 13 | — |
| Age | |||
| 60–70 | 5 | 5 | — |
| 71–80 | 7 | 7 | — |
| 81–90 | 5 | 5 | — |
| Average | 74 | 74 | — |
| Race | |||
| African American | 5 | 5 | — |
| Caucasian | 12 | 12 | — |
| Hypertension∗ | 7/17 | 8/17 | — |
| Diabetes∗ | 6/17 | 3/17 | — |
| Average RAVLT (total = 15) | 5.0 ± 3.91 | 11.1 ± 2.87 | <.001 |
| Average LMI (total = 25) | 8.7 ± 3.12 | 16.3 ± 3.35 | <.001 |
| Average LMII (total = 25) | 7.3 ± 4.55 | 16.35 ± 4.50 | <.001 |
| Average TMT-B† | 106.6 ± 224.67 | 80.3 ± 34.95 | .07 |
| Average MMSE (total = 30) | 27 ± 3.72 | 29 ± 0.70 | .03 |
Abbreviations: aMCI, amnestic mild cognitive impairment; RAVLT, Rey Auditory Verbal Learning Test; LMI, logical memory test I or immediate recall; LMII, logical memory test II or delayed recall; TMT-B, Trail Making Test, part B; MMSE, Mini-Mental State Examination.
Subjects with retinopathy related to hypertension or diabetes were excluded.
TMT-B scores generally fell within normal limits for the age group studied.
RNFL thickness, macular sublayer thickness, and total macular thickness/volume comparisons between aMCI and controls are shown in Table 2. We found no statistically significant difference between aMCI and control groups in terms of RNFL thickness for all quadrants. Effect size was calculated, and the largest effect for RNFL thickness was 0.41, indicating that the small sample size alone does not account for the difference and that the groups truly are very similar. There was no significant difference between the two groups with respect to contrast sensitivity, visual acuity, color vision, VFQ-25, and IOP. ANCOVA adjustment for diabetes and hypertension did not alter the results.
Table 2.
OCT: RNFL and macular sublayer thickness results
| OCT measurement | aMCI∗ | Controls∗ | Paired t test P value |
|---|---|---|---|
| RNFL thickness (μm) | |||
| Total | |||
| Right eye | 91.8 ± 11 | 91.8 ± 11 | .99 |
| Left eye | 89.3 ± 15 | 90.2 ± 12 | .86 |
| Superior | |||
| Right eye | 104.8 ± 15 | 106.9 ± 16 | .66 |
| Left eye | 105.2 ± 23 | 105.4 ± 20 | .99 |
| Inferior | |||
| Right eye | 121.2 ± 19 | 120.4 ± 22 | .91 |
| Left eye | 118 ± 23 | 118.8 ± 18 | .90 |
| Nasal | |||
| Right eye | 76 ± 21 | 72.6 ± 17 | .61 |
| Left eye | 71.4 ± 18 | 68.9 ± 21 | .72 |
| Temporal | |||
| Right eye | 65.6 ± 17 | 67.4 ± 13 | .72 |
| Left eye | 62.5 ± 15 | 67.7 ± 17 | .32 |
| Macula volume (mm3) | |||
| Right eye | 8.14 ± 0.58 | 8.29 ± 0.56 | .51 |
| Left eye | 8.21 ± 0.51 | 8.28 ± 0.51 | .51 |
| Macula GC-IPL (μm) | |||
| Right eye | 385 ± 39 | 390 ± 46 | .74 |
| Left eye | 287 ± 38 | 388 ± 45 | .93 |
Abbreviations: OCT, optical coherence tomography; RNFL, retinal nerve fiber layer; aMCI, amnestic mild cognitive impairment; GC-IPL, ganglion cell layer and inner plexiform layer.
n = 16 for right eye and 17 for left eye.
Table 3 shows the regression coefficients (P values) for the relationships between cognitive scores and RNFL thickness in our aMCI participants. There was a statistically significant negative correlation between LMII and the RNFL superior and inferior quadrants and a significant negative correlation between RAVLT and the RNFL inferior quadrant. This suggests that thinner RNFL in these respective quadrants correlated with better cognitive scores.
Table 3.
