Abstract
Introduction: Medical undergraduates are heavily burdened by their curriculum. The females, in addition, suffer from vivid affective or somatic premenstrual syndrome (PMS) symptoms such as bloating, mastalgia, insomnia, fatigue, mood swings, irritability, and depression. The present study was proposed to attenuate the symptoms of PMS by simple lifestyle measures like yoga and/or oral calcium.
Methods: 65 medical female students (18-22 years) with a regular menstrual cycle were asked to self-rate their symptoms, along with their severity, in a validated questionnaire for two consecutive menstrual cycles. Fifty-eight students were found to have PMS. Twenty girls were given yoga training (45 minutes daily, five days a week, for three months). Another group of 20 was given oral tablets of calcium carbonate daily (500 mg, for three months) and rest 18 girl served as control group. Data were analyzed by SPSS ver.13 software.
Results: The yoga and calcium groups showed a significant decrease in number and severity of premenstrual symptoms whereas in the control group there was not the significant difference.
Conclusion: Encouraging a regular practice of yoga or taking a tablet of calcium daily in the medical schools can decrease the symptoms of premenstrual syndrome.
Keywords: Premenstrual syndrome, Yoga, Relaxation, Calcium
Introduction
Premenstrual syndrome (PMS), a common cyclic disorder of young and middle-aged women, is characterized by physical, emotional and behavioral symptoms such as bloating, mastalgia, insomnia, fatigue, mood swings, irritability, and depression, that consistently occur during the luteal phase of the menstrual cycle; disappearing within a few days of the onset of menstruation.1
Although evidence for a hormonal abnormality has not been established, the symptoms of the premenopausal disorders are related to ovarian hormones. The progesterone metabolites may bind to a neurosteroid binding site on the membrane of the neurotransmitters.2
Prevalence of PMS is difficult to establish because of its variable clinical manifestations and interpretations. Nevertheless, a general consensus based on the questionnaire data is that 80%-95% of the female population admit to recurrent premenstrual symptoms, of which 5% suffer from symptoms severe enough to disrupt their lives.3
Since the symptoms are diverse, there is a wide array of the theories proposed and the approaches offered to manage PMS. The milder cases that constitute the major group may respond well to non-pharmacological approaches like counseling, stress management, complementary approaches like acupuncture, relaxation techniques, yoga, and consumption of micronutrients like calcium, magnesium, zinc etc. On the other hand, some cases can only be managed by drugs like serotonergic antidepressants and selective serotonin reuptake inhibitors are the agents that constitute well-established, highly effective and first-line pharmacologic therapy.4
Stress appears to be one of the accepted causes of premenstrual syndrome. Thus, stress relaxation techniques like yoga can be of reasonable value. Properly performed yogasanas are associated with not only relaxation of the related muscles as shown by EMG changes, but also are associated with relaxation of mind and body by increasing parasympathetic activity. Regular elicitation of relaxation response results in decreased norepinephrine sensitivity and hence decrease in PMS symptoms like irritability and anxiety.5,6
Literature states that women with mild to moderate luteal phase symptomatology have some underlying calcium dysregulation7with a secondary hyperparathyroidism and vitamin D deficiency.8 There is evidence that this calcium deficiency is unmasked with the rise in ovarian steroid hormone levels during the menstrual cycle.8,9
Medical Undergraduates are heavily burdened by their packed curriculum. The females, in addition, suffer from affective or somatic premenstrual syndrome (PMS) symptoms that adversely affect their quality of life. The present study was thus, proposed to attenuate the symptoms of PMS by practicing yoga and oral calcium administration in medical undergraduates.
Materials and methods
This qusi-experimental study was conducted on 78 young female medical students of age group 18-22 years from JLN Medical College, Ajmer and Rajasthan, India. In each batch of 100 medical undergraduates, there were around 30-35 girls. Amongst all the girls, 78 volunteered for the study.
We selected healthy females with a menstrual cycle ranging from 21-35 days and not varying more than 4 days. The females having a past or present history of some psychiatric illness, prolonged medication, chronic backaches or usage of oral contraceptives were excluded from the study.
Sixty-five females out of 78 volunteers were recruited for the study. To sensitize them to the study, they were given a lecture on the physiology of normal menstrual cycle; the hormonal and endocrinal changes during different phases of the menstrual cycle and premenstrual syndrome.
