ABSTRACT
Background:
Multiple sclerosis is accompanied by secondary clinical signs such as insomnia. Considering the side effects of drugs and also increasing acceptability of psychotherapy methods in health systems, we aimed to determine the effect of group cognitive behavioral therapy on the quality of sleep in women with multiple sclerosis in 2014.
Methods:
This study is a randomized controlled clinical conducted on 72 women with multiple sclerosis who referred to medical centers of Isfahan. After convenience sampling, participants were randomly allocated into two equal groups of control (n=36) and intervention (n=36). In the intervention group, cognitive behavioral therapy was performed in 8 sessions. The control group, along with receiving the common drugs, participated in 3 group sessions and talked about their feelings and experiences. Data were gathered using Pittsburgh Sleep Quality Index (PSQI) and analyzed through independent t-test, Chi-square, Mann Whitney, ANOVA with repeated measure, using SPSS 18.
Results:
There was a significant difference between the mean score of sleep quality of the control and intervention groups immediately and one month after the intervention (P<0.001). ANOVA with repeated measure test showed that the mean score of sleep quality of patients in the intervention group had a significant difference at three stages of before, immediately and one month after the intervention.
Conclusions:
According to the results of this study, cognitive behavioral therapy, as an effective and cost-effective therapy, could improve sleep quality in patients with multiple sclerosis.
Trial Registration Number: IRCT2015012720833N1
KEYWORDS: Sleep disorders, Cognitive behavioral therapy, Multiple sclerosis
INTRODUCTION
Multiple sclerosis (MS) is one of the most common chronic diseases of the central nervous system, in which demyelinated neurons caused by the disease, would affect its sensory and motor functions.1 The most common age of the onset for this disease is from 20 to 40 years old and it usually happens when the individual is taking a great deal of family and social responsibilities. Therefore, the damages caused by this disease would target the productive forces of the society and hence everybody that lives in the society.2
The prevalence rate of the disease varies from 60 to 200 per 100,000 people in the United States. Iran is considered to be located in a medium prevalence zone for MS and its rates have dramatically increased in the past 20 years.3
Sleep disorder is one of the secondary clinical signs of this disease and one of the complications caused because of central nervous system damage that involves more than 50% of patients. Therefore, these patients experience more sleep problems than general population and patients with other chronic diseases. Also, according to the results of previous studies, MS female patients suffer from sleep disorders more than males.4,5
Sleep disorders in these patients could have many reasons and potentially start with symptomatic and immunological treatments.5 Also, disease-related factors like pain and intensification of patient’s physical and mental problems could induce poor quality of sleep in these patients. In mental dimension, anxiety and depression are the most important symptoms of the disease that could affect the patient’s quality of sleep. 5,6 Thus, according to the results of some studies, by treating the anxiety and depression of patients with multiple sclerosis, their quality of sleep would be enhanced.7 Disorders like insomnia, difficulty sleeping during the day, breathing problems during sleep, frequent waking (waking up more than once), and having difficulty falling asleep (falling time of more than 30 minutes) are some of the factors that could affect the quality of sleep.
According to the results of different studies, patients with sleep disorders are at risk for co-occurrence of other problems like vascular diseases, obesity and diabetes that would threaten the health of patients in long term. 7,8
Different methods are used for treatment of the patients’ insomnia, like tranquilizers or sleeping pills. Due to the complications and side effects of drug therapy, following psychotherapy methods that could reduce sleep disorder in patients with MS seems rational. 9
Cognitive–behavioral therapy (CBT) has represented an innovative psychotherapy approach. Since its introduction which dates back to more than 40 years ago, it has continuously developed and overall it has been highly successful. 10 Regarding the conducted research, this type of treatment could slow the pace of the disease and delay the onset of perpetual disability. 11
Most of the patients with multiple sclerosis, due to their insomnia, have wrong thoughts and beliefs about sleep and their sleep disorders and these thoughts would lead to disturbed functionality, thus increasing the intensity of insomnia. 12 The main mechanism involved in the effect of cognitive behavioral treatment is its deep effect on patient’s thoughts and beliefs about insomnia.
Cognitive behavioral treatment could reduce anxiety by changing these thoughts and beliefs and consequently reduce the symptoms of insomnia. 12,13 Also, using methods like stop thinking, distracting the attention and problem resolving would decrease negative thoughts during the day and at bedtime that could lead to decrement of sleep disorders in patients. 13
According to the literature about necessity of attention to quality of sleep in patients with multiple sclerosis on one hand, and insufficient studies aimed to evaluate the effects of psychological interventions such as cognitive behavioral therapy on sleep quality of these patients on the other hand, this study was conducted to evaluate the effect of group cognitive behavioral treatment on the quality of sleep in women with multiple sclerosis.