Regression coefficients (P values) correlating “peripapillary” RNFL thickness to cognitive function in participants with amnestic mild cognitive impairment
| Cognitive test | RNFL quadrant P values |
|||
|---|---|---|---|---|
| Temporal | Nasal | Superior | Inferior | |
| LMI | 0.40 (.55) | 0.24 (.67) | −0.95 (.19) | −1.11 (.14) |
| LMII | −0.14 (.78) | 0.31 (.45) | −1.18 (.022)∗ | −1.35 (.012)∗ |
| RAVLT | −0.28 (.64) | 0.42 (.31) | −0.65 (.39) | −1.79 (.026)∗ |
Abbreviations: RNFL, retinal nerve fiber layer; LMI, logical memory test I or immediate recall; LMII, logical memory test II or delayed recall; RAVLT, Rey Auditory Verbal Learning Test.
Statistically significant P value <.05.
3.2. Meta-analysis
3.2.1. Studies included
The initial search yielded 71 hits, from which a final list of 12 relevant articles was identified for further review. Three articles were excluded because of lack of raw OCT data and two because of poor exclusion criteria. Finally, one article used the term “mild cognitive criteria” to refer to newly diagnosed DAT. The remaining six studies were selected for the meta-analysis based on the quality criteria as determined by the three reviewers.
Table 4 summarizes detailed demographic and OCT data for the final selected articles, which includes 161 MCI participants and 300 controls [18], [19], [20], [21], [22], [25]. In the last row, we have inserted data from the present study for comparison. Included studies were based in Spain, China, Israel, and Singapore. The quality of diagnosis was deemed fair because of lack of clear cognitive testing methodology or lack of adjustment for confounders.
Table 4.
Summary of “peripapillary” RNFL findings on optical coherence tomography in studies included in the meta-analysis and the present study
| Authors | Year | Location | # MCI | Mean age, MCI (±SD) | Average MMSE MCI | # Control | Mean age, control (±SD) | Grade | Total RNFL |
Superior |
Inferior |
Nasal |
Temporal |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MCI | Control | MCI | Control | MCI | Control | MCI | Control | MCI | Control | |||||||||
| Ascaso et al. | 2014 | Spain | 21 | 72.1 ± 8.7 | 19.3 | 41 | 72.9 ± 7.9 | Fair | 87.3 ± 7.22∗ | 102.7 ± 6.89∗ | 104.0 ± 15.74∗ | 128.2 ± 14.4∗ | 111.1 ± 19.0∗ | 132.7 ± 13.25∗ | 65.9 ± 17.6 | 75.9 ± 13.3 | 68.5 ± 16.5∗ | 74.9 ± 13.5∗ |
| Gao et al. | 2014 | China | 26 | 73.4 ± 1.5 | 25.8 | 21 | 72.1 ± 1.0 | Good | 92.38 ± 1.94 | 98.60 ± 1.67 | 112.12 ± 3.31 | 122.25 ± 2.95 | 123.87 ± 3.36 | 127.59 ± 2.72 | 68.54 ± 1.52 | 69.71 ± 1.55 | 66.56 ± 2.44∗ | 74.60 ± 2.11∗ |
| Kesler et al. | 2011 | Israel | 24 | 71.0 ± 10.0 | 28.1 | 24 | 70.9 ± 9.2 | Fair | 85.8 ± 10.0∗ | 94.3 ± 11.3∗ | 101.3 ± 15.2 | 110.0 ± 16.7 | 111.9 ± 16.1∗ | 127.0 ± 15.5∗ | 65.9 ± 15.1 | 76.4 ± 21.8 | 64.2 ± 13.9 | 67.8 ± 15.1 |
| Shen et al. | 2014 | China | 23 | 74.4 ± 3.2 | 22.2 | 52 | 74.1 ± 2.6 | Good | 82.6 ± 10.5 | 85.6 ± 10.2 | 101.8 ± 16.8 | 104.7 ± 15.4 | 104.5 ± 17.6 | 109.3 ± 21.3 | 61.5 ± 8.1 | 64.8 ± 8.4 | 62.7 ± 12.2 | 65.5 ± 10.1 |
| Liu et al. | 2015 | China | 26 | 70.2 ± 6.5 | — | 39 | 69.7 ± 7.8 | Fair | 95.4 ± 17.11 | 100.12 ± 15.0 | 115.14 ± 13.5∗ | 119.1 ± 15.3∗ | 120.23 ± 18.0 | 125.7 ± 11.2 | 74.8 ± 12.36 | 79.9 ± 12.9 | 63.8 ± 13.2 | 67.34 ± 15.3 |
| Cheung et al. | 2015 | Singapore | 41 | 70.4 ± 10.2 | — | 123 | 65.7 ± 3.8 | Fair | 87.3 ± 7.22 | 102.7 ± 6.89 | 104.0 ± 15.74 | 128.2 ± 14.4 | 111.1 ± 19.0 | 132.7 ± 13.25 | 65.9 ± 17.6 | 75.9 ± 13.3 | 68.5 ± 16.5 | 74.9 ± 13.5 |
| Knoll et al. | Present study | USA | 17 | 74.5 ± 8.9 | 27.3 | 17 | 74.8 ± 8.3 | Good | 90.2 ± 12.2 | 91.0 ± 10.5 | 106.8 ± 18.2 | 106.2 ± 18.8 | 120.0 ± 18.6 | 119.2 ± 17.4 | 75.3 ± 19.5 | 68.2 ± 21.6 | 65.1 ± 15.1 | 67.8 ± 16.2 |
Abbreviations: MCI, mild cognitive impairment; MMSE, Mini-Mental State Examination; RNFL, retinal nerve fiber layer; SD, standard deviation.
