Abstract
Background:
Computed tomography-guided percutaneous core needle biopsy (PCNB) is a diagnostic technique for initial assessment of mediastinal mass lesions. This study was conducted to evaluate its diagnostic yield and its complication rate.
Materials and Methods:
We reviewed the records of CT-guided PCNB in 110 patients with mediastinal mass lesions performed in Kashani and Alzahra Hospitals, Isfahan, from 2006 to 2012. Gender, age at biopsy, size, and anatomic location of the lesion, number of passes, site of approach, complications, and final diagnosis were extracted.
Results:
Our series encompasses 52 (47.2%) females and 58 (52/7%) males with mean age of 41 ± 8 years. The most common site of involvement was the anterior mediastinum (91.8% of cases). An average of 3/5 passes per patient has been taken for tissue sampling. Parasternal site was the most frequent approach taken for PCNB (in 78.1% of cases). Diagnostic tissue was obtained in 99 (90%) biopsies while, in 11 (10%) cases, specimen materials were inadequate. Lymphoma (49.5%) and bronchogenic carcinoma (33.3%) were the most frequent lesions in our series. The overall complication rate was 17.2% from which 10.9% was pneumothorax, 5.4% was hemoptysis, and 0.9% was vasovagal reflex.
Conclusion:
CT-guided PCNB is a safe and reliable procedure that can provide a precise diagnosis for patients with both benign and malignant mediastinal masses, and it is considered the preferred first diagnostic procedure use for this purpose.
Keywords: Computed tomography scan, mediastinal mass, percutaneous core needle biopsy, pneumothorax
INTRODUCTION
Mediastinal mass lesions include wide spectrum of benign and malignant conditions. In recent years, invasive and potentially high-risk surgical procedures for assessment of mediastinal mass lesions have been replaced with percutaneous core needle biopsy (PCNB). This technique under guidance of fluoroscopy, ultrasonography, or computed tomography (CT) allows sufficient tissue sampling for accurate histologic and immunohistochemical evaluation; thereby it could highlight the need for further mediastinoscopy, mediastinotomy, thoracoscopy, or open chest surgery.[1,2,3,4] Previous reports have been shown higher accuracy of histology in comparison with cytology in evaluation of mediastinal lesions.[3,4,5]
Although image-guided PCNB is less invasive as compared to the surgical techniques, occurrence of complications in this procedure is inevitable.[6]
We conducted a retrospective study to determine the diagnostic yield and the complication rate of CT-guided PCNB in assessment of patients with mediastinal mass lesions in two university hospitals of Isfahan, Iran.
MATERIALS AND METHODS
A retrospective case note review was performed of all patients who had referred for thoracic CT-guided PCNB for initial evaluation of mediastinal mass lesions, from 2006 to 2012 in two radiology centers in Alzahra and Kashani Hospitals, Isfahan, Iran. The lesions presented as solid masses in imaging studies. The following information were collected from the case notes of 110 patients; gender, age at biopsy, size of the lesions, location of the lesion in mediastinum, number of passes, diagnostic approach (transpleural, parasternal, direct mediastinal, transsternal, suprasternal, extrapleural), inadequate biopsies which were considered of not being provided enough pathologic material for diagnostic evaluation, complications of PCNB (pneumothorax, hemoptysis, and vasovagal reaction), histological results of the biopsy, and final diagnosis which was determined by surgical histopathological examination or clinico-radiologic follow-up.
The procedure of tissue sampling in all patients was performed with the same protocol, as follows: “All biopsies were performed with CT guidance using an 18-gauge automated or semi-automated cutting needle system. The patients were placed in a prone, supine, or oblique position depending on the location of the lesion. Preliminary, 10 mm CT scans were obtained to localize the lesions and to select the optimal approach. Generally, we have chosen the shortest vertical path to afford a reasonable window to the lesion and to avoid traversing lung parenchyma, bulla, or vessels. The skin entry site was marked by using the laser light from the CT gantry and then biopsy area cleansed with a suitable antiseptic solution and anesthesia obtained with lidocaine 2% solution injected intradermally and subcutaneously. It is important to adequately anesthetize the pleura. A small stab incision is also made to aid introduction of the needle and then biopsy needle was introduced into the margin of the lesion and after CT confirmation of an adequate needle tip position, the biopsy system was fired obtaining a core of tissue in front of the needle [Figure 1].
Figure 1.
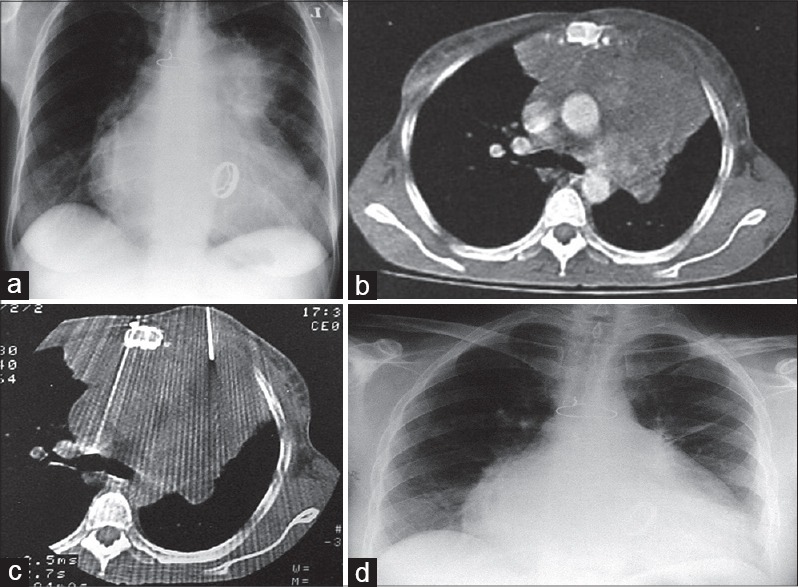
(a) In a 42-year-old female patient with prosthetic heart valve, plain X-ray shows a large anterior mediastinal mass. (b) After contrast-enhanced computed tomography scan, vascular structures are well demarcated. (c) Computed tomography-guided core needle biopsy was performed and pathologically established as Hodgkin's disease. (d) Chest X-ray of the same patient 2 years later. Mediastinal mass is completely disappeared
The numbers of samples obtained depend on the suspected disease and patient's collaboration. The samples were obtained, fixed in a formalin solution, and sent for histopathologic evaluation. After removal of the biopsy needle, immediate postbiopsy pneumothorax or bleeding was searched for on CT images around the puncture site or at the uppermost portion of the lung, in the cases with transpulmonary approach. The patient was then placed rapidly in a puncture site down position. Efforts to reduce the prevalence of biopsy-induced pneumothorax have focused mainly on limiting the number of pleural punctures, administering 100% oxygen during and after the procedure for speed resorption of pneumothorax. Patients with enlarging pneumothoraces on several chest radiographs and those with symptomatic pneumothoraces were treated with placement of a chest tube.”[2]
After review of the notes, all data were entered into SPSS Statistics (version 20, IBM, Somers, NY, USA). Appropriate statistical tests were used as needed.
RESULTS
A total of 110 cases with mediastinal mass lesions were consecutively enrolled to the study. The age at biopsy was ranged from 15 to 78 years (mean 41 ± 8). There were 52 (47.2%) females and 58 (52/7%) males. The maximum diameter of lesions ranged 3–11 cm, which 90 (81/8%) were larger than 4 cm. In 101 (91.8%) of cases, the lesions were localized in the anterior mediastinum, 5 (4.5%) were in the middle, and 4 (3.6%) were in the posterior mediastinum. The rate of two, three, four, and five passes for tissue sampling were 13 (11.8%), 43 (39.1%), 35 (31.8%), and 19 (17.2%), respectively, giving an average of 3/5 passes per patients. In 86 (78.1%) cases, CT-guided PCNB were performed by parasternal approach, 22 (20%) by transpleural, and 2 (1.8%) by suprasternal approach. Diagnostic tissue was obtained in 99 (90%) biopsies while, in 11 (10%) cases, specimen materials were inadequate.
Table 1 demonstrates the diagnoses made on the basis of histopathological study of PCNB. Lymphoma (49.5%) and bronchogenic carcinoma (33.3%) were the most frequent lesions in our biopsy cases. The final diagnosis was also confirmed by surgery in 10 patients. In the other 89 cases, the histopathological study of PCNB was accepted as the final diagnosis which had correlation with their courses in long-term clinical follow-up (from 1 to 6 years) and response to treatment.
Table 1.
Spectrum of histopathologic results of mediastinal mass lesions
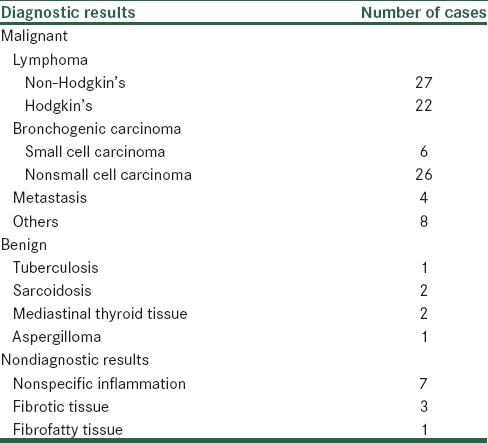
There was no false positive diagnosis of malignancy or specific benign lesions. The specificity of procedure for both malignant and benign lesions was 100%. There were four false negative diagnoses for lymphoma, giving sensitivity in its diagnosis of 92.4%.
Pneumothorax was the most frequently encountered complication occurring in 12 (10.9%) patients, of which two required chest tube insertion. Hemoptysis (minor) occurred in 6 (5.4%) of patients, and one patient had transitory hypotension due to vasovagal reflex. The overall complication rate was 17.2%, of which 15/4% were minor complication.
DISCUSSION
In this study, we report our experience in the utility of CT-guided PCNB in the diagnosis of both malignant and benign mediastinal mass lesions as an initial diagnostic procedure. The findings of this study have demonstrated that CT-guided PCNB is a safe and reliable procedure for initial assessment of mediastinal mass lesions which could conclusively help us for proper therapeutic.
In our series, most of the mediastinal mass lesions were located in anterior mediastinum. Further, lymphoma was the most frequent diagnosis. Several studies have reported that mediastinum is commonly involved by lymphoma.[7,8,9,10] Considering the predominance of lymphoma in our series and high sensitivity of PCNB for the diagnosis of lymphoma, this study also confirm the usefulness of image-guided PCNB for evaluation of patients with lymphoma. In a study by Demharter et al., PCNB obtained a sensitivity of 89% and specificity of 97% for diagnosis of malignant lymphoma and also indicated the usefulness of this technique in subclassification of lymphoma.[9] Zinzani et al. reported that image-guided PCNB is effective in the initial diagnosis of mediastinal lymphoma with a sensitivity of 81%.[8] Sklair-Levy et al. reported a success rate of 71.5% for CT-guided PCNB in mediastinal lymphoma.[11]
The procedure resulted in a higher degree of histopathological diagnosis (90%). This rate has reported to be 87% and 97% in the studies of Greif et al. and Loubeyre et al., respectively.[12,13]
In our study, PCNB provided adequate specimen material in 99 cases giving an accuracy sample yield of 90% which was higher than that reported by Greif et al.[12] In the study of Zafar et al. adequate material rate by this technique was 92%.[14]
Our complication rate compares favorably with previously reported studies.[15,16,17] The overall complication rate of PCNB was 17.2% in our study. The relatively low rate of complication in our study may be due to our methods and approaches used in the study.
Our results demonstrate high sensitivity in the diagnosis of both malignant and benign lesions and we had no false positive specific diagnosis, either malignant or benign. Bungay et al.[17] and Greif et al.[12] have reported no false positive results in this study, too. All these findings confirm the accuracy of the procedure.
CONCLUSION
Determining the nature of mediastinal lesions and their precise histopathological diagnosis are necessary to reach the correct therapeutic decision and to avoid unnecessary invasive procedures. The results of our experience demonstrate that PCNB is an easy, safe, and reliable method which can provide the mentioned goals for accurate diagnostic information in the majority of mediastinal lesions. PCNB should be considered whether the lesion is thought to be malignant or benign because of its high sensitivity and acceptable complication rate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ansari-Gilani K, Deurdulian C, Azar N, Nakamoto DA. Use of sonographic guidance for selected biopsies in the lung and superior mediastinum. J Ultrasound Med. 2012;31:1697–702. doi: 10.7863/jum.2012.31.11.1697. [DOI] [PubMed] [Google Scholar]
- 2.Herman SJ, Holub RV, Weisbrod GL, Chamberlain DW. Anterior mediastinal masses: Utility of transthoracic needle biopsy. Radiology. 1991;180:167–70. doi: 10.1148/radiology.180.1.1647039. [DOI] [PubMed] [Google Scholar]
- 3.Kulkarni S, Kulkarni A, Roy D, Thakur MH. Percutaneous computed tomography-guided core biopsy for the diagnosis of mediastinal masses. Ann Thorac Med. 2008;3:13–7. doi: 10.4103/1817-1737.37948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Priola AM, Priola SM, Cataldi A, Ferrero B, Garofalo G, Errico L, et al. CT-guided percutaneous transthoracic biopsy in the diagnosis of mediastinal masses: Evaluation of 73 procedures. Radiol Med. 2008;113:3–15. doi: 10.1007/s11547-008-0233-1. [DOI] [PubMed] [Google Scholar]
- 5.Capalbo E, Peli M, Lovisatti M, Cosentino M, Mariani P, Berti E, et al. Trans-thoracic biopsy of lung lesions: FNAB or CNB? Our experience and review of the literature. Radiol Med. 2014;119:572–94. doi: 10.1007/s11547-013-0360-1. [DOI] [PubMed] [Google Scholar]
- 6.de Margerie-Mellon C, de Bazelaire C, Amorim S, Brice P, Tazi A, Brière J, et al. Diagnostic yield and safety of computed tomography-guided mediastinal core needle biopsies. J Thorac Imaging. 2015;30:319–27. doi: 10.1097/RTI.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 7.Takahashi K, Al-Janabi NJ. Computed tomography and magnetic resonance imaging of mediastinal tumors. J Magn Reson Imaging. 2010;32:1325–39. doi: 10.1002/jmri.22377. [DOI] [PubMed] [Google Scholar]
- 8.Zinzani PL, Corneli G, Cancellieri A, Magagnoli M, Lacava N, Gherlinzoni F, et al. Core needle biopsy is effective in the initial diagnosis of mediastinal lymphoma. Haematologica. 1999;84:600–3. [PubMed] [Google Scholar]
- 9.Demharter J, Müller P, Wagner T, Schlimok G, Haude K, Bohndorf K. Percutaneous core-needle biopsy of enlarged lymph nodes in the diagnosis and subclassification of malignant lymphomas. Eur Radiol. 2001;11:276–83. doi: 10.1007/s003300000540. [DOI] [PubMed] [Google Scholar]
- 10.Lal H, Neyaz Z, Nath A, Borah S. CT-guided percutaneous biopsy of intrathoracic lesions. Korean J Radiol. 2012;13:210–26. doi: 10.3348/kjr.2012.13.2.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sklair-Levy M, Polliack A, Shaham D, Applbaum YH, Gillis S, Ben-Yehuda D, et al. CT-guided core-needle biopsy in the diagnosis of mediastinal lymphoma. Eur Radiol. 2000;10:714–8. doi: 10.1007/s003300050991. [DOI] [PubMed] [Google Scholar]
- 12.Greif J, Staroselsky AN, Gernjac M, Schwarz Y, Marmur S, Perlsman M, et al. Percutaneous core needle biopsy in the diagnosis of mediastinal tumors. Lung Cancer. 1999;25:169–73. doi: 10.1016/s0169-5002(99)00053-7. [DOI] [PubMed] [Google Scholar]
- 13.Loubeyre P, Copercini M, Dietrich PY. Percutaneous CT-guided multisampling core needle biopsy of thoracic lesions. AJR Am J Roentgenol. 2005;185:1294–8. doi: 10.2214/AJR.04.1344. [DOI] [PubMed] [Google Scholar]
- 14.Zafar N, Moinuddin S. Mediastinal needle biopsy. A 15-year experience with 139 cases. Cancer. 1995;76:1065–8. doi: 10.1002/1097-0142(19950915)76:6<1065::aid-cncr2820760622>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 15.Powers CN, Silverman JF, Geisinger KR, Frable WJ. Fine-needle aspiration biopsy of the mediastinum. A multi-institutional analysis. Am J Clin Pathol. 1996;105:168–73. doi: 10.1093/ajcp/105.2.168. [DOI] [PubMed] [Google Scholar]
- 16.Wu CC, Maher MM, Shepard JA. Complications of CT-guided percutaneous needle biopsy of the chest: Prevention and management. AJR Am J Roentgenol. 2011;196:W678–82. doi: 10.2214/AJR.10.4659. [DOI] [PubMed] [Google Scholar]
- 17.Bungay HK, Adams RF, Morris CM, Haggett PJ, Traill ZC, Gleeson FV. Cutting needle biopsy in the diagnosis of clinically suspected non-carcinomatous disease of the lung. Br J Radiol. 2000;73:349–55. doi: 10.1259/bjr.73.868.10844858. [DOI] [PubMed] [Google Scholar]