MATERIALS AND METHODS
Study Design and Participants
The present randomized controlled clinical trial study was conducted on two groups (control and intervention) in three stages of before, immediately and one month after the treatment process. 5
Statistical population was all the women with multiple sclerosis who referred to neurology specialized clinics, including MS clinics of Kashani and Al-Zahra hospitals. After receiving recommendation letter from research council of Isfahan University of Medical Sciences, the researcher referred to the study environment from June to August 2014. Samples were selected by convenience method from 100 women who had multiple sclerosis and referred to the study environment. 5
The inclusion criteria were definite diagnosis of multiple sclerosis by a neurologist based on Mc-Donald criteria, passing at least 6 months from the time of diagnosis, gaining a score of 5 or more for quality of sleep based on PSQI, having at least diploma (considering the active and participatory nature of cognitive behavioral therapy and its daily homework), not being a medical staff (physician, nurse), not using other psychotherapy methods like physical therapy, acupuncture, yoga and psychotherapy sessions at the time of the study, no recurrence of the disease during the previous month, not having any diagnosed mental and physical (chronic or acute) diseases at the time of the study (like vascular or renal diseases, severe depression, dysarthria or hearing impairment), no previous participation in therapeutic sessions like relaxation or cognitive therapy in the past 6 months and gaining a score of zero(normal neurological tests) to 5.5 (Ambulatory for 100 meters, disability precludes full daily activities) according to Expanded Disability Status Scale (EDSS) and based on the patients’ records and consultation with their doctors. 7
The exclusion criteria were unwillingness to participate in the study, inability for regular participation in sessions (being absent for more than 2 sessions), and encountering severe crisis and stress during the study.
Considering formula, the mean difference, reliability of 95%, power of 80%, minimum acceptable difference of 0.7s, and 10% possibility of sampling loss, 72 patients were selected for the study. The samples were randomly allocated to control (n=36) and test groups (n=36) through minimization method. In randomized controlled clinical trial studies with samples less than 200, there is a possibility of significant differences between the control and test groups, so the aim of minimization is to minimize the imbalance between the number of patients in each group.7,8
Instruments
Data gathering tool was a questionnaire that consisted of two parts; the first part was about demographic and clinical characteristics (sex, age, marital status, educational level, duration of the disease, number of hospitalizations, job, income and stage of the disease), and the second part was Pittsburgh Sleep Quality Index (PSQI). Pittsburgh Sleep Quality Index questionnaire is a standard self-report tool that evaluates the sleep quality during the previous month.9 This questionnaire’s reliability was calculated in a study conducted in Taiwan (r=0.88). Also, diagnostic sensitivity and specificity of the questionnaire in distinguishing between good and poor sleepers were 90% and 87%, respectively. Also, the internal consistency (Cronbach’s a) of the PSQI in this study was 0.66.11 Reliability and validity of this questionnaire in an Iranian population were evaluated by Farrahi Moghaddam et al (2012) and Cronbach’s alpha coefficient for all the subjects was 0.77. Moreover, when the general health questionnaire-12 was used as a measure of psychiatric morbidity, it was well correlated with the PSQI scores (r=0.54, P<0.001).15
This questionnaire contains 18 questions in 7 dimensions of intellectual quality, delay in falling sleep, and duration of sleep, sleep disorder, consumptions of sleeping drugs and dysfunction during the day. Each dimension has a score of zero (not having any problem) to three (having a serious problem). The total score of Pittsburgh’s sleep is achieved from the sum of the scores of 7 dimensions from 0 to 21. Higher scores indicate lower quality of sleep. Score of 5 or more indicates undesirable quality of sleep.
Procedures
The intervention program was designed and performed based on previous studies, literature and the opinion of specialized experts (neurologists and psychiatrics). It was conducted in eight 90-minute sessions and one session per week that were managed by a psychiatric nurse (the researcher) (table 1).
Table 1.