Study found significant difference between MCI and controls in this quadrant.
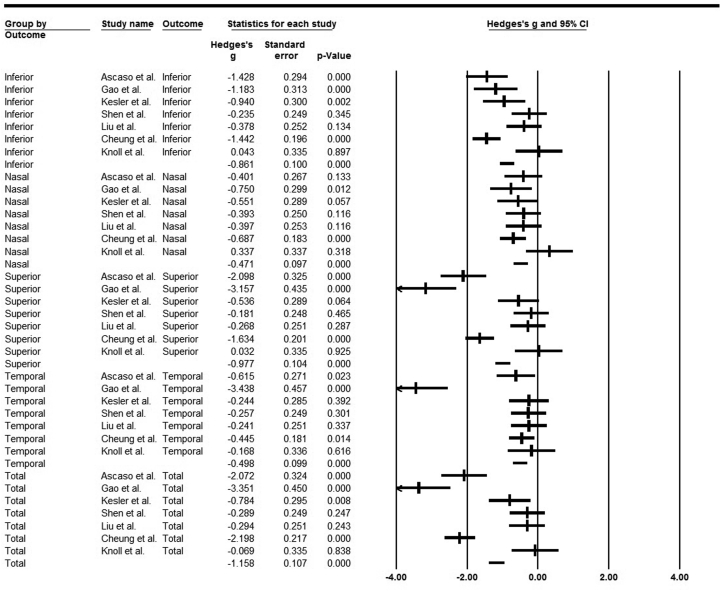
We first examined heterogeneity of RNFL thickness measurements in MCI and control subjects. The I2 value was 88.2%, which indicates high heterogeneity, and thus, a random-effects analysis was performed. Based on the small sample size and different imaging modalities used to measure the RNFL thickness, a Hedges g value was calculated. These values are shown in Table 5. The forest plots for this data are shown in Fig. 1. Finally, we conducted a publication bias analysis, and the Egger regression intercept was −2.67 (95% confidence interval from −7.35 to 2.00) with a P value of .25, indicating an unbiased study.
Table 5.
Hedges g values using random-effects model for “peripapillary” RNFL thickness
| RNFL thickness quadrant | Hedges g value | P value | Q value | P value | I2 |
|---|---|---|---|---|---|
| Total | −1.27 | .003 | 90.94 | <.001 | 93.40 |
| Superior | −1.09 | .004 | 77.33 | <.001 | 92.25 |
| Inferior | −0.80 | .001 | 30.89 | <.001 | 80.58 |
| Nasal | −0.45 | <.001 | 8.33 | .215 | 27.94 |
| Temporal | −0.70 | .014 | 45.38 | <.001 | 86.78 |
Abbreviation: RNFL, retinal nerve fiber layer.
Fig. 1.
Forest plots for retinal nerve fiber layer thickness (by quadrant) comparing participants with mild cognitive impairment with controls using Hedges g model.