All the subjects were required to record the number of symptoms, along with their severity, in a predesigned, validated questionnaire, prospectively for two consecutive menstrual cycles. The questionnaire was designed on the diagnostic criteria for the diagnosis of PMS given by American College of Obstetricians and Gynaecologists (ACOG). Symptoms must appear in three consecutive menstrual cycles:
The questionnaire included a list of somatic symptoms such as breast tenderness, abdominal bloating, headache and swelling of extremities. The affective symptoms listed were depression, angry outbursts, irritability, anxiety, confusion, and social withdrawal.10
The presence of at least one somatic and one affective listed symptoms occurring from five days before the menstrual phase and relieving within 4 days of the onset of menstruation were the diagnostic criteria of PMS. The severity of the symptoms was assessed by self-rating, the number of days of discomfort & whether any medication was taken for relief of the symptoms.10
Fifty-eight subjects were found to have PMS. After recording weight, pulse, BP, they were divided into three groups. One group of 20 girls who volunteered for yoga, constituted yoga group; another group of 20 chose to take oral tablets of calcium carbonate. Rest 18, who showed their unwillingness for yoga or oral calcium administration, served as controls.
The yoga group underwent yoga training, one hour daily, five days a week for a period of three months under the supervision of an expert and trained instructor. The plan was tailored by a yoga instructor of the institute. It was a general yoga plan for all age groups; not specific only for PMS group. The schedule included “OM”) is a mantra or vibration coming from Hinduism and yoga chanting (; various yogasanas in standing, sitting and lying down positions; pranayama and bhramari gunjan. The session was concluded with Shavasana.11
Twenty girls that constituted the calcium group, were given 500 mg of calcium carbonate orally, for a period of 3 months. The students were made to take calcium tablets in front of the researcher, to ensure adherence to the dosage.
The control group of 18 subjects was neither given yoga training, nor oral calcium. After 3 months, the assessment of the symptoms & severity of PMS was again done by the same questionnaire.
We received the approval from the institutional ethical committee of JLN Medical College, Ajmer for conducting the study. This study was done as a part of MD Physiology Thesis. We were supposed to present our work before a committee of members and were asked to make amendments, if any, during that time.
The study was hence conducted and thesis approved by permission of the members of the instituteAlso, a written informed consent was taken from all the participants, after clearly explaining them the purpose of the study.
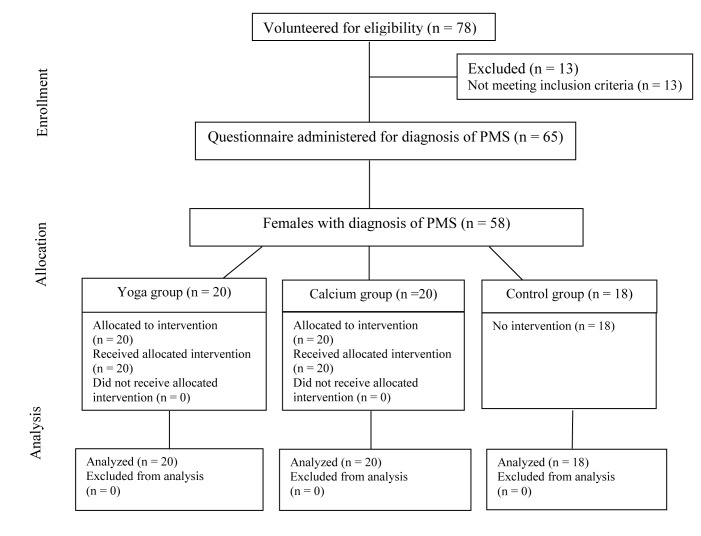
Flowchart of the study showed as figure 1.
Figure 1.
Flowchart of the study
Results
Fifty eight medical undergraduates with a mean age of 19.4 (1.07) years participated in the study. The mean weight of control group was 51.2 kg at the beginning which declined to 51 kg at the end of the study (P>0.05). In calcium group, the mean weight was 53.9 kg and 52 kg at the commencement and completion of the study, respectively (P<0.05).
The yoga group showed a maximal decline in weight from mean weight of 48.8 kg at the start and 46.6 kg at the end of three months of yoga training (P< 0.01).