The content of cognitive behavioral therapy sessions for patients with multiple sclerosis
| Session | Content of the session |
|---|---|
| 1st session | Introducing and getting acquainted with the program and the researcher, understanding multiple sclerosis (definition, etiology, risk factors, complications, treatment), explaining sleep and its quality among patients with multiple sclerosis |
| 2nd session | Introducing cognitive behavioral therapy for patients’ tiredness , explaining muscle relaxation and implementing muscle relaxation with 8 muscle groups first by the researcher and then by the patients |
| 3rd session | Introducing ABCD model, determining the relationship between thoughts and emotions, explaining stages of diaphragmatic breathing and visualization, learning methods to control stimulants |
| 4th session | Learning 10 cognitive faults and negative automatic thoughts, learning the importance of stability and coordination between activity and resting, learning methods of sleep restriction |
| 5th session | Learning strategies to cope with negative thoughts (steps for replacing rational thoughts), explaining sleep improvement factors, encouraging the patients to attend a program to improve their sleep condition |
| 6th session | Learning strategies to cope with stress (emotion-oriented, problem-oriented and incompatible), training problem solving method |
| 7th session | Learning the method of thought experimenting |
| 8th session | Reviewing all the discussed subjects, receiving the feedback of the participants about the subjects, question and answer, group discussion and conclusion |
The presented program for this study was designed to determine, challenge and change the participants’ negative cognitions based on ABCD model; A: existence of a reality, event or behavior, B: belief, C: emotional and behavioral consequences and D: challenging and confronting the thoughts.
Each session was designed in a way that each participant, other than learning a cognitive technique, would also learn and practice a behavioral technique (muscle relaxation, using diaphragmatic breathing and visualization), too. At the beginning of each session, previous discussions and participants’ homework were reviewed and the sessions ended with questioning and group discussion. Also, relaxation techniques were conducted at the beginning and end of each session.
The control group was asked to only participate in pre-intervention, post-intervention and follow-up stages, and in addition to receiving the common treatment (drugs) during the intervention, a separate place was selected for the control group and 3 sessions were assigned for them to participate and talk about their disease and experiences.
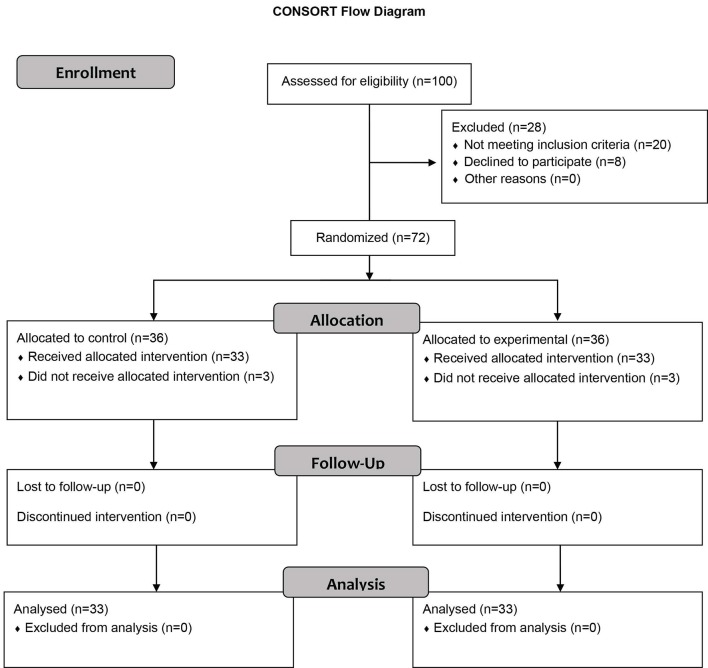
During the intervention, 3 patients from the intervention group (due to encountering severe crisis and stress and inability to participate in the sessions) and 3 patients from the control group (due to inability to participate in the sessions and re-occurrence of the disease) withdrew from the study. Therefore, the study was completed with 33 patients in the intervention group and 33 in the control group (figure 1).
Figure1.
Diagram of the participants in the study.
At the end of the study, some of the patients from the control group, voluntarily and free of charge, participated in this treatment procedure.
Ethical Considerations
The researcher explained the aims of the study for all the participants and received written informed consent form from them. All the participants were ensured about the confidentiality of their information. Also, they were free to continue or leave the study at any point. It must be noted that in the present study the doze of sleeping drugs in both groups had no significant difference before and after the intervention and regarding ethical considerations, no recommendations were made to participants about reducing or quitting the drugs; only the dosage of these drugs before and after the intervention was evaluated.