4. Discussion
The major finding from this case-control study was an absent statistically significant difference in RNFL and macular sublayers comparing aMCI and matched cognitively healthy control participants. This finding was consistent with some previous studies but differed from others. Our findings suggest that in a well-characterized sample, where aMCI had MCI (average Mini-Mental State Examination [MMSE] = 27.3) and were carefully matched to controls, retinal thickness measured with OCT does not correlate with cognitive status, a finding supported by an RNFL effect size of 0.41 suggesting very similar populations, rather than low power of our study.
A secondary finding was an inverse relationship between “peripapillary” RNFL and test scores of two cognitive tests: the superior and inferior RNFL quadrants and delayed story recall (LMII) and thickness of the inferior RNFL quadrant and word-list learning test (RAVLT). An inverse relationship implies that with lower cognitive test scores, the RNFL is thicker. Although this appears paradoxical at first, a potential explanation could relate to pathologic gliosis preceding loss of neurons and ultimate decreased thickness, a pathologic finding that has been shown in other degenerative eye diseases [44]. In particular, the superior RNFL quadrant may be an ideal location to distinguish patients at risk for DAT because it would be a distinct location from the inferior quadrant, which is usually involved early on glaucoma patients, another age-related optic neuropathy [45]. Gliosis may also explain the lack of statistically significant difference in RNFL thickness between our aMCI participants and matched controls. Given that multiple studies have shown thinning in the retina of DAT patients, it is possible that gliosis occurs first in the disease process, leading to lack of difference or an initial paradoxical increase in RNFL thickness on OCT. Then, with disease progression, axonal degeneration and RNFL thinning proceed in DAT, at which point RNFL thinning can be discerned on OCT with statistical significance.
Further support for the gliosis hypothesis stems from histopathologic studies that show gliosis is an early marker of DAT pathology in the brain [28], [29]. In the eyes, gliosis has also been demonstrated in a rat model of glaucoma, an ocular condition also known to ultimately cause RNFL thinning [44], [45]. It is now hypothesized that in glaucoma, RNFL gliosis occurs first and is then followed by thinning that can be identified on OCT in later stages [46]. Unfortunately, OCT imaging of the RNFL does not reveal a unique signature for gliosis. With the availability of new modalities of retinal imaging, such as the adaptive optics scanning laser ophthalmoscope (AO-SLO), it is now possible to visualize the RNFL in greater detail because of the enhanced lateral resolution of these technologies [47], [48]. The inverse correlation between RNFL and cognitive function in aMCI subjects would suggest that gliosis could also be occurring in these eyes. We believe this finding is important, as it may actually explain the variability in the previous OCT reports and may partly explain the previous reports that failed to identify a difference between controls and aMCI. If the earliest change in the retina of aMCI subjects were gliosis of the inner retina and hence “thickening of the RNFL” based on our findings, this would necessitate a significantly changed approach for early detection of AD in the eye. Our work, and validation by other studies in different populations, could lead to a paradigm shift in the field.
This case-control study carries several major strengths that distinguish it from the previous reports. We included a strictly defined population of aMCI subjects, who are theoretically at the greatest risk of advancing on to DAT, subjects were carefully matched to healthy controls, and the entire study population underwent visual function tests by the same researcher. Furthermore, a board-certified ophthalmologist, retina specialist, carefully evaluated all the OCT images to ensure exclusion of subjects with confounding age-related ocular pathology. In addition, the cognitive tests performed in this study met the current standards for MCI diagnosis and were performed by trained professionals at the CNADC. Finally, we verified reported past medical history against the EMR, whenever possible. This additional verification allowed us to identify and exclude two participants with underlying glaucoma who would otherwise have been missed because they self-reported no history of ocular disease.
There are several limitations of our study. Because of the interactive nature of these tests, the researcher who performed the cognitive and visual function tests could not be masked to participant group. The small sample size could be a limitation; however, given the small effect size of RNFL, we believe the lack of significance likely represent true absence of difference between the two groups. Overall, the small sample size remains an important limitation in our study and others in this line of research, given the need to exclude glaucoma and other neurologic and age-related ocular diseases, to avoid confounding. Finally, in this study, we did not use brain imaging to rule out vascular pathology. Nevertheless, we do not believe this is a limitation of our study, given that current cognitive testing, such as that performed by Northwestern CNADC, is designed and validated to distinguish vascular type dementia from dementia of Alzheimer's type.
