Abstract
Background and Purpose
Youth participation in basketball is on the rise, with basketball one of the top five participation sports in Australia. With increased participation there is a need for greater awareness of the importance of the pre-participation examination, including musculoskeletal screening and functional performance testing as part of a multidisciplinary approach to reducing the risk for future injuries. As majority of all basketball injuries affect the lower extremities, pre-participation musculoskeletal screening and functional performance testing should assess fundamental movement qualities throughout the kinetic chain with an emphasis on lower extremity force characteristics, specifically eccentric loading tasks. Thus, the purpose of this clinical commentary is to review the existing literature elucidating pre-participation musculoskeletal screening and functional performance tests that can be used as a framework for rehabilitation professionals in assessing basketball athletes’ readiness to safely perform the movement demands of their sport.
Methods
Relevant articles published between 2000 and 2016 using the search terms ‘musculoskeletal screening’, ‘functional testing’, ‘youth athletes’, and ‘basketball’ were identified using MEDLINE. From a basketball-specific perspective, several relevant musculoskeletal assessments were identified, including: the Functional Hop Test Combination, the Landing Error Scoring System, the Tuck Jump Assessment, the Weight-Bearing Lunge Test, and the Star Excursion Balance Test. Each of these assessments creates movement demands that allow for easy identification of inefficient and/or compensatory movement tendencies. A basic understanding of musculoskeletal deficits including bilateral strength and flexibility imbalances, lower crossed syndrome, and dominance-related factors are key components in determination of injury risk.
Discussion
Assessment of sport-specific movement demands through musculoskeletal screening and functional performance testing is essential for rehabilitation professionals to determine movement competency during performance of fundamental movements related to basketball performance. Youth athletes represent a unique population due to their developing musculoskeletal and neuromuscular systems and should undergo pre-participation musculoskeletal screening for identification of movement limitations. Such an approach to musculoskeletal screening and functional performance may assist in identifying injury risk and also be useful at the end of rehabilitation in determining readiness to return to sport models.
Level of Evidence
Level 5
Keywords: Basketball, injury prevention, musculoskeletal screening, youth athletes
INTRODUCTION
The popularity of basketball is on the increase with an estimated 11% of the world's population (450 million people) currently playing basketball across 213 countries affiliated with Fédération International de Basketball (FIBA).1 While basketball is often thought of as an ‘American’ game, it is equally as popular in Europe, Asia, and Australia. With the expansion of the Australian National Basketball League, basketball is now the second highest team participation sport in Australia, with a significant increase in youth participation.2 Not only is the popularity of basketball increasing, so is the intensity at which the sport is being played.3 The physiological demands of basketball include aerobic and anaerobic capacity in addition to integrating physical characteristics including muscular strength, power, endurance, flexibility, speed, agility, and skill.4,5 Frequent jump landings and change of direction throughout the game contribute much of the physiological load imposed during competitive games, with players exposed to high levels of eccentric loading. For example, examining the physiological load of Australian National Basketball League (NBL) players during competitive games McInnes et al6 reported an average of 46 jumps occurring per player, with 105 high-intensity run efforts (sprints) performed once every 21 seconds. Players performed an average of 1000 movement pattern changes (one every 2.0 seconds) with 31% and 10% of movements consisting of lateral shuffling and sprints, respectively. This indicates that force interplay characteristics such as force reduction, dynamic stabilization, and force production7 associated with acceleration, deceleration and rapid changes in direction appear to be a key component in game demands. The anaerobic energy system is most dominant while performing such movements, thus, basketball appears to be more dependent upon anaerobic power, in contrast to aerobic capacity.8 Additionally, the need for muscular size and strength in basketball athletes is becoming more paramount and are deemed essential physical characteristics as the game at both collegiate9 and professional10,11 levels has evolved into a highly physical contact sport.12 Collectively, the increased intensity of practice and game-play,3 combined with the greater physicality and athleticism of the modern game,9,11 are thought to be significant factors contributing to the increase in the number of injuries reported.9,11,13,14
As such, a central component of athlete preparation is pre-participation musculoskeletal screening and functional testing.15-18 The National Athletic Trainers’ Association (NATA)17 highlights that musculoskeletal injury is a common cause of restriction of sports activities (i.e., lost training and game time); therefore, pre-participation musculoskeletal screening and functional testing should be directed towards detection of any underlying musculoskeletal limitations that might predispose an athlete to injury. While literature on sport-specific pre-participation musculoskeletal screening and functional testing protocols is limited,19-21 lower extremity and lower back symptoms appear to be common complaints.20 Screening movement quality throughout the kinetic chain emphasizing lower-extremity force interplay characteristics,7 specifically eccentric loading should be targeted. As such, rehabilitation professionals should not only possess a basic understanding of musculoskeletal deficits including bilateral strength and flexibility imbalances, lower crossed syndrome, and dominance-related factors which are key components in determination of injury risk, but should also be familiar with the incidence of injury (injury rate) and injury characteristics (injury type) related to basketball practice and games.
From a basketball-specific perspective, musculoskeletal assessments such as the Functional Hop Test Combination, the Landing Error Scoring System, the Tuck Jump Assessment, the Weight-Bearing Lunge Test, and the Star Excursion Balance Test allow for easy identification of inefficient and/or compensatory movement tendencies. However, to the authors’ knowledge there are no published basketball-specific pre-participation musculoskeletal screening and functional testing protocols.22 Therefore, the purpose of this clinical commentary is to review the existing literature elucidating pre-participation musculoskeletal screening and functional performance tests that can be used as a framework for rehabilitation professionals in assessing basketball athletes’ readiness to safely perform the movement demands of their sport.
INJURY RATES AND CHARACTERISTICS IN BASKETBALL
Injury Rates
For the purpose of this paper injury rates will be reported as the number of injuries per 1000 athlete exposures (AE),9,11,23 with AE defined as one athlete participating in one basketball practice or game when he or she is exposed to the possibility of injury.3 Amongst high school athletes,13 overall injury rates for girls are reported at 2.08 per 1000 AE (3.66 and 1.43, respectively, for competition and practice) and 1.83 per 1000 AE (2.93 and 1.38, respectively, for competition and practice) for boys.
The National Collegiate Athletic Association (NCAA) reported an injury rate for men of 9.9 per 1000 AE for games and 4.3 per 1000AE for practices,9 while for women the injury rates were 7.68 per 1000 AE for games and 3.99 per 1000 AE practice.23 When comparing the period of the season (pre-season versus in-season), injury rates are higher in the pre-season for both practice and games. Dick et al9 reported that pre-season injury rate in practice was almost 3.0 times higher than in-season practice injury rate in NCAA men's basketball (7.5 versus 2.8 injuries per 1000 AE). Similar data is reported for female athletes,23 with pre-season practice injury rates more than twice as high as regular-season practice injury rates (6.8 versus 2.8 injuries per 1000 AE). The higher injury rates may be attributed to off-season deconditioning, increased training intensity and fatigue, inappropriate recovery, and pressure on players to earn starting positions.23 Collectively, with respect to playing position, the guard position accounted for the most injuries, followed by forward, and center.10,13
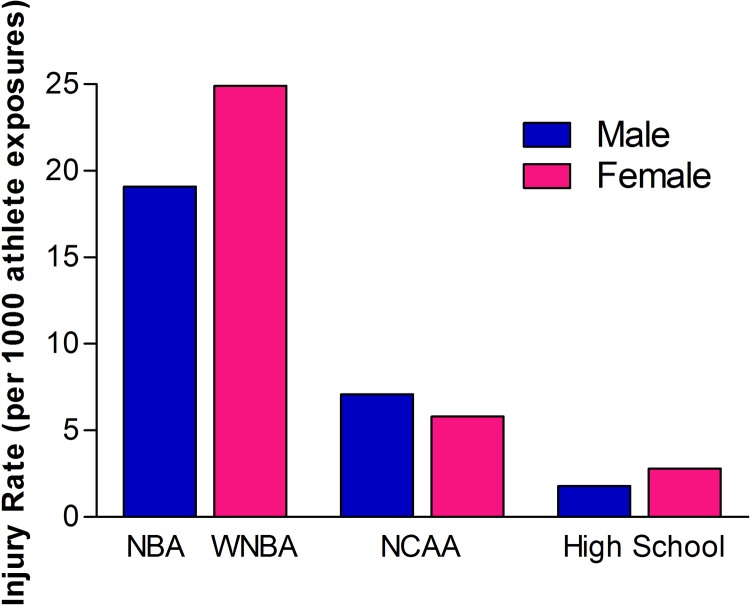
Much higher injury rates are reported during professional basketball in both the National Basketball Association (NBA) (19.1- 19.3 per 1000 AE),11,14 and Women's National Basketball Association (WNBA) (24.9 per 1000 AE).14 These injury rates are two-fold and three-fold higher, respectively, for men and women, than those reported in the NCAA. This may be explained by the combination of higher game intensity of the NBA/WNBA, with a more unpredictable and significantly greater physical competitive environment.9 Figure 1 displays injury rates with gender comparisons between NBA/WNBA, NCAA and high school basketball players.