Data Analysis
The collected data were analyzed using independent t-test, Chi-square and Mann Whitney to compare the demographic characteristics of the intervention and control groups. Also, to compare the quality of sleep of the intervention and control groups, we used independent t-test and at the time periods of before, immediately and one month after the intervention ANOVA with repeated measure test and Least Significant Difference test (LSD) to compare the data distribution of quantitative variables (the mean score of sleep quality) at all time periods. Data were analyzed using SPSS 18.
RESULTS
The results showed that both the intervention and control groups were similar regarding variables like age, duration of disease, educational level, marital status, employment status, family income, and the clinical course of the disease (P>0.05). The mean and standard deviation of the patients’ age in the intervention and the control groups were 35.3 (5.3) and 33.2 (8.9) respectively, and 70% of the women in both groups were married and housewife. Also, 60.5% of the intervention group and 75% of the control group had diploma; moreover, 85.2% of the intervention group and 88.3% of the control group had a clinical course of relapse-remission. The mean duration of the disease for the intervention group was 5.6 (5.8) years and for the control group it was 6.1 (6.5) years.
The result of independent t-test showed no significant difference between the mean score of sleep quality of both groups before the intervention (P=0.5).
ANOVA with repeated measure test showed that while the mean score of sleep quality of the intervention group had a significant difference at three stages of before, immediately and one month after the intervention, this difference was not significant for the control group (P=0.332) (table 2).
Table 2.
Comparison of the mean score of sleep quality of patients before, immediately and one month after the intervention between the control and intervention groups
| Time period Variable | Before the intervention | Immediately after the intervention | One month after the intervention | ANOVA with repeated measure test | ||
|---|---|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean±SD | F | P value | ||
| Sleep quality of patients | Intervention | 14.58±0.86 | 11.73±0.65 | 11.5±0.42 | 89.807 | <0.001 |
| Control | 13.44±0.65 | 13±0.48 | 13.7±0.54 | 0.979 | 0.332 | |
P values lower than 0.05 are statistically significant
Moreover, the results of comparing dimensions of sleep quality using independent t test before, immediately and one month after the intervention showed a significant difference in all dimensions except for duration of sleep (P=0.115), use of sleeping drugs (P=0.225), and daily dysfunction (P=0.105) (table 3).
Table 3.
Comparison of the mean score of each dimension of sleep quality index before, immediately and one month after the intervention between the control and intervention groups
| Sleep quality dimensions | Before the intervention | immediately after the intervention | One month after the intervention | ANOVA with repeated measure test | ||||
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | |||
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | F | P | |
| Intellectual quality of sleep | 1.74±1.69 | 2.52±0.75 | 1.45±0.56 | 2.05±1.81 | 1.34±0.50 | 2.41±0.50 | 65.8 | <0.001 |
| Sleep sufficiency | 2.57±13.9 | 1.74±1.68 | 1.70±1.67 | 1.28±1.40 | 1.03±2.82 | 1.16±1.15 | 50.7 | <0.001 |
| Delay in falling sleep | 1.91±0.85 | 2.31±0.79 | 1.78±0.78 | 2.42±0.69 | 1.42±0.74 | 2.90±0.71 | 45.6 | <0.001 |
| Duration of sleep | 1.40±0.91 | 1.22±1.08 | 1.47±0.60 | 2.14±0.64 | 1.26±0.50 | 2.06±0.59 | 88.8 | 0.115 |
| Sleep disorder | 2.40±2.74 | 2.14±2.56 | 2.28±2.50 | 2.48±2.58 | 2.15±2.39 | 2.21±2.56 | 35.5 | <0.001 |
| Consumption of sleeping drugs | 2.60±1.37 | 2.60±0.69 | 2.65±0.65 | 2.66±0.85 | 2.75±0.61 | 2.50±0.86 | 43.4 | 0.225 |
| Dysfunction during the day | 2.20±1.34 | 2.60±0.94 | 2.42±1 | 2.77±0.97 | 2.48±1.01 | 2.79±1 | 28.6 | 0.105 |
P values lower than 0.05 are statistically significant
DISCUSSION
The present study evaluated the effect of group cognitive behavioral therapy on sleep quality of women with multiple sclerosis. According to the results, the mean score of sleep quality of patients in the intervention group was significantly lower immediately and one month after the intervention than before the intervention.