The effect of interventions on the pulse rate of all the three groups is shown in Table 1. The result showed that both systolic and diastolic BP in all the three groups was not significantly different (P > 0.05).
Table 1. The effect of interventions on mean pulse rate (per min) of three groups.
| Group | Mean (SD) | Mean (SD) | P |
| Before | After 3 months | ||
| Control | 81.9 (5.0) | 79.7 (5.4) | 0.1006 |
| Yoga | 82.05 (6.1) | 79.2 (5.4) | 0.0068 |
| Calcium | 80.05 (8.0) | 78.8 (5.03) | 0.4666 |
The number of symptoms in yoga ranged from 3-12 prior to the commencement of the study that declined to 1-7 after yoga training (P<0.05). Eighteen out of 20 (90%) subjects also reported a decrease in the severity of the existing symptoms (P<0.05).
Eleven out of 20 subjects (55%) in calcium group showed a decline in the severity of symptoms. The number of symptoms declined from a mean value of 5.3 at the beginning of the study to 4.3 at the end of intervention (P< 0.05).
In the control group, there was no significant changes in the number and severity of symptoms. 38.89% of subjects showed a decrease in the symptoms, while the severity increased in 33% (P> 0.05).
The mean number of PMS symptoms in different groups is shown in Figure 2.
Figure 2.
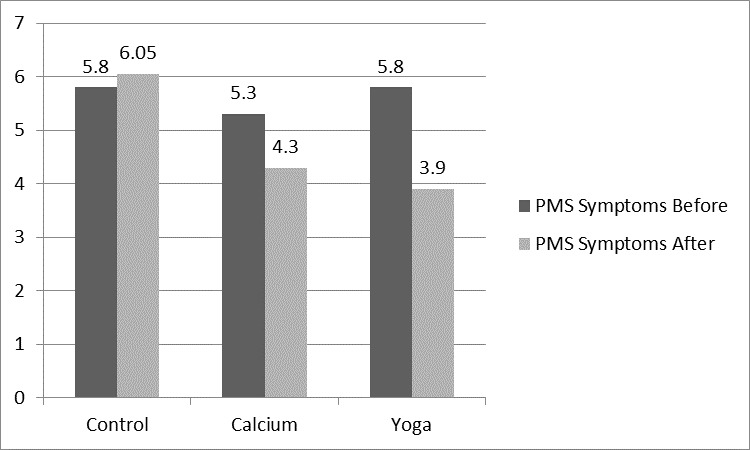
Mean number of PMS symptoms in different groups
On comparing the effects of the yoga and calcium groups, a Kruskal-Wallis test showed that there was a statistically significant decrease in PMS symptoms between these groups (χ2 = 10.654, P = 0.004).
Discussion
The premenstrual syndrome is a physioclinical entity, afflicting a large segment of the female population of reproductive age group, severely hampering their lifestyle and efficiencies.2
The precise etiology of this multifactorial, psychoneuroendocrinal disorder remains unclear but lifestyle, nutrition, and general health considerations seem to be important issues in the management of menstrual symptoms. Severe intensity of symptoms is seen associated with young age or students, lower education, unemployment, smoking, sedentary work, poor health, stress, and dysmenorrhea.12In the present study, a significant reduction in weight in calcium group (P<0.05) and yoga group was seen. A decrease in water retention and weight was seen in women fed high calcium diet in a study.13 Yoga is known to reduce weight by burning calories, boosting metabolism and also by improving thyroid functions.14,15
A significant reduction in pulse rate was found in the yoga group (P<0.05). A decline in heart rate after yogic exercises was reported by Telles et al.,16Literature states that there occurs a decrease in noradrenergic receptor sensitivity by yoga.5
There was no significant change in the BP in none of the three groups. Probably our samples was a group of healthy young females whom none of them had hypertension.
However, we found a highly significant reduction in the number of symptoms of PMS in the yoga group. Prior studies have reported that relaxation techniques like 61-PR which is a type of hatha yoga reduces the stress among women with PMS.17 Wu et al., performed a study to evaluate the efficacy of yoga in PMS. It was revealed that the alpha brain wave percentage was higher immediately after yoga exercise in the PMS group. This suggests that the participants felt more relaxed or were in a more peaceful mental condition after yoga exercise.18,19
To evaluate the strength of evidence for treatments for premenstrual syndrome, Sue Douglas performed an advanced MEDLINE search from January 1990 to December 2001.