With these study size limitations in mind, we performed the meta-analysis, which showed that MCI subjects (not limited to aMCI) had statistically significant thinning of the RNFL that affected all quadrants of the optic nerve, compared with cognitively intact control population. Overall, by combining these relatively small studies including our own, we identified evidence that ocular involvement revealed on OCT is likely present at this early stage. Strengths of the meta-analysis include rigorous exclusion and inclusion criteria and quality analysis of each article. Our findings are in line with a recent meta-analysis in subjects with DAT, which showed reduced RNFL thickness compared with cognitively healthy controls [14].
In examining the current world literature, we identified high variability among studies with regard to methodology as a significant limitation. Significantly, the exclusion criteria for confounding diseases varied from study to study. For example, many studies did not state whether an ophthalmologist was involved to ensure exclusion of confounding ocular pathology, and it was not always stated how subjects were screened for confounding diseases. Furthermore, many studies compared the mean ages of their MCI and control groups but did not adjust for age or race in the final analysis. Additionally, many studies relied only on the MMSE to characterize cognitively normal control subjects, which may not be ideal as shown by a recent review that concluded that MMSE alone is not sufficient to distinguish participants with MCI from controls [49]. We were also unable to compare the OCT data with cognitive scores in other studies because there was great deal of inconsistency in reporting cognitive data. Finally, although our case-control study focused on aMCI, most previous studies did not specify the specific axis of cognitive impairment in their MCI population, likely including a widely heterogeneous MCI population.
In summary, our case-control study revealed that OCT findings may be subtle in a well-defined subpopulation of aMCI and that “peripapillary” RNFL may be inversely related to cognitive tests, suggesting a potential role for gliosis in this population. The meta-analysis suggested that the RNFL is statistically significantly thinner in subjects with MCI, compared with cognitively healthy controls. Unfortunately, most previous studies have used inconsistent methodology and had variable results, which highlights the need to initiate large population prospective standardized OCT studies. Ultimately, the goal is to identify an ocular imaging modality that is capable of identifying aMCI patients who are at the highest risk of developing DAT. We foresee that a multidisciplinary, longitudinal approach with stringent cognitive testing, including high-resolution technologies such as AO-SLO, will be required to identify and perhaps predict those individuals who are highest risk for DAT, so that they can be targeted for preventive therapies as these become available.
Research in context.
-
1.
Systematic review: Ocular involvement in mild cognitive impairment (MCI) remains a subject of controversy. Previous literature suffers from lack of standardized protocols to define MCI, exclude, and/or adjust for confounders. To address these deficiencies, we performed a rigorous case-control study focusing on amnestic MCI (aMCI) participants.
-
2.
Interpretation: Our study found no statistically significant difference in optical coherence tomography (OCT) between aMCI subjects and controls, but uncovered that OCT thickness was significantly (inversely) related to cognitive scores. The meta-analysis showed statistically significant thinning in MCI subjects compared with controls.
-
3.
Future direction: Overall, ocular involvement in MCI may be more complex than previously thought. With this in mind, we believe that longitudinal OCT studies are needed to explore whether OCT can predict aMCI subjects at risk for Alzheimer's disease. Based on the inverse relationship found, we suggest future studies incorporate new retinal imaging modalities that are capable of examining the complex retinal pathology.
Acknowledgments
The authors would like to acknowledge Zach Seeskin, graduate student in statistics at the Institute for Policy Research at northwestern, who helped with initial steps of designing the meta-analysis and Leon Kwak who helped with the sublayer macula analysis at Duke. This study was supported by the National Institutes of Health grant NIA-AG13584 (CNADC), Eleanor Wood-Prince Grants: A Project of The Woman's Board of NMH (AAF), the Illinois Society for the Prevention of Blindness grant SP0029632 (BK), and the Research to Prevent Blindness in New York (Department of Ophthalmology).