A study conducted to evaluate the effect of sleep health trainings and behavioral therapy on sleep quality of some Japanese workers, similar to the present study, indicated that the group who received cognitive therapy had a significantly better sleep quality than the group who just received sleep health trainings. Also, this change was maintained in the intervention group 3 months after the intervention.16 Also, the results of another study aiming to evaluate the effectiveness of clinical cognitive behavioral therapy on the insomnia of cancer patients showed that cognitive behavioral therapy could be an effective and efficient clinical method to reduce the patients’ sleep disorders. The changes in sleep quality of patients continued for 6 months after the intervention.13 But the results of a research about the role of reducing dysfunctional beliefs in improving insomnia showed that improper beliefs related to sleep disorders could be reduced with cognitive behavioral therapy, but this change in beliefs could not have an important role in reduction of insomnia in patients.17 The reason for this difference between the results could be due to the content of the sessions. In the present study, along with emphasis on cognitive therapies, implementing relaxation exercises and intellectual visualization at the beginning and end of each session and also doing exercises at home as homework had an important role in improvement of sleep quality in patients. Also, in the present study the mean changes of scores of intellectual quality of sleep, sufficiency of sleep, delay in falling sleep and sleep disorders at three stages of before, immediately and one month after the intervention showed a significant difference (P<0.05). In the similar study, patients who received cognitive behavioral therapy reported more decrement in delay in falling sleep and more improvement in sleep sufficiency than the control group and these changes in the patients’ sleep quality of continued until the 3-month follow-up after the intervention.18 The results of another study showed that progressive muscle relaxation increased the total score of insomnia severity index and its dimensions including inability to initiate sleep, number of waking during the night and the duration of real sleep among hemodialysis patients.19 Also, the results of a research aiming to evaluate the effectiveness of group cognitive therapy on symptoms of insomnia in women with chronic insomnia showed that group cognitive therapy along with drug therapy, in comparison to just drug therapy, has been more effective on the insomnia symptoms of patients with chronic insomnia. This result was relatively stable until 3 months after the therapy.20Therefore, according to the results of this study, through cognitive behavioral therapy sessions, patients learned about cognitive distortions and negative automatic thoughts and strategies to encounter these thoughts and consequently learned that by using these strategies at different life situations they could feel more relaxed. Therefore, considering the effects of these thoughts in creating anxiety in patients and consequently reducing sleep quality in different dimensions, this therapy was able to improve the sleep quality of patients by improving the delay in falling sleep, intellectual quality of sleep, sleep sufficiency and sleep disorders. However, it seems that more time and sessions are required to have more effective interventions for sleep quality of patients with multiple sclerosis in dimensions of consumption of sleeping drugs, dysfunction during the day, and duration of sleep.
Limitation of this study included individual differences in response to treatment and impact of environmental factors which could potentially affect the patient’s perception of cognitive behavioral therapy effects. We restricted the effect of these limitations by allocating the patients to the control and intervention group randomly.
CONCLUSION
According to the results of this study, cognitive behavioral therapy, as an effective and cost-effective therapy, could improve sleep quality in patients with multiple sclerosis. Therefore, providing this type of psychological interventions in mental health care services for patients with chronic diseases like multiple sclerosis is suggested. Also, in addition to minimizing the limitations mentioned above, conducting studies with more samples and longer follow-up periods is recommended. Also, considering the results of this study, we suggest using inter-professional approach and partnership between psychiatric nurses and physicians in order to maintain and improve mental health of these patients.
ACKNOWLEDGEMENT
The present article was financially supported by Isfahan University of Medical Sciences. Researchers would like to thank all the patients who participated in this study and also the authorities of MS clinics of Kashani and Al-Zahra hospitals.
Conflict of Interest:None declared.