The Cochrane Library and personal contacts were also used. The author concluded that calcium carbonate should be recommended as first-line therapy for women with mild-to-moderate PMS.20 There is evidence that a daily intake of 1,000 mg of calcium in women with premenstrual syndrome have decreased 61% of their physical and 62% of psychiatric symptoms.9 There is scientific evidence supporting cyclic fluctuations of calcium and vitamin D during the menstrual cycle that may help explain some features of PMS like depression, anxiety and the dysphoric states.8 Calcium and vitamin D may influence the development of PMS through their relationship to endogenous estrogens. Calcium, parathyroid hormone, and vitamin D levels have been observed to fluctuate across the menstrual cycle in response to changes in estradiol at ovulation and during the luteal phase in several studies.8,21,12 Buchanan et al., concluded that endogenous estrogen elevation promotes the formation of 1,25 (OH) 2D from 25 (OH) D and that it may reciprocally inhibit synthesis of 24,25 (OH) 2D. Thus, Calcium supplementation is a highly effective method to relieve symptoms of PMS.22
At the end of the study, students, motivated & encouraged with the results of intervention. They stated that they will include yoga or calcium as a lifestyle measure regularly. However, we didn’t follow the participants regarding adherence to this change.
The limitations of the present study are its small sample size and non-randomized allocation of the participants to various groups.23
Conclusion
According to the result, yoga offers a natural and effective way to alleviate PMS symptoms and serves as an alternative to painkillers and hormonal supplements.
Besides stress reduction, it also provides a moderate degree of exercise or toning to the body and hence can be adopted as a healthy lifestyle adjunct. Calcium is also relatively inexpensive, simple, safe, and effective approach to alleviate the symptoms of PMS and is also important in preventing osteoporosis. Since the decrease in number and severity of symptoms was more in yoga than calcium group, yoga seems to be more effective than calcium supplementation in relieving PMS symptoms.
Physical distress is known to cause absenteeism from work, hence, it would be reasonable to state that if a girl is free from her monthly distress, her well-being and work efficiency would increase. Thus encouraging a regular practice of yoga or taking a tablet of calcium daily in the medical schools can improve psychological well-being and work efficiency of students.
Acknowledgments
The author would like to appreciate the contribution of all the students who participated in the study.
Ethical issues
None to be declared.
Conflict of interest
The authors declare no conflict of interest in this study.
Please cite this paper Bharati M. Comparing the effects of yoga & oral calcium administration in alleviating symptoms of premenstrual syndrome in medical undergraduates. J Caring Sci 2016; 5 (3): 179-85. doi: 10.15171/jcs.2016.019.
References
- 1.Ryu A, Kim TH. Premenstrual syndrome: a mini review. Maturitas. 2015;82(4):436–40. doi: 10.1016/j.maturitas.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 2.Imai A, Ichigo S, Matsunami K, Takagi H. Premenstrual syndrome: management and pathophysiology. Clin Exp Obstet Gynecol. 2015;42(2):123–8. [PubMed] [Google Scholar]
- 3. Kwan I, Onwude JL. Premenstrual syndrome. BMJ Clin Evid 2009. Available from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2907788/. [PubMed]
- 4.Smith MA, Youngkin EQ. Managing the premenstrual syndrome. Clin Pharm. 1986;5(10):788–97. [PubMed] [Google Scholar]
- 5.Goodale IL, Domar AD, Benson H. Alleviation of premenstrual syndrome symptoms with the relaxation response. Obstet Gynecol. 1990;75(4):649–55. [PubMed] [Google Scholar]