References
- 1.Alzheimer A. A contribution concerning the pathological anatomy of mental disturbances in old age, 1899. Alzheimer Dis Assoc Disord. 1991;5:69–70. [PubMed] [Google Scholar]
- 2.Albert M.S., DeKosky S.T., Dickson D., Dubois B., Feldman H.H., Fox N.C. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:270–279. doi: 10.1016/j.jalz.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McKhann G.M., Knopman D.S., Chertkow H., Hyman B.T., Jack C.R., Jr., Kawas C.H. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:263–269. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hinton D.R., Sadun A.A., Blanks J.C., Miller C.A. Optic-nerve degeneration in Alzheimer's disease. N Engl J Med. 1986;315:485–487. doi: 10.1056/NEJM198608213150804. [DOI] [PubMed] [Google Scholar]
- 5.Javaid F.Z., Brenton J., Guo L., Cordeiro M.F. Visual and Ocular Manifestations of Alzheimer's Disease and Their Use as Biomarkers for Diagnosis and Progression. Front Neurol. 2016;7:55. doi: 10.3389/fneur.2016.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bussel I.I., Wollstein G., Schuman J.S. OCT for glaucoma diagnosis, screening and detection of glaucoma progression. Br J Ophthalmol. 2014;98 Suppl 2:ii15–ii19. doi: 10.1136/bjophthalmol-2013-304326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang D., Swanson E.A., Lin C.P., Schuman J.S., Stinson W.G., Chang W. Optical coherence tomography. Science. 1991;254:1178–1181. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Inzelberg R., Ramirez J.A., Nisipeanu P., Ophir A. Retinal nerve fiber layer thinning in Parkinson disease. Vision Res. 2004;44:2793–2797. doi: 10.1016/j.visres.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 9.Kirbas S., Turkyilmaz K., Tufekci A., Durmus M. Retinal nerve fiber layer thickness in Parkinson disease. J Neuroophthalmol. 2013;33:62–65. doi: 10.1097/WNO.0b013e3182701745. [DOI] [PubMed] [Google Scholar]
- 10.Hassenstein A., Meyer C.H. Clinical use and research applications of Heidelberg retinal angiography and spectral-domain optical coherence tomography—a review. Clin Experiment Ophthalmol. 2009;37:130–143. doi: 10.1111/j.1442-9071.2009.02017.x. [DOI] [PubMed] [Google Scholar]
- 11.Ratchford J.N., Quigg M.E., Conger A., Frohman T., Frohman E., Balcer L.J. Optical coherence tomography helps differentiate neuromyelitis optica and MS optic neuropathies. Neurology. 2009;73:302–308. doi: 10.1212/WNL.0b013e3181af78b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adhi M., Duker J.S. Optical coherence tomography—current and future applications. Curr Opin Ophthalmol. 2013;24:213–221. doi: 10.1097/ICU.0b013e32835f8bf8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.He X.F., Liu Y.T., Peng C., Zhang F., Zhuang S., Zhang J.S. Optical coherence tomography assessed retinal nerve fiber layer thickness in patients with Alzheimer's disease: a meta-analysis. Int J Ophthalmol. 2012;5:401–405. doi: 10.3980/j.issn.2222-3959.2012.03.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coppola G., Di Renzo A., Ziccardi L., Martelli F., Fadda A., Manni G. Optical Coherence Tomography in Alzheimer's Disease: A Meta-Analysis. PLoS One. 2015;10:e0134750. doi: 10.1371/journal.pone.0134750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Becker R.E., Greig N.H., Giacobini E. Why do so many drugs for Alzheimer's disease fail in development? Time for new methods and new practices? J Alzheimers Dis. 2008;15:303–325. doi: 10.3233/jad-2008-15213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Petersen R.C., Doody R., Kurz A., Mohs R.C., Morris J.C., Rabins P.V. Current concepts in mild cognitive impairment. Arch Neurol. 2001;58:1985–1992. doi: 10.1001/archneur.58.12.1985. [DOI] [PubMed] [Google Scholar]
- 17.Akar G., Gozke E., Agirman Y., Kurna S.A. Retinal nerve fiber layer thickness in cases with mild cognitive impairment and Alzheimer-type dementia. Biomed Res. 2014;25:597–602. [Google Scholar]
- 18.Ascaso F.J., Cruz N., Modrego P.J., Lopez-Anton R., Santabarbara J., Pascual L.F. Retinal alterations in mild cognitive impairment and Alzheimer's disease: an optical coherence tomography study. J Neurol. 2014;261:1522–1530. doi: 10.1007/s00415-014-7374-z. [DOI] [PubMed] [Google Scholar]
- 19.Cheung C.Y., Ong Y.T., Hilal S., Ikram M.K., Low S., Ong Y.L. Retinal ganglion cell analysis using high-definition optical coherence tomography in patients with mild cognitive impairment and Alzheimer's disease. J Alzheimers Dis. 2015;45:45–56. doi: 10.3233/JAD-141659. [DOI] [PubMed] [Google Scholar]
- 20.Gao L., Liu Y., Li X., Bai Q., Liu P. Abnormal retinal nerve fiber layer thickness and macula lutea in patients with mild cognitive impairment and Alzheimer's disease. Arch Gerontol Geriatr. 2015;60:162–167. doi: 10.1016/j.archger.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 21.Kesler A., Vakhapova V., Korczyn A.D., Naftaliev E., Neudorfer M. Retinal thickness in patients with mild cognitive impairment and Alzheimer's disease. Clin Neurol Neurosurg. 2011;113:523–526. doi: 10.1016/j.clineuro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 22.Liu D., Zhang L., Li Z., Zhang X., Wu Y., Yang H. Thinner changes of the retinal nerve fiber layer in patients with mild cognitive impairment and Alzheimer's disease. BMC Neurol. 2015;15:14. doi: 10.1186/s12883-015-0268-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oktem E.O., Derle E., Kibaroglu S., Oktem C., Akkoyun I., Can U. The relationship between the degree of cognitive impairment and retinal nerve fiber layer thickness. Neurol Sci. 2015;36:1141–1146. doi: 10.1007/s10072-014-2055-3. [DOI] [PubMed] [Google Scholar]
- 24.Paquet C., Boissonnot M., Roger F., Dighiero P., Gil R., Hugon J. Abnormal retinal thickness in patients with mild cognitive impairment and Alzheimer's disease. Neurosci Lett. 2007;420:97–99. doi: 10.1016/j.neulet.2007.02.090. [DOI] [PubMed] [Google Scholar]
- 25.Shen Y., Liu L., Cheng Y., Feng W., Shi Z., Zhu Y. Retinal nerve fiber layer thickness is associated with episodic memory deficit in mild cognitive impairment patients. Curr Alzheimer Res. 2014;11:259–266. doi: 10.2174/1567205011666140131114418. [DOI] [PubMed] [Google Scholar]
- 26.Shi Z., Wu Y., Wang M., Cao J., Feng W., Cheng Y. Greater attenuation of retinal nerve fiber layer thickness in Alzheimer's disease patients. J Alzheimers Dis. 2014;40:277–283. doi: 10.3233/JAD-131898. [DOI] [PubMed] [Google Scholar]
- 27.Ingelsson M., Fukumoto H., Newell K.L., Growdon J.H., Hedley-Whyte E.T., Frosch M.P. Early Abeta accumulation and progressive synaptic loss, gliosis, and tangle formation in AD brain. Neurology. 2004;62:925–931. doi: 10.1212/01.wnl.0000115115.98960.37. [DOI] [PubMed] [Google Scholar]
- 28.Mandybur T.I. Cerebral amyloid angiopathy and astrocytic gliosis in Alzheimer's disease. Acta Neuropathol. 1989;78:329–331. doi: 10.1007/BF00687764. [DOI] [PubMed] [Google Scholar]
- 29.Bates K.A., Fonte J., Robertson T.A., Martins R.N., Harvey A.R. Chronic gliosis triggers Alzheimer's disease-like processing of amyloid precursor protein. Neuroscience. 2002;113:785–796. doi: 10.1016/s0306-4522(02)00230-0. [DOI] [PubMed] [Google Scholar]
- 30.Scuderi C., Stecca C., Bronzuoli M.R., Rotili D., Valente S., Mai A. Sirtuin modulators control reactive gliosis in an in vitro model of Alzheimer's disease. Front Pharmacol. 2014;5:89. doi: 10.3389/fphar.2014.00089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Craft J.M., Watterson D.M., Van Eldik L.J. Human amyloid beta-induced neuroinflammation is an early event in neurodegeneration. Glia. 2006;53:484–490. doi: 10.1002/glia.20306. [DOI] [PubMed] [Google Scholar]
- 32.Kashani A.H., Zimmer-Galler I.E., Shah S.M., Dustin L., Do D.V., Eliott D. Retinal thickness analysis by race, gender, and age using Stratus OCT. Am J Ophthalmol. 2010;149:496–502.e1. doi: 10.1016/j.ajo.2009.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alasil T., Wang K., Keane P.A., Lee H., Baniasadi N., de Boer J.F. Analysis of normal retinal nerve fiber layer thickness by age, sex, and race using spectral domain optical coherence tomography. J Glaucoma. 2013;22:532–541. doi: 10.1097/IJG.0b013e318255bb4a. [DOI] [PubMed] [Google Scholar]
- 34.Morris J.C., Weintraub S., Chui H.C., Cummings J., Decarli C., Ferris S. The Uniform Data Set (UDS): clinical and cognitive variables and descriptive data from Alzheimer Disease Centers. Alzheimer Dis Assoc Disord. 2006;20:210–216. doi: 10.1097/01.wad.0000213865.09806.92. [DOI] [PubMed] [Google Scholar]
- 35.Weintraub S., Salmon D., Mercaldo N., Ferris S., Graff-Radford N.R., Chui H. The Alzheimer's Disease Centers' Uniform Data Set (UDS): the neuropsychologic test battery. Alzheimer Dis Assoc Disord. 2009;23:91–101. doi: 10.1097/WAD.0b013e318191c7dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gold D.A. An examination of instrumental activities of daily living assessment in older adults and mild cognitive impairment. J Clin Exp Neuropsychol. 2012;34:11–34. doi: 10.1080/13803395.2011.614598. [DOI] [PubMed] [Google Scholar]
- 37.Estevez-Gonzalez A., Kulisevsky J., Boltes A., Otermin P., Garcia-Sanchez C. Rey verbal learning test is a useful tool for differential diagnosis in the preclinical phase of Alzheimer's disease: comparison with mild cognitive impairment and normal aging. Int J Geriatr Psychiatry. 2003;18:1021–1028. doi: 10.1002/gps.1010. [DOI] [PubMed] [Google Scholar]
- 38.Chiu S.J., Li X.T., Nicholas P., Toth C.A., Izatt J.A., Farsi S. Automatic segmentation of seven retinal layers in SDOCT images congruent with expert manual segmentation. Opt Express. 2010;18:19413–19428. doi: 10.1364/OE.18.019413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boynton G.E., Stem M.S., Kwark L., Jackson G.R., Farsiu S., Gardner T.W. Multimodal characterization of proliferative diabetic retinopathy reveals alterations in outer retinal function and structure. Ophthalmology. 2015;122:957–967. doi: 10.1016/j.ophtha.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Higgins J.P., Altman D.G., Gotzsche P.C., Juni P., Moher D., Oxman A.D. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 42.Hedges L., Olkin I. Florida Academic Press; Orlando: 1985. Statistical methods for meta-analysis. [Google Scholar]
- 43.Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen M.F., Chui T.Y., Alhadeff P., Rosen R.B., Ritch R., Dubra A. Adaptive optics imaging of healthy and abnormal regions of retinal nerve fiber bundles of patients with glaucoma. Invest Ophthalmol Vis Sci. 2015;56:674–681. doi: 10.1167/iovs.14-15936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sihota R., Sony P., Gupta V., Dada T., Singh R. Diagnostic capability of optical coherence tomography in evaluating the degree of glaucomatous retinal nerve fiber damage. Invest Ophthalmol Vis Sci. 2006;47:2006–2010. doi: 10.1167/iovs.05-1102. [DOI] [PubMed] [Google Scholar]
- 46.Inman D.M., Horner P.J. Reactive nonproliferative gliosis predominates in a chronic mouse model of glaucoma. Glia. 2007;55:942–953. doi: 10.1002/glia.20516. [DOI] [PubMed] [Google Scholar]
- 47.Scoles D., Higgins B.P., Cooper R.F., Dubis A.M., Summerfelt P., Weinberg D.V. Microscopic inner retinal hyper-reflective phenotypes in retinal and neurologic disease. Invest Ophthalmol Vis Sci. 2014;55:4015–4029. doi: 10.1167/iovs.14-14668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liang J., Williams D.R., Miller D.T. Supernormal vision and high-resolution retinal imaging through adaptive optics. J Opt Soc Am A Opt Image Sci Vis. 1997;14:2884–2892. doi: 10.1364/josaa.14.002884. [DOI] [PubMed] [Google Scholar]
- 49.Mitchell A.J. A meta-analysis of the accuracy of the mini-mental state examination in the detection of dementia and mild cognitive impairment. J Psychiatr Res. 2009;43:411–431. doi: 10.1016/j.jpsychires.2008.04.014. [DOI] [PubMed] [Google Scholar]