REFRENCES
- 1.Ghaem H, Borhani Haghighi A. The impact of disability, fatigue and sleep quality on the quality of life in multiple sclerosis. Annals of Indian Academy of Neurology. 2008;11:236–41. doi: 10.4103/0972-2327.44559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sarraf P, Azizi S, Moghaddasi AN, et al. Relationship between Sleep Quality and Quality of Life in Patients with Multiple Sclerosis. International Journal of Preventive Medicine. 2014;5:1582–6. [PMC free article] [PubMed] [Google Scholar]
- 3.Masoudi R, Abedi HA, Abedi P, Mohammadianinejad SE. Iranian family caregivers’ challenges and issues in caring of multiple sclerosis patients: A descriptive explorative qualitative study. Iran J Nurs Midwifery Res. 2014;19:416–23. [PMC free article] [PubMed] [Google Scholar]
- 4.Lunde HMB, Aae TF, Indrevåg W, et al. Poor sleep in patients with multiple sclerosis. PLoS One Journal. 2012;7:e49996. doi: 10.1371/journal.pone.0049996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pagnini F, Bosma CM, Phillips D, Langer E. Symptom changes in multiple sclerosis following psychological interventions: a systematic review. BMC Neurology. 2014;14:222. doi: 10.1186/s12883-014-0222-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carnicka Z, Kollar B, Siarnik P, et al. Sleep disorders in patients with multiple sclerosis. Journal of Clinical Sleep Medicine. 2015;11:553–7. doi: 10.5664/jcsm.4702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garland SN, Johnson JA, Savard J, et al. Sleeping well with cancer: a systematic review of cognitive behavioral therapy for insomnia in cancer patients. Neuropsychiatric Disease and Treatment. 2014;10:1113–24. doi: 10.2147/NDT.S47790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vitkova M, Gdovinova Z, Rosenberger J, et al. Factors associated with poor sleep quality in patients with multiple sclerosis differ by disease duration. Disability and Health Journal. 2014;7:466–71. doi: 10.1016/j.dhjo.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Bahreini S, Naji SA, Manani R, Bekhradi R. Effects of massage therapy on sleep quality in women with multiple sclerosis. Journal of Oromieh School of Nursing and Midwifery. 2010;4:197–203. [In persian] [Google Scholar]
- 10.Johnsen TJ, Friborg O. The Effects of Cognitive Behavioral Therapy as an Anti-Depressive Treatment is Falling: A Meta-Analysi. Psychological Bulletin. 2015;141:747–68. doi: 10.1037/bul0000015. [DOI] [PubMed] [Google Scholar]
- 11.Cheng SH, Shih CC, Lee IH, et al. A study on the sleep quality of incoming university students. Psychiatry Research. 2012;197:270–4. doi: 10.1016/j.psychres.2011.08.011. [DOI] [PubMed] [Google Scholar]
- 12.Bastani F, Sobhani M, Shamsikhani S, et al. Effect of Acupressure on sleep quality in women with Multiple Sclerosis. Complementary Medicine Journal of Faculty of Nursing & Midwifery. 2013;3:574–84. [In persian] [Google Scholar]
- 13.Espie CA, Fleming L, Cassidy J, et al. Randomized controlled clinical effectiveness trial of cognitive behavior therapy compared with treatment as usual for persistent insomnia in patients with cancer. Journal of Clinical Oncology. 2008;26:4651–8. doi: 10.1200/JCO.2007.13.9006. [DOI] [PubMed] [Google Scholar]
- 14.Saghaei M. An overview of randomization and minimization programs for randomized clinical trials. Journal of Medical Signals & Sensors. 2011;1:55–61. [PMC free article] [PubMed] [Google Scholar]
- 15.Farrahi Moghaddam J, Nakhaee N, Sheibani V, et al. Reliability and validity of the Persian version of the Pittsburgh Sleep Quality Index (PSQI-P) Sleep Breath. 2012;16:79–82. doi: 10.1007/s11325-010-0478-5. [DOI] [PubMed] [Google Scholar]
- 16.Dayapoğlu N, Tan M. Evaluation of the Effect of Progressive Relaxation Exercises on Fatigue and Sleep Quality in Patients with Multiple Sclerosis. Journal of Alternative and Complementary Medicine. 2012;18:983–7. doi: 10.1089/acm.2011.0390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishinoue N, Takano T, Kaku A, et al. Effects of sleep hygiene education and behavioral therapy on sleep quality of white-collar workers: a randomized controlled trial. Industrial Health. 2012;50:123–31. doi: 10.2486/indhealth.ms1322. [DOI] [PubMed] [Google Scholar]
- 18.Okajima I, Nakajima S, Ochi M, Inoue Y. Reducing dysfunctional beliefs about sleep does not significantly improve insomnia in cognitive behavioral therapy. PLoS One. 2014;9:e102565. doi: 10.1371/journal.pone.0102565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lovato N, Lack L, Wright H, Kennaway DJ. Evaluation of a brief treatment program of cognitive behavior therapy for insomnia in older adults. Sleep. 2014;37:117–26. doi: 10.5665/sleep.3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saeedi M, Ashktorab T, Shamsikhani S, Saatchi K. The effect of progressive muscle relaxation on insomnia severity of hemodialysis patients. Journal of Complementary Medicine. 2013;2:159–70. [In persian] [Google Scholar]