Figure 1.
Injury rates (per 1000 athlete exposures). Gender comparisons between NBA/WNBA, NCAA and high school basketball players. Data combined for games and practices.9,11,13,14
NBA = National Basketball Association; WNBA = Women's National Basketball Association; NCAA = National Collegiate Athletic Association.
Injury Characteristics
At the three levels of competition reviewed (high school, NCAA, NBA/WNBA), sprains are the most commonly reported injury representing between 28% and 52% of total injuries reported (Table 1).9,11,13,14,23,24 Gender comparisons demonstrate little difference in the instance of sprain injuries between female and male athletes at the collegiate and professional level. For example, NCAA data indicates that sprains account for 31% of injuries in females,23 compared to 30% of injuries in male players,9 with similar data reported for professional players (30.4% WNBA versus 29.9% NBA).14 However, at the high school level when practice and game-related data are combined, female athletes suffer more sprains than males representing 56% of overall injuries in female players versus 47% in male players.24 Game-related data only reveals that sprains account for 49% of injuries in females and 45% of the injuries in males.13 Following sprains, in professional basketball (WNBA and NBA) overuse and inflammatory conditions accounted for 27% and 22% of injuries, respectively;14 while others25 have reported overuse and inflammatory conditions as high as 39% during a 32 week basketball season.
Table 1.
Common basketball injuries combined across levels (high school, collegiate, semi-professional and professional) of play and gender
| Injury classification | Occurrence (%) |
|---|---|
| Sprains | 28-52% |
| Overuse | 22-39% |
| Strains | 15-18% |
| Contusions | 8-25% |
| Fractures | 4-8% |
The most common region of injury, accounting for approximately two thirds of injuries in both games and practices, was the lower extremity,9,14,23 with ankle sprains being the most frequent injury associated with basketball games and practices at all levels of play. McKay et al26 highlight that nearly half (45%) of ankle injuries occurred during landing; with another third (30%) sustained during a cutting (twist/turn) maneuver. Knee internal derangements, specifically anterior cruciate ligament (ACL) injuries are the second most common injury in female athletes,23 and the most common injury requiring surgery in female high school basketball players.13 Agel and colleagues23 reported that injuries to the ACL accounted for 8% of all game injuries in women's basketball and of these, 64% occurred as a result of non-contact injury mechanisms. In a retrospective review of professional basketball (WNBA and NBA) over 6 seasons, Deitch et al14 reported that although the overall frequency of knee ligament injuries was low, the rate of ACL injury for women was 1.6 times greater than that of the men.
An emerging injury concern in basketball players is that of patellar tendinopathy,27 which can arise at a younger age than was previously thought.28 While the pathophysiology of chronic tendinopathy is not fully understood, patellar tendinopathy is characterised by activity-related anterior knee pain associated with focal patellar-tendon tenderness.29 Prevalence ranges from 7-26% in young players (14–18 years), 24% in asymptomatic collegiate basketball players,30 and 32% in elite basketball players.31 Furthermore, 55% of elite players reported current or previous symptoms of patella tendonopothy31 highlighting that rehabilitation professionals specifically involved with training basketball players should acquire a fundamental understanding of tendon pathology and the importance of exercise prescription in the management of athletes at risk as preventative measures,32 especially in youth athletes.28
Given the implications of repeated jump landing (eccentric loading) on athletes with patellar tendinopathy,33 and non-contact ACL injury mechanisms,23 screening how an athlete lands is an important consideration. For example asymptomatic athletes with a patellar tendon abnormality display an altered landing strategy.34,35 Edwards et al35 reported altered hip movement strategy in patellar tendon abnormality (PTA) athletes. During the stop–jump task landing, athletes with a PTA displayed altered sequencing by landing with significantly greater knee flexion and extending their hips, which in turn may increase the tensile and compressive loads on the proximal part of the patellar tendon and contribute to the development of patellar tendinopathy. Furthermore, hip range of motion (ROM), knee joint angle at initial contact during the stop–jump task landing, as well as quadriceps flexibility were recently reported34 as substantial predictors of the presence of PTA, with patellar tendinopathy severity determined via the Victorian Institute of Sport Assessment (VISA) Scale36, which may be used as an index of symptom severity (Appendix 1). Collectively, identification of altered landing strategies through an injury prevention through prediction screening framework34,37,38 could potentially identify those athletes who are at an increased risk of developing patellar tendinopathy and allow corrective movement strategies to be implemented.
Injury Prevention through Prediction
The ‘injury prevention through prediction’ approach aims to assess fundamental movement qualities in order to identify injury risk,34 as reduced movement quality is suggestive of higher injury risk,38 especially in youth athletes. Inclusion of movement competency assessment prior to performance testing may identify primary and secondary sources of movement dysfunction,39 which can lead to development of compensatory movement patterns,40 in turn leading to repeated micro trauma and muscular imbalances. By implementing an injury prevention through prediction framework, the rehabilitation professional can identify athletes at risk and introduce corrective exercises as part of a prehabilitation approach.7,41 Additionally, implementation of strategies such as functionally integrated movement preparation7 and prehabilitation41 is of value for injury risk reduction and performance enhancement.37,38 The rationale behind such strategies relates to the concept of movement rehearsal, which is commonly integrated into prehabilitation and rehabilitation programs for the purpose of reducing injury risk, especially targeting control of the lumbo-pelvic-hip complex.7,42-44 In following the injury prevention through prediction philosophy the authors have implemented injury prevention initiatives which are deemed to be practical risk modification strategies that may reduce injury rates, especially in youth athletes.34,45,46
MUSCULOSKELETAL SCREENING FOR INJURY PREVENTION
Movement Screening
Early reports of musculoskeletal screening aimed at injury risk reduction and improving athletic performance were centered on isolated assessments of muscular strength and flexibility as part of the pre-participation examination.18 However, such an approach to injury prevention did not assess the fundamental movement qualities related to athlete performance, as the body segments do not work in isolation during athletic movements. More recently, there has been a move away from such isolated assessments to integrated movement screening.15,16,37,38,47,48 Assessing an athlete's movement competency, or the ability to perform fundamental movements related to athletic performance is considered by many to be a more appropriate examination of an athlete's potential injury risk and readiness to train/compete.37,49 This integrated movement screening approach for injury prevention through prediction and performance enhancement assesses force interplay characteristics7 along the mobility/stability continuum, allowing determination of primary and secondary sources of movement dysfunction.38 While several movement screens have been developed to examine asymmetries in fundamental movement qualities,15,16,38,47 there appear to be three frequently reported considerations for physical therapists, athletic trainers and rehabilitation professionals; 1) time restraints when conducting movement screening on larger numbers of athletes; 2) does the movement screen assess the athletic movement patterns commonly seen in a competitive environment? and 3) will the movement screen data provide specific exercise prescription information to assist in determining athlete loading parameters?
With this in mind, the Australian Institute of Sport (AIS), in consultation with Basketball Australia,50,51 developed a comprehensive basketball-specific movement screen that include five primary movement screens and four supplementary tests (Table 2). Each of the five primary movement screens have been described elsewhere.37,52,53 The primary movement screens are subjectively scored on a scale of 1 to 3 (1 = cannot complete exercise without major flaws; 2 = can complete exercise but with some minor flaws; 3 = can execute exercise with technical proficiency). Therefore, the maximum score (15 points) would be awarded to a technically proficient athlete demonstrating no flaws, with the criterion cut-off score of less than 12 points (80%) classified as a fail.50 Additionally, the athlete is required to successfully pass the supplementary tests by completing the suggested repetitions/time while demonstrating good technique. The above-mentioned basketball-specific movement screen and supplementary tests aim to identify functional limitations throughout the kinetic chain and sport-specific performance characteristics (core stability, muscular strength, balance, coordination). For example, poor results during the single-leg glute bridge may be attributed low back or hamstring pain54 due to lumbar extensor substitution or contralateral pelvic drop. The Broomstick overhead squat can indicate limited strength and mobility of the glenohumeral joint, thoracic spine and flexion of the hips and dorsiflexion of the ankles.38 Likewise, poor performance during the Push up test may suggest reduced scapular control and/or a lack of trunk stability.55 However, the injury predictive ability and criterion cut-off score of the AIS basketball-specific movement screen is yet to be investigated.
Table 2.
Basketball-specific movement screen - Australian Institute of Sport/Basketball Australia
| Primary movement screens | Supplementary tests |
|---|---|
| 1) Back squat with dowel | 1) Single-leg glute bridge – 12 repetitions @ |
| 2) Overhead squat with dowel | 2) Push-up – 6 repetitions |
| 3) In-line lunge with dowel | 3) Prone plank hold – 1 minute |
| 4) Box drop to landing - 30cm box | 4) Single leg calf rise – 20 repetitions @ |
| 5) Single-leg hop plus stick landing |
Primary movement screens: 5 repetitions are performed for each screen with screens 3 and 5 performed on both left and right sides. Supplementary tests: Repetitions are outlined for each test with tests 1 and 4 performed on both left and right sides. Abbreviations: @ = each side. Source: Legg.50
Hop and Jump Assessments
Given the dynamic movement patterns in basketball, which involve multiple directional changes (vertical, horizontal, and/or lateral) and jump landings, the assessment of an athlete's lower extremity neuromuscular control through multidirectional hop and jump assessments have received significant research interest.56-59 Hewett and colleagues60 recommend that in high-risk jumping and cutting sports, such as basketball, youth athletes need to demonstrate proficiency in neuromuscular performance of such skills. This is of significant importance given that in basketball repetitive directional changes are not always performed using a bilateral take-off or landing.57 The use of multidirectional hop and jump assessments may allow for greater observation of muscle imbalances that could affect the success of the movement pattern, thereby providing rehabilitation professionals with data that can be used for both training program design and monitoring, and/or assessment of neuromuscular control deficits and injury risk.
Several hop and jump assessments are described in the literature as reliable, inexpensive, and easily administered measures of neuromuscular control in both athletic and rehabilitation populations. These include hop tests,56,61,62 landing error scoring system (LESS),63-65 and tuck jump assessment.58,66 Commonly reported neuromuscular control deficits observed in athletes during hop and jump assessments include high-force landings and bilateral imbalances in landing force,60 limb dominance-related issues [ligament dominance, quadriceps dominance, leg dominance, for extensive review see Myer et al67], excessive valgus knee position (medial knee collapse),68 and trunk dominance. Commonly used hop and jump assessments recommended for basketball athletes are described below.
Four Functional Hop Test Combination
The four functional hop test combination provide valuable information when assessing strength, power, and neuromuscular control of the lower extremity.69 Importantly, such tests allow observation of the lower extremity under eccentric loading and quantification of the limb symmetry index. A limb symmetry index score of less than 85% is considered abnormal.70,71 The following instructions outline how to conduct the four functional hop test combinations56,61,62,72 displayed in Figure 2.
Figure 2.
Functional hop tests. A, Single-leg hop for distance; B, Triple hop for distance; C, Crossover triple hop for distance; D, 6-metereter one-legged timed hop. Adapted from Cates and Cavanaugh.56
How to Conduct the Four Functional Hop Test Combination
Single-leg Hop for Distance (Figure 2a). The athlete stands on the designated testing leg, with their toe on the starting line and instructed to hop as far as possible forward and land on the same leg. Measure the distance hopped from the starting line to the point where the athlete's heel lands. The athlete is encouraged to ‘stick and hold’ the landing position with control and minimal body sway for a minimum of three seconds.
Triple Hop for Distance (Figure 2b). Athletes begin standing on the designated testing leg, with their toe on the starting line and are instructed to take three maximal hops forward with the designated leg. Measure the distance hopped from the starting line to the point where the athlete's heel lands on completing the third hop. Encourage the athlete to ‘stick and hold’ the final landing position with control and minimal body sway for a minimum of three seconds.
Crossover Triple Hop for Distance (Figure 2c). Athletes begin by standing on the same side of the centre tape as the designated testing leg, with their toe on the starting line. For example, if athletes were hopping with their right leg, stand on the right side of the tape. Athletes are instructed to take three consecutive maximal hops forward with the designated leg, crossing over the strip of tape each time in a zig-zag pattern. Measure the distance hopped from the starting line to the point where the athlete's heel lands on completing the third hop. Athletes’ are encourage to ‘stick and hold’ the final landing position with control and minimal body sway for a minimum of three seconds.
Six-meter One-legged Timed Hop (Figure 2d). Athletes’ begin standing on the designated testing leg, with their toe on the starting line. On the command of “3, 2, 1, go” the athlete hops the 6-meter distance as quickly as possible with the designated leg. Timing ends when the athlete crosses the 6-meter finish line.
Landing Error Scoring System (LESS)
The landing error scoring system (LESS) is reported to be a reliable screening tool63 developed to identify individuals at increased risk for non-contact ACL injury through evaluation of landing mechanics associated with the drop box vertical jump (DBVJ) test.63-65 The LESS evaluates 17 jump-landing characteristics following a DBVJ test and is scored by reviewing a recorded video of the jump landing task. A higher LESS score indicates poor technique in jump landing; a lower LESS score indicates better jump-landing technique.63 Most recently, Padua and colleagues73 reported that elite youth soccer players with LESS scores of five or more were at a higher risk for sustaining ACL injuries than athletes with LESS scores less than five, suggesting that five was the optimal cut-off point for the LESS for elite youth field and court sport athletes. However, a practical limitation for rehabilitation professionals is that the LESS is not assessed in real time and requires the use of video cameras. This led to the development of the Landing Error Scoring System-Real Time (LESS-RT),65 which examines 10 jump-landing characteristics (Table 3) and is scored over four trials of the jump-landing task.
Table 3.
Definitions of Individual Items in the LESS-REAL TIME (LESS-RT)
| LESS-RT item | Definitions | Example Score | View position | Jump trial which item is scored |
|---|---|---|---|---|
| 1. Stance width | If the subject lands with a wide or narrow stance when evaluated from the frontal plane, he/she receives an error. An error is only scored if the stance is observed to be very wide or very narrow (+1). | +1 | Front | Jump trial 1 |
| 2. Maximum foot-rotation position | If a subject's feet are moderately externally rotated or slightly internally rotated at any point during the jump landing, he/she receives an error (+1). | +1 | Front | Jump trial 1 |
| 3. Initial foot-contact symmetry | If one foot lands before the other or if one foot lands heel-to-toe and the other lands toe-to- heel, the subject receives an error (+1). | 0 | Front | Jump trial 1 |
| 4. Maximum knee-valgus angle | If the subject moves into a small amount of knee valgus, he/she receives an error (+1). If the subject moves into a large amount of knee valgus, he/she receives an error (+2). | +1 | Front | Jump trial 2 |
| 5. Amount of lateral trunk flexion | If the subject is leaning to the right or left side so that the trunk is not vertical in the frontal plane, he/she receives an error (+1). | +1 | Front | Jump trial 2 |
| 6. Initial landing of feet | If the subject lands heel to toe or with a flat foot, he/she receives an error (+1). | 0 | Side | Jump trial 3 |
| 7. Amount of knee-flexion displacement | If the subject goes through a small (+2) or average amount (+1) of knee flexion displacement, he/she receives an error. | +1 | Side | Jump trial 3 |
| 8. Amount of trunk-flexion displacement | If the subject goes through a small (+2) or average amount (+1) of trunk flexion displacement, he/she receives an error. | +1 | Side | Jump trial 4 |
| 9. Total joint displacement in the sagittal plane | If the subject goes through large displacement of the trunk and knees, then score soft (0). If the subject goes through an average amount of trunk and knee displacement, then score average (+1). If the subject goes through a small amount of any trunk and knee displacement, then score stiff (+2). | 0 | Side | Jump trial All |
| 10. Overall impression | Score excellent (0) if the subject displays a soft landing and no frontal-plane motion at the knee. Score poor (+2) if the subject displays a stiff landing and large frontal-plane motion at the knee, or only large frontal-plane motion at the knee. All other landings, score average (+1). | +1 | N/A | Jump trial All |
| Adapted from Pudua and colleagues65 | LESS TOTAL | +7 | Note: A lower score is better | |
How to conduct the LESS-RT
The athlete begins standing on a 30-cm-high box placed at a distance of half the body height away from a target landing area, which is marked on the ground;
Instruct the athlete to jump forward so that both limbs leave the box simultaneously, to land in target landing area, and to jump as high as they can after their initial landing from the box;
- A successful jump is characterized by the following as outlined in the LESS-RT scoring sheet65 presented in Table 4;
- both feet simultaneously leaving the box;
- jumping forward off the box without a large upward motion after take-off from the box to reach the target landing area below; and
- completing the jump in a fluid motion (no pause in movement of body's center of mass after making contact with the ground until take-off for subsequent jump).
If a jump is unsuccessful the athlete repeats the DBVJ without additional instructions.
Table 4.
Scoring sheet for the Landing Error Scoring System-Real Time (LESS-RT)
| Frontal plane motion | Sagittal plane motion |
|---|---|
1. Stance width
|
1. Initial landing of feet
|
2. Maximum foot rotation position
|
2. Amount of knee flexion displacement
|
3. Initial foot contact
|
3. Amount of trunk flexion displacement
|
4. Maximum knee valgus angle
|
4. Total joint displacement in sagittal plane
|
5. Amount of lateral trunk flexion
|
5. Overall impression
|
Adapted from Pudua and colleagues65
The Tuck Jump Assessment
Given the repetitive jump and landing actions in basketball, the tuck jump assessment, as suggested by Myer and colleagues,58 may be useful for the identification of lower extremity jump and landing error technique. Insufficient neuromuscular control of lower limb biomechanics, particularly the knee joint, may predispose youth athletes, especially female athletes, to higher injury risk. The tuck jump assessment challenges muscular force interplay characteristics of the lower extremity,7 including explosive triple extension of the hips, knees, and ankles on take-off, force absorption through the hips, knees, and ankles on landing, and utilization of the stretch shortening cycle.58 Extensive work by Myer and colleagues44,46,58,74,75 highlights the practical application of the tuck jump assessment in identifying lower extremity dysfunction such as decreased neuromuscular control, trunk dominance, high risk landing patterns, excessive knee valgus, and increased risk of anterior cruciate ligament injury. The tuck jump assessment may also be used as a monitoring tool to track changes in dynamic lower extremity biomechanics76 by addressing four fundamental areas: 1) correct posture (i.e., chest over knees) throughout the jump, 2) following a purely vertical trajectory without any medial/lateral or anterior/posterior deviations, 3) soft landings, including toe-to-heel rocking and bent knees, and 4) instant recoil preparation for the next jump. Criteria may be grouped into the neuromuscular risk factor dominance categories58,77 presented in Table 5
Table 5.
The Tuck Jump Assessment criteria
| Tuck Jump Assessment | Errors | Neuromuscular deficits | Comments |
|---|---|---|---|
| Knee and thigh motion | |||
| 1. Lower extremity medial knee collapse landing | □ | Ligament dominance | |
| 2. Thighs do not reach parallel at peak jump height | □ | Trunk dominance/core dysfunction | |
| 3. Thighs not equal side-to-side during jump flight | □ | Leg dominance/residual injury deficit | |
| Foot position during landing | |||
| 4. Foot placement not shoulder width apart | □ | Ligament dominance | |
| 5. Foot placement not parallel (front to back) | □ | Leg dominance/residual injury deficit | |
| 6. Foot contact timing not equal | □ | Leg dominance/residual injury deficit | |
| 7. Excessive landing contact noise | □ | Quadriceps dominance | |
| Plyometric technique | |||
| 8. Pause between jumps | □ | Trunk dominance/core dysfunction | |
| 9. Does not land in same footprint (deviation in flight) | □ | Trunk dominance/core dysfunction | |
| 10. Technique declines prior to 10 s | □ | ||
| Total errors | |||
 | |||
Note: Score any deviations from correct performance before, during, and after the performance of several tuck jumps over 10 seconds. More checked boxes indicates poorer technique, and also suggests the areas upon which the athlete should concentrate during training. Adapted from Myer and colleagues.58,77 Image taken by SPB. Basketball WA High Performance Program.
How to Conduct the Tuck Jump Assessment
The athlete starts in an athletic stance position with feet shoulder width apart. Initiate the jump with a slight crouch downward while extending their arms behind the body.
Simultaneously jumping and swinging the arms forward the athlete pulls the knees up toward the chest as high as possible. Knees should be parallel at the top of the jump.
Landing softly on the toes, the athlete should immediately attempt the next tuck jump.
Repetitions should be performed with maximal effort and as quickly as possible for 10 seconds. The test is terminated if the athlete cannot control the high landing force or if they demonstrate excessive knee valgus on landing.
Ankle Dorsiflexion Range of Motion: Weight-Bearing Lunge Test (WBLT)
In sports such as basketball, poor landing technique has been linked to both initial injury and re-injury.78 Risk for such injuries may be reduced by identifying key characteristics that inhibit correct landing technique. The amount of ankle dorsiflexion range of motion (ROM), as well as the strength of the muscles performing plantar flexion are considered the most important components in the shock absorption phase during landing.79 Restricted ankle dorsiflexion ROM during landing is accompanied by decreased knee-flexion and hip-flexion resulting in “stiff” landings characterized by an erect landing posture and diminished sagittal-plane movement of the LE's resulting in greater ground reaction forces.80 Such biomechanical factors are considered risk factors for anterior cruciate ligament (ACL) injury, and Fong et al80 reported that greater passive ankle dorsiflexion ROM was not only associated with greater knee-flexion movement but also smaller ground reaction forces during jump landing, which reduces strain on the skeletal structures as well as injury risk.
Basketball players lacking adequate ankle dorsiflexion ROM are nearly five times more likely to reinjure an ankle after a prior ankle injury.26 Backman and Danielson79 reported that ankle dorsiflexion ROM less than 36.5 degrees, as measured by a gravity inclinometer, predisposes elite junior basketball player to patellar tendinopathy. Hoch and colleagues81 reported a significant moderated correlation (r = 0.53; p < 0.001) between ankle dorsiflexion ROM and Star Excursion Balance Test - anterior reach (SEBT-AR) in healthy adults with no history of lower extremity injury. Hoch et al82 confirmed that patients with chronic ankle instability (CAI) demonstrated significantly less ankle dorsiflexion ROM and impairments in dynamic postural control compared to healthy controls. The authors concluded that ankle dorsiflexion ROM significantly influences dynamic balance, highlighting the importance of assessing ankle dorsiflexion ROM. A simple and practical measure of ankle dorsiflexion ROM is the weight-bearing lunge test (WBLT),83-85 which has been reported to have excellent inter-tester and intra-tester reliability.84 The WBLT method utilizes the knee-to-wall principle85 with the athlete placing the foot perpendicular to a wall and lunging forward so the knee touches the wall (Figure 3). Therefore, we recommend that the WBLT be included in the musculoskeletal screen for basketball athletes.
Figure 3.
The weight-bearing lunge test to evaluate ankle dorsiflexion range of motion. The foot must remain flat on the ground. Image taken by SPB. Basketball WA High Performance Program.
How to Conduct the Weight-Bearing Lunge Test
The athlete places the test foot on a tape measure perpendicular to the wall and lunges forward so the knee touches the wall;
The heel should not be lifted off from the floor, and the subtalar joint should be locked. Look out for exaggerated hip flexion and inhibited knee flexion;
The foot is sequentially moved further away from the wall until knee can only make slight contact with the wall while the foot remains flat on the ground;
This position is maximum ankle dorsiflexion ROM and the distance from the great toe to the wall is measured in centimeters (each centimeter corresponds to approximately 3.6 degrees of ankle dorsiflexion);84
Star Excursion Balance Test and Y-Balance Test
The Star Excursion Balance Test (SEBT) is a multidirectional test of static balance and dynamic postural control that involves balancing on one leg and reaching maximally with the other leg in eight different directions including three anterior, two lateral, and three posterior.86 The SEBT is commonly used in athletic research settings 87-91 during assessment of key characteristics of static and dynamic balance, including ankle dorsiflexion, knee flexion, and hip flexion ranges of motion and strength, proprioception, and neuromuscular control. The SEBT is a sensitive and valid musculoskeletal screening tool,87,90,92 with reduced SEBT performance evident in conditions such as chronic ankle instability,92 anterior cruciate ligament (ACL) deficiency,93 and patellofemoral pain syndrome.94 Test-retest reliability and response stability of the SEBT ranges from 0.89 to 0.93 with method error coefficient of variation of 3.0% to 4.6%, suggesting good measurement stability.87
The SEBT protocol can be time-consuming due to the number of trials required for each of the eight directions (six practice attempts, three test trials).95 As such, Hertel and colleagues96 argue that there is redundancy in testing all eight reach directions, with the modified three direction SEBT (referred to as the Y Balance Test) more applicable. The Y-Balance Test (YBT) incorporates three reach components of the SEBT (anterior, posteromedial and posterolateral)97,98 with research primarily focused on reach asymmetries and composite score which can be used to identify potential injury risks in athletic populations.87
The SEBT/YBT appear to be valuable musculoskeletal screens that contribute to the identification of movement dysfunction in basketball players. Bressel et al91 reported that NCAA Division I female basketball players display both inferior static balance compared with gymnasts and impaired dynamic balance compared with soccer players as determined by the SEBT. Additionally, Plisky et al87 predicted lower extremity injuries in high school basketball athletes by utilizing a modified-SEBT (3 reach directions - anterior, posteromedial and posterolateral). The authors reported that high school basketball players with right versus left lower extremity anterior reach differences greater than 4cm were 2.5 times more likely to sustain a lower extremity injury. Females with a composite reach distance less than 94% of their limb length were 6.5 times more likely to sustain a lower extremity injury.87 Therefore, the practical relevance of the SEBT/YBT for physical therapists, athletic trainers and rehabilitation professionals’ centers on its potential application as a prediction tool to identify functional deficits related to the trunk and lower extremity.
Analyzing total reach distance normalized to the limb length (reach distance/leg length) x100, and calculating total composite score (sum of the best reach distance for the three directions) divided by three times the leg length allows identification of high-risk athletes, and individualization of corrective strength and conditioning training programs. Additionally, this data may be used to as part of a return to play criteria for athletes following lower extremity injury, with the achievement of minimum standards required before returning to on-court training or competitive drills. For example, an athlete must achieve a limb symmetry score of less than 4 cm difference between lower extremities in the anterior reach direction.87,92 Finally, a recent systematic review of measurement properties and correlation with injury by Hegedus and colleagues99 reported that there is strong evidence that the modified three-direction SEBT/YBT can identify injury risk in field and court sport athletes, with both a composite reach score difference of less than 94% and an anterior reach difference of 4 cm or greater being associated with increased injury risk. As such, we recommend that the YBT be incorporated as a musculoskeletal screening assessment. Additionally, the YBT could be prescribed as a balance and postural stability movement preparation task7 to develop hip strength, postural awareness, and proprioception potentially reducing risk of lower extremity injury.88
How to Conduct the Modified Three-direction SEBT and Y Balance Test
Modified Three-direction SEBT
Construct a “Y” by securing three tape measures tape on the ground, one oriented anteriorly (ANT) to the apex and the other two aligned at 135 degrees to this in the posteromedial and posterolateral directions (Figure 4).100 Each length of tape should be between 1.8-2.5m;101
Instruct the athlete to stand in the center of the Y barefoot with an equal portion of the stance foot to the anterior and posterior of the middle of the Y (this is a fixed position for all three reach attempts) while performing series of maximal reaches along the three vectors with the opposite leg without compromising the base of support;96,100
Using the most distal part of the foot of the reach limb, touch the ground lightly with the toes without bearing weight through the reach limb and return to a standing position at the start;
Maximum reach distances are measured from the start point to the point of maximum reach at the toe.
Figure 4.
The testing order of the SEBT/YBT with reach directions labelled in reference to right (R) stance foot (a) anterior, (b) posteromedial, and (c) posterolateral.
Y-Balance Test (Lower quarter)
Have the athlete stand on the elevated central footplate with the great toe lined up with the red line on the commercially available YBT device (Y Balance Test, Move 2 Perform, Evansville, IN);
The athlete pushes the reach block with the foot in each of the three directions by touching the side of the reach plate and not bearing weight on the reaching limb;
The maximum reach distance is recorded as the point at which the reach block rested when the subject had returned to the start position after carrying out the reach. The subject is not allowed to accelerate the reach block.
Instruct the athlete to complete a familiarization trial for all three targets on both legs. Given the times contraints placed on rehabilitation professionals, the authors support the recommendation in reducing the number of practice attempts from six to four in a group/team setting.95 A trial is classified as invalid if the participant removed the hands from the hips, did not return to the start position, applied sufficient weight through the reach foot so as to gain an increase in reach distance (SEBT), placed the reach foot on the ground either side of the line or tube, raised or moved the stance foot during the test, or kicked the plate with the reach foot to gain more distance (YBT).96,100
For the most accurate results Gribble et al102 suggested that the recorded reach scores should be normalized in relationship to limb length. This is recommended in a group setting to better compare individual athletes’ scores and diminish the influence of height on reach distance. The athlete's limb length is measured (using a standard tape measure) from the anterior superior iliac spine (ASIS) to the middle of the medial malleolus while the subject is supine.89 Scores are normalized to limb length by calculating the maximal reach distance (%MAXD) using the formula (Reach distance/limb length) × 100 = % MAXD.102 In addition, the composite score is determined by adding the greatest reach attempt from all three directions and dividing this sum by three times the limb length to provide a comprehensive overview of the athlete's overall performance on the test. Consideration must be given to the fact that reach distances are likely affected by which sport the athlete participate in and by gender. We recommend that the YBT comparisons occur with norms by gender and sport. Table 6 presents suggested normative reach values for athletes performing the YBT based on our previous work with elite surfers.98
Table 6.
Reach distance values for athletes performing the Y-Balance Test
| Directions | Reported Values | Normalized Reach Scores | Recommended Standard | |||
|---|---|---|---|---|---|---|
| Plisky et al.87 | de Noronha et al.113 | Plisky et al.114 | Plisky et al.87 | Plisky et al.114 | ||
| Anterior (cm) | 78.2 ± 8.2 | 83.5 ± 7.0 | 72.9 ± 5.8 | 83.9 ± 7.1% | 78.3 ± 3.9% | 81 |
| Posteromedial (cm) | 107.0 ± 11.7 | 85.5 ± 9.7 | 114.9 ± 7.3 | 113.4 ± 9.7% | 123.5 ± 5.0% | 118 |
| Posterolateral (cm) | 100.4 ± 12.0 | 89.8 ± 9.7 | 112.3 ± 6.5 | 106.4 ± 10.8% | 120.8 ± 5.3% | 113 |
| Composite Score (%) | 100.9 ± 8.4% | 107.5 ± 3.5% | 104 | |||
Balance Error Scoring System
The Balance Error Scoring System (BESS) evaluates static bilateral and unilateral balance qualities on firm and unstable surfaces, consisting of three stances: double-leg stance (hands on the hips and feet together), single-leg stance (standing on the nondominant leg with hands on hips), and tandem stance (nondominant foot behind the dominant foot).103 Balance tests are performed on a firm surface and/or a foam surface with the eyes closed. Errors are counted during each 20-second trial with errors defined as opening the eyes, lifting the hands off hips, stepping, stumbling or falling out of position, lifting the forefoot or heel, abducting the hip by more than 30 degrees, or failing to return to the test position in more than five seconds.103,104 The BESS has primarily been used to identify individuals with functional ankle instability amongst collegiate athletes;105 while more recently there is interest in the BESS as a sideline environment concussion testing tool for assessing an athlete's balance abilities.106 The BESS is reported to have moderate to good reliability (intraclass correlations 0.87-0.98)107 in assessing static balance. However, from a practical perspective the two-legged stance position may be redundant as it failed to illustrate significant variance. Hunt and colleagues108 found that removing the two leg stance improved the reliability of the BESS and resulted in an intraclass reliability coefficient of 0.88.
Poor static balance performance and increased postural sway measures have been associated with higher incidence of ankle sprains in high school basketball players. McGuine and colleagues109 utilized a modified BESS (Romberg test, barefoot) while on a force platform (NeuroCom, Clackamas, OR) to quantify postural sway velocity (the distance, measured as degrees of sway [°S] of the center of gravity away from the stable position per time) in 210 high school basketball athletes (119 male, 91 female). Each trial was performed for 10 seconds, with the total °S produced during the trial divided by 10 to produce a score represented as COG degrees of sway per second (°S/S). The authors found that players with higher postural sway scores (poor static balance) had nearly seven times as many ankle sprains than those with better postural control.109 Conversely, players with low-sway scores (good balance) may have an enhanced risk reduction mechanism (Figure 5).
Figure 5.
Distribution of ankle sprain injuries per 1,000 exposures according to compilation sway balance scores between the low-sway, mod-sway, and high-sway groups (p = 0.0002). Figure adapted from McGuine and colleagues.109
How to Conduct the Modified Balance Error Scoring System
Have the athlete complete the test under four conditions (2 stance positions – (i) tandem stance: non-dominant foot behind dominant foot; and (ii) single leg stance) on 2 surfaces (firm/flat surface and a foam surface);
For each test condition the subject close his or her eyes and record the number of errors observed in 20 seconds;
Errors include opening the eyes, taking the hands off hips, any movement from initial stance position (stumble, step), lifting the forefoot or heel, excessive hip rotation in non-stance leg (abducting hip by > 30 °) or not returning to test position in a time period of five seconds;110
The average of three trials be used to enhance reliability of the test and to familiarize the athlete;
Table 7 describes the stance positions and the measurement associated with each position. We recommended rehabilitation professionals video record each test and review the video and revise the score at a later date for greatest accuracy.
Table 7.
Description of stance positions for the Balance Error Scoring System.
| Stance Position | Description | Measurement |
|---|---|---|
1. Two-Legs
|
|
Count/record number of errors in 20 seconds |
2. Tandem
|
|
Count/record number of errors in 20 seconds |
3. Single-leg
|
|
Count/record number of errors in 20 seconds |
PRACTICAL APPLICATIONS
Of importance to rehabilitation professionals is the establishment of valid and reliable pre-participation musculoskeletal screening and functional testing protocols56,111 aimed at identifying injury risk in athletes. This must take into consideration not only the sport-specific game demands but also the developmental stage of the athlete.38 Given the potential influence of force interplay characteristics7 on postural demands during basketball game-play situations that frequently involve high intensity change of directions, dynamic tests that challenge postural control and balance allow identification of movement limitations in basketball athletes compared to isolated assessments of muscle function. Collectively, the musculoskeletal screens and functional performance tests described in this clinical commentary may allow easy identification of inefficient and/or compensatory movement tendencies in athletes, and provide an inexpensive and practical means in determining athletes that may be at risk.111 The recommended protocols are not limited to rehabilitation professionals during pre-participation screening, such an approach to musculoskeletal screening and functional performance may also be useful during and following rehabilitation in determining readiness to return to sport. While the authors have employed such protocols with elite youth and elite senior male and female athletes as part of a multidisciplinary approach to injury prevention, further studies with athletes from different sports and of various ages are required to quantify the relationships between pre-participation musculoskeletal screening results, functional performance testing, and injury risk. This clinical commentary offers evidence informed choices for a battery of musculoskeletal screens and functional performance tests used by the authors from a basketball-specific perspective. The authors acknowledge that there is limited research to support or refute their combined use specifically for basketball athletes.
Appendix 1.
Victorian Institute of Sport Assessment (VISA) Scale - Index of Symptoms Severity
 |
Note: maximal VISA score for an asymptomatic, fully performing individual is 100 points. Adapted from Visentini et al.36
REFERENCES
- 1.International Basketball Federation. Quick facts. Available at: http://www.fiba.com. Accessed Feb 11 2013.
- 2.Basketball Australia. Key facts: Update 2012. Sydney: Basketball Australia (BA) 2012. [Google Scholar]
- 3.Hoffman J R. Epidemiology of basketball injuries. In: Douglas BM, ed. Handbook of Sports Medicine and Science: Basketball; 2008: 3-11. [Google Scholar]
- 4.Stapff A. Protocols for the physiological assessment of basketball players. Physiological tests for elite athletes. Champaign: IL: Human Kinetics; 2000. [Google Scholar]
- 5.Drinkwater EJ Pyne DB McKenna MJ. Design and interpretation of anthropometric and fitness testing of basketball players. Sports Med. 2008;38:565-578. [DOI] [PubMed] [Google Scholar]
- 6.McInnes SE Carlson JS Jones CJ, et al. The physiological load imposed on basketball players during competition. J Sports Sci. 1995;13:387-397. [DOI] [PubMed] [Google Scholar]
- 7.Bird SP Stuart W. Integrating balance and postural stability exercises into the functional warm up for youth athletes. Strength Cond J. 2012;34:73-79. [Google Scholar]
- 8.Ostojic SM Mazic S Dikic N. Profiling in basketball: Physical and physiological characteristics of elite players. J Strength Cond Res. 2006;20:740-744. [DOI] [PubMed] [Google Scholar]
- 9.Dick R Hertel J Agel J, et al. Descriptive epidemiology of collegiate men's basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42:194-201. [PMC free article] [PubMed] [Google Scholar]
- 10.Henry JH Lareau B Neigut D. The injury rate in professional basketball. Am J Sports Med. 1982;10:16-18. [DOI] [PubMed] [Google Scholar]
- 11.Drakos MC Domb B Starkey C, et al. Injury in the National Basketball Association: a 17-year overview. Sports Health. 2010;2:284-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simenz CJ Dugan CA Ebben WP. Strength and conditioning practices of National Basketball Association strength and conditioning coaches. J Strength Cond Res. 2005;19:495-504. [DOI] [PubMed] [Google Scholar]
- 13.Borowski LA Yard EE Fields SK, et al. The epidemiology of US High School basketball injuries, 2005–2007. Am J Sports Med. 2008;36:2328-2335. [DOI] [PubMed] [Google Scholar]
- 14.Deitch JR Starkey C Walters SL, et al. Injury risk in professional basketball players: A comparison of women's National Basketball Association and National Basketball Association athletes. Am J Sports Med. 2006;34:1077-1083. [DOI] [PubMed] [Google Scholar]
- 15.Cook G Burton L Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function – Part 1. N Am J Sports Phys Ther. 2006;1:62-72. [PMC free article] [PubMed] [Google Scholar]
- 16.Cook G Burton L Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function – Part 2. N Am J Sports Phys Ther. 2006;1:132-139. [PMC free article] [PubMed] [Google Scholar]
- 17.Conley KM Bolin DJ Carek PJ, et al. National Athletic Trainers’ Association position statement: Preparticipation physical examinations and disqualifying conditions. J Athl Train. 2014;49:102-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kibler WB Chandler TJ Uhl T, et al. A musculoskeletal approach to the preparticipation physical examination: Preventing injury and improving performance. Am J Sports Med. 1989;17:525-531. [DOI] [PubMed] [Google Scholar]
- 19.Headlee D Nord W Huntington MK. Preparticipation physical evaluations in youth sports: A systematic review of current recommendations. South Dakota Medicine. 2014;67:273-277. [PubMed] [Google Scholar]
- 20.Legault ÉP Descarreaux M Cantin V. Musculoskeletal symptoms in an adolescent athlete population: a comparative study. BMC Musculoskel Disord. 2015;16:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Metzl JD. Preparticipation Examination of the Adolescent Athlete: Part 2. Pediatr Rev. 2001;22:227-239. [DOI] [PubMed] [Google Scholar]
- 22.Gonzalo-Skok O Serna J Rhea MR, et al. Relationships between functional movement tests and performance tests in young elite male basketball players. Int J Sports Phys Ther. 2015;10:628-638. [PMC free article] [PubMed] [Google Scholar]
- 23.Agel J Olson DE Dick R, et al. Descriptive epidemiology of collegiate women's basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42:202-210. [PMC free article] [PubMed] [Google Scholar]
- 24.Messina DF Farney WC DeLee JC. The incidence of injury in Texas high school basketball. A prospective study among male and female athletes. Am J Sports Med. 1999;27:294-299. [DOI] [PubMed] [Google Scholar]
- 25.Cumps E Verhagen E Meeusen R. Prospective epidemiological study of basketball injuries during one competitive season: ankle sprains and overuse knee injuries. J Sports Sci Med. 2007;6:204-211. [PMC free article] [PubMed] [Google Scholar]
- 26.McKay GD Goldie PA Payne WR, et al. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35:103-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cook JL Khan KM Kiss ZS, et al. Reproducibility and clinical utility of tendon palpation to detect patellar tendinopathy in young basketball players. Victorian Institute of Sport tendon study group. Br J Sports Med. 2001;35:65-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cook JL Khan KM Kiss ZS, et al. Patellar tendinopathy in junior basketball players: a controlled clinical and ultrasonographic study of 268 patellar tendons in players aged 14-18 years. Scand J Med Sci Sports. 2000;10:216-220. [DOI] [PubMed] [Google Scholar]
- 29.Warden SJ Brukner P. Patellar tendinopathy. Clin Sports Med. 2003;22:743-759. [DOI] [PubMed] [Google Scholar]
- 30.Major NM Helms CA. MR imaging of the knee: Findings in asymptomatic collegiate basketball players. Am J Roentgenol. 2002;179:641-644. [DOI] [PubMed] [Google Scholar]
- 31.Lian O Engebretsen L Bahr R. Prevalence of jumper's knee among elite athletes from different sports. Am J Sports Med. 2005;33:561-567. [DOI] [PubMed] [Google Scholar]
- 32.van der Worp H van Ark M Roerink S, et al. Risk factors for patellar tendinopathy: a systematic review of the literature. Br J Sports Med. 2011;45:446-452. [DOI] [PubMed] [Google Scholar]
- 33.Cook JL Purdam CR. Rehabilitation of lower limb tendinopathies. Clin Sports Med. 2003;22:777-789. [DOI] [PubMed] [Google Scholar]
- 34.Mann K Edwards S Drinkwater EJ, et al. A lower limb assessment tool for athletes at risk of developing patellar tendinopathy. Med Sci Sports Exerc. 2013;45:527-533. [DOI] [PubMed] [Google Scholar]
- 35.Edwards S Steele JR McGhee DE, et al. Landing strategies of athletes with an asymptomatic patellar tendon abnormality. Med Sci Sports Exerc. 2010;42:2072-2080. [DOI] [PubMed] [Google Scholar]
- 36.Visentini PJ Khan KM Cook JL, et al. The VISA score: An index of severity of symptoms in patients with jumper's knee (patellar tendinosis). Victorian Institute of Sport Tendon Study Group. J Sci Med Sport. 1998;1:22-28. [DOI] [PubMed] [Google Scholar]
- 37.Nessler T. Using movement assessment to improve performance and reduce injury risk Int J Athl Ther Train. 2013;18:8-12. [Google Scholar]
- 38.Moore NR Kertesz AHM Bird SP. A modified movement screen for pre-elite youth athletes. J Aust Strength Cond. 2012;20:44-53. [Google Scholar]
- 39.Cook G. Weak links: screening an athlete's movement patterns for weak links can boost your rehab and training effects. Training and Conditioning. 2002;12:29-37. [Google Scholar]
- 40.Page P. Sensorimotor training: A “global” approach for balance training. J Bodywork Movement Ther. 2006;10:77-84. [Google Scholar]
- 41.Pearce PZ. Prehabilitation: preparing young athletes for sports. Curr Sports Med Rep. 2006;5:155-160. [DOI] [PubMed] [Google Scholar]
- 42.Etty Griffin LY. Neuromuscular training and injury prevention in sports. Clin Orthop Relat Res. 2003:53-60. [DOI] [PubMed] [Google Scholar]
- 43.Myer GD Ford KR Palumbo JP, et al. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19:51-60. [DOI] [PubMed] [Google Scholar]
- 44.Myer GD Chu DA Brent JL, et al. Trunk and hip control neuromuscular training for the prevention of knee joint injury. Clin Sports Med. 2008;27:425-448, ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Frisch A Croisier J-L Urhausen A, et al. Injuries, risk factors and prevention initiatives in youth sport. Br Med Bull. 2009;92:95-121. [DOI] [PubMed] [Google Scholar]
- 46.Myer GD Faigenbaum AD Chu DA, et al. Integrative training for children and adolescents: techniques and practices for reducing sports-related injuries and enhancing athletic performance. Physician Sportsmed. 2011;39:74-84. [DOI] [PubMed] [Google Scholar]
- 47.Kritz M. Movement Competency Screen: Function to athletic. International Conference on Applied Strength and Conditioning. Gold Coast, QLD; 2009. [Google Scholar]
- 48.Clifton DR Grooms DR Onate JA. Overhead deep squat performance predicts Functional Movement Screen™ score. Int J Sports Phys Ther. 2015;10:622-627. [PMC free article] [PubMed] [Google Scholar]
- 49.Pyne DB Montgomery PG Klusemann MJ, et al. Basketball Players. In: Tanner R Gore C, eds. Physiological Tests for Elite Athletes. 2nd ed. Champaign, IL: Human Kinetics; 2013: 273-287. [Google Scholar]
- 50.Legg J. Movement screen: Minimum Standards for AIS Basketball Scholarship. Canberra, ACT: Australian Institute of Sport and Basketball Australia; 2012. [Google Scholar]
- 51.Legg J. Basketball warm-ups incorporating basic movement patterns. Canberra, ACT: Australian Institute of Sport and Basketball Australia; 2012. [Google Scholar]
- 52.McCunn R aus der Fünten K Fullagar HHK, et al. Reliability and association with injury of movement screens: A critical review. Sports Med. 2016;46:763-781. [DOI] [PubMed] [Google Scholar]
- 53.McKeown I Taylor-McKeown K Woods C, et al. Athletic ability assessment: A movement assessment protocol for athletes. Int J Sports Phys Ther. 2014;9:862-873. [PMC free article] [PubMed] [Google Scholar]
- 54.Dennis RJ Finch CF Elliott BC, et al. The reliability of musculoskeletal screening tests used in cricket. Phys Ther Sport. 2008;9:25-33. [DOI] [PubMed] [Google Scholar]
- 55.Kritz M Cronin J Hume P. Screening the upper-body push and pull patterns using body weight exercises. Strength Cond J. 2010;32:72-82. [Google Scholar]
- 56.Cates W Cavanaugh J. Advances in rehabilitation and performance testing. Clin Sports Med. 2009;28:63-76. [DOI] [PubMed] [Google Scholar]
- 57.Hewit J Cronin J Hume P. Multidirectional leg asymmetry assessment in sport. Strength Cond J. 2012;34:82-86. [Google Scholar]
- 58.Myer GD Ford KR Hewett TE. Tuck jump assessment for reducing anterior cruciate ligament injury risk. Athletic Ther Today. 2008;13:39-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hamilton RT Shultz SJ Schmitz RJ, et al. Triple-hop distance as a valid predictor of lower limb strength and power. J Athl Train. 2008;43:144-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hewett TE Myer GD Ford KR, et al. Preparticipation physical examination using a box drop vertical jump test in young athletes: The effects of puberty and sex. Clin J Sport Med. 2006;16:298-304. [DOI] [PubMed] [Google Scholar]
- 61.Fitzgerald GK Lephart SM, Hwang JH, et al. Hop tests as predictors of dynamic knee stability. J Orthop Sports Phys Ther. 2001;31:588-597. [DOI] [PubMed] [Google Scholar]
- 62.Gustavsson A Neeter C Thomeé P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy. 2006;14:778-788. [DOI] [PubMed] [Google Scholar]
- 63.Padua DA Marshall SW Boling MC, et al. The Landing Error Scoring System (LESS) Is a valid and reliable clinical assessment tool of jump-landing biomechanics: The JUMP-ACL study. Am J Sports Med. 2009;37:1996-2002. [DOI] [PubMed] [Google Scholar]
- 64.Smith HC Johnson RJ Shultz SJ, et al. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Med. 2012;40:521-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Padua DA Boling MC Distefano LJ, et al. Reliability of the landing error scoring system-real time, a clinical assessment tool of jump-landing biomechanics. J Sport Rehab. 2011;20:145-156. [DOI] [PubMed] [Google Scholar]
- 66.Herrington L Myer GD Munro A. Intra and inter-tester reliability of the tuck jump assessment. Phys Ther Sport. [DOI] [PubMed] [Google Scholar]
- 67.Myer GD Ford KR Hewett TE. Rationale and clinical techniques for anterior cruciate ligament injury prevention among female athletes. J Athl Train. 2004;39:352-364. [PMC free article] [PubMed] [Google Scholar]
- 68.Herrington L. Knee valgus angle during landing tasks in female volleyball and basketball players. J Strength Cond Res. 2011;25:262-266. [DOI] [PubMed] [Google Scholar]
- 69.Myers BA Jenkins WL Killian C, et al. Normative data for hop tests in high school and collegiate basketball and soccer players. Int J Sports Phys Ther. 2014;9:596-603. [PMC free article] [PubMed] [Google Scholar]
- 70.Barber SD Noyes FR Mangine RE, et al. Quantitative assessment of functional limitations in normal and anterior cruciate ligament-deficient knees. Clin Orthop Relat Res. 1990:204-214. [PubMed] [Google Scholar]
- 71.Noyes FR Barber SD Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513-518. [DOI] [PubMed] [Google Scholar]
- 72.Ross MD Langford B Whelan PJ. Test-retest reliability of 4 single-leg horizontal hop tests. J Strength Cond Res. 2002;16:617-622. [PubMed] [Google Scholar]
- 73.Padua DA DiStefano LJ Beutler AI, et al. The Landing Error Scoring System as a screening tool for an anterior cruciate ligament injury-prevention program in elite-youth soccer athletes. J Athl Train. 2015;50:589-595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Myer GD Paterno MV Ford KR, et al. Rehabilitation after anterior cruciate ligament reconstruction: Criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36:385-402. [DOI] [PubMed] [Google Scholar]
- 75.Myer GD Ford KR Brent JL, et al. An integrated approach to change the outcome part I: neuromuscular screening methods to identify high ACL injury risk athletes. J Strength Cond Res. 2012;26:2265-2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hewett TE Lindenfeld TN Riccobene JV, et al. The effect of neuromuscular training on the incidence of knee injury in female athletes: A prospective study. Am J Sports Med. 1999;27:699-706. [DOI] [PubMed] [Google Scholar]
- 77.Hewett TE Ford KR Hoogenboom BJ, et al. Understanding and preventing ACL injuries: Current biomechanical and epidemiologic considerations - update 2010. N Am J Sports Phys Ther. 2010;5:234-251. [PMC free article] [PubMed] [Google Scholar]
- 78.Louw Q Grimmer K. Biomechanical factors associated with the risk of knee injury when landing from a jump. S Afr J Sports Med. 2006;18:18-23. [Google Scholar]
- 79.Backman LJ Danielson P. Low range of ankle dorsiflexion predisposes for patellar tendinopathy in junior elite basketball players: a 1-year prospective study. Am J Sports Med. 2011;39:2626-2633. [DOI] [PubMed] [Google Scholar]
- 80.Fong CM Blackburn JT Norcross MF, et al. Ankle-dorsiflexion range of motion and landing biomechanics. J Athl Train. 2011;46:5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hoch MC Staton GS McKeon PO. Dorsiflexion range of motion significantly influences dynamic balance. J Sci Med Sport. 2011;14:90-92. [DOI] [PubMed] [Google Scholar]
- 82.Hoch MC Staton GS Medina McKeon JM, et al. Dorsiflexion and dynamic postural control deficits are present in those with chronic ankle instability. J Sci Med Sport. 2012;15:574-579. [DOI] [PubMed] [Google Scholar]
- 83.Clanton TO Matheny LM Jarvis HC, et al. Return to play in athletes following ankle injuries. Sports Health. 2012;4:471-474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bennell KL Talbot RC Wajswelner H, et al. Intra-rater and inter-rater reliability of a weight-bearing lunge measure of ankle dorsiflexion. Aust J Physiother. 1998;44:175-180. [DOI] [PubMed] [Google Scholar]
- 85.Konor MM Morton S Eckerson JM, et al. Reliability of three measures of ankle dorsiflexion range of motion. Int J Sports Phys Ther. 2012;7:279-287. [PMC free article] [PubMed] [Google Scholar]
- 86.Gray G. Lower extremity functional profile. Adrian, MI: Wynn Marketing; 1995. [Google Scholar]
- 87.Plisky PJ Rauh MJ Kaminski TW, et al. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36:911-919. [DOI] [PubMed] [Google Scholar]
- 88.Leavey VJ Sandrey MA Dahmer G. Comparative effects of 6-week balance, gluteus medius strength, and combined programs on dynamic postural control. J Sport Rehab. 2010;19:268-287. [DOI] [PubMed] [Google Scholar]
- 89.Robinson R Gribble P. Kinematic predictors of performance on the Star Excursion Balance Test. J Sport Rehab. 2008;17:347-357. [DOI] [PubMed] [Google Scholar]
- 90.Overmoyer GV Reiser RFI. Relationships between asymmetries in functional movements and the Star Excursion Balance Test. J Strength Cond Res. 2013;27:2013-2024. [DOI] [PubMed] [Google Scholar]
- 91.Bressel E Yonker JC Kras J, et al. Comparison of static and dynamic balance in female collegiate soccer, basketball, and gymnastics athletes. J Athl Train. 2007;42:42-46. [PMC free article] [PubMed] [Google Scholar]
- 92.Olmsted LC Carcia CR Hertel J, et al. Efficacy of the Star Excursion Balance Tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train. 2002;37:501-506. [PMC free article] [PubMed] [Google Scholar]
- 93.Herrington L Hatcher J Hatcher A, et al. A comparison of Star Excursion Balance Test reach distances between ACL deficient patients and asymptomatic controls. The Knee. 2009;16:149-152. [DOI] [PubMed] [Google Scholar]
- 94.Aminaka N Gribble PA. Patellar taping, patellofemoral pain syndrome, lower extremity kinematics, and dynamic postural control. J Athl Train. 2008;43:21-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Robinson RH Gribble PA. Support for a reduction in the number of trials needed for the Star Excursion Balance Test. Arch Phys Med Rehabil. 2008;89:364-370. [DOI] [PubMed] [Google Scholar]
- 96.Hertel J Braham RA Hale SA, et al. Simplifying the star excursion balance test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36:131-137. [DOI] [PubMed] [Google Scholar]
- 97.Coughlan GF Fullam K Delahunt E, et al. A comparison between performance on selected directions of the star excursion balance test and the y balance test. J Athl Train. 2012;47:366-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Freeman JP Bird SP Sheppard J. Surfing performance, injuries and the use of the Y balance test J Aust Strength Cond. 2013;21:32-39. [Google Scholar]
- 99.Hegedus EJ McDonough SM Bleakley C, et al. Clinician-friendly lower extremity physical performance tests in athletes: a systematic review of measurement properties and correlation with injury. Part 2—the tests for the hip, thigh, foot and ankle including the star excursion balance test. Br J Sports Med. 2015;49:649-656. [DOI] [PubMed] [Google Scholar]
- 100.Fullam K Caulfield B Coughlan GF, et al. Kinematic analysis of selected reach directions of the Star Excursion Balance Test compared with the Y-Balance Test. J Sport Rehab. 2014;23:27-35. [DOI] [PubMed] [Google Scholar]
- 101.Brumitt J. Assessing athletic balance with the Star Excursion Balance Test. NSCA Perf Train J. 2008;7:6-7. [Google Scholar]
- 102.Gribble PA Hertel J. Considerations for normalizing measures of the Star Excursion Balance Test. Measurement in Physical Education and Exercise Science. 2003;7:89-100. [Google Scholar]
- 103.Bell DR Guskiewicz KM Clark MA, et al. Systematic review of the Balance Error Scoring System. Sports Health. 2011;3:287-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Burk JM Munkasy BA Joyner AB, et al. Balance Error Scoring System performance changes after a competitive athletic season. Clin J Sport Med. 2013;23:312-317. [DOI] [PubMed] [Google Scholar]
- 105.Docherty CL Valovich McLeod TC Shultz SJ. Postural control deficits in participants with functional ankle instability as measured by the Balance Error Scoring System. Clin J Sport Med. 2006;16:203-208. [DOI] [PubMed] [Google Scholar]
- 106.Rahn C Munkasy BA Barry Joyner A, et al. Sideline performance of the Balance Error Scoring System during a live sporting event. Clin J Sport Med. 2015;25:248-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Riemann BL Guskiewicz KM Shields EW. Relationship between clinical and forceplate measures of postural stability. J Sport Rehab. 1999;8:71-82. [Google Scholar]
- 108.Hunt TN Ferrara MS Bornstein RA, et al. The reliability of the modified Balance Error Scoring System. Clin J Sport Med. 2009;19:471-475. [DOI] [PubMed] [Google Scholar]
- 109.McGuine TA Greene JJ Best T, et al. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med. 2000;10:239-244. [DOI] [PubMed] [Google Scholar]
- 110.Harmon KG Drezner JA Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013;47:15-26. [DOI] [PubMed] [Google Scholar]
- 111.Werner G. Strength and conditioning techniques in the rehabilitation of sports injury. Clin Sports Med. 2010;29:177-191. [DOI] [PubMed] [Google Scholar]
- 112.McKay GD Goldie PA Payne WR, et al. A prospective study of injuries in basketball: a total profile and comparison by gender and standard of competition. J Sci Med Sport. 2001;4:196-211. [DOI] [PubMed] [Google Scholar]
- 113.de Noronha M França LC Haupenthal A, et al. Intrinsic predictive factors for ankle sprain in active university students: A prospective study. Scand J Med Sci Sports. 2013;23:541-547. [DOI] [PubMed] [Google Scholar]
- 114.Plisky PJ Gorman PP Butler RJ, et al. The reliability of an instrumented device for measuring components of the Star Excursion Balance Test. N Am J Sports Phys Ther. 2009;4:92-99. [PMC free article] [PubMed] [Google Scholar]