- 6.Sharma B, Misra R, Singh K, Sharma R, Archana null. Comparative study of the effect of anuloma-viloma (pranayama) and yogic asanas in premenstrual syndrome. Indian J Physiol Pharmacol. 2013;57(4):384–9. [PubMed] [Google Scholar]
- 7.Saeedian Kia A, Amani R, Cheraghian B. The Association between the Risk of Premenstrual Syndrome and Vitamin D, Calcium, and Magnesium Status among University Students: A Case-Control Study. Health Promot Perspect. 2015;25(3):225–30. doi: 10.15171/hpp.2015.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thys-Jacobs S. Micronutrients and the premenstrual syndrome: the case for calcium. J Am Coll Nutr. 2000;19(2):220–7. doi: 10.1080/07315724.2000.10718920. [DOI] [PubMed] [Google Scholar]
- 9.Akhlaghi F, Hamedi A, Javadi Z, Hosseinipoor F. Effects of calcium supplementation on premenstrual syndrome. Razi Journal of Medical Sciences. 2004;10(37):669–75. [Google Scholar]
- 10.Yonkers KA, O’Brien PMS, Eriksson E. Premenstrual syndrome. Lancet. 2008;371(9619):1200–10. doi: 10.1016/S0140-6736(08)60527-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rakhshaee Z. Effect of three yoga poses (cobra, cat and fish poses) in women with primary dysmenorrhea: a randomized clinical trial. J Pediatr Adolesc Gynecol. 2011;24(4):192–6. doi: 10.1016/j.jpag.2011.01.059. [DOI] [PubMed] [Google Scholar]
- 12.Bianco V, Cestari AM, Casati D, Cipriani S, Radici G, Valente I. Premenstrual syndrome and beyond: lifestyle, nutrition, and personal facts. Minerva Ginecol. 2014;66(4):365–75. [PubMed] [Google Scholar]
- 13.Penland JG, Johnson PE. Dietary calcium and manganese effects on menstrual cycle symptoms. Am J Obstet Gynecol. 1993;168(5):1417–23. doi: 10.1016/S0002-9378(11)90775-3. [DOI] [PubMed] [Google Scholar]
- 14.Udupa KN, Singh RH, Settiwar RM. Physiological and biochemical studies on the effect of yogic and certain other exercises. Indian J Med Res. 1975;63(4):620–4. [PubMed] [Google Scholar]
- 15.Kristal AR, Littman AJ, Benitez D, White E. Yoga practice is associated with attenuated weight gain in healthy, middle-aged men and women. Altern Ther Health Med. 2005;11(4):28–33. [PubMed] [Google Scholar]
- 16.Telles S, Narendran S, Raghuraj P, Nagarathna R, Nagendra HR. Comparison of changes in autonomic and respiratory parameters of girls after yoga and games at a community home. Percept Mot Skills. 1997;84(1):251–7. doi: 10.2466/pms.1997.84.1.251. [DOI] [PubMed] [Google Scholar]
- 17.Dvivedi J, Dvivedi S, Mahajan KK, Mittal S, Singhal A. Effect of “61-points relaxation technique” on stress parameters in premenstrual syndrome. Indian J Physiol Pharmacol. 2008;52(1):69–76. [PubMed] [Google Scholar]
- 18.Wu W-L, Lin T-Y, Chu I-H, Liang J-M. The acute effects of yoga on cognitive measures for women with premenstrual syndrome. J Altern Complement Med. 2015;21(6):364–9. doi: 10.1089/acm.2015.0070. [DOI] [PubMed] [Google Scholar]
- 19.Morse CA, Dennerstein L, Farrell E, Varnavides K. A comparison of hormone therapy, coping skills training, and relaxation for the relief of premenstrual syndrome. J Behav Med. 1991;14(5):469–89. doi: 10.1007/BF00845105. [DOI] [PubMed] [Google Scholar]
- 20.Douglas S. Premenstrual syndromeEvidence-based treatment in family practice. Can Fam Physician. 2002;48:1789–97. [PMC free article] [PubMed] [Google Scholar]
- 21.Thys-Jacobs S, Ceccarelli S, Bierman A, Weisman H, Cohen MA, Alvir J. Calcium supplementation in premenstrual syndrome: a randomized crossover trial. J Gen Intern Med. 1989;4(3):183–9. doi: 10.1007/BF02599520. [DOI] [PubMed] [Google Scholar]
- 22.Buchanan JR, Santen R, Cauffman S, Cavaliere A, Greer RB, Demers LM. The effect of endogenous estrogen fluctuation on the metabolism of 25-hydroxyvitamin D. Calcif Tissue Int. 1986;39(3):139–44. doi: 10.1007/BF02555109. [DOI] [PubMed] [Google Scholar]
- 23. Mehta B. Effect of yoga and Calcium intake on premenstrual syndrome (tension) in young females- a comparative Physiological and biochemical study. [Dissertation]. India: University of Rajasthan; 